Abstract
Background
Child abuse and/or neglect is a serious issue, and in many cases, parents are the perpetrators. Hospital-based child protection teams (CPTs) play pivotal roles in the management of not only abused and/or neglected children but also of their parents; this is generally conducted through multidisciplinary practice. The aim of this study is to survey hospital-based CPT members to determine the professions they perceive to be most applicable to participation in CPTs.
Participants and methods
The participants were members of CPTs affiliated with hospitals that had pediatric emergency departments and which were located in Chiba Prefecture; specifically, 114 CPT members from 23 hospitals responded to this survey. The two main questionnaire items concerned are as follows: 1) each respondent’s evaluation of conducting assessments, providing support, and implementing multidisciplinary collaborative practice in the treatment of abusive and negligent parents, and 2) each CPT member’s opinion on the professions that are most important for CPT activities. An exploratory factor analysis (EFA) was performed to explore the factor structure of the data, and a correlation analysis was performed using the result obtained.
Results
The EFA returned two factors: multidisciplinary collaborative practice (α = 0.84) and assessment and support (α = 0.89). A correlational analysis showed that multidisciplinary collaborative practice had a positive correlation for obstetricians (r = 0.315, p = 0.001), neonatologists (r = 0.261, p = 0.007), midwives (r = 0.248, p = 0.011), and psychiatrists (r = 0.194, p = 0.048); however, assessment and support was only significantly correlated with midwives (r = 0.208, p = 0.039).
Conclusion
This study showed that hospital-based CPT members highly evaluate multidisciplinary collaborative practice for the management of abusive and/or negligent parents, and they believe that, in addition to pediatric physicians and nurses, perinatal care and mental health professionals are the most important participants in advanced CPT activities.
Introduction
Child abuse and/or neglect (CAN) is a serious global issue. Its prevalence is particularly notable in Japan, where an increase in the number of child abuse cases has been reported in recent years; for example, in 2014, ~90,000 CAN cases were reported to regional child consultation centers in Japan, which represents an increase by a factor of 80 on the situation 25 years ago.Citation1 Many countries have various child protection services tasked with preventing and saving abused or neglected children from the perpetrators;Citation2–Citation5 notably, in many cases, such children are abused and/or neglected by parents with histories of childhood abuse.Citation6,Citation7 In fact, according to data compiled by Japan’s Ministry of Health, Labor and Welfare in 2014, in 86% of child abuse cases, the suspected perpetrators were one or both parents.Citation1 As, in many countries, general hospitals that treat emergent pediatric patients frequently attend to abused or neglected children and their parents, most have organized hospital-based child protection teams (CPTs), and these teams play crucial roles in the management of abused or neglected children and their abusive or negligent parents and families.Citation8–Citation10
Previous studies have reported that members of CPTs can have various professions, with variations evident between hospitals, regions, and countries.Citation11–Citation13 Darlington et al reported that, to effectively assist children and their parents, child protection services must engage in interagency collaboration with mental health professionals.Citation14 However, according to the Japan’s first hospital-based CPT manual, which was published in 2011, pediatricians, medical social workers, and nurses of emergency outpatient units and pediatrics departments are defined as core members of CPT, with pediatric psychiatrists and psychologists categorized as extended members; moreover, psychiatrists are categorized as supplemental members, along with otorhinolaryngologists, urologists, and medical clerks.Citation15 However, there were few studies that discussed what professions CPT members need for consulting on abusive or negligent parents in multidisciplinary collaborative practice. We hypothesize that the real-world hospital-based CPT practice would differ from the team recommended in the Japan’s first hospital-based CPT manual. Our investigation in this regard is notable, as few previous studies have investigated the multidisciplinary collaborative practice-related needs of current CPTs in regard to caring for abusive or negligent parents.
Considering this, the aim of this study was to determine hospital-based CPT members’ evaluations of methods of caring for parents who abuse and/or neglect their children, and to determine individual CPT members’ opinions on the professions that are most important for CPT activities. To examine this, we distributed a questionnaire survey to general hospitals that had pediatric emergency care units and that were based in Japan’s Chiba Prefecture. The reasons to choose Chiba Prefecture as the area to survey for this study were that, first, the authors’ institutions are located in Chiba Prefecture, and second, Chiba Prefecture consists of rural and urban regions in a balanced manner.
Participants and methods
Study design and participants
A cross-sectional survey was utilized in this study. The questionnaire used was developed by the authors and directly mailed to 38 hospitals in Chiba Prefecture that had pediatric emergency departments; the respondents to this survey were members of CPTs or similar teams. The questionnaire survey was conducted between August 1 and 24, 2017.
The content of the questionnaire
The questionnaire consisted of two parts. The first part focused on characteristic information concerning the hospitals, such as whether they had a CPT or similar team; the manager of each CPT answered this part. If there was not a CPT or similar team in a hospital, the questionnaire asked the hospital’s staff who were in charge of CAN problems to answer it. The second part of the questionnaire contained three items. The first concerned an inquiry into the profiles of each respondent, such as their occupations. The second asked each respondent to evaluate the use of assessment, support, and multidisciplinary collaborative practice when caring for parents who abuse or neglect their children. In this second item, we divided the questionnaire contents concerning the respondents’ evaluations into 12 subcategories and asked the respondents to rate these using a four-point Likert scale ranging from 1 (insufficient) to 4 (sufficient). The third questionnaire item examined CPT members’ opinions on the professions that more proactively and regularly participate in CPT activities; specifically, for this item, respondents were asked to rate the relevance of 21 preselected professions using a four-point scale ranging from 1 to 4 (1 = not at all, 2 = slightly needed, 3 = frequently needed, 4 = constantly needed). If a hospital did not have a CPT or a similar team, the respondent did not need to answer the second part of the questionnaire.
Ethics
The survey protocol was reviewed and approved by the Institutional Review Board of Chiba University School of Medicine. We enclosed a letter of informed consent presenting this study’s purpose and assurances of confidentiality with the questionnaire. Completion and return of the questionnaire was considered to represent informed consent to participate in this study.
Primary and secondary outcomes
The primary outcome was to reveal the relationships between CPT members’ evaluations of the use of multidisciplinary collaborative practice to care for abusive or negligent parents and their opinions on the kinds of professions most suitable for participation in CPT activities. Then, using these results, we planned to perform a factor and correlation analyses to explore the factor structure of the data relating to the CPT members’ evaluations. The secondary outcome was to determine the types of hospitals for which the professions identified in the primary outcome analysis are most involved in multidisciplinary collaborative practice in terms of hospital-based CPT activities.
Statistical analysis
Statistical analysis was performed using the SPSS 19.0J software program (SPSS Inc., Chicago, IL, USA); for all statistical tests, a significance level of 0.05 was used. An exploratory factor analysis (EFA) with promax rotation was used for items concerning the respondents’ evaluations of methods of caring for parents; Cronbach’s alpha was also calculated for each component. Correlational analyses were performed using Pearson correlation. In cases where a correlation was detected, one-way analysis of variance (ANOVA) with Tukey’s multiple comparison tests was performed between each correlated profession and each hospital type.
Results
Responses were received from 23 hospitals, yielding a response rate of 60.5%. Of the 23 hospitals, 14 (60.9%) had CPTs, and we received answer sheets from 114 members of these CPTs. shows the hospitals’ demographics, specifically number of inpatient beds, pediatric inpatient beds, presence or absence of birthing facilities, and number of deliveries in the hospital per year. Meanwhile, shows the respondents’ gender, ages, and occupations. Finally, the characteristics of the CPTs are shown in . Some of the hospitals answered that they have comprehensively organized family support teams that play not only a role as CPT but also roles of addressing domestic violence or elder abuse. Therefore, showed that the CPTs surveyed by this study actually consulted on various family problems.
Table 1 Characteristics of the hospitals
Table 2 Distribution of respondents in terms of gender, age, and profession (n=114)
Table 3 Characteristics of CPTs (n = 14)
CPT members’ attitudes toward means of caring for abusive and/or negligent parents
An EFA was conducted to explore the factor structure of the data. As the data were normally distributed and the factors were expected to be correlated, a maximum likelihood estimation procedure was used with a promax rotation method. These analyses returned a two-factor solution that explained 54.7% of the variance. The first factor, explaining 33.5% of the variance, corresponded to the assessment and support scale; meanwhile, the second factor, explaining 21.2% of the variance, reflected the Multidisciplinary Collaborative Practice Scale. Thus, the EFA returned the two factors of multidisciplinary collaborative practice (α = 0.84) and assessment and support (α = 0.89). presents the items and their factor loadings.
Table 4 Factor loadings of the items relating to approaches to caring for parents treated by CPTs
Correlations between CPT care and highly evaluated professions
The correlational analysis showed that multidisciplinary collaborative practice has a positive correlation for obstetricians (r = 0.315, p = 0.001), neonatologists (r = 0.261, p = 0.007), midwives (r = 0.248, p = 0.011), and psychiatrists (r = 0.194, p = 0.048); however, the factor of assessment and support was determined to only be significantly correlated with midwives (r = 0.208, p = 0.039) ().
Table 5 Correlations between “the assessment and support scale,” “the multidisciplinary collaborative practice scale,” and necessary professions
Efficiency of each of the four professions and treatment of pregnant women with high psychosocial risk
According to the results of the abovementioned correlation analysis, the correlated professionals are midwives, obstetricians, psychiatrists, and neonatologists. Since these are considered to be related to the perinatal period, in order to investigate whether there is a difference between hospitals with different functions or character in regard to opinions on the necessity of each profession, we performed a one-way ANOVA in which we distributed the necessity of each of the four professions as dependent variables and three groups of hospitals as independent variables. Specifically, these three groups concerned: 1) hospitals with no delivery facilities, 2) hospitals possessing delivery facilities but incapable of treating pregnant women with a high psychosocial risk (these are individuals for whom CPTs must be especially diligent, as they may abuse or neglect their offspring after childbirth), and 3) hospitals possessing delivery facilities and capable of treating pregnant women with a high psychosocial risk.
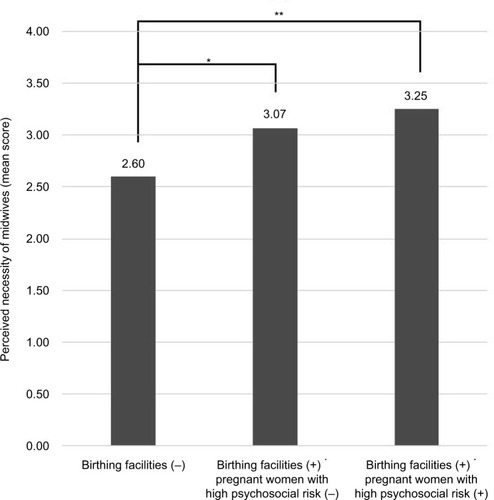
Consequently, a significant main effect was observed for all four professions, indicating that there is a significant difference between the abovementioned three groups in regard to the perceived necessity of each profession (midwives: F [2,109]=7.797, p = 0.001; obstetricians: F [2,108]=15.263, p < 0.001; neonatologists: F [2,109]=7.541, p = 0.001; psychiatrists: F [2,108]=5.181, p = 0.007). On the basis of these results, a multiple comparison using Tukey’s test was performed; the results are shown in –.
Figure 1 Result of the multiple comparison using Tukey’s test: Psychiatrists.
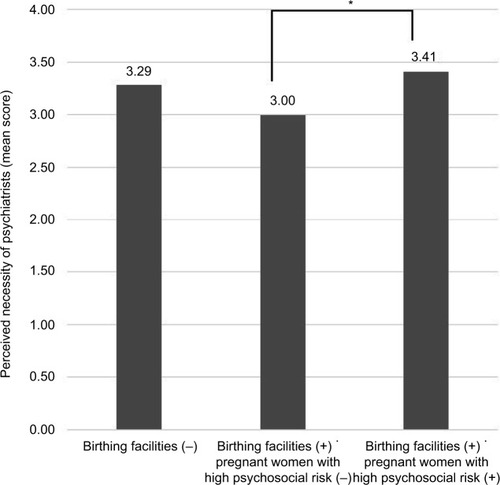
Figure 2 Result of the multiple comparison using Tukey’s test: Obstetricians.
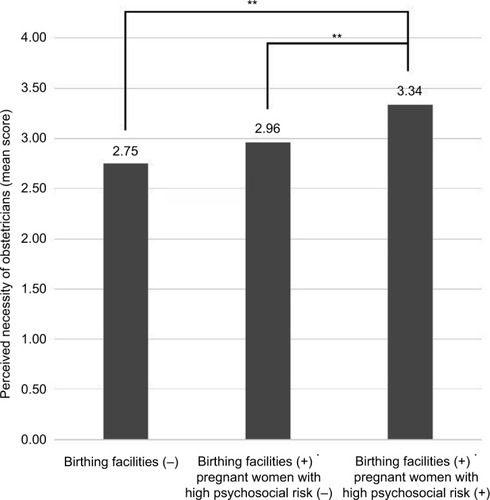
Figure 3 Result of the multiple comparison using Tukey’s test: Neonatologists.
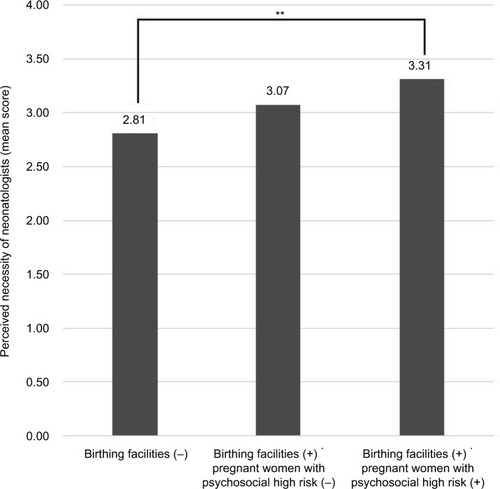
Figure 4 Result of the multiple comparison using Tukey’s test: Midwives.
Discussion
In this study, three important findings concerning the management of Japanese CPTs, which currently consist of four core professions (pediatricians, medical social workers, emergency unit nurses, and pediatric department nurses), deserve particular mention. First, through the use of factor analysis on the CPT members’ responses, our study determined that the means of caring for parents who abuse or neglect their children can be divided into two measures: 1) assessment and support and 2) multidisciplinary collaborative practice. Second, this study demonstrates the degree to which CPT members’ evaluations of multidisciplinary collaborative practice concerning caring for abusive or negligent parents is positively correlated with their opinions on the necessity of the participation of obstetricians, neonatologists, midwives, and psychiatrists in CPT activities. Third, our results show that the abovementioned four professions are needed significantly more in hospitals with birth facilities and that are capable of treating pregnant women with high psychosocial risk than in hospitals without birth facilities or that are incapable of providing such treatment.
In our study, the CPT members’ evaluations of means of caring for abusive and negligent parents showed that multidisciplinary collaborative practice is distinguished from assessment and support. This finding indicates that multidisciplinary collaborative practice in CPT activity differs from the other two activities in terms of the quality of work involved. While it is likely that most CPT members provide care by assessing and supporting their patients through teamwork, it is probable that these workings are common and basic among not only child protection services but also most health care areas. Meanwhile, the effectiveness of multidisciplinary collaboration has been shown in various health care research studies.Citation16–Citation18 In particular, one study demonstrated that, in experimental psychological tasks, collective intelligence produced through group performance is superior to general intelligence.Citation19 Given that child protection services require multidisciplinary collective intelligence to address CAN, it is clear that the organization and management of CPT in Japan should be more collaborative and involve multidisciplinary professional teams.
Our findings demonstrate that CPT members’ evaluations of the use of multidisciplinary collaborative practice for the cases of abusive or negligent parents are positively correlated with their opinions concerning the necessity of the participation of obstetricians, neonatologists, midwives, and psychiatrists in CPT activities. Given that these four professions are similar in that they are involved in perinatal health care, including parental mental health, the findings of the present study suggest that multidisciplinary collaborative practice as a CPT activity should be particularly implemented from the antenatal period in order to prevent children experiencing CAN and to care for their parents and families. These measures are not unprecedented; the UK’s guidelines for obstetricians and gynecologists state that obstetricians, midwives, and health outreach nurses should comprehend mental health issues and the relationship between partners for both pregnant and postpartum women;Citation20 moreover, the Scottish Intercollegiate Guidelines Network has placed an emphasis on the execution of multidisciplinary practice among perinatal health care professions.Citation21 To increase the effectiveness of protection for children who are at potential risk of experiencing CAN, CPTs should implement early interventions for pregnant women with a high psychosocial risk and their families from the beginning of the pregnancy period.
In addition, in this study, the abovementioned four professions (obstetrician, neonatologist, midwife, and psychiatrist) are determined to be needed significantly more in hospitals with birth facilities and that are capable of treating pregnant women with high psychosocial risks than in hospitals without such birth facilities or that are incapable of providing such treatment. These findings indicate that central district general hospitals with birth facilities capable of treating cases at risk of experiencing CAN should organize advanced hospital-based CPTs that include obstetricians, neonatologists, midwives, and psychiatrists. In addition, several studies of other countries’ hospitals have reported that CPTs should consist of mental health specialists such as psychiatrists or psychologistsCitation13,Citation22 or child and adolescent psychiatrists and psychologists.Citation11,Citation12 Given our findings and the results of the previous studies mentioned earlier, it is clear that CPTs should be proactively involved from the antenatal period with pregnant women, along with their partners and families, who are at risk of engaging in CAN, and that regular members of hospital-based CPTs should be not only pediatricians and pediatric nurses but also professionals engaged in pregnancy and delivery and/or psychologists or psychiatrists; the number of members of each profession should be in proportion to each hospital’s size.
Limitations
There are some limitations to this study. First, despite a credible response rate of 60.5%,Citation23,Citation24 as with any self-selecting sample, there is a potential for bias; it is possible that CPT members who specialized in and were with enthusiasm for the subject of CAN participated in the study. Second, all of the hospitals to which we mailed the questionnaire were located in Chiba Prefecture, which is the sixth most populous prefecture in Japan and is located in the Greater Tokyo Area. Hence, the result may only reflect regional characteristics. Third, the questionnaire did not obtain details of the cases that each CPT commonly addresses. Fourth, the present study was designed with limited information concerning each CPT member and hospital, and conducted in a localized area, Chiba Prefecture. Further studies are needed to identify whether the present findings are reliable and generalizable to other regions in multiple areas. Future studies should establish the practical and ethical conditions for such data collection and analysis so that an understanding of how the contexts of individual cases impact multidisciplinary collaborative practice can be developed.
Conclusion
This study showed that hospital-based CPT members, who highly evaluated multidisciplinary collaborative practice as a method of caring for abusive or negligent parents, believe that the participation of perinatal care and mental health professionals, obstetricians, neonatologists, midwives, and psychiatrists in advanced CPT activities is necessary. The findings of this study also indicate that advanced CPT activities should be extended to not only suspected abused or neglected children but also pregnant women, who CPT should carefully observe to prevent them from abusing or neglecting their offspring before childbirth through multidisciplinary collaborative practice involving perinatal care and mental health professionals.
Author contributions
Study concept and design: AO, TH. Making contents of questionnaire: AO, TH, MT, AM, JO, ME, MS, NS. Analysis and interpretation of data: AO, TH, MT. Drafting of manuscript: AO, TH, MT. Study supervision: MS, MI. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing. We declare that this work was financially supported by Chiba University Psychiatry Doumonkai (Chiba, Japan) and Chiba University Graduate School of Medicine (Chiba, Japan). We thank all medical staff for their participation in this study. We further thank the clinical research nurses (Kaoru Ikeda, Chisako Fujishiro, and Chiharu Fujita), the research assistant (Komako Ito), and the members of CPT in Chiba University Hospital (Kyoko Tanabe, Ryoko Igarashi, Saki Eshima, and Mizuho Kawasaki) for supporting this work at Chiba University Hospital.
Disclosure
Dr. Hashimoto reported personal fees from research support of a clinical trial that the bracket global company manages. Dr. Iyo received consultant fees from Janssen, Eli Lilly, Otsuka, and Meiji Seika Pharma and reports honoraria from Janssen, Eli Lilly, Otsuka, Meiji Seika Pharma, Astellas, Dainippon Sumitomo, Ono, Mochida, MSD, Eisai, Daiichi-Sankyo, Novartis, Teijin, Shionogi, Hisamitsu, and Asahi Kasei. The authors report no other conflicts of interest in this work.
References
- Report on Social Welfare Administration and Services 2014 [PDF on the Internet, in Japanese only]Ministry of Health, Labour and Welfare [updated 2015 December 10]. Available from: http://www.mhlw.go.jp/toukei/saikin/hw/gyousei/14/dl/gaikyo.pdfAccessed October 26, 2017
- PalusciVJChild protection and the development of child abuse pediatrics in New York CityJ Forensic Leg Med20175215916728942263
- BalsellsMAFuentes-PeláezNPastorCListening to the voices of children in decision-making: A challenge for the child protection system in SpainChild Youth Serv Rev201779418425
- PengJShaoJZhuHA systems approach to addressing child maltreatment in China: China needs a formalized child protection systemChild Abuse Negl201550334126410480
- GillesSFloraBMaking better sense of children’s trajectories in child protection in FranceChild Youth Serv Rev201773145148
- LeveyEJGelayeBBainPA systematic review of randomized controlled trials of interventions designed to decrease child abuse in high-risk familiesChild Abuse Negl201765485728110205
- van der PutCEBouwmeester-LandweerMBRLandsmeer-BekerEAScreening for potential child maltreatment in parents of a newborn baby: the predictive validity of an Instrument for early identification of Parents At Risk for child Abuse and Neglect (IPARAN)Child Abuse Negl20177016016828618320
- TienIBauchnerHReeceRMWhat is the system of care for abused and neglected children in children’s institutions?Pediatrics200211061226123112456923
- SedlakAJSchultzDWellsSJChild protection and justice systems processing of serious child abuse and neglect casesChild Abuse Negl200630665767716782193
- BenbenishtyRChenWDecision making by the child protection team of a medical centerHealth Soc Work200328428429214679707
- Thun-HohensteinLInterdisciplinary child protection team work in a hospital settingEur J Pediatr2006165640240716622657
- JudALipsULandoltMACharacteristics associated with maltreatment types in children referred to a hospital protection teamEur J Pediatr2010169217318019475422
- BenbenishtyRJedwabMChenWPredicting the decisions of hospital based child protection teams to report to child protective services, police and community welfare servicesChild Abuse Negl2014381112423948314
- DarlingtonYFeeneyJARixonKInteragency collaboration between child protection and mental health services: practices, attitudes and barriersChild Abuse Negl200529101085109816315352
- The management manual of hospital-based CPT [PDF on the Internet, in Japanese only]Japanese Medical Society on Child Abuse and Neglect [updated 2011 March]. Available from: https://jamscan.jp/manual.htmlAccessed October 26, 2017
- TrujilloJAFernandezYGhafooriLLokKValenciaAInterdisciplinary family conferences to improve patient experience in the Neonatal Intensive Care UnitHealth Soc Work201742424124629025070
- ZerilloJASchouwenburgMGvan BommelACMColorectal Cancer Working Group of the International Consortium for Health Outcomes Measurement(ICHOM)An International collaborative standardizing a comprehensive patient-centered outcomes measurement set for colorectal cancerJAMA Oncol20173568669428384684
- RubensteinLZJosephsonKRWielandGDEnglishPASayreJAKaneRLEffectiveness of a geriatric evaluation unit. A randomized clinical trialN Engl J Med198431126166416706390207
- WoolleyAWChabrisCFPentlandAHashmiNMaloneTWEvidence for a collective intelligence factor in the performance of human groupsScience2010330600468668820929725
- Management of Women with Mental Health Issues during Pregnancy and the Postnatal Period (Good Practice No. 14) [homepage on the Internet]Royal College of Obstetricians and Gynaecologists [updated 2011 September 6]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/good-practice-14/Accessed October 26, 2017
- Management of perinatal mood disorders [homepage on the Internet]the Scottish Intercollegiate Guidelines Network [updated 2012 March]. Available from: http://www.sign.ac.uk/our-guidelines.htmlAccessed October 26, 2017
- Child Protection Team Program Policy and Procedure Handbook [PDF on the Internet]Florida Department of Health [updated 2015 June]. Available from: http://www.floridahealth.gov/alternatesites/cms-kids/providers/prevention/documents/handbook_cpt.pdfAccessed October 26, 2017
- DelnevoCDAbatemarcoDJSteinbergMBPhysician response rates to a mail survey by specialty and timing of incentiveAm J Prev Med200426323423615026104
- AschDAJedrziewskiMKChristakisNAResponse rates to mail surveys published in medical journalsJ Clin Epidemiol19975010112911369368521
