Abstract
Nurse practitioners (NPs) have a unique opportunity as frontline caregivers and patient educators to recognize, assess, and effectively treat the widespread problem of uncontrolled asthma. This review provides a perspective on the role of the NP in implementing the revised National Asthma Education and Prevention Program (NAEPP) Guidelines put forth by the National Heart, Lung, and Blood Institute, thereby helping patients achieve and maintain asthma control. A literature search of PubMed was performed using the terms asthma, nurse practitioner, asthma control, burden, impact, morbidity, mortality, productivity, quality of life, uncontrolled asthma, NAEPP guidelines, assessment, pharmacotherapy, safety. Despite the increased morbidity and mortality and impaired quality of life attributable to uncontrolled asthma, the 2007 NAEPP asthma guidelines are greatly underused. NPs have an opportunity to identify patients at risk and provide enhanced care and education for asthma control. Often, NPs can prescribe medication for and manage these patients, but it is necessary to be able to discern which patients require referral to a specialist.
Introduction
Asthma is a global health problem, burdening patients, families, health care systems, and governments.Citation1 Despite the availability of several treatments and disease management guidelines, many patients have asthma that remains uncontrolled or not adequately controlled.Citation2,Citation3 In a study by Sullivan et al, few patients with severe or difficult-to-treat asthma achieved asthma control during a 2-year period: 83% of patients had uncontrolled asthma, 16% had asthma inconsistently controlled, and only 1.3% had controlled asthma during all assessment periods.Citation4
The review
This article is intended to increase nurse practitioners’ (NPs) awareness of the prevalence of uncontrolled asthma and provide key information and tools for assessing and maintaining asthma control.
Source materials
The 2007 National Asthma Education Prevention Plan (NAEPP) guideline recommendations for asthma assessment and management, including referral of patients with difficult-to-treat asthma to an asthma specialist, serve as the primary source material. In addition, selected references related to asthma epidemiology and pathophysiology were obtained from a literature search of PubMed using the terms: asthma, nurse practitioner, asthma control, burden, impact, morbidity, mortality, productivity, quality of life, uncontrolled asthma, NAEPP guidelines, assessment, pharmacotherapy, safety.
Benefits of controlled asthma
Uncontrolled asthma can lead to increased morbidity and mortality, impaired quality of life (QOL), and increased absenteeism from work and school.Citation5 Increased health care costs including both direct and indirect costs of asthma management are another consequence of uncontrolled asthma,Citation5 thus underscoring the need for improved symptom control among people with asthma.
Controlled asthma has been shown to reduce morbidity, improve QOL, increase productivity, and improve health outcomes.Citation4,Citation6 In addition, data from the 2006 US National Health and Wellness Survey showed that patients with controlled asthma reported decreased medical resource utilization (fewer emergency department visits, hospitalizations, and unscheduled clinic visits) compared with patients who had uncontrolled asthma.Citation6 The improved health outcomes associated with asthma control indicate that management with therapies that optimize asthma control may reduce direct and indirect costs of treatment.Citation4
2007 NAEPP asthma guidelines (EPR-3) for asthma control
In 2007, the NAEPP issued the third Expert Panel Report (EPR-3), a set of evidence-based clinical practice guidelines that incorporate best practices to help people with asthma control their disease, and provide guidance to clinicians in asthma management.Citation7 Major changes from the previous set of guidelines include a new focus on monitoring asthma control as the goal for asthma therapy and on distinguishing between classifying asthma severity (defined as the intensity of the disease process) and monitoring asthma control (defined as the degree to which therapeutic interventions minimize the manifestations of asthma or meet the goals of therapy).Citation7 These guidelines emphasize that the functions of assessment and monitoring are closely linked to the concepts of severity, control, and the patient’s responsiveness to treatment, and that both severity and control include the domains of current impairment and future risk.Citation7 Impairment is described as the frequency and intensity of symptoms or functional limitations the patient encounters, and risk is defined as the possibility of asthma exacerbations, progressive decline in lung function (or, for children, lung growth), or adverse effects related to asthma medications.Citation7 Including the domains of current impairment and future risk reflects the multifaceted nature of asthma, and the need to consider separately the impact of asthma QOL, functional capacity, and the risk of future adverse events (AEs).Citation7
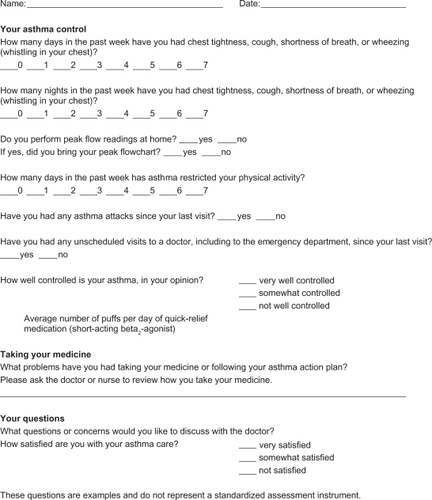
The EPR-3 provides specific guidance for periodic assessment and ongoing monitoring to determine whether the goals of asthma therapy are being achieved and asthma is being controlled.Citation7 shows the recommended methods for classifying asthma severity; shows the recommended methods for classifying asthma control. Asthma severity should be assessed to provide a basis for initial treatment; once treatment is initiated, the focus of clinical management becomes the assessment of asthma control to determine whether therapy should be maintained or adjusted. Periodic assessment of asthma control is recommended at 1- to 6-month intervals and should include measuring signs and symptoms of asthma, pulmonary function, history of asthma exacerbations, and aspects of pharmacotherapy.Citation7 The level of asthma control is the degree to which both domains of the manifestations of asthma – impairment and risk – are minimized by therapeutic intervention.Citation7 The current guidelines classify levels of asthma control using the following categories: well controlled, not well controlled, or very poorly controlled.Citation7
Figure 1 Methods of classifying asthma severity and initiating treatment in patients 12 years of age and older.
Abbreviations: EIB, exercise-induced bronchospasm; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICU, intensive care unit.
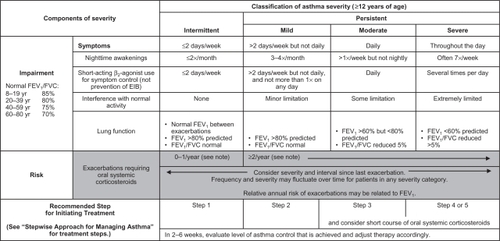
Figure 2 Methods of classifying asthma control and adjusting treatment in patients 12 years of age and older.
Abbreviations: FEV1, forced expiratory volume in 1 second; EIB, exercise-induced bronchospasm; N/A, not applicable; ATAQ, Asthma Therapy Assessment Questionnaire; ACQ, Asthma Control Questionnaire; ACT, Asthma Control Test.
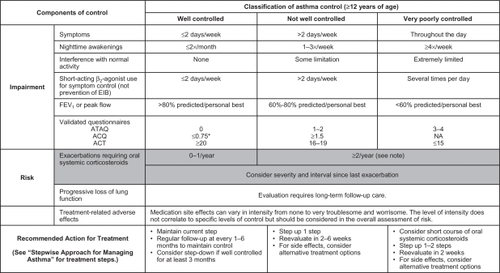
To achieve and maintain control of asthma, the guidelines recommend a stepwise approach that utilizes 6 steps.Citation7 This approach is outlined in .
Figure 3 Stepwise approach for managing asthma in patients aged ≥12 years.
Abbreviations: ICS, inhaled corticosteroid; LABA, long-acting inhaled beta2-agonist; LTRA, leukotriene receptor antagonist; SABA, inhaled short-acting beta2-agonist.
The importance of adhering to guidelines in order to meet and maintain goals of asthma control was demonstrated in a large, randomized, double-blind, intervention trial in which significant reductions in the rate of severe exacerbations and improvements in QOL resulted when asthma control as defined by the Global Initiative for Asthma/National Institutes of Health (NIH) was achieved.Citation8
Results from an intervention-based asthma assessment and management program suggested that implementing asthma guidelines at the point of care may lead to improved asthma control.Citation9 Nevertheless, there are known gaps between the development and distribution of guidelines and their implementation; in fact, it often takes many years for guidelines to be incorporated into clinical practice.Citation10 The NAEPP treatment guidelines have had limited effects on physician behavior, thus contributing to their underutilization in practice.Citation11 Possible barriers to guideline use include patient- and environmental-related factors such as patient resistance to guidelines or the need for additional office and counseling resources. In addition, if guidelines are inconvenient, cumbersome, or confusing, they may not be incorporated into clinical practice.Citation12–Citation15
The advantages of NPs as educators and primary providers
NPs have a unique opportunity to identify patients at risk, and provide enhanced care and education for asthma control, because they are at the front line of patient care.Citation16 Both prospective and “real-world” observational studies have shown that NPs are key primary providers and educators in the management of chronic diseases, including asthma, acting as partners with physicians in providing complementary, collaborative, chronic disease management associated with favorable patient outcomes.Citation17,Citation18 A cross-sectional survey showed that nearly 50% of patients preferred NPs to general practitioners (or had no preference) for educational aspects of care, and were more satisfied with the NP for those aspects of care related to support of patients and their families.Citation19 Conversely, patients preferred medical aspects of care to be managed by the physician.Citation19 A qualitative interview study showed that the input of specialist nurses helped practice nurses to identify, follow-up, and audit the care of high-risk asthma patients.Citation20 In the inpatient setting, pediatric NPs have been shown to be effective care managers and educators.Citation21 These findings underscore the beneficial skill mix provided when NPs and physicians work together for their patients, showing that this approach may meet the needs of patients more effectively than care from the physician alone.
A sound partnership between the NP and patient is critical for consistent asthma control.Citation7 The NP can develop an active partnership with the patient by establishing open communication; identifying and addressing patient and family concerns about asthma and asthma treatment; developing treatment goals; selecting medications collaboratively with the physician, patient, and family; and encouraging self-monitoring and treatment.Citation7 Self-management education, in particular, has been shown to improve outcomes (eg, reduced the number of emergency department visits, hospitalizations, limitations on activities, improved health status, QOL, and perceived control of asthma).Citation7 A hospital-based study showed that asthma consultations with specialist asthma nurses improved patient self-management behavior and thereby reduced symptoms, improved lung function, and decreased work days lost.Citation22
Assessment of asthma control
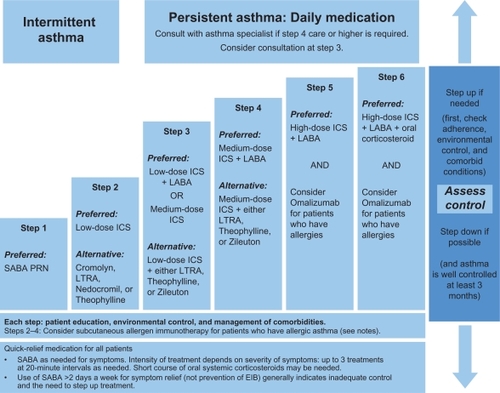
A key role of the NP is evaluating the patient’s asthma control. This ongoing process involves both clinical and patient self-assessment (see for a sample patient’s assessment sheet). The primary methods for clinical monitoring and control of asthma in clinical practice are assessment of symptoms; use of short-acting β2-agonists for quick relief of symptoms; and limitations on normal activities due to asthma, pulmonary function, and exacerbations.Citation7 In addition, the EPR-3 recommends that patients be encouraged to use self-assessment tools.Citation7 Obtaining the perspective of the patient and/or the patient’s family on whether the patient’s asthma is well controlled can add to the clinical evaluation. The “rule of 2s”, which classifies asthma control based on frequency of asthma symptoms, nighttime awakenings, and use of short-acting beta2 agonists (SABAs) for symptom control, is a helpful interpretation of the patient’s input. These and other components of asthma control are described in .Citation7
Table 1 Classification of well-controlled asthma
Assessing asthma control can help the NP evaluate both current health status and identify patients at risk for future health impairment.Citation23 Some of the validated instruments available for assessing asthma control include the Asthma Control Questionnaire (ACQ), the Asthma Therapy Assessment Questionnaire (ATAQ), and the Asthma Control Test (ACT) ().Citation7 An official statement by the American Thoracic Society/European Respiratory Society acknowledged that these tools are easy to administer and interpret but do not provide full information on a patient’s current clinical state and should only be used as a part of a full assessment.Citation24
Table 2 Validated instruments for assessing asthma controlCitation25–Citation27,Citation29
ACQ
The ACQ is a questionnaire developed to meet the criteria set forth by international guidelines (ie, those issued by the Global Initiative for Asthma and the British Thoracic Society) for optimizing asthma control.Citation25 This tool measures the adequacy of and change in asthma control (spontaneous or as a result of treatment).Citation26 Consisting of 7 equally weighted items, the ACQ scores the patient-reported frequency of nighttime awakenings, symptoms on waking, activity limitation, shortness of breath, wheeze, rescue SABA use during the prior week, and clinic-evaluation forced expiratory volume in 1 second % predicted prebronchodilator.Citation25 The total ACQ score is the mean of the 7 items, which ranges from 0 (totally controlled) to 6 (severely uncontrolled).Citation25
ATAQ
The ATAQ is a self-administered questionnaire that assesses asthma control with questions about self-perceived asthma symptom control; missed work, school, or daily activities; nighttime awakenings due to symptoms; and use of quick-relief inhaler medication.Citation27 The number of control problems is summed from all questions for a total score in which 0 = no control issues present and 4 = all 4 control issues present.Citation27 This index provides a simple way to identify patients potentially at risk of poor asthma control, and can detect specific problem areas (eg, overuse of reliever medications, nocturnal wakening, and interference with activities) that can serve as a basis for discussion with the patient.Citation28
ACT
The ACT is a 5-item questionnaire, administered in the doctor’s office, which evaluates patient-reported shortness of breath, asthma control, use of rescue medication, productivity at work or school, and nighttime awakenings due to asthma symptoms.Citation29 Although ACT could be used for many different applications (eg, an investigator selecting patients for clinical trials or a clinician involved in a disease management program), it does not provide a particular score level as a cut point; rather, the designers of this instrument encourage health care providers to select the most appropriate cut point for their patient’s situation.Citation29 The combination of the ACT and lung function testing has been shown to be a more useful strategy for predicting future exacerbation of asthma compared with either method used alone.Citation30
The asthma action plan
An asthma action plan – a written, individualized set of instructions for daily management (including actions to manage worsening asthma and signs and symptoms that indicate the need for immediate medical care) – is a tool NPs can use to help optimize a patient’s asthma control. The NAEPP recommends that all asthma patients be provided with such a plan.Citation7 The use of an action plan as part of the patient’s asthma self-management has been shown to reduce the number of missed school and work days, unscheduled clinic visits, ED visits, and hospitalizations.Citation31 With the use of an asthma action plan, patients are empowered to prevent their symptoms from getting worse, monitor symptoms or peak expiratory flows to guide an appropriate response, and take their prescribed controller and rescue medications. It is important to note that studies have shown that reviewing a patient’s asthma action plan at every visit can increase the patient’s medication adherence.Citation32 Patients should bring their asthma action plans to every scheduled and unscheduled asthma-related visit. This will enhance continuity of care.
Five effective elements of asthma action plans include: (1) recommended doses and schedule of daily medications and how to adjust them in response to particular symptoms or peak flow measurements; (2) a record of the patient’s “best” peak flow measurement, as well as ranges of impairment, which can help patients recognize when control is being compromised; (3) warning signs and symptoms that indicate the need for closer monitoring or acute care; (4) emergency telephone numbers for the health care provider, ED, rapid transportation, and family or friends; and (5) list of triggers that may cause an asthma attack to inform the patient and others of triggers to avoid.
Anticipating and answering patients’ questions
As part of overall asthma management, NPs are well prepared to provide the education necessary to improve symptom control.Citation16 The role of education extends to anticipating and answering patients’ questions about their degree of asthma control. The patient may want and need to address issues that can be resolved with information or a change in therapy. If the patient asks why his or her asthma is not controlled, the NP should explore possible reasons and ensure that patients know their asthma triggers and avoid environmental exposures that worsen their asthma, such as allergens, irritants, and tobacco smoke.Citation7 It is equally important to ensure that the patient is taking medication as prescribed. This includes the correct use of devices such as inhalers, spacers, and nebulizers, which should be demonstrated to the patient by the NP and then demonstrated by the patient to the NP.Citation7 The patient should not be blamed if he or she is not taking medication as prescribed; rather, he or she should be made aware that many patients with asthma and other chronic diseases are nonadherent to therapy but that adherence is extremely important for successful outcomes.Citation33,Citation34
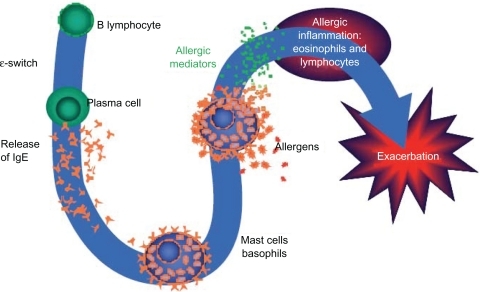
Patients who are practicing trigger avoidance and are taking their medications as prescribed, yet still have uncontrolled asthma, may require a change in treatment. For example, patients with allergic asthma, who comprise more than half of individuals with asthma, may need a medication that addresses the allergic component of the disease.Citation35 If this is the case, these patients should be educated about the nature of their allergic triggers () and informed about avoidance measures and medications available for treatment.
Figure 5 Overview of the allergic cascade. IgE (immunoglobulin E) is produced by the plasma cells, which are derived from B lymphocytes. The IgE moves through the extracellular fluid and vasculature until it binds to a high-affinity receptor, primarily found on mast cells and basophils. Cross-linking of the membrane IgE results in degranulation of the cell with mediator release and the resultant symptoms of asthma.
Ledford DK. Expert Opin Biol Ther. 2009;9:933–943. Copyright © 2009. Informa Healthcare. Reproduced with permission of Informa Healthcare.Citation49
Pharmacotherapy
Classes of asthma medications
NPs have many medication options available when treating their asthma patients. Medications for asthma consist of agents for long-term control and quick-relief rescue.Citation7 provides an overview of these medications and their mechanisms of action. Long-term control agents are used daily to achieve and maintain asthma control. The most effective agents in this class counteract the inflammation that underlies asthma.Citation7 This class includes inhaled corticosteroids (ICSs), the cornerstone of treatment for persistent asthma.Citation7,Citation36 In contrast, quick-relief medications (the preferred among which are SABAs) treat acute symptoms, and help prevent exercise-induced bronchoconstriction, and exacerbations.Citation7 The anticholinergic agent ipratropium bromide and oral systemic corticosteroids are used in addition to SABAs for the rescue treatment of moderate to severe exacerbations.Citation7 Unlike SABAs, long-acting β2-agonists (LABAs) have a duration of bronchodilatory action of at least 12 hours and are used as controller agents in combination with ICSs (see safety discussion below).Citation7,Citation32,Citation37,Citation38
Table 3 Classes of asthma medicationsCitation7,Citation36–Citation38,Citation40
Leukotrienes are the key proinflammatory mediators in asthma and the most powerful bronchoconstrictors found in humans to date.Citation39 Leukotriene modifiers consist of 5-lipoxygenase inhibitors (zileuton), which block cysteinyl leukotriene production, and leukotriene receptor antagonists (montelukast and zafirlukast), which block cysteinyl leukotrienes from binding to their primary receptor.Citation7,Citation40 Leukotriene receptor antagonist agents are alternative but not preferred therapy for the treatment of mild persistent asthma.Citation7
The immunomodulator class currently consists solely of omalizumab, a monoclonal antibody that inhibits binding of immunoglobulin E (IgE) to its receptor on the surface of mast cells and basophils, thereby decreasing mediators of asthmatic inflammation and the allergic response.Citation7,Citation36 Omalizumab is indicated for adolescents and adults with moderate to severe persistent asthma inadequately controlled with ICS who have documented reactivity to a perennial aeroallergen.Citation41 Omalizumab significantly reduced exacerbations in 2 randomized, double-blind, placebo-controlled, multicenter trials, each consisting of a 16-week stable steroid phase and a 12-week steroid reduction phase.Citation42,Citation43 Fewer patients with asthma exacerbations were observed with omalizumab versus placebo in the stable steroid phase of these 2 trials (14.6% vs 23.3% and 12.8% vs 30.5%, respectively) as well as the steroid-reduction phase (21.3% vs 32.3% and 15.7% vs 29.8%, respectively).Citation42,Citation43 In a separate study by Holgate et al,Citation44 exacerbation rates in patients treated with omalizumab were 35%–45% lower than the rates observed in the patients treated with placebo, although these differences did not reach statistical significance.Citation44
Safety concerns
Inhaled corticosteroids
The NAEPP guidelines state that ICSs are generally well tolerated and safe when used at the recommended doses.Citation7 However, long-term use (>1 year) of high doses of ICSs, particularly if given in combination with frequent courses of oral corticosteroids, may be associated with the risk of cataracts or reduced bone mineral density.Citation7
Long-acting β2-agonists
Clinical trial evidence of an increased risk of asthma-related deaths in patients treated with salmeterol, and an increased risk of severe asthma exacerbations leading to hospitalizations and deaths, led to the Food and Drug Administration (FDA) determination in February 2010 that a black box warning was warranted on the labeling for all LABAs used in asthma.Citation32,Citation45 The FDA also recommended that these agents be used only for patients whose asthma is inadequately controlled with a long-term asthma control medication such as an ICS, or whose disease severity clearly warrants initiation of treatment with both an ICS and LABA, and that LABAs should be discontinued (but ICSs continued) once asthma control is achieved.Citation7,Citation45 This safety communication also added a contraindication for LABA use without concomitant treatment with an asthma controller medication such as an ICS.Citation45
Omalizumab
An analysis of data from controlled studies with omalizumab showed that the incidence of anaphylaxis (reported by investigator) was rare (omalizumab 0.14%, control 0.07%).Citation46 A separate analysis of the postmarketing safety database, including an estimated exposure of 57,300 patients from June 2003 to December 2006, indicated 124 cases of anaphylaxis attributable to omalizumab (0.2%).Citation47 The labeling for omalizumab includes a warning concerning this risk of anaphylaxis, and recommends that patients be observed closely after drug administration.Citation41 The warning also stipulates that health care providers administering omalizumab be prepared to manage anaphylaxis, and inform patients of the signs and symptoms of the condition so that they can seek immediate medical care should symptoms occur.Citation41
Malignant neoplasms were observed in 0.5% of omalizumab-treated patients compared with 0.2% of control patients in clinical studies of adults and adolescents (aged ≥ 12 years) with asthma and other allergic disorders.Citation46 The majority of malignant neoplasms were reported during the first 52 weeks of treatment and the impact of longer exposure to omalizumab is not known.Citation46 Based on comparisons with the NIH Surveillance, Epidemiology and End Results (SEER) database, the incidence of malignancy in the omalizumab group was found to be similar to the incidence expected in the general population.Citation46 In a separate analysis, an expert panel of oncologists concluded that the increased occurrence of malignancies observed in clinical trials was not due to omalizumab and that the malignancies occurred before the study began.Citation48 Furthermore, of the 25 reported neoplasms, 22 were found to be unrelated to the study drug and 3 were believed to have a remote relation to it.Citation48
The patient with difficult-to-treat asthma: when to refer to a specialist
Some patients with asthma are beyond the scope of general practice. The NAEPP guidelines recommend referral to a specialist if the patient meets any of the following criteria: asthma is difficult to control or is persistent, the patient has needed more than 2 oral corticosteroid bursts per year, exacerbations have required hospitalization, therapy at step 4 or higher is required to achieve adequate asthma control, immunotherapy or therapy with omalizumab is being considered, or additional testing is needed.Citation7 summarizes these criteria.
Table 4 Criteria for referring a patient with difficult-to-treat asthma to a specialist
Conclusion
Many patients live with uncontrolled asthma, despite the availability of effective treatment options. NPs have a unique opportunity as frontline caregivers and patient educators to recognize and assess uncontrolled asthma as well as determine the steps necessary to help patients gain and maintain symptom control. With the implementation of the NAEPP guidelines, the role of NPs in asthma care will become particularly critical. NPs are ideally suited to the roles of primary purveyors of asthma education, promoters of patient partnerships for health care optimization, and providers of ongoing monitoring to ensure consistent achievement of therapeutic goals for asthma control.Citation16
Acknowledgements
The author would like to thank Kristin Carlin, RPh, MBA, and Embryon, Inc for writing and editorial assistance.
Funding
This article was funded by Genentech, Inc, South San Francisco, CA, and Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Disclosure
Dr Rance is a speaker for Merck and Co, Inc.
References
- MasoliMFabianDHoltSThe global burden of asthma: executive summary of the GINA Dissemination Committee reportAllergy20045946947815080825
- PetersSPJonesCAHaselkornTReal-world Evaluation of Asthma Control and Treatment (REACT): findings from a national Web-based surveyJ Allergy Clin Immunol20071191454146117481716
- ChapmanKRBouletLPReaRMSuboptimal asthma control: prevalence, detection and consequences in general practiceEur Respir J20083132032517959642
- SullivanSDRasouliyanLRussoPAExtent, patterns, and burden of uncontrolled disease in severe or difficult-to-treat asthmaAllergy20076212613317298420
- American Lung AssociationAmerican Lung Association Epidemiology and Statistics Unit Research and Program ServicesTrends in asthma morbidity and mortality2008140
- WilliamsSAWagnerSKannanHThe association between asthma control and health care utilization, work productivity loss and health-related quality of lifeJ Occup Environ Med20095178078519528828
- National Heart Lung and Blood InstituteExpert Panel Report 3: guidelines for the Diagnosis and Management of Asthma Summary Report 20072007174
- BatemanEDBousheyHABousquetJCan guideline-defined asthma control be achieved? The Gaining Optimal Asthma Control studyAm J Respir Crit Care Med200417083684415256389
- CarltonBGLucasDOEllisEFThe status of asthma control and asthma prescribing practices in the United States: results of a large prospective asthma control survey of primary care practicesJ Asthma20054252953516169784
- LomasJAndersonGMDomnick-PierreKDo practice guidelines guide practice? The effect of a consensus statement on the practice of physiciansN Engl J Med1989321130613112677732
- RastogiDShettyANeugebauerRNational Heart, Lung, and Blood Institute guidelines and asthma management practices among inner-city pediatric primary care providersChest200612961962316537859
- CabanaMDRandCSPoweNRWhy don’t physicians follow clinical practice guidelines? A framework for improvementJAMA19992821458146510535437
- NavaratnamPJayawantSSPedersenCAPhysician adherence to the national asthma prescribing guidelines: evidence from national out-patient survey data in the United StatesAnn Allergy Asthma Immunol200810021622118426140
- WoolfSHPractice guidelines: a new reality in medicine. III. Impact on patient careArch Int Med1993153264626558250661
- CabanaMDEbelBECooper-PatrickLBarriers pediatricians face when using asthma practice guidelinesArch Pediatr Adolesc Med200015468569310891020
- HaydenMLRachelefskyGPartners for better athma control. Newest guidelines highlight value of NP careAdv Nurse Pract20081645485052545619999033
- MundingerMOKaneRLLenzERPrimary care outcomes in patients treated by nurse practitioners or physicians: a randomized trialJAMA2000283596810632281
- LitakerDMionLPlanavskyLPhysician – nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients’ perception of careJ Interprof Care20031722323712850874
- LaurantMGHermensRPBraspenningJCAn overview of patients’ preference for, and satisfaction with, care provided by general practitioners and nurse practitionersJ Clin Nurs2008172690269818647199
- FosterGGantleyMFederGHow do clinical nurse specialists influence primary care management of asthma? A qualitative studyPrim Care Respir J20051415416016701715
- BorgmeyerAGyrPMJamersonPAEvaluation of the role of the pediatric nurse practitioner in an inpatient asthma programJ Pediatr Health Care20082227328118761228
- LevyMLRobbMAllenJA randomized controlled evaluation of specialist nurse education following accident and emergency department attendance for acute asthmaRespir Med20009490090811001084
- ChenHGouldMKBlancPDAsthma control, severity, and quality of life: quantifying the effect of uncontrolled diseaseJ Allergy Clin Immunol200712039640217561244
- ReddelHKTaylorDRBatemanEDAn official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practiceAm J Respir Crit Care Med2009180599919535666
- JuniperEFBousquetJAbetzLIdentifying ‘well-controlled’ and ‘not well-controlled’ asthma using the Asthma Control QuestionnaireRespir Med200610061662116226443
- JuniperEFO’ByrnePMGuyattGHDevelopment and validation of a questionnaire to measure asthma controlEur Respir J19991490290710573240
- VollmerWMMarksonLEO’ConnorEAssociation of asthma control with health care utilization and quality of lifeAm J Respir Crit Care Med19991601647165210556135
- VollmerWMAssessment of asthma control and severityAnn Allergy Asthma Immunol20049340941315562878
- NathanRASorknessCAKosinskiMDevelopment of the asthma control test: a survey for assessing asthma controlJ Allergy Clin Immunol2004113596514713908
- SatoRTomitaKSanoHThe strategy for predicting future exacerbation of asthma using a combination of the Asthma Control Test and lung function testJ Asthma20094667768219728204
- GibsonPGPowellHCoughlanJSelf-management education and regular practitioner review for adults with asthmaCochrane Database Syst Rev2003CD00111712535399
- National Heart Lung and Blood InstituteExpert Panel Report 3: guidelines for the Diagnosis and Management of Asthma Full Report 200714408282007
- DekkerFWDielemanFEKapteinAACompliance with pulmonary medication in general practiceEur Respir J199368868908339810
- De SmetBDEricksonSRKirkingDMSelf-reported adherence in patients with asthmaAnn Pharmacother20064041442016507619
- ArbesSJJrGergenPJVaughnBAsthma cases attributable to atopy: results from the Third National Health and Nutrition Examination SurveyJ Allergy Clin Immunol20071201139114517889931
- HananiaNATargeting airway inflammation in asthma: current and future therapiesChest200813398999818398119
- CreticosPSManaging asthma in adultsAm J Manag Care20006S940S96311184565
- DonohueJFTherapeutic responses in asthma and COPD. BronchodilatorsChest2004126125S137S15302773
- SinghRKGuptaSDastidarSCysteinyl leukotrienes and their receptors: molecular and functional characteristicsPharmacology20108533634920516735
- TantisiraKGLimaJSylviaJ5-lipoxygenase pharmacogenetics in asthma: overlap with Cys-leukotriene receptor antagonist lociPharmacogenet Genomics20091924424719214143
- US Food and Drug AdministrationDrugs@FDA: FDA approved drug productswww fda gov82010 http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction_Search.Label_ApprovalHistory. Accessed June 26, 2011.
- BusseWCorrenJLanierBQOmalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthmaJ Allergy Clin Immunol200110818419011496232
- SolerMMatzJTownleyRThe anti-IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmaticsEur Respir J20011825426111529281
- HolgateSTChuchalinAGHebertJEfficacy and safety of a recombinant anti-immunoglobulin E antibody (omalizumab) in severe allergic asthmaClin Exp Allergy20043463263815080818
- US Food and Drug AdministrationFDA Drug Safety Communication: new safety requirements for long-acting inhaled asthma medications called Long-Acting Beta-Agonists (LABAs)2182010
- CorrenJCasaleTBLanierBSafety and tolerability of omalizumabClin Exp Allergy20093978879719302249
- LimbSLStarkePRLeeCEDelayed onset and protracted progression of anaphylaxis after omalizumab administration in patients with asthmaJ Allergy Clin Immunol20071201378138117936893
- KuhnRImmunoglobulin E blockade in the treatment of asthmaPharmacotherapy2007271412142417896896
- LedfordDKOmalizumab: overview of pharmacology and efficacy in asthmaExpert Opin Biol Ther2009993394319527111