Abstract
Objectives
To determine whether body composition is related to long-term outcomes amongst vascular inpatients with lower limb ulcers.
Design
Prospective study with 3 years follow-up.
Materials and methods
Body mass index (BMI), fat, and fat-free mass were measured and associations with readmission to hospital (number, cause, length of stay) and all-cause mortality were explored.
Results
Thirty patients (22 men, 8 women) participated in the study. Ten patients (33%) had a BMI ≥ 30 kg/m2. 18/20 (90%) patients with a BMI < 30 kg/m2 and 9/10 (90%) patients with a BMI ≥ 30 kg/m2 were admitted to hospital in the 3 years of follow-up. Patients with a BMI < 30 kg/m2 were admitted more frequently, earlier and for longer compared to those with BMI ≥ 30 kg/m2 but these did not reach statistical significance. The 3 year mortality rate for patients with BMI ≥ 30 kg/m2 was 20% (n = 2/10) compared to 70% (n = 14/20) with a BMI < 30 kg/m2, P = 0.019.
Conclusion
This preliminary study suggests that higher BMI may have a protective effect against mortality in vascular patients with lower limb ulcers. These findings contradict the universal acceptance that obesity leads to poor health outcomes. Further work is required to confirm these findings and explore some of the potential mechanisms for this effect.
Introduction
Overweight and obesity have recently been reported as modifiable risk factors for vascular disease.Citation1 In contrast to this, there is evidence to suggest that being malnourished can impair wound healing and recovery from vascular surgery.Citation2,Citation3 This is a challenge for both clinicians and consumers as recommendations for a healthy body composition will conflict according to disease progression.
In established vascular disease, particularly the presence of critical limb ischemia, it is not uncommon for patients to present in a state of nutritional deficiency. These patients also have increased nutrient requirements for wound healing (eg, protein, zinc)Citation4,Citation5 and being malnourished has been shown to increase the incidence of septic complications.Citation6 In established vascular disease it is still unknown what the ideal body composition might be but there has been some indication in the literature that it might be higher than the levels conventionally used as the ideal targets.
Two studies have examined the effect of body composition on mortality for vascular patients and reported that levels of fatness higher than conventionally used to describe healthy body composition might be beneficial. Davenport et alCitation7 concluded that mild obesity (defined as body mass index [BMI] > 30 kg/m2 and ≤35 kg/m2) may be an advantage rather than a risk factor for adverse outcomes at 30 days postsurgery including morbidity and mortality. Similarly Nafiu et alCitation8 concluded that patients within the conventional healthy BMI range were at greater risk of 30-day mortality postsurgery than those who were overweight or obese.
The rationale for the seemingly protective effect in vascular patients is not yet established but the protective effects are not unlike emerging evidence in studies of older adults whereby a higher BMI and avoiding weight loss has been demonstrated to be protective rather than detrimental.Citation9–Citation11 Similar findings have also been demonstrated in other groups of hospitalized patients.Citation12–Citation14 In contrast to previous studies that looked at short term outcomes associated with the protective effect of higher BMI, the purpose of this preliminary study was to determine whether this relationship persists longer term in vascular patients with lower limb ulcers. A particular emphasis is placed on outcomes of clinical relevance including hospital readmissions and all-cause mortality.
Materials and methods
Patients
All patients admitted to the Vascular Unit at the Repatriation General Hospital, Adelaide, South Australia, were screened for eligibility to participate in the study between August 2007 and November 2007. Patients were eligible if they were admitted for management of a lower limb ulcer of any etiology and excluded if they were palliative receiving comfort care, unable to fulfill the requirements of the study due to impaired cognitive function or receiving nutrition via enteral feeding or total parenteral nutrition. Patients with critical limb ischemia according to the TransAtlantic Inter-Society Consensus criteria were diagnosed with arterial ulcers. Venous ulcers were diagnosed with documented venous incompetence on duplex imaging, in the absence of established arterial disease as evidenced by ankle-brachial pressure indices > 0.9. Neuropathic ulcers were diagnosed clinically in diabetic patients in the absence of venous or arterial disease.
The study was approved by the Repatriation General Hospital Research and Ethics Committee and the Southern Adelaide Clinical Human Research Committee. All patients provided written informed consent prior to commencement of data collection and were free to withdraw at any time.
Measurements and procedures
Baseline characteristics of participants including date of birth, gender, and medical history were obtained from medical records.
Body weight was measured in the morning with participants in light clothing and without shoes using calibrated chair scales (±0.1 kg) (TI BWB-800C; Wedderburn, Malaga, WA, Australia). Knee height was measured as an estimate of standing height as the majority of patients were unable to assume the correct position for accurate measurement of standing height. Knee height (±0.1 cm) was measured using a caliper with a fixed foot plate and an adjustable, sliding end plate with the lower right leg positioned at an angle of 90° (Ross Laboratories, Columbus, OH). Standard validated equations for age and gender were used to estimate standing height.Citation15 Weight and estimated standing height from knee height were used to calculate estimated BMI (kg/m2). Participants were classified as: (1) BMI < 30 kg/m2, or (2) BMI ≥ 30 kg/m2 (obese) for the purpose of this study.Citation16
There is mounting evidence that percentage fat and fat-free mass are stronger predictors of health outcomes than body weight alone.Citation17,Citation18 Given the shortcoming of BMI reflecting only body size not body composition, measurement of fat and fat-free mass were included in this study. Fat and fat-free mass were determined to the nearest 0.1 kg using bioimpedance spectroscopy (BIS). BIS is a valid, portable, and relatively inexpensive method of estimating body composition.Citation19 Impedance was measured in the morning with an empty bladder between the wrist and ankle using a tetrapolar electrode method as recommended by the manufacturer (SFB7 Multi-Frequency Analysis Version 5.2.4.0; ImpediMed, Eight Mile Plains, Australia). The patients were dressed in light clothing without shoes, socks, or jewelry and were instructed to lie supine with arms separated from the body and legs not touching each other. Measurements were taken on the right side consistent with standard protocol.Citation20
Three year follow-up outcome data were obtained from medical records. Data included: time to first readmission (days), number of readmissions, cause of readmission (cardiovascular disease, respiratory, amputation, infection, other) total days in hospital from readmissions (days), all-cause mortality (alive/deceased) and days to death.
All data was analyzed using the SPSS statistical package (PASW version 18.0; SPSS Inc, Chicago, IL). Data was expressed as median (range) or n (%). Mann–Whitney U tests were performed to determine associations between fat mass and fat-free mass according to whether patients were readmitted or died in the subsequent 3 years. Mann–Whitney U tests were also performed to determine whether cause of readmission, number of readmissions, and total days of hospitalization in the subsequent 3 years were associated with BMI classification. Chi-square analyses were performed to determine whether BMI classification was associated with readmission to hospital or death in the subsequent 3 years. Kaplan–Meier survival analyses with log rank (Mantel-Cox) tests were performed to determine whether BMI classification was associated with days to first readmission and days to death. Hierarchical cox regression was performed to determine the effect of BMI on mortality independent of ulcer etiology. Findings were considered significant at the level of P < 0.05.
Results
represents the baseline characteristics of the 30 patients included in this study. Patients were mostly elderly (median age 78 years, range 40–91 years) and there was no significant difference in age between those with BMI < 30 kg/m2 and BMI ≥ 30 kg/m2. Similarly there was no significant difference in sex between those with BMI < 30 kg/m2 and BMI ≥ 30 kg/m2, with the majority being male (n = 22/30, 73%). Diabetes, heart disease, hyperlipidemia, and hypertension were common as was obesity. No patients were under-weight (BMI < 18.5 kg/m2). The etiology of the lower limb ulcers included arterial (n = 12/20 BMI < 30 kg/m2; 2/10 BMI ≥ 30 kg/m2), neuropathic (n = 4/20 BMI < 30 kg/m2; 7/10 BMI ≥ 30 kg/m2), and others (venous ulcers, pressure ulcers, squamous cell carcinoma each n = 1, 2 unknown).
Table 1 Baseline descriptive characteristics of 30 patients admitted to the vascular unit with lower limb ulcers between August and November 2007
reports the outcomes at 3 years for the 30 patients included in this study according to BMI classification. 18/20 (90%) patients with a BMI < 30 kg/m2 and 9/10 (90%) patients with a BMI ≥ 30 kg/m2 were admitted to a hospital in the 3 years of follow-up. There were a total of 154 admissions (60 vascular, 38 general medicine, 25 respiratory, 14 cardiovascular, 6 orthopedics, 6 gastroenterology, and 5 renal); 102 for those with BMI < 30 kg/m2 and 52 for those with BMI ≥ 30 kg/m2. Patients with a BMI < 30 kg/m2 were admitted more frequently, earlier, and for longer compared to those with BMI ≥ 30 kg/m2. However, these did not reach statistical significance. Readmissions for cardiovascular disease, respiratory disease, or amputation (minor/major) of the lower limb were evenly distributed between both BMI classifications. Kaplan–Meier survival analysis () demonstrated that there was no difference in time to hospitalization for those with a BMI ≥ 30 kg/m2 compared to those with BMI < 30 kg/m2 (P = 0.498).
Figure 1 Survival curve for number of days to first readmission according to BMI.
Abbreviation: BMI, body mass index.
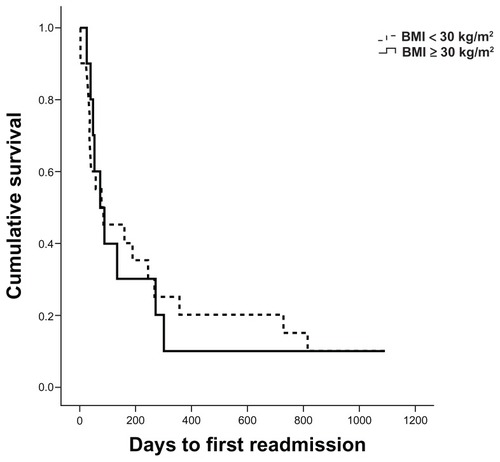
Table 2 Outcome data for 30 patients admitted to the vascular unit with lower limb ulcers between August and November 2007
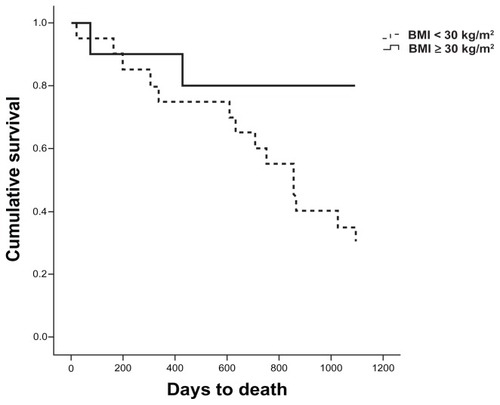
Sixteen (53%) patients died during the 3 year follow-up (4 respiratory, 2 cardiovascular, 10 unknown). Two (20%) patients with a BMI ≥ 30 kg/m2 died while 14 (70%) patients with a BMI < 30 kg/m2 died (P = 0.019). Kaplan–Meier survival analysis () demonstrated that those patients with a BMI ≥ 30 kg/m2 survived longer than those with a BMI < 30 kg/m2 (P = 0.027). Hierarchical cox regression determined that those patients with BMI < 30 kg/m2 were 4.6 times more likely to die than those with BMI ≥ 30 kg/m2 (95% confidence interval [CI]: 1.04–20.4; P = 0.04). When ulcer etiology was entered into the model those with BMI < 30 kg/m2 were 4.1 times more likely to die than those with BMI ≥ 30 kg/m2 (95% CI: 0.89–19.19; P = 0.07) and those with arterial ulcers were no more likely to die than those with ulcers of other etiology (hazard ratio, 1.4; 95% CI: 0.48–3.90; P = 0.57).
Figure 2 Survival curve for number of days to death according to BMI.
Abbreviation: BMI, body mass index.
Fat and fat-free mass according to whether patients were admitted to a hospital or had died in the subsequent 3 years are reported in . Median fat mass for those that died in the subsequent 3 years follow-up was significantly lower compared to those that survived the 3 years follow-up (P = 0.033). There was no significant relationship found between fat mass and readmission to hospital, or fat-free mass and either mortality or readmission to a hospital. When explored as percent fat and fat-free mass there were no significant differences identified.
Table 3 Outcome data at 3 years for 30 patients admitted to the vascular unit with lower limb ulcers between August and November 2007 according to fat (kg, %) and fat-free mass (kg, %) as measured by bioelectrical impedance analysis
Discussion
The findings of this small study suggest that obesity is common for patients with lower limb ulcers and that a higher weight for height may be protective in terms of mortality. These findings challenge evidence that poor outcomes are routinely associated with higher BMICitation16 and provides direction for further research to evaluate whether strategies for weight maintenance, regardless of baseline weight, improves health outcomes.
The concept that having a BMI above the ideal weight range seems to have a protective effect for vascular patients was supported with a trend suggesting that those with a BMI < 30 kg/m2 were also readmitted to a hospital sooner and stayed longer than those classified as obese (BMI ≥ 30 kg/m2).
While inconsistent with evidence suggesting higher body weight for height is associated with poor outcomes,Citation16 the findings of the present study do appear to be consistent with two previous studies exploring the ideal BMI range for vascular patients.Citation7,Citation8 Davenport et alCitation7 found in a sample of 7543 vascular patients undergoing a variety of surgical procedures that BMI between 30–35 kg/m2 was protective against perioperative 30 day mortality. Similarly, Nafiu et alCitation8 reported poorest outcomes amongst vascular patients that were underweight or in the desirable BMI range compared to those classified as overweight or obese. These outcomes included perioperative 30 day mortality and trends were also evident for a range of postoperative complications. For both studies the mean age of participants was >60 years, perhaps allowing some synergies to be drawn from longstanding evidence in geriatrics and inpatient populations that higher BMI is protective.Citation16
Increasingly, there is evidence amongst older adults that a higher BMI might be advantageous. While the mechanism underlying this protective effect is not clearly understood, the ‘obesity paradox’ as it has been reported, is clearly a valid concept with many studies reporting a significant survival benefit for older adults.Citation21–Citation23 One proposed mechanism for the protective effects illustrated in the geriatric literature is the reduction in oxidative stress and inflammation associated with maintaining a higher body weight and avoiding weight loss and sarcopenia.Citation22 Lower fat-free mass has been linked to reduced antioxidant capacity and poor outcomes.Citation24 The additional energy reserves assist in retaining lean body mass and hence prevention of malnutrition may also be responsible for the protective effects observed. Adiposity in the latter years is also understood to assist in maintaining bone mineral density and can provide protection against fall-related fractures, an event known to be associated with a high mortality rate.Citation22 Which, if any, of these mechanisms are responsible for the findings of the present study cannot be determined but highlights that the question is worthy of further exploration. So too is the evaluation of energy needs and expenditures associated with ulcers of different size and etiology which would aid calculation of nutritional requirements for specific patient groups, potentially preventing weight loss and malnutrition and improving outcomes.
There is an argument that increased survival at any cost may not be the preference of patients. Some studies have shown that there is an increased risk of other complications and delayed wound healing in patients that are overweight or obeseCitation25 and hence quality of life, not only quantity of life, needs to be considered. A discrete choice experiment to elicit the views and preferences of vascular patients about alternative health states would be helpful to inform this discussion.
Of interest in this study was the lack of effect observed for a relationship between fat mass and readmission to hospital and fat-free mass and either mortality or readmission to hospital. While there was a trend for those with lower fat mass to be more likely to be readmitted to hospital and for those with a lower fat-free mass to be deceased, the differences did not achieve statistical significance and were not consistent when examining percent fat and fat-free mass. In contrast, and against what might be expected, those participants with higher fat-free mass seemed to be more likely to be readmitted to hospital however statistical significance again was not achieved so these findings should be interpreted with caution as they might simply be a chance trend that does not persist with a larger sample size. There are no clear indications why this trend would in fact be true.
It is important to acknowledge that the present study did not allow for classifications across the range of obesity classes due to the small sample size. Caution is therefore necessary in extrapolating the findings to those with a BMI > 40 kg/m2 where there is some evidence to suggest that poorer health outcomes once again become concerning.Citation7,Citation8 The small sample size and associated risk of type 2 error may likely have contributed to the inability to demonstrate statistically significant findings for the range of outcomes explored. The study could also have been strengthened with a sample size sufficient to undertake multivariate analyses to determine the strength of BMI, fat mass, and fat-free mass in predicting mortality and hospital admissions after controlling for a range of potential confounders (including concomitant disease, medication, and mobility). In the present study it was clear that there was a difference in the proportion of participants with an arterial ulcer between the BMI classifications, an important consideration for multivariate analyses in the future as it is recognized that patients with critical limb ischemia have higher mortality. It would also be of interest for future studies with sufficient samples to generate survival curves by ulcer type to help illustrate the above. Alternative measures of body size and composition may also be warranted for future studies. BMI does not differentiate between central or peripherally stored weight which may influence outcomes.Citation16 Waist and hip circumference may be more useful for examining differences in position of stored weight and should be considered for future studies.Citation16 Similarly, there are arguments that BIS may not provide a valid estimate of fat and fat-free mass and that dual energy X-ray absorptiometry would be more appropriate.Citation26 While dual energy X-ray absorptiometry is clearly a more valid technique, it is far less accessible and more expensive than BIS and hence its application for clinical purposes is limited.Citation27,Citation28 Despite these limitations, the findings of the present study do extend the current body of evidence by demonstrating preliminary evidence to suggest that the protective effect of a higher BMI may extend beyond the 30 days previously reported in surgical patients over a longer duration in vascular patients with lower limb ulcers.
Given these findings, recommendations regarding weight management for vascular patients may need to be revised in the future; what is recommended for the general population may not be appropriate for vascular patients. Future investigations should be conducted to confirm these preliminary findings and further study the long-term outcomes for these patients and what mechanisms are responsible for this potentially protective effect.
Acknowledgments
The authors wish to acknowledge the participation of the patients without whom this study would not have been possible.
Disclosure
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
The authors report no conflicts of interest in this work.
References
- RaoGHThethiIFareedJVascular disease: obesity and excess weight as modulators of riskExpert Rev Cardiovasc Ther20119452553421517735
- ThompsonCFuhrmanMNutrients and wound healing: still searching for the magic bulletNutr Clin Pract200520333134716207672
- WilliamsJZBarbulANutrition and wound healingSurg Clin North Am200383357159612822727
- BreslowRAHallfrischJGuyDGCrawleyBGoldbergAPThe importance of dietary protein in healing pressure ulcersJ Am Geriatr Soc19934143573628463519
- GreavesMWSkillenAWEffects of long-continued ingestion of zinc sulphate in patients with venous leg ulcerationLancet1970276798898914097278
- DurkinMTMercerKGMcNultyMFContribution of malnutrition to postoperative morbidity in vascular surgical patientsBr J Surg1999865690711
- DavenportDLXenosESHosokawaPRadfordJHendersonWGEndeanEDThe influence of body mass index obesity status on vascular surgery 30-day morbidity and mortalityJ Vasc Surg200949114014719028047
- NafiuOOKheterpalSMouldingRThe association of body mass index to postoperative outcomes in elderly vascular surgery patients: a reverse J-curve phenomenonAnesth Analg20111121232921127285
- BeckAMOvesenLAt which body mass index and degree of weight loss should hospitalized elderly patients be considered at nutritional risk?Clin Nutr199817519519810205338
- BannermanEMillerMDDanielsLAAnthropometric indices predict physical function and mobility in older Australians: the Australian Longitudinal Study of AgeingPublic Health Nutr20025565566212372159
- NewmanABYanezDHarrisTWeight change in old age and its association with mortalityJ Am Geriatr Soc200149101309131811890489
- LandiFOnderGGambassiGPedoneCCarboninPBernabeiRBody mass index and mortality among hospitalized patientsArch Intern Med2000160172641264410999978
- HallJAFrenchTKRasmussonKDThe paradox of obesity in patients with heart failureJ Am Acad Nurse Pract2005171254254616293163
- VigderCBen IsraelYMeiselSRKaykovEGottliebSShotanAManagement and 1 year outcome of oldest-old hospitalized heart failure patients: a subacute geriatric hospital surveyIsr Med Assoc J201012848348821337817
- ChumleaWCGuoSEquations for predicting stature in white and black elderly individualsJ Gerontol1992476M197M2031430854
- Dietitians Association of AustraliaBest Practice Guidelines for the Treatment of Overweight and Obesity in AdultsCanberra, AustraliaDietitians Association of Australia2005
- SegalKRDunaifAGutinBAlbuJNymanAPi-SunyerFXBody composition, not body weight, is related to cardiovascular disease risk factors and sex hormone levels in menJ Clin Invest1987804105010553654969
- VanItallieTBYangMUHeymsfieldSBFunkRCBoileauRAHeight-normalised indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional statusAm J Clin Nutr19905269539592239792
- TengvallMEllegårdLMalmrosVBosaeusNLissnerLBosaeusIBody composition in the elderly: reference values and bioelectrical impedance spectroscopy to predict total body skeletal muscle massClin Nutr2009281525819010572
- HeywardVHPractical body composition assessment for children, adults, and older adultsInt J Sport Nutr1998832853079738136
- ChapmanIMObesity paradox during agingInterdiscip Top Gerontol201037203620703053
- OreopoulosAKalantar-ZadehKSharmaAMFonarowGCThe obesity paradox in the elderly: potential mechanisms and clinical implicationsClin Geriatr Med200925464365919944265
- TrullàsJCFormigaFMonteroMParadox of obesity in heart failure: results from the Spanish RICA RegistryMed Clin (Barc)20111371567167721719051
- SparkJIRobinsonJMGallavinLPatients with chronic critical limb ischaemia have reduced total antioxidant capacity and impaired nutritional statusEur J Vasc Endovasc Surg200224653553912443751
- FasolRSchindlerMSchumacherBThe influence of obesity on perioperative morbidity: retrospective study of 502 aortocoronary bypass operationsThorac Cardiovasc Surg19924031261291412377
- BussolottoMCecconASergiGGiantinVBenincàPEnziGAssessment of body composition in elderly: accuracy of bioelectrical impedance analysisGerontology199945139439852379
- LiCFordESZhaoGBalluzLSGilesWHEstimates of body composition with dual-energy X-ray absorptiometry in adultsAm J Clin Nutr20099061457146519812179
- WilliamsJEWellsJCWilsonCMHarounDLucasAFewtrellMSEvaluation of Lunar Prodigy dual-energy X-ray absorptiometry for assessing body composition in healthy persons and patients by comparison with the criterion 4-component modelAm J Clin Nutr20068351047105416685045