Abstract
Background:
We recently indicated that patient age on its own is not a determinant of quality of allied health care received after an acute stroke. It has not been tested whether other non-age variables influence care decisions made by allied health professionals. This paper explores demographic and stroke-related variables that are putatively associated with the quality of care provided to acute stroke patients by allied health professionals.
Methods:
Data were retrospectively audited from 300 acute stroke patient records regarding allied health care. Compliance with each of 20 indicators of allied health care quality was established. The influence of various demographic and stroke-related variables on each performance indicator was examined. We undertook a series of analyses using univariate logistic regression models to establish the influence of these variables on care quality.
Results:
Patient age had a significant correlation with only one process indicator (early mobilization). Seven variables, including stroke severity and level of dependence, were associated with patient age. The majority of these age proxies had significant associations with process indicator compliance. Correlations between non-age variables, in particular stroke severity and comorbidity, suggest the potential for complex confounding relationships between non-age variables and quality of allied health care.
Conclusion:
Compliance with individual indicators of allied health care was significantly associated with variables other than patient age, and included stroke severity, previous independence, comorbidities, day of admission, stroke unit admission, and length of stay. The inter-relationships between these non-age variables suggest that their influence on quality of care is complex.
Introduction
Ensuring the highest quality of health care for all stroke patients is important in the current climate of scarce resources and the increasing burden of stroke to the health sector. There is a strong international momentum to improve the quality of acute stroke management.Citation1 This is supported by high level evidence that now underpins many acute stroke interventions, including several provided by allied health professionals.Citation2
Although much of the current research on quality in stroke care has focused on factors that may influence medical interventions,Citation3–Citation7 allied health professionals are similarly interested in ways to implement best practice care.Citation8 Allied health professionals are members of multidisciplinary stroke teams and contribute to patient care from early in acute admission, through the stroke rehabilitation phase, and beyond. The professional composition of acute stroke teams may vary internationally. In the Australian context of this study, allied health members include physiotherapists, occupational therapists, speech pathologists, social workers, dietitians, and psychologists.Citation2
Several researchers suggest that patient age is a determinant of the quality of medical and allied health care patients receive following acute stroke.Citation3–Citation5,Citation9–Citation13 We have previously reported that age and gender, on their own, are not related to an overall index of allied health care quality.Citation14 Further investigation is now required to determine whether patient age and gender are associated with individual measures of allied health care, and further, whether other variables, such as comorbidity, prestroke independence, and stroke severity, are putatively associated with allied health care. If there are differences in allied health care provided to patients with acute stroke, it is important to understand why care might differ, so that quality improvement strategies can be effectively targeted at problem areas.
This paper explores demographic and stroke-related factors (predictor variables), including patient age, which may be associated with individual measures of quality of care provided to acute stroke patients by allied health professionals. Our aim was to provide systematically determined information to guide clinical quality audits and targeted quality improvement strategies in stroke care.
Methods
Ethical considerations and our sampling framework have been reported in detail previously.Citation14 In summary, we conducted a retrospective clinical audit of medical records for 300 acute stroke patients from three metropolitan tertiary hospitals in Adelaide, South Australia, Australia. Sampled patients had been consecutively admitted to hospital prior to August 2009, and the audit was conducted between November 2009 and April 2010.
Quality of care
We previously reported on an overall index of 20 performance indicators of allied health service quality, identified from a literature review (listed in ).Citation14,Citation15 Although several of these indicators relate to interdisciplinary elements of stroke care which may be shared within a stroke team, the focus of this study is the ability of allied health professionals to contribute to this work, because this is largely unexplored. In our earlier study, quality of care was determined by per patient compliance with all 20 process indicators.Citation14 In the current study phase, compliance with each process indicator was considered individually and associations were explored with predictor variables. Allied health professionals of interest in our research were from physiotherapy, occupational therapy, speech pathology, dietetics, social work, and psychology.
Table 2 Eligibility for process indicator care, care adherence and association with age
Predictor variables
Previous clinical audits and literature reviews of stroke provided awareness of the demographic and clinical variables that could be extracted retrospectively from medical records.Citation13–Citation15 These variables are captured by stroke clinicians to assist diagnosis and clinical management, or for service monitoring.
Data were extracted from medical records on patient age, gender, premorbid levels of independence and accommodation type, English proficiency, comorbidity levels, weekend or weekday admission, stroke unit admission, initial stroke severity, length of stay in the acute hospital, and process indicator compliance. Many of these demographic and clinical variables have been associated with care quality in the stroke literature, especially for medical care,Citation14 or as predictors of stroke outcomes. However, none of these predictor variables have previously been well explored for their influence on stroke care by allied health professionals.
In addition to the evidence discussed above regarding age-related differences in care, researchers have reported associations between gender and stroke care quality.Citation16–Citation18 Stroke severity is strongly linked to survival and discharge destination outcomes,Citation19,Citation20 and a priori reasoning suggests that it may prompt allied health care processes, such as swallow assessment, in patients with obvious risks of poor outcome. Stroke severity may also influence the ease with which specific care, such as early rehabilitation, can be achieved. Admission over a weekend has previously been reported to influence care standards and patient outcomes following acute stroke.Citation12,Citation21 The scarcity of allied health staff at the research sites over weekends suggested that day of admission may alter care. Patient outcomes following stroke have been associated with previous levels of independence and accommodation,Citation22,Citation23 comorbidity levels,Citation24,Citation25 and length of stay in the acute hospital.Citation26,Citation27 These factors may influence allied health staff decisions regarding care, for example, the priority given to early rehabilitation interventions. Factors such as length of stay may also influence the achievability of some care processes for patients. We considered English proficiency in our study because it has previously been linked to stroke outcomes and the quality of health care patients receive.Citation28,Citation29
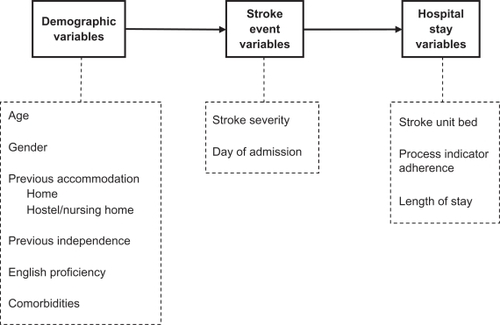
Development of a priori causal pathway
A simple causal pathway was constructed to assist in our understanding of how to undertake the analysis of the putative predictors of the allied health indicators of care. We constructed a flowchart of conditions and events (). This approach was based on the causal modeling theory of Rothman and Greenland.Citation30 We called this a simple causal pathway because we had no understanding at this point of the ongoing influence of early predictor variables on other variables which become important along the pathway.
Statistical analysis
We undertook a series of analyses to understand the relationships between the putative predictor variables and each care process indicator, using our causal pathway as an analysis model. Univariate logistic regression models were constructed between: adherence with individual process indicators and age; adherence with individual process indicators and non-age predictor variables; the association of age with other predictor variables; and the association between non-age variables.
Data were analyzed using SAS proprietary software (v 9.2; SAS Institute, Cary, NC). Correlations between variables were expressed as relative risks, odds ratios (OR, as appropriate), and 95% confidence intervals (CI). We report relative risks for the first two of the analyses because we were examining associations between independent care predictors with dependent variables (indicators of care quality derived from cross-sectional observational data). We reported OR for the third and fourth analyses because we were examining the association between independent variables.
Data management
As reported in our earlier paper, age was most appropriately dichotomized as younger (<75 years) and older (75+ years) patients.Citation14 Stroke severity on admission was determined by retrospectively extracting data from medical records to complete a National Institute of Health Stroke Scale (NIHSS) for each patient. The NIHSS is a widely used, valid, and reliable measure of stroke severity.Citation31,Citation32 It is also reliable and valid when data are extracted retrospectively from patient medical records.Citation33,Citation34 Based on previous stroke studies, NIHSS scores were divided into three groups for analysis, ie, mild strokes (NIHSS <8), moderate severity strokes (NIHSS 8–16), and severe strokes (NIHSS > 16).Citation35
Comorbidity levels were measured using the Charlson Comorbidity Index (CCI), which is a summary score of the existence or absence of 17 medical conditions, weighted to account for disease severity.Citation36 This index has been validated as a predictive comorbidity index for patients with stroke. It has been used in previous stroke outcome studies and has also been validity and reliability tested for retrospective data extraction.Citation37,Citation38 Comorbidity information was extracted from the medical records to complete a CCI for each patient. Based on analysis reported in previous studies, patient CCI scores were dichotomized as low comorbidity levels (CCI ≤ 1) vs high comorbidity levels (CCI > 1).Citation38
Patients admitted between 1600 hours on a Friday and 2400 hours on a Sunday, when access to allied health professionals was scarce, were recorded as weekend admissions. Admission directly from the emergency department to a stroke unit was recorded in binary terms (yes = 1, no = 0).
Nonaphasic patients were recorded as not proficient in English if there was evidence that assistance had been required with language translation, or if “limited English” or similar was found in the medical records.
Premorbid dependence level was recorded as independent or dependent, according to whether assistance was required with activities of daily living or instrumental activities of daily living.Citation39 Premorbid accommodation was recorded as a private home or a residential care facility (nursing home or hostel).
Length of stay was a measure of days spent in the acute hospital. Length of stay data (in days) was broadly classified for analysis. For univariate analysis, length of stay was dichotomized into shorter stay (<12 days) and longer stay (≥12 days). The cut point of 12 days was the mean length of stay for the data set and was also the average length of stay for acute stroke patients at the three data collection hospitals in 2007/08 and 2008/09.Citation40 To provide more detailed consideration of the possible influence of length of stay on care, analysis considered length of stay in three groups divided at the data tertiles (<4 days, 4–9 days, and ≥10 days).
Results
Description of participants
The characteristics of the 300 sampled patients are reported in . Mean age at stroke onset was 74.7 years (standard deviation [SD]: 13.5, range 18–100 years). The mean length of stay in acute care was 12.5 days (SD: 15.6, range 1–98 days). The sample was proportionally balanced for gender. Despite similar mean ages for males and females, a larger proportion of females were in the older age groups, with 72% females aged 75 years or older, compared with 53% of males. A greater proportion of females suffered a moderate or severe stroke (28%) than males (18%). For the whole sample, there were weak relationships between increasing age and increasing stroke severity (r2 = 0.21) and comorbidity levels (r2 = 0.20).
Table 1 Patients characteristics (n = 300)
Process indicator adherence
Compliance with each process indicator was generally poor (, columns 2 and 3). For 16 of the process indicators (80%), less than half of the appropriate patients received recommended care.
Analysis 1: process indicator adherence and age
The outcome of univariate logistic regression models, associating process indicator adherence with age, is reported as relative risks in , column 4. Only one process indicator had a significant association with age, where patients younger than 75 years were significantly more likely to receive first mobilization within 24 hours of stroke onset than older patients.
Analysis 2: process indicator adherence and other non-age predictor variables
Compliance with 12 of the 20 process indicators (60%) was significantly correlated with non-age variables. The only variables which were not associated with any process indicator compliance were previous accommodation type and English proficiency. For 30% of the process indicators, there was more than one non-age correlate ().
Table 3 Univariate model of independent variables (excluding age) and adherence to process indicators
Analysis 3: associations of age with other predictor variables
Significant correlations were found between patient age, and the predictor variables of stroke severity, comorbidity levels, premorbid accommodation, premorbid independence level, gender, English proficiency, and length of stay.
In summary, compared with younger patients, patients 75 years or older were significantly more likely to have a moderate-to-severe or severe stroke (OR: 1.8, 95% CI: 1.1–3.2 and OR: 2.9, 95% CI: 1.4–6.1, respectively), to have higher comorbidity levels (OR: 2.5, 95% CI: 1.5–4.2), to have lived in residential care (OR: 2.6, 95% CI: 1.1–6.2), or been previously dependent (OR: 6.2, 95% CI: 3.2–12). Older patients were also more likely to be female (OR: 2.2, 95% CI: 1.4–3.6), to have a length of stay of 5–9 days (OR: 0.6, 95% CI: 0.3–0.9), and to have poor English proficiency (OR: 3.2, 95% CI: 1.1–9.7). Detailed results are shown in .
Appendix 1 Correlations between age and other predictor variables
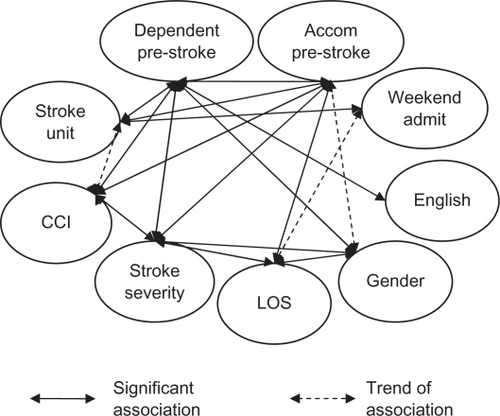
Analysis 4: associations between non-age variables
There were a number of significant associations between non-age predictor variables. Females were less likely than males to have been previously independent (OR: 2.2, 95% CI: 1.4–3.7), more likely to have a moderate or severe (NIHSS ≥ 8) stroke (OR: 0.4, 95% CI: 0.2–0.6), and a length of stay ≥ 10 days (OR: 0.4, 95% CI: 0.2–0.7). Patients who suffered a moderate-to-severe stroke (NIHSS ≥ 8) were more likely to have lived previously in residential care (OR: 0.3, 95% CI: 0.1–0.7), to have high comorbidity levels (OR: 0.6, 95% CI: 0.4–0.98), and to have a length of stay ≥ 10 days (OR: 2.6, 95% CI: 1.5–4.7). Compared with patients having low comorbidity, high comorbidity levels were associated with previous residential care (OR: 8.3, 95% CI: 2.0–35.6), and previous dependence (OR: 4.1, 95% CI: 2.1–8.0). Patients were less likely to be admitted to a stroke unit if they were previously dependent (OR: 5.5, 95% CI: 2.7–11.3) or living in residential care (OR: 8.5, 95% CI: 3.0–24.3). Patients with poor English proficiency were more likely to be dependent prior to their stroke (OR: 2.9, 95% CI: 1.3–6.9). Patients admitted on a weekend were less likely to have a short length of stay (<4 days) or long length of stay (≥10 days) compared with weekday admissions (OR: 0.4, 95% CI: 0.2–0.8 and OR: 0.6, 95% CI: 0.3–1.0, respectively). There was also a trend for less likelihood of stroke unit care if admitted on a weekend.
This analysis also demonstrated the potential redundancy in considering some non-age variables for their relevance to quality of allied health care. For example, an association between previous accommodation and previous independence was impossible to assess because all patients in residential care were, by default, also dependent. When this is considered in the light of earlier findings, previous independence may be the more important predictor variable because it is associated with process indicator compliance and has a stronger correlation than accommodation, with age.
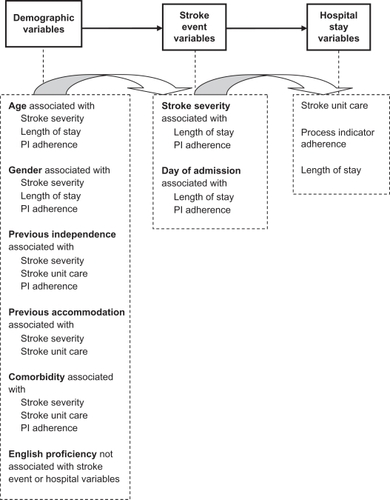
Further details are provided in . The complex confounding associations between the various non-age predictor variables are illustrated in .
Figure 2 Confounding relationships between non-age variables.
Appendix 2 Matrix of non-age variables
In we revisit our initial causal pathway, adding in the associations found between adherence to allied health process indicators, and the early predictor variables captured in patient demographic and stroke event data. This new pathway summarizes the journey for patients admitted with acute stroke and the multiple factors that can impact on the care they receive from allied health professionals.
Discussion
This paper provides new data regarding the possible predictors of allied health care quality for patients with acute stroke. The sample is robust because it is appropriately powered and derived from a consecutive sample of stroke patient records. Based on our findings, we suggest that the quality of acute stroke care contributed by allied health in multidisciplinary settings could be improved. This is the first known study to examine a range of individual processes of care by allied health professionals and the factors which may relate to compliance with these processes. The findings suggest a complex relationship between variables which may be related to the provision of best practice by allied health professionals caring for acute stroke patients.
We acknowledge that the generalizability of the findings for some variables chosen in our study may be limited by international variations in health care systems and policy. Length of stay data and admissions directly to a stroke unit, for example, are both particularly influenced by local contexts. Variability in the roles of stroke team members must also be taken into account when interpreting our results. For example, in the study settings, speech pathologists and dietitians made a strong contribution to team decisions regarding enteral feeding (process indicator 12), but this may not be an allied health role in some settings. Furthermore, we recognize that, as part of a multidisciplinary team with shared roles and responsibilities, the work of the allied health professions can be difficult to consider separately.
Correlates were found for older age, including increased stroke severity, higher comorbidity levels, previous residential care accommodation, previous dependence, female gender, poor English proficiency, and longer length of stay. These predictor variables were age proxies in our sample and may be stronger predictors of care decisions than patient age per se.
Some medical literature suggest that the age of an acute stroke patient is a determinant of the quality of medical care for stroke.Citation3–Citation5,Citation9–Citation12 In allied health care, we suggest that other factors may be at work. Patient age had a strong correlation with only one quality process indicator (early first mobilization), and this process indicator was even more strongly correlated with stroke severity. Non-age variables were more frequently correlated with process indicator compliance (twelve indicators) than was patient age. Stroke severity was the most frequent predictor variable (seven process indicators), with length of stay the second most common predictor (five process indicators). Both of these variables were also age proxies. This analysis also demonstrated the lack of importance of some non-age variables, such as previous residential care accommodation data made redundant by data on previous independence.
It is possible that systematic variations between professions may contribute to age-related differences in the medical care provided following stroke, which do not apply to allied health care. It is recognized, for example, that older patients are under-represented in some of the primary stroke research which guides evidence-based medical diagnostics and interventions.Citation3 Patients over 80 years have been excluded from many thrombolysis trials,Citation41 and similar age exclusions are reported for secondary prevention stroke medications.Citation42 The evidence base for allied health stroke care is still in early development and may therefore have less influence on which patients receive particular elements of care. As well as practicing within the biomedical framework adopted by medical practice, many areas of care provided by allied health professionals also fit within a biopsychosocial model.Citation43 These differences may result in different clinical reasoning processes and decision-making by the separate professions.
Allied health professional decision-making regarding the care delivered to patients with stroke has not been well explored. There may be complex influences on the decisions they make about the care they provide to patients with acute stroke, underpinned by their perspectives of the role of non-age predictor variables on patient outcome. Our causal pathway ( and ) suggests that many factors cannot be adjusted because they are a priori to the stroke. How allied health professionals account for these factors is yet to be established.
Conclusion
Ensuring the highest quality of allied health care for all stroke patients is important in the current climate of scarce resources and the increasing burden of stroke to the health sector. The associations identified between independent variables, including patient age, indicate that there are unlikely to be simple explanations for why some patients receive recommended care and others do not. To understand fully the important factors influencing the quality of care provided to acute stroke patients by allied health professionals will require further investigations into their perspectives on the capacity of stroke patients to improve, and how they make care decisions.
Acknowledgements
JAL undertook this research as part of a PhD candidature which was supported by an Australian Postgraduate Award government scholarship.
Disclosure
The authors report no conflicts of interest in this work.
References
- FedderWNational and international quality initiatives to improve stroke careNeurol Clin2008261191120719026908
- National Stroke FoundationClinical Guidelines for Stroke Management 2010 MelbourneAustraliaNational Stroke Foundation2010
- SanossianNOvbiageleBPrevention and management of stroke in very elderly patientsLancet Neurol200981031104119800847
- FairheadJFRothwellPMUnderinvestigation and under treatment of carotid disease in elderly patients with transient ischaemic attack and stroke: comparative population based studyBMJ200633352552716849366
- HeidrichJHeuschmannPUKolominsky-RabasPRuddAGWolfeCDEuropean BIOMED II Study of Stroke Care GroupVariations in the use of diagnostic procedures after acute stroke in Europe: Results from the BIOMED II study of stroke careEur J Neurol20071425526117355544
- SaposnikGBlackSHakimAFangJTuJVKapralMKAge disparities in stroke quality of care and delivery of health servicesStroke2009403328333519696418
- GallSLDonnanGDeweyHMSex differences in presentation, severity, and management of stroke in a population-based studyNeurology20107497598120181922
- ZorowitzRStroke rehabilitation quality indicators: raising the bar in the inpatient rehabilitation facilityTop Stroke Rehabil20101729430420826417
- BhallaAGrieveRTillingKRuddAGWolfeCDBIOMED II European Study of Stroke CareOlder stroke patients in Europe: stroke care and determinants of outcomeAge Ageing20043361862415501838
- McKevittCCoshallCTillingKWolfeCAre there inequalities in the provision of stroke care? Analysis of an inner-city stroke registerStroke20053631532015618440
- PalnumKDPetersenPSørensenHOlder patients with acute stroke in Denmark: quality of care and short-term mortality. A nationwide follow-up studyAge Ageing200837909517965039
- RuddAGHoffmanADownCPearsonMLoweDAccess to stroke care in England, Wales and Northern Ireland: the effect of age, gender and weekend admissionAge Ageing20073624725517360793
- LukerJAGrimmer-SomersKAFactors influencing acute stroke guideline compliance: a peek inside the ‘black box’ for allied health staffJ Eval Clin Pract20091538338919335501
- LukerJABernhardtJGrimmer-SomersKAAge and gender as predictors of allied health quality stroke careJ Multidiscip Healthc2011In press.
- LukerJAWallKBernhardtJEdwardsIGrimmer-SomersKAMeasuring the quality of dysphagia management following stroke: a systematic reviewInt J Stroke2010546647621050403
- Di CarloALamassaMBaldereschiMPracucciGBasileAMWolfeCDSex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicentre multinational hospital-based registryStroke2003341114111912690218
- SmithMALisabethLDBrownDLMorgensternLBGender comparisons of diagnostic evaluation for ischemic stroke patientsNeurology20056585585816186523
- GarganoJWWehnerSReevesMSex differences in acute stroke care in a statewide stroke registryStroke200839242918048851
- DeweyHSturmJDonnanGMacdonellRMcNeilJThriftAIncidence and outcome of subtypes of ischaemic stroke: initial results from the North East Melbourne Stroke Incidence Study (NEMESIS)Cerebrovasc Dis20031513313912499723
- FrankMConzelmannMEngelterSPrediction of discharge destination after neurological rehabilitation in stroke patientsEur Neurol20106322723320215754
- SaposnikGBaibergenovaABayerNHachinskiVWeekends: a dangerous time for having a stroke?Stroke2007381211121517347472
- AgarwalVMcRaeMPBhardwajATeasellRWA model to aid in the prediction of discharge location for stroke rehabilitation patientsArch Phys Med Rehabil2003841703170914639573
- ColantonioAKaslSOstfeldABerkmanLPrestroke physical function predicts stroke outcomes in the elderlyArch Phys Med Rehabil1996775625668831472
- BerlowitzDRHoenigHCowperDCDuncanPWVogelWBImpact of comorbidities on stroke rehabilitation outcomes: does the method matter?Arch Phys Med Rehabil2008891903190618929019
- BushnellCDLeeJDuncanPWNewbyLKGoldsteinLBImpact of comorbidities on ischemic stroke outcomes in womenStroke2008392138214018451349
- TanWSHengBHChuaKSChanKFFactors predicting inpatient rehabilitation length of stay of acute stroke patients in SingaporeArch Phys Med Rehabil2009901202120719577034
- SaxenaSKNgTPYongDFongNPGeraldKTotal direct cost, length of hospital stay, institutional discharges and their determinants from rehabilitation settings in stroke patientsActa Neurol Scand200611430731417022777
- John-BaptisteANaglieGTomlinsonGThe effect of English language proficiency on length of stay and in-hospital mortalityJ Gen Intern Med20041922122815009776
- ShiLLebrunLATsaiJThe influence of English proficiency on access to careEthn Health20091462564219953393
- RothmanKJGreenlandSCausation and causal inference in epidemiologyAm J Public Health200595Suppl 1S144S15016030331
- BrottTAdamsHOlingerCMeasurements of acute cerebral infarction: a clinical examination scaleStroke1989208648702749846
- GoldsteinLBBertelsCDavisJNInterrater reliability of the NIH Stroke ScaleArch Neurol1989496606622730378
- BairdADasheJComparison of retrospective and prospective measurement of the National Institutes of Health Stroke ScaleCerebrovasc Dis200010808110629353
- WilliamsLSYilmazEYLopez-YunezAMRetrospective assessment of initial stroke severity with the NIH Stroke ScaleStroke20003185886210753988
- BernhardtJDeweyHThriftACollierJDonnanGA very early rehabilitation trial for stroke (AVERT): phase II safety and feasibilityStroke20083939039618174489
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis1987403733833558716
- TessierAFinchLDaskalopoulouSSMayoNEValidation of the Charlson Comorbidity Index for predicting functional outcome of strokeArch Phys Med Rehabil2008891276128318586129
- GoldsteinLBSamsaGPMatcharDBHornerRDCharlson Index comorbidity adjustment for ischemic stroke outcome studiesStroke2004351941194515232123
- KatzSAssessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily livingJ Am Geriatr Soc1983317217276418786
- South Australian Department of HealthAcute Stroke Service Report 2010 for Metropolitan South AustraliaSouth Australian Government, AdelaideStatewide Stroke Clinical Network2010
- SchellingerPDJansenOFiebachJBMonitoring intravenous recombinant tissue plasminogen activator thrombolysis for acute ischemic stroke with diffusion and perfusion MRIStroke2000311318132810835451
- MusiniVMTejaniAMBassettKWrightJMPharmacotherapy for hypertension in the elderlyCochrane Database Syst Rev20094CD00002819821263
- Borrell-CarrioFSuchmanALEpsteinRMThe biopsychosocial model 25 years later: principles, practice and scientific enquiryAnn Fam Med2004257658215576544