Abstract
Introduction:
Overactive bladder (OAB) is a prevalent and persistent condition that is often under-diagnosed and under-treated, and which frequently requires tailored treatment for successful management.
Methods:
This consensus opinion-based review summarizes the discussions of a group of experts in the field of OAB that were assembled to evaluate the importance of correct diagnosis and appropriate pharmacotherapy in patients with OAB.
Results:
A thorough diagnostic process is crucial for allowing exclusion of underlying medical issues and differentiation from genitourinary conditions other than OAB. In addition, selecting the most appropriate pharmacotherapy needs to be carefully considered in the context of each patient with OAB. In general, patients with OAB tend to be older with various comorbidities and often receiving multiple concomitant medications. Treatment decisions should take into consideration the differing potential for antimuscarinic medications to alter cognitive and cardiovascular functions, both of which may be compromised in this patient population.
Conclusion:
Tailoring treatment to individual patients by comprehensive patient assessment may lead to more effective management of patients with OAB, especially those receiving polypharmacy for comorbidities.
Introduction
This short communication is a consensus opinion-based review highlighting the discussions of an advisory board of renowned experts in the field of overactive bladder (OAB). These professionals, who are all specialists in urogynecology or obstetrics and gynecology, were assembled to provide their perspectives on the importance of correct diagnosis and effective, appropriate treatment of patients with OAB. The remit of the advisory board was to discuss factors affecting diagnosis and successful pharmacotherapy of OAB with antimuscarinic agents. The participants who provided valuable input into the discussions and gave approval for this article are recognized in the acknowledgments.
OAB defined
OAB comprises a group of symptoms (ie, urinary urgency usually accompanied by increased frequency of micturition and nocturia with or without urgency incontinence), in the absence of urinary tract infection or other obvious pathology.Citation1 This condition is highly prevalent, affecting approximately 12% of adults in Europe and Canada.Citation2 Prevalence increases with advancing age and is similar for men and women, particularly in the population ≥60 years of age.Citation2 OAB can be a life-long, persistent (often lasting for at least 10 years), and progressive (from OAB without incontinence to OAB with incontinence) condition.Citation3,Citation4 Furthermore, OAB has a significant detrimental impact on patients’ quality of life, which is often greater than that resulting from other chronic diseases such as diabetes.Citation5 It is therefore crucial that treatment strategies take into account that patients often require effective and well tolerated therapy for prolonged periods.
OAB: potential barriers to initial diagnosis
Recent publications have focused on the fact that OAB is undertreated, revealing that up to 76% of diagnosed patients remain untreated,Citation6,Citation7 but correct diagnosis is essential to ensure appropriate management of patients with urinary symptoms. Diagnosis may be hampered by patients failing to discuss their OAB symptoms, perhaps through embarrassment or the misconception that this condition is a normal part of aging and cannot be treated.Citation5 Although physicians rely on patients’ complaints to trigger action, primary care physicians may not ask their patients about OAB symptoms,Citation8 possibly due to time constraints, or lack of knowledge or awareness of available effective treatments. To overcome these barriers, questions on incontinence and bladder habits should ideally be included in the primary care physicians’ list of standard screening questions for all adult patients.Citation8
Patient assessment
As the pathophysiology of OAB is not fully understood, the syndrome is a diagnosis of exclusion. Therefore, a holistic approach to patient assessment should be employed,Citation5 including appraisal of a patient’s genitourinary history as well as diagnostic tools and physical examination.
When a patient presents with symptoms that are potentially indicative of OAB, it is important to rule out other conditions that produce urological symptoms, such as bladder cancer, urinary tract infection, urethral inflammation, interstitial cystitis or simply urogenital atrophy, before initiating treatment. Initial assessments should focus on patients’ symptoms, but physical examination and diagnostic procedures should also be performed. Physical examination including pelvic examination (particularly in post-menopausal women) will exclude urogenital atrophy and pelvic organ prolapse. Indeed, it has been estimated that 23%–88% of patients with pelvic organ prolapse have varying combinations of urgency, urgency incontinence, frequency and/or nocturia.Citation9 Urinalysis should determine if urinary tract infection (UTI) or urethral inflammation is present. UTI is the most common cause of bothersome urinary symptoms in women of all ages and treatable with antibiotics, however, symptoms of OAB will persist even after successful treatment. In addition, routine measuring of post-void residual (PVR) volumes following micturition is often useful for determining urinary retention issues, especially in patients with bladder and prolapse symptoms, elderly patients with voiding symptoms and/or recurrent urinary tract infections, patients with neurogenic bladder and voiding dysfunction, and those patients with symptoms suggestive of decreased detrusor contractility or bladder outlet obstruction.Citation5 The volume of residual urine can be measured either directly with a catheter inserted into the bladder (in-and-out catheterization), or indirectly with an ultrasound scan.
In the majority of patients with symptoms indicative of OAB, urodynamic assessment (beyond PVR testing) is not usually required. However, in some cases urodynamic assessment will provide a definitive diagnosis.Citation5 Cystometry and measurement of PVR will exclude detrusor hyperactivity with impaired contractility (DHIC) during voiding, as 70% of women over the age of 70 years with symptoms of OAB may have DHIC.Citation10 Furthermore, in cases where treatment with antibiotics and antimuscarinics has failed to improve symptoms, cytology and cystoscopy would exclude bladder neoplasias and interstitial cystitis. Indeed, urodynamic studies are indicated for specific patient types: OAB refractory to pharmacotherapy based on symptoms; women with suspected outlet obstruction; and OAB associated with concurrent neurological disease. However, the role of urodynamic assessment in OAB diagnosis is not clearly defined currently. Evidence has shown that urodynamic diagnosis of detrusor overactivity and symptomatic diagnosis of OAB only co-existed in 54% of patients classified as having OAB.Citation11
Bladder diaries or frequency/volume charts are very helpful but often underutilized tools in the diagnosis of OAB that allow physicians to review patients’ accurate record of micturition frequency, number of incontinence episodes and urinary leakage, as well as fluid intake. There are various different formats for the bladder diary but all assess similar parameters. Bladder diaries can be used to evaluate stress and urgency associated with incontinence (OAB-related incontinence), thereby helping physicians to distinguish between stress incontinence and urgency incontinence. Differentiating between these two conditions is important for selecting appropriate management strategies. Stress incontinence should be managed with pelvic floor exercises for at least 3–6 months before referral for surgery. Recommended first-line therapy for OAB includes behavioral interventions (lifestyle modifications, fluid management, bladder retraining, and pelvic floor exercises) with or without pharmacotherapy. Many patients with OAB start on anticholinergic therapy with bladder training, then after 1 month are reviewed and advised on next steps. Continual reassessment of the patient may aid symptom management, especially with pharmacotherapy.
Determination of a patient’s medical history is not only vital for assessing genitourinary history but also comorbidities, which may affect treatment options. Looking at full patient profiles rather than just their symptoms could aid treatment choice and, importantly, allow treatment to be individualized to each patient’s needs.
Comorbidities and antimuscarinic therapy
Antimuscarinic agents are the mainstay of pharmacotherapy for OAB. It is widely agreed that antimuscarinic agents have similar efficacy but different tolerability and safety profiles. One of the main differences is the varying potential of antimuscarinics to alter cognitive and cardiac functions.Citation12,Citation13 These potential effects are of particular concern for OAB patients, who tend to be older and are often receiving concomitant medication for a variety of other conditions, including those relating to cognitive and cardiac function ().Citation14–Citation16 Therefore, the patient’s concomitant medications and comorbidities should be carefully considered when selecting antimuscarinic therapy for the management of OAB, which highlights the need for tailored therapy.
Figure 1 The prevalence of overactive bladder (OAB), taking prescription medicines and comorbidities all increase with age.Citation14–Citation16
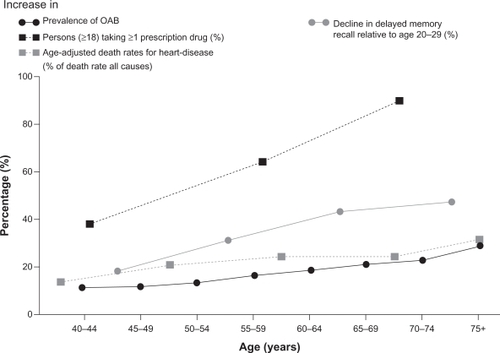
Increasing age has been associated with reduced cognitive function and greater permeability of the blood–brain barrier, which can leave patients more vulnerable to the central nervous system effects of drugs with anticholinergic properties.Citation12 To date, darifenacin has the most clinical evidence (three randomized, double-blind, placebo-controlled studies in healthy participants, n = 302) for a lack of effect on cognitive function. In contrast, oxybutynin has been associated with a decline in cognitive function, especially memory loss, compared with placebo, darifenacin and tolterodine.Citation12 Memory loss is of particular concern in older patients who may be receiving concomitant medication. A recent case study reported that memory loss secondary to administration of oxybutynin in a 66-year-old female with OAB led to non-adherence to medication regimens.Citation17
Specific data on cognitive function are limited for other antimuscarinic agents, although small clinical studies with tolterodine (n = 22 healthy participants), solifenacin (n = 12 healthy participants) and trospium (n = 12 patients with OAB) have compared these agents favorably with both placebo and/or oxybutynin.Citation12,Citation18,Citation19
Impairment of cognitive function may also be increased as a result of ‘hidden’ anticholinergic effects of concomitant medications administered for a variety of comorbid conditions unrelated to OAB. These medications add to the total anticholinergic burden on the patient and may cause non-degenerative mild cognitive impairment.Citation20 Commonly prescribed drugs that have anticholinergic effects include: cimetidine, prednisolone, digoxin, furosemide, isosorbide dinitrate, warfarin, and codeine. Therefore, awareness of concomitant comorbidities and associated medications is of particular importance and careful management of patients’ medication is required to avoid prescribing agents with potential drug–drug interactions related to their mechanisms of action and/or side-effect profiles. For example, the administration of anticholinergics for OAB therapy may potentially occur at the same time as cholinesterase inhibitors (eg, donepezil, rivastigmine), which are typically used to improve memory and cognition in Alzheimer’s disease. In addition, medications often used in persons with diabetes, such as thiazolidinediones for glucose control and gabapentin for neuropathic pain, can lead to nocturia; and the use of anticholinergic agents in the treatment of Parkinson’s disease can impair bladder emptying.Citation21
In addition to the decline in cognitive function, advancing age is associated with increasing prevalence of cardiovascular (CV) disease.Citation16 Moreover, CV disease occurs more frequently in patients with OAB than those without OAB.Citation22 In a recent US database analysis of >6000 patients with OAB, 39% had some type of CV comorbidity at the time of OAB diagnosis compared with 21% of age-matched non-OAB patients (P < 0.0001).Citation22 Hypertension (21%), diabetes (8%), CV symptoms (6%), and ischemic heart disease (6%) were the most common CV conditions.Citation22
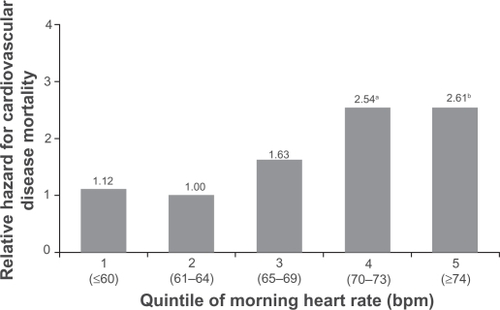
Antimuscarinics have the potential to increase CV risk through prolongation of the QT interval, which may lead to potentially fatal cardiac tachyarrhythmia or torsade de pointes,Citation23 and increased heart rate.Citation13,Citation24 Faster resting heart rate, even by single digit increases, is associated with an increased risk of CV events and death in patients with and without CV disease ().Citation25 In an observational longitudinal study, an increase in heart rate of only 5 bpm was associated with a 16%–17% increase in mortality (P = 0.03).Citation25 Added to this, analysis of a separate US database indicated that almost 40% of patients with OAB had an elevated heart rate of ≥80 bpm before receiving antimuscarinic treatment.Citation22 Hence, any further increases in heart rate resulting from antimuscarinic treatment may add to the CV risk. Selected antimuscarinic agents, such as tolterodine, have been associated with increased heart rate (between 2–12 bpm) compared with placebo in clinical studies enrolling healthy volunteers.Citation13,Citation24 In contrast, darifenacin did not increase heart rate from baseline compared with placebo or tolterodine.Citation13,Citation24 Although the magnitude of heart rate effects observed in these studiesCitation13,Citation24 may not be of consequence in healthy volunteers, the same changes may have a greater impact in patients with an established higher risk for CV events and CV comorbidities, such as patients with OAB.
Figure 2 Increased heart rate is associated with increased cardiovascular mortality.
Abbreviation: bpm, beats per minute.
These data demonstrate that patient comorbidities should be considered carefully during the treatment of OAB. However, as there are no guidelines for the treatment of patients with OAB and comorbidities, the medication needs of each patient should be individually assessed and resulting treatment tailored appropriately.
Conclusion
The expert panel noted that ideally more patients should be treated successfully in the primary care setting, which would leave only those patients requiring specialist help being referred as and when appropriate. However, the main findings from the advisory board centered on the need for more comprehensive assessment of patients, which should assist in the correct diagnosis of OAB, and suitable pharmacotherapy for patients with OAB and comorbidities. In particular, increased awareness of the differences between antimuscarinic agents should allow for appropriate treatment of patients with OAB and comorbidities, who may be receiving concomitant medications. Antimuscarinics have differing potential to negatively impact on patients’ CV and CNS function, which could result in a reduction of quality of life, hence patients may benefit from treatment tailored towards their individual needs.
Acknowledgements
The author would like to acknowledge and thank his fellow advisory board participants, the Specialist Advisory Group on OAB (Lake Como, Italy, June 2009), who provided their input and approval of this short communication: Peter Dwyer (Australia); Jorge Haddad (Brazil); Karin Glavind (Denmark); Heinz Koelbl (Germany); Charlotte Greppe (Sweden); Annette Kuhn-Dörflinger (Switzerland); Linda Cardozo (UK); Vikram Khullar (UK). The author would also like to acknowledge Gunnar Lose (Denmark) who provided input during the advisory board.
The author would also like to thank Claire Chinn (professional writer with ACUMED®) for her assistance in drafting and revising this manuscript.
Disclosure
Funding for the original advisory board, editorial support, drafting and revising this article was provided by Novartis Pharma AG.
References
- HaylenBTDe RidderDFreemanRMAn International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunctionNeurourol Urodyn201029142019941278
- IrwinDEMilsomIHunskaarSPopulation-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC studyEur Urol20065061306131417049716
- GarnettSSwithinbankLEllis-JonesJThe long-term natural history of overactive bladder symptoms due to idiopathic detrusor overactivity in womenBJU Int2009104794895319389015
- MalmstenUGMolanderUPeekerRIrwinDEMilsomIUrinary incontinence, overactive bladder, and other lower urinary tract symptoms: a longitudinal population-based survey in men aged 45–103 yearsEur Urol201058114915620356669
- AbramsPWeinAThe overactive bladder: a widespread but treatable conditionStockholmErik Sparre Medical AB1998
- BallertKNUnder treatment of overactive bladderJ Urol201018341282128320171673
- HelfandBTEvansRMMcVaryKTA comparison of the frequencies of medical therapies for overactive bladder in men and women: analysis of more than 7.2 million aging patientsEur Urol201057458659120036783
- CohenSJRobinsonDDuganECommunication between older adults and their physicians about urinary incontinenceJ Gerontol A Biol Sci Med Sci1999541M34M3710026660
- de BoerTASalvatoreSCardozoLPelvic organ prolapse and overactive bladderNeurourol Urodyn2010291303920025017
- ResnickNYallaSVLaurinoEThe pathophysiology of urinary incontinence among institutionalized elderly personsN Engl J Med19893201172909873
- DigesuGAKhullarVCardozoLSalvatoreSOveractive bladder symptoms: do we need urodynamics?Neurourol Urodyn200322210510812579626
- KayGGEbingerUPreserving cognitive function for patients with overactive bladder: evidence for a differential effect with darifenacinInt J Clin Pract200862111792180018699842
- OlshanskyBSpieringsEBrumJValidation of the differential cardiovascular effects of the antimuscarinic agents, darifenacin and tolterodine, in a randomized, placebo-controlled, 3-way crossover studyUro Today Int J200924
- CrookTHLebowitzBDPirozzoloFJRecalling names after introduction: changes across the adult life span in two culturesDev Neuropsychol199392103113
- MilsomIAbramsPCardozoLRobertsRGThuroffJWeinAJHow widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence studyBJU Int200187976076611412210
- US Department of Health and Human Services National Center for Health StatisticsCenters for Disease Control and Prevention and National Center for Health Statistics2009 Available from: http://www.cdc.gov/nchs/.
- NyeAMClinardVBBarnesCLMedication nonadherence secondary to drug-induced memory lossConsult Pharm201025211712120211824
- StaskinDKayGTannenbaumCTrospium chloride has no effect on memory testing and is assay undetectable in the central nervous system of older patients with overactive bladderInt J Clin Pract20106491294130020561092
- WesnesKAEdgarCTretterRNBolodeokuJExploratory pilot study assessing the risk of cognitive impairment or sedation in the elderly following single doses of solifenacin 10 mgExpert Opin Drug Saf20098661562619747069
- AncelinMLArteroSPortetFDupuyAMTouchonJRitchieKNon-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort studyBMJ2006332753944544916473859
- DuBeauCETreatment of OAB in geriatric patientsClin Geriatr200715Suppl 246
- AnderssonKESarawateCKahlerKHStanleyELKulkarniASCardiovascular morbidity, heart rates and use of antimuscarinics in patients with overactive bladderBJU Int2010106226827419922546
- RodenDMDrug-induced prolongation of the QT intervalN Engl J Med2004350101013102214999113
- SchiffersMSauermannPSchurchBThe effect of tolterodine 4 and 8 mg on the heart rate variability in healthy subjectsWorld J Urol201028565165620140437
- HozawaAOhkuboTKikuyaMPrognostic value of home heart rate for cardiovascular mortality in the general population: the Ohasama studyAm J Hypertens20041711 Pt 11005101015533725