Abstract
Background:
The use of evidence-based practice (EBP) is often not reflected in allied health (AH) practitioners’ day-to-day practice (the research-practice gap). Research suggests that considerable differences between and within AH disciplines exist, which require different approaches in order to influence practice behavior. It is therefore important to develop a better understanding of what influences individual AH practitioners’ adoption of evidence into daily practice.
Objective:
This systematic review aims to examine the individual characteristics of AH practitioners which determine their uptake of evidence into practice.
Methods:
Studies which examined individual factors or variables that influence research evidence use by any AH practitioner were included in the review. The methodological quality of the included papers was assessed using the Quality Assessment and Validity Tool for Cross-sectional Studies. A narrative summary of the findings was presented.
Results:
Six studies were included and the methodological quality scores indicated that two were weak and the remainder had moderate–weak quality. The review demonstrated that factors such as educational degree or academic qualification, involvement in research or EBP-related activities, and practitioners’ perceptions, attitudes and beliefs about research and EBP are significant predictors of self-reported research evidence use in AH. The effect of other factors such as professional characteristics, clinical setting/work environment, information-seeking behavior and sociodemographic variables are less clear. Whether there is an interaction effect between evidence-uptake factors has not been tested.
Conclusion:
Improving the research knowledge of clinicians and overcoming negative attitudes toward EBP have the potential to move AH practitioners towards regularly utilizing evidence in practice. Allied health practitioners may benefit from participation in regular educational opportunities such as case studies or journal clubs which can put them at the same level of thinking and awareness of research evidence. Future research should aim to review organizational and contextual factors and explore their interaction with individual determinants of research evidence use.
Introduction
Evidence-based practice (EBP) involves the integration of three key components: knowledge arising from one’s clinical expertise/clinical reasoning, patient’s preferences and research evidence.Citation1 Allied health (AH) practitioners are increasingly expected to use EBP as a basis for making clinical decisions.Citation2 There is little information on what prompts practitioners to make evidence-based decisions for clinical practice, or the ways in which they subsequently implement these decisions. Thus, because of the importance of ensuring that health care is evidence-based, this is an area of increasing research endeavor.
The literature suggests that AH practitioners in general have positive attitudes toward EBP, and believe their practice should be evidence-based.Citation3–Citation6 However, despite their recognition of its importance and value, their use of EBP is often not reflected in an individual AH practitioner’s day-to-day practice.Citation4,Citation7,Citation8 This is called the research-practice gap. For many AH practitioners, regularly utilizing evidence in practice may be an ongoing challenge. For example, in a survey conducted on 1755 rehabilitation practitioners in Canada (ie, physiotherapists, occupational therapists, speech pathologists), their use of family-related interventions for post-stroke clients was low, despite evidence of its effectiveness on stroke outcomes.Citation9 Thus, unless treatment is based on current evidence, patients may be receiving suboptimal or even ineffective treatment.
The literature outlines differences between and within AH disciplines in terms of practitioners’ knowledge and skills relevant to EBP.Citation2,Citation10 Their learning needs appear to vary according to their disciplines and prior research experience.Citation3,Citation11 There are also considerable differences in terms of practitioners’ access to evidence resources and the support they receive from their professional association, and their employer/training institution.Citation3,Citation10 This highlights that there is no “one-size-fits-all” strategy to promote research evidence uptake into practice that is likely to be effective for all AH practitioners or for all organizations in which AH practitioners work. Thus it appears to be important to recognize differences within and between AH practitioners and disciplines, which may require different approaches in order to influence evidence-into-practice behaviors.
Applying research findings to clinical decisions is not a simple process and is often difficult to achieve. There are two elements related to the successful implementation and uptake of evidence in AH: the practical component and the knowledge component.Citation3,Citation4,Citation6 The practical component refers to the time and resources to search for, access, analyze, and interpret the evidence as well as the organizational support to implement evidence into practice. The knowledge component, on the other hand, relates to health practitioners’ understanding of research concepts (eg, designs, methods, analysis, interpretation) which will allow them to become proficient readers of research. To bridge the gap between research and practice, these practical and knowledge barriers need to be understood and addressed.
There is scant research evidence from intervention studies which evaluate the effectiveness of strategies which aim to promote EBP uptake by AH practitioners. Those studies which are available demonstrate either modest or no effects.Citation7,Citation12,Citation13 One of many reasons for this could be the failure to systematically account for factors that influence individual AH practitioner’s use of research evidence in day-to-day practices. It is therefore necessary to develop a better understanding of what factors influence individual AH practitioners’ adoption of evidence into daily practice, so that these can be addressed by targeted training.
The aim of this review is to examine literature which describes individual characteristics of AH practitioners which could influence their uptake of research evidence. For the purpose of this review, AH practitioners include physiotherapists, occupational therapists, speech pathologists, dieticians, social workers, psychologists, podiatrists, ambulance paramedics, music therapists, art therapists, exercise physiologists, and intensive care paramedics.Citation14 An understanding of individual determinants of research evidence use is necessary to design targeted interventions to address the research-practice gap.
Methods
Studies that examined the influence of individual factors on the uptake of research evidence by any AH practitioner were considered. Uptake of research evidence refers to any of the following:
the extent to which the key steps involved in EBP (formulating a clinical question, searching for the most appropriate evidence to address the question, critically appraising the retrieved evidence, incorporating the evidence into a strategy for action, and evaluating the effects of any decisions and action taken) are integrated into day-to-day practice
research- or information-seeking behavior
use of research-based information
The review was limited to correlational studies because this type of research examines the relationships between variables. Only articles published in the English language were included, with no restriction on publication date. Studies were included if they measured both an independent (ie, one or more potential individual determinants of AH practitioner’s uptake of research evidence) and a dependent variable (ie, any measure of research evidence use), evaluated the influence of the independent variable on the dependent variable, and reported this relationship in terms of strength of association.Citation15
Search strategy
Relevant articles were identified using a wide range of keywords grouped into three categories. Concept one represented keywords in the category of “allied health”, concept two represented “evidence-based practice”, and concept three represented keywords in the category of “determinants.” These three concepts were combined in the electronic search in order to capture the most number of relevant articles.
Concept one: “allied health” or “allied health practitioner” or “allied health personnel” or physiotherap* or “physical therap*” or “occupational therap*” or “speech therap*” or “speech patholog*” or diet* or nutrition* or “social work*” or psycholog* or podiatr* or “ambulance paramedic” or “music therap*” or “art therap*” or “exercise physiolog*” or “ambulance officer” or “intensive care paramedic”.
Concept two: “getting knowledge into practice” or “getting research into practice” or “translating research into practice” or “evidence implementation” or “knowledge exchange” or “knowledge transfer” or “knowledge use” or “diffusion of innovation” or “evidence-based practice” or “research utilization” or “research use” or “research transfer” or “research uptake” or “research translation” or “knowledge translation” or “evidence translation” or “evidence uptake”.
Concept three: predict* or determinant or “individual characteristic”.
The following electronic databases were searched:
Academic search premier
Biomed Central Gateway
CINAHL
Cochrane Library
Current Contents Connect
ERIC
EMBASE
PsycARTICLES
Psych Info
TRIP Database
Web of Science
HighWire Press
Informit e-library
Journal citation reports
Meditext
MEDLINE
PubMed
PubMed central
Science citation index expanded
Science Direct
Scopus
The reference lists of retrieved papers were scrutinized for additional studies that were not indexed in any of the electronic databases.
Selection of studies for inclusion
The titles and abstracts of articles identified from the search strategy were independently reviewed by two reviewers (LL and SK) to determine eligibility for inclusion. Full texts of potentially relevant papers were retrieved for a more detailed examination. The decision to include or exclude studies, based on the set criteria, was made independently by the same authors. Disagreements regarding adherence to inclusion criteria were resolved by discussion.
Critical appraisal
The methodological quality of the included papers was assessed independently by two authors (LL and SK) using the Estabrooks’ Quality Assessment and Validity Tool for Cross-sectional Studies.Citation15 The tool consists of twelve criteria which examine sampling, measurement, and statistical analysis. The quality score of each included study was calculated by dividing the total number of points obtained by the total number of possible points, yielding a score between 0 and 1 for each study. The studies were then classified as weak (<0.50), moderate-weak (0.51–0.65), moderate-strong (0.66–0.79), or strong (0.80–0.10).Citation15 Differences in opinion were resolved by discussion. All relevant articles were included in the review irrespective of their methodological quality.
Data extraction and analysis
The first author (LL) extracted a range of information from each included study, comprising setting, participants, individual determinants or predictors of research evidence use (independent variables), outcome measures used to evaluate evidence uptake (dependent variable), and findings from each study. Extracted data were double-checked by another author (KGS) for accuracy. A quantitative synthesis of findings was not possible due to the heterogeneity of variables (individual determinants) and outcomes examined by individual studies. Thus, findings were synthesized in a qualitative manner to construct a narrative summary.
Results
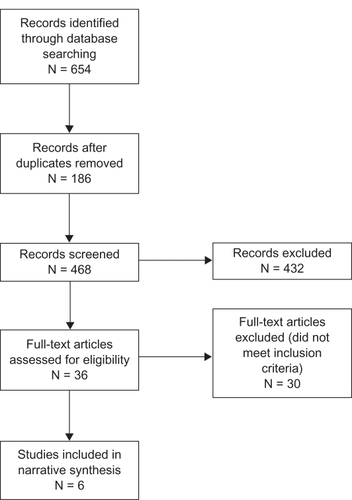
The search strategy identified 654 publications, which were reviewed by the authors (LL, KGS, SK) for duplicates. A total of 468 studies were screened for possible inclusion in the review and only 36 were considered to be potentially relevant and were retrieved for closer examination. After scrutiny, 30 articles were further excluded as they did not meet the inclusion criteria, leaving six studies for the systematic review. illustrates the process involved in the selection of studies for review.
Overview of included studies
All six studies that met the inclusion criteria were survey designs, and used self-reported questionnaires to gather data on research evidence uptake by AH practitioners. Of these, three examined predictor variables in physiotherapyCitation16–Citation18 and there was one each for occupational therapy,Citation19 social work and psychology,Citation20 and nutrition/dietetics.Citation21 Three of the studies (50%) were undertaken in the US, one in Canada, another in Australia and one study had participants from Australia, the UK, and Taiwan.
Methodological quality of included studies
Quality rating scores were either 0.43 or 0.64, indicating that two studies were of weak methodological quality, and four had moderate-weak strength. summarizes the methodological quality scores obtained by each of the included studies.
Table 1 Summary of methodological quality score
All studies drew their sample from more than one site, and achieved a response rate of more than 50%. More than half of the papers (67%) reported use of random sampling and 50% appeared to have adequate sample size. In all studies, measurement of the dependent variable (research evidence use) was undertaken using self-reported questionnaires. These questionnaires had acceptable reliability in half of the studies and adequate levels of validity in most of the papers (67%). Appropriate statistical tests were used in all studies, with the majority (83%) reporting P-values, however only two (33%) presented confidence intervals. Not one of the studies described missing data or how this was managed.
Individual determinants of research evidence use in AH
In all studies, research uptake outcomes were measured using self-reported questionnaires that examined information-seeking behavior, propensity to adopt EBP, and use of EBP in clinical practice. summarizes the individual determinants investigated by each of the included studies, including the outcome measures used.
Table 2 Summary of predictor variables examined and outcome measures
The individual determinants extracted from relevant studies were categorized into seven subgroupings of information: sociodemographic factors, education, beliefs and attitudes, involvement in research or EBP-related activities, professional characteristics/experiences, clinical setting, and information seeking. reports the predictor variables examined by individual studies and highlights those which were found to have significant correlation with research uptake. Education and professional characteristics were the most commonly examined individual determinants, while information-seeking was the least commonly reported.
Table 3 Summary of findings
Sociodemographic factors
Four studies assessed one or more individual determinants in this category,Citation16,Citation17,Citation19,Citation21 and only two found significant relationships.Citation16,Citation17 Age was examined by four studiesCitation16,Citation17,Citation19,Citation21 and gender was considered in two articles.Citation16,Citation21 In physiotherapy, being male was associated with the frequency of searching online databases.Citation16 In another study involving physiotherapists, age was found to have a negative correlation with propensity to adopt EBP.Citation17
Education
All six studies examined the relationship between educational background and different measures of research evidence use.Citation16–Citation21 Dietitians who were working on their doctoral degrees or those with advanced-level board certifications had significantly higher PAK (perceptions, attitudes, and knowledge of evidence-based practice) scores than their counterparts.Citation21 Three studiesCitation16–Citation18 examined the relationship between education and evidence uptake in physiotherapy but only two reported results. In one of the articles, holding a postgraduate degree was a significant predictor of positive perceived importance of research.Citation18 In the other study involving physiotherapists, the higher the degree of education obtained, the more likely they were to demonstrate propensity to adopt EBP.Citation17 Similarly for occupational therapists, higher levels of academic qualification were predictive of self-reported EBP uptake.Citation19 However, for mental health practitioners such as social workers and psychologists, no difference was found between doctoral and masters’ level of practitioners.Citation20
Beliefs and attitudes
Five studies assessed one or more determinants in this category.Citation16–Citation20 Two studiesCitation18,Citation20 assessed attitude towards research while one studyCitation19 examined attitudes toward establishing current best practice. Perceptions about organizational support and usefulness of research were reported in one study.Citation16 Practicality,Citation17 nonconformityCitation17 and self-efficacyCitation16 were measured in two studies. A positive correlation between perceptions, attitudes, beliefs, and evidence uptake was consistently found in all studies.
Involvement in research or EBP-related activities
Involvement in research or EBP-related activities was examined in four studies, all of which found significant associations with research evidence use.Citation16,Citation18,Citation20,Citation21 Allied health practitioners such as physiotherapists,Citation16 social workers,Citation20 psychologists,Citation20 and dietitiansCitation21 who had previous research experience, participated in research activities at work or have taken a research or EBP course were likely to report use of EBP, engage themselves in information-seeking behavior, report positive perceptions and attitudes towards research, and consider it important.
Professional characteristics/experiences
All six studies assessed one or more individual determinants in this category and the most frequently examined factors were years of practice, or work experience.Citation16–Citation21 However a significant relationship between work experience and evidence uptake was found in only one.Citation17 This study found a negative correlation between the number of years licensed and propensity to adopt EBP in physiotherapists. Membership in a professional organization was associated with reading the research literature among physiotherapists.Citation16 Dietitians who are members of at least two professional associations showed higher perception, attitude, and knowledge (PAK) scores compared to those whose membership is in only one association.Citation21 This paper also reported that working full-time was also associated with higher PAK scores in dietitians. There was a negative correlation between percentage of time in direct patient care and propensity to adopt EBP in physiotherapy.Citation17
Clinical setting or type of work environment
Only three studies reported findings in this category.Citation18,Citation20,Citation21 Mental health workers from hospitals or university clinics reported higher levels of EBP use compared to those working in private practice, community mental health centre, schools, and other clinical settings.Citation20 In physiotherapy, working in a hospital is a significant predictor of positive perceived importance of research.Citation18 Registered dietitians employed by universities and colleges scored significantly higher PAK scores than other practice settings such as acute care, ambulatory care, long term care, private office, and community.Citation21
Information seeking
Only one study examined the relationship between reading publications and research evidence use.Citation21 Dietitians who read professional publications bimonthly, weekly, or daily have higher PAK scores than those who reported reading monthly.Citation21
Summary of results
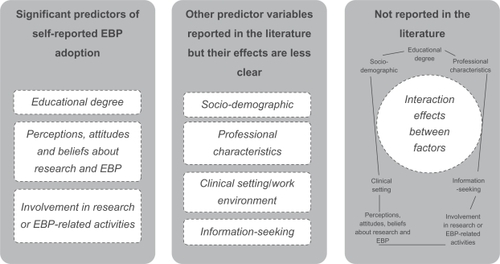
This review described a number of individual factors that were associated with the uptake of research evidence into AH clinical practice. illustrates the synthesized findings from the reviewed literature. The review demonstrated that factors such as educational degree or academic qualification, involvement in research or EBP-related activities, and practitioners’ perceptions, attitudes and beliefs about research, and EBP are significant predictors of self-reported EBP use in AH. The effect of other factors such as professional characteristics, clinical setting/work environment, information-seeking behavior, and sociodemographic variables (eg, age, gender) are less clear. Whether there is an interaction effect between evidence-uptake factors has not been tested.
Discussion
The diverse geographic origin of studies identified in this review highlights a worldwide interest in understanding why AH practitioners adopt evidence into clinical practice decisions. This validated the importance of bringing this information together in a review, so that efforts to address the research-practice gap can be addressed efficiently and effectively. The current review showed that factors such as educational degree or academic qualification, involvement in research or EBP-related activities, and practitioners’ perceptions, attitudes and beliefs about research, and EBP are significant predictors of self-reported research evidence use in AH.
The educational or academic qualification of practitioners was a significant predictor of evidence uptake in AH. This finding concurs with other literature which reports an association between level of education and research utilization in nurses.Citation15,Citation22 It could be argued that the academic or educational level in itself may not be the important predictor in EBP but the research knowledge obtained during additional education. This contention concurs with our review finding that AH practitioners who had been involved in research or EBP-related activities (ie, participation in research activities, or have taken a course in research or EBP) are likely to report uptake of research evidence, and regard it as important. Similar outcomes have been reported in nursing literature, which show that clinicians who have previous exposure to research perceive EBP more favorably than those who have not been exposed.Citation23–Citation25 In medicine, McColl et alCitation26 reported that physicians who were educated about research and participated in a practice-based research network had positive perceptions of EBP. It seems logical therefore, that if AH practitioners are to use research evidence in making decisions about the care of individual clients, they should be provided with training or education about research and EBP. To adopt an evidence-based approach, they should have the knowledge and skills to undertake the processes involved in EBP, which include formulating clinical questions, searching for relevant evidence, critically appraising evidence, implementing it into practice, and evaluating outcomes.Citation27,Citation28 Without these requisite knowledge and skills, AH practitioners may find it difficult to find, interpret, contextualize, and operationalize research evidence in practice. Previous studies, which have examined the impact of training programs to facilitate learning of EBP processes, have shown improvements in EBP competencies.Citation29–Citation34 The literature supports the importance of providing such training to health care practitioners to adopt an evidence-based approach.Citation32–Citation34 Our review results propose that exposure to research and EBP should be initiated in an undergraduate setting and then followed up in postgraduate training in order to produce optimum influence on research evidence uptake. Such an approach can instill a culture of research and harness EBP philosophy among health practitioners.
This review also found that perceptions, attitudes, and beliefs about EBP and research were significant predictors of research uptake in AH. Earlier studies found similar results for nurses, and reported a strong support for a link between beliefs and attitudes, and research utilization in nursing.Citation15,Citation35 Practitioners who perceive research as relevant to their work may be expected to be more open to EBP than those who view research as irrelevant to their practice. Those who have negative attitudes generally reflect a belief that EBP forces the practitioner to use research evidence as the sole basis for making clinical decisions, with little regard to clinical experience and patients’ unique circumstances.Citation36,Citation37 One of the frequently cited barriers in EBP is negative attitude which reflects the misconception about the use of research evidence in clinical practice.Citation37–Citation39 Correcting this misconception about what EBP is, and what it is not, may facilitate EBP uptake.Citation27,Citation40,Citation41 It is therefore important to emphasize that EBP does not consider research as the only source of evidence but rather suggests that research evidence be considered alongside clinical experience and patient values when making clinical decisions. The use of research evidence in practice would likely increase if AH practitioners have a better understanding of the EBP processes and what research evidence is.
Our review findings suggest that improving the research knowledge of practitioners and overcoming negative attitudes toward EBP have the potential to move AH practitioners towards regularly utilizing evidence in practice. According to Menon et al,Citation42 “Knowledge acquisition creates a strong foundation for promoting change in clinicians’ attitudes and practice behaviors, with the ultimate goal of improving patient-related outcome.” Allied health practitioners who do not have substantial knowledge about research, and do not have positive attitudes towards EBP may benefit from strategies that facilitate collaborative work between practitioners and researchers. Studies suggest that collaboration between research and practice may play a key role in the process leading to evidence-based practice innovations.Citation43–Citation47 Partnership between researchers and AH practitioners may result in amalgamation of expertise that may enhance the process of utilizing research evidence into practice. Researchers can mentor practitioners on how to develop answerable clinical questions, formulate a search strategy, and critique research evidence.Citation43 Practitioners, on the other hand, can help in developing research questions which are more in line with their needs, and hence could have a positive impact on the perceived value of research to practice.Citation47,Citation48 This collaborative approach may work effectively in clinically integrated interventions such as journal clubs or case discussions. There is emerging evidence from the literature that journal clubs which utilize a partnership between researchers/academics and practitioners may encourage EBP.Citation49,Citation50 Being involved in regular professional development activities such as journal clubs can put AH practitioners at the same levels of thinking and awareness of research evidence which are recognized to facilitate adoption of EBP.Citation50–Citation52
This review has limitations which should be considered when interpreting the results. First, this study examined only the individual determinants of research evidence use and did not address contextual and organizational factors (eg, culture, structure, resources) which have both been identified to influence evidence uptake by practitioners.Citation38,Citation53,Citation54 This is important because focusing only on how individual AH practitioners use evidence is insufficient as practice occurs in organizational contexts. Future research should aim to review these other factors and explore the interaction between characteristics of individual practitioners and the contextual components in the organization. This will ensure a targeted and holistic approach for effective and sustainable change in AH practices. Second, it is evident from this review that there has been reliance on self-report as a measure of research evidence use in AH. Social desirability bias in self-reported outcomes is believed to lead to overestimation of performance which does not reflect actual practice.Citation55,Citation56 On average, clinicians tend to overestimate their adherence to recommended practices by a median absolute difference of 27%.Citation55 Consequently the objective measurement of evidence uptake remains a persistent and unresolved problem. Currently, one of the most serious limitations to furthering research on EBP in AH practice is the lack of sensitive and valid measures of clinical behavior. This should be the subject of future research in the field of EBP implementation.
Conclusion
This review suggests that the most important individual determinants of research evidence use in AH are “level of academic qualification,” “being involved in research- or EBP-related activities” and “having positive perceptions, attitudes and beliefs about research or EBP.”
Implications to practice
Our findings highlighted the importance of understanding the unique characteristics of individual AH practitioners when designing interventions to address the research-practice gap. Efforts to promote evidence uptake in AH need to take into consideration these individual differences. Providing individually-targeted, multifaceted strategies is necessary to achieve change in the practice behavior of AH practitioners. Integral to these EBP strategies is an educational component. Therefore, opportunities should be made available to AH practitioners to engage in professional development activities relevant to EBP and research, such as journal clubs or case discussions. Pursuing postgraduate studies containing a significant research component can also influence AH practitioners’ propensity to use research evidence.
Implications to research
Future research in the field of EBP implementation should focus on three important areas: exploring the interaction of the individual determinants of research evidence use and determining whether or not this can influence practitioner behavior; understanding the interface between practitioner characteristics and the contextual components of their organization in order to ensure sustainable change in practice; and designing an objective and psychometrically sound instrument to measure the uptake and sustainability of evidence-based clinical decision making.
Disclosure
The authors report no conflicts of interest in this work.
References
- SackettDLRosenbergWMCGrayJAMHaynesRBRichardsonWSEvidence based medicine: what it is and what it isn’tBMJ1996312702371728555924
- UptonDUptonPKnowledge and use of evidence based practice by allied health and health science professionals in the United KingdomJ Allied Health200635312713317036666
- MetcalfeCLewinRWisherSPerrySBanniganKMoffettJKBarriers to implementing the evidence base in four NHS therapies: dieticians, occupational therapists, physiotherapists, speech and language therapistsPhysiotherapy2001878433441
- JetteDUBaconKBattyCEvidence-based practice: beliefs, attitudes, knowledge and behaviors of physical therapistsPhys Ther200383978680512940766
- BennettSToothLRMcKennaKTPerceptions of evidence-based practice: a survey of Australian occupational therapistsAust Occup Therap J20035011322
- IlesRDavidsonMEvidence based practice: a survey of physiotherapists’ current practicePhysiother Res Int2006112903103
- StevensonKLewisMHayEDoes physiotherapy management of low back pain change as a result of an evidence-based educational programmeJ Eval Clin Pract200612336537516722923
- SallsJDohliCSilvermanLHansenMThe use of evidence based practice by occupational therapistsOccup Ther Health Care2009232134145
- RochetteAKorner-BitenskyNDesrosiersJActual vs best practice for families post-stroke according to three rehabilitation disciplinesJ Rehabil Med200739751351917724549
- GoslingASWestbrookJIAllied health professionals’ use of online evidence: a survey of 290 staff working in the Australian public hospital systemInt J Med Inf2004734391401
- HadleyJHassanIKhanKKnowledge and beliefs concerning evidence-based practice amongst complementary and alternative medicine health care practitioners and allied health care professionals: a questionnaire surveyBMC Complement Altern Med200884518651937
- TaylorRSReevesBCEwingsPETaylorRJCritical appraisal skills training for health care professionals: a randomized controlled trialBMC Med Educ2004413015585061
- McCluskeyALovariniMProviding education on evidence-based practice improved knowledge but did not change behaviour: a before and after studyBMC Med Educ200554016364181
- TurnbullCGrimmer-SomersKKumarSMayELawDAshworthEAllied, scientific and complementary health professionals: a new model for Australian allied healthAust Health Rev2009331273719203331
- SquiresJEEstabrooksCAGustavssonPWallinLIndividual determinants of research utilisation by nurses: a systematic review updateImplementation Sci201161
- SalbachSMGuilcherSJTJaglalSBDavisDAFactors influencing information seeking by physical therapists providing stroke managementPhys Ther200989101039105019661160
- BridgesPHBieremaLLValentineTThe propensity to adopt evidence-based practice among physical therapistsBMC Health Serv Res2007710317615076
- Grimmer-SomersKLekkasPNylandLYoungAKumarSPerspectives on research evidence and clinical practice: a survey of Australian physiotherapistsPhysiother Res Int200712314716117624895
- BrownTTsengMHCaseyJMcDonaldRLyonsCPredictors of research utilization among paediatric occupational therapistsOTJR Occup Part Heal2010304172183
- NelsonTDSteeleRGPredictors of practitioners self–reported use of evidence-based practices: practitioners training, clinical setting and attitudes towards researchAdm Policy Ment Health200734431933017268858
- Byham-GrayLDGillbrideJADixonBKing StageFEvidence-based practice: what are dieticians’ perceptions, attitudes and knowledgeJ Am Diet Assoc2005105101574158116183358
- MichelYSneedNDissemination and use of research findings in nursing practiceJ Prof Nurs19951153063117593975
- OladeRAEvidence-based practice and research utilization activities among rural nursesJ Nurs Scholarsh200436322022515495490
- McClearyLBrownGTAssociation between nurses’ education about research and their research useNurs Educ Today2003238556565
- TsaiSLNurses’ participation and utilization of research in the republic of ChinaInt J Nurs Stud200037543544410785534
- McCollASmithHWhitePFieldJGeneral practitioners’ perceptions of the route to evidence-based medicine: a questionnaire surveyBMJ199831671283613659487174
- CordellWHChisholmCDWill the real evidence please stand up?EMN20012361114
- DawesMSummerskillWGlasziouPSicily statement on evidence-based practiceBMC Med Educ200551115634359
- RichardsonWSWilsonMCNishikawaJHaywardRSThe well-built clinical question: a key to evidence-based decisionsACP J Club199512331213
- RosenbergWMDeeksJLusherASnowballRDooleyGSackettDImproving searching skills and evidence retrievalJ R Coll Physicians Lond19983265575639881313
- TaylorRReevesBEwingsPBinnsSKeastJMearsRA systematic review of the effectiveness of critical appraisal skills training for cliniciansMed Educ200034212012510652064
- ParkesJHydeCDeeksJJMilneRTeaching critical appraisal skills in health care settingsCochrane Database Syst Rev20013CD00127011686986
- Flores-MateoGArgimonJMEvidence based practice in postgraduate healthcare education: a systematic reviewBMC Health Serv Res2007711917655743
- IlicDTeaching evidence-based practice: perspectives from the undergraduate and postgraduate viewpointAnn Acad Med Singapore200938655956519565109
- EllerLSKleberELanwangSResearch knowledge, attitudes and practices of health professionalsNurs Outlook200351416517012949476
- DiCensoACullumNCiliskaDImplementing evidence-based nursing: some misconceptionsEvid Based Nurs199813839
- PagotoSLSpringBCoupsEJMulvaneySCoutuMFOzakinciBarriers and facilitators of evidence-based practice perceived by behavioral science health professionalsJ Clin Psychol200763769570517551940
- GrolRWensingMWhat drives change? Barriers to and incentives for achieving evidence–based practiceMed J Aust2004180Suppl 6S57S6015012583
- BelizanMMeierAAlthabeFFacilitators and barriers to adoption of evidence-based practice perinatal care in Latin American hospitals: a qualitative studyHealth Educ Res200722683985317395605
- JenningsBMLoanLAMisconceptions amongst nurses about evidence-based practiceJ Nurs Scholarsh200133212112711419306
- TurkelsonCHughesJEWhy aren’t you doing evidence-based practice?AAOS Bulletin200654314
- MenonAKorner-BitenskyNKastnerMMcKibbonKAStrausSStrategies for rehabilitation professionals to move evidence-based knowledge into practice: a systematic reviewJ Rehabil Med20094131024103219893996
- RosswurmMALarrabeeJHA model for change to evidence-based practiceImage J Nurs Sch199931431732210628096
- LandryRAmaraNLamariMUtilization of social science knowledge in CanadaRes Policy2001302333349
- FoxNJPractice-based evidence: towards collaborative and transgressive researchSociology200337181102
- OsterlingKLAustinMJThe dissemination and utilization of research for promoting evidence-based practiceJ Evid Based Soc Work200851–229531919064452
- ChagnonFPouliotLGervaisMJPigeonMEComparison of determinants of research utilization by practitioners and administrators in the field of child and family social servicesImplement Sci201054120525270
- BergerRPractitioners in search of evidenceJ Soc Work2010102175191
- AustinTMRichterRRFreseTUsing a partnership between academic faculty and a physical therapist to develop a framework for an evidence-based journal club: a discussionPhysiother Res Int200914421322319562725
- LizarondoLKumarSGrimmer-SomersKSupporting allied health practitioners in evidence-based practice: a case reportInt J Ther Rehabil2009164226236
- McQueenJMillerCNivisonCHusbandVAn investigation into the use of journal club for evidence-based practiceInt J Ther Rehab2006137311316
- Campbell-FlemingJCataniaKCourtneyLPromoting evidence-based practice through a travelling journal clubClin Nurse Spec2009231162019098510
- BostromAMWallinLNordstromGEvidence-based practice and determinants of research use in elderly care in SwedenJ Eval Clin Pract200713466567317683312
- SalbachNMJaglalSBJorner-BitenskyNRappoltSDavisDPractitioner and organizational barriers to evidence-based practice of physical therapists for people with strokePhys Ther200787101284130317684088
- AdamsASSoumeraiSBLomasJRoss-DegnanDEvidence of self-report bias in assessing adherence to guidelinesInt J Qual Health Care199911318719210435838
- Van de MortelTFFaking it: social desirability response bias in self-report researchAust J Adv Nurs20082544048