Abstract
Purpose
The optimal setting for interprofessional education (IPE) for prelicensure health care trainees is unclear, especially in a field as complex and emotionally challenging as oncology. In this article, the authors describe the initiation of the Cross Cancer Institute Multidisciplinary Summer Studentship in Palliative and Supportive Care in Oncology, a 6-week, multidisciplinary team-based clinical placement in supportive care, designed to incorporate features of best practice cooperative learning.
Methods
A steering committee established goals, structure, eligibility criteria, application process, funding, and a consensus approach to instruction and evaluation for the IPE program. Studentship components included mandatory and flexible clinical time, an exploratory investigation, discussion groups, and a presentation. Two senior students per iteration were selected from clinical nutrition, medicine, nursing, occupational therapy, pharmacy, physiotherapy, respiratory therapy, social work, and speech–language pathology applicants. These students completed questionnaires investigating their views of their own and others’ professions at baseline, at the end of the rotation, and 6 months after the studentship.
Results
Eight students from medicine, clinical nutrition, occupational therapy, physiotherapy, and speech–language pathology have participated to date. At the elective’s end, students have described a more positive view of multidisciplinary team practice, with each participating discipline perceived as both more caring and more subservient than at baseline. In general, changes in attitudes were maintained 6 months after completion of the placement.
Conclusion
This 6-week multidisciplinary placement is feasible, successful, and potentially transferable to other academic settings. The results of this study suggest that even over as short a period as 6 weeks, objective attitudinal and perceptual change is seen.
Introduction
Interprofessional education (IPE) is defined as students from two or more professions associated with health care learning with, from, and about each other.Citation1 IPE empowers practitioners to cope with issues that surpass the scope of any one profession. It aims to improve trust and communication, ultimately leading to improvements in attitudes that members of one discipline may have toward another.Citation1 Commonly in IPE, teams of students encounter a real-life situation, plan what they are to do as a group, carry out the plan under supervision, gather observations of the outcomes, and create generalizations that reinforce, modify, or change the way they would handle similar cases in the future.Citation2
Many examples of methods for teaching IPE to prelicensure (undergraduate) students have been reported. It is unclear which method is optimal for knowledge transfer, as the literature proving long-term behavioral and attitudinal change is thin.Citation3 Working with illustrative cases is thought to expose “students to problematic situations and challenge them to apply … knowledge to analyze the issues and formulate workable solutions.”Citation2 Learning from experience is unplanned learning that takes place in the normal course of real-life encounters. Similarly, in-service learning involves students being immersed in a task-oriented service-provision environment (ie, a work setting similar to the one that will be entered on completion of training).Citation2
Best practice cooperative learning, meanwhile, has five aspects. The first is positive interdependence, which describes students as being interconnected by roles that complement one another.Citation2 The second aspect is face-to-face promotive interaction, which means close, purposeful activity such as debate or joint decision making. The third, group processing, involves the student reflecting on his or her own actions and those of the group, determining what contributed to team effectiveness. The fourth aspect is individual accountability, which means that each individual is expected to contribute to the success of the group. The final aspect encompasses the interpersonal and small-group skills required to succeed in such a setting.Citation2
In Canada, the University of Alberta’s Interprofessional Initiative offers an undergraduate course that provides practice with team building and is mandatory for undergraduate students of ten different health care disciplines. While an exceptional classroom foundation, this course does not involve experiential learning in clinical placements. There is also no formal mechanism in place to promote IPE at the Cross Cancer Institute (CCI) (Edmonton, Alberta, Canada), the city’s tertiary cancer center, at which many University of Alberta health care students are trained. Any IPE that takes place at the CCI is on an ad hoc basis, when students shadow discipline-specific mentors involved in care teams.
In this article, the authors describe the initiation of the CCI Multidisciplinary Summer Studentship in Supportive and Palliative Care in Oncology, an elective clinical placement designed to incorporate each of the five aforementioned features of optimal IPE. At the CCI, psychosocial support, symptom control, and palliative care are delivered largely by multidisciplinary teams (MDTs) whose members practice both discipline-specific and team process skills. These skills, although essential in supporting patients with complex needs via a team approach, have largely been learned “on the job.” The studentship has two main aims: (1) to learn what supportive care encompasses and (2) to learn how it is delivered by frontline professionals working within a MDT. To the authors’ knowledge, this article describes the first multidisciplinary, prelicensure clinical placement focused on patients with advanced cancer.
IPE program description
Faculty
The multidisciplinary Steering Committee (SC) comprised seven department heads or clinical program leads plus representatives from nursing education and patient concerns, all of whom had an interest in IPE, role-specific expertise, a strong academic focus, and past collaborative successes. Most were already involved in training their respective undergraduate and/or postgraduate students. Subsequent to establishment of the SC, general objectives for both students and committee members were formulated (), and a common vision and logistical framework were described. Subsequently, SC members solicited feedback from colleagues on appropriate timing and length of placement, insurance, course credit, and tuition. SC members investigated possible clinical experiences, funding, and types of exploratory investigation projects.
Table 1 Studentship goals and objectives
Eligibility criteria and application procedure
As the principle of mutual interdependence suggests that students must have some background in their own disciplines before coming together as team members,Citation2 eligible trainees were required to have completed at least one previous clinical placement. For example, medical (MD) students completing their second year, and registered nursing (RN) students completing their third year were invited to apply. Training programs of disciplines involved in MDT care provision at the CCI were approached for participation, including clinical nutrition (CN), MD, RN, occupational therapy (OT), pharmacy (pharm), physiotherapy (PT), social work, speech–language pathology (SLP), and respiratory therapy. Advertising methods included email, posting information on websites, notices in classrooms, short presentations to students, and brochures. Applicants were asked to provide a curriculum vitae, a one-page cover letter describing their interest, and one letter of reference. SC members and one community representative vetted the completed application packages. A shortlisted group of students was interviewed either in person or by teleconference. Two successful candidates from different disciplines per iteration were identified and placed concurrently to encourage cooperation and teamwork.
Structure
Although preceptor vacation did complicate scheduling, a summer placement was chosen for several reasons: there are few other students present at the CCI, and staff have few other academic commitments at this time; participants are largely free from classes; and an honorarium can be provided if it is considered an “extra” experience.
The vision of the studentship was twofold: (1) to view the cancer experience through a patient’s eyes and (2) to view health care collaboration and service provision from the perspective of multiple health care disciplines. To accomplish this, the studentship has five main components ().
Table 2 Summary of studentship structure
The students form a “team within a team” and are mentored in the art of patient and family support by the entire spectrum of disciplines in their mandatory clinical time, sometimes separately and sometimes concurrently. Even in the setting of clinical preceptors mentoring trainees from other disciplines, passive observation was avoided in favor of graded responsibility during integration into care teams as clinical skills allowed. A wide variety of experiences in many departments and settings, and with different MDTs, were scheduled. This included support groups, case conferences, tumor boards, in-hospital (acute care) consultation services, ambulatory clinics, the city’s tertiary palliative care unit, educational rounds, hospice visits, and home care. For areas in which it may have been inappropriate to allow students to observe actual patient interactions – such as psychology, chaplaincy, clinical ethics, or patient concerns – alternative activities such as role-playing were scheduled. Additionally, flexible clinical time could be used for pursuing preexisting clinical interests or the exploratory investigation.
The exploratory investigation was intended to be beneficial to or of educational value for patients, the department, or the institution. It had to be suitable for completion in a 6-week period, incorporate a literature review, and preferably be suitable for publication.Citation4,Citation5
Both students per iteration and one clinical mentor met for weekly discussion groups (fireside chats) to explore common professional knowledge, reflect on specific patient encounters, and discuss issues related to collaborative practice. Facilitators were given a list of small-group teaching tips and examples of leading questions (eg, “When do you think the group was working at its best?”).Citation6 The students were encouraged to reflect on group actions, MDT and discipline roles, and their own actions and feelings. Constructive feedback on the placement was elicited.
Finally, the end-of-placement presentation was an opportunity to practice speaking to a multidisciplinary audience.
Evaluation
Educational research must help define practice, necessitating an evaluation component.Citation3 General surveys were completed exploring the students’ personal objectives and background clinical and MDT experience. Validated questionnaires were completed to determine what changes in attitude, if any, occurred (–). The Interdisciplinary Education Perception Scale (IEPS)Citation7 has 18 response items that measure competency within one’s own profession, perceived need for interdisciplinary cooperation, the experience of actual cooperation, and willingness to understand the contributions of other professionals. Each item is scored on a Likert scale, where 1 indicates “strongly disagree” and 6 indicates “strongly agree.” Larger scores indicate that the respondent thinks more highly of their own profession. The Attitudes to Health Professions Questionnaire (AHPQ)Citation8 measures attitudes toward other health professionals to assist in understanding differences between disciplines. It is a 20-item, 10 cm visual analogue scale with caring and subservient subscales. Smaller absolute scores indicate that the respondent thinks more highly of other health professions. Successful completion of the studentship was determined as outlined in . Students were contacted 6 months after completion of the studentship (with their permission) and the same questionnaires were readministered. Finally, feedback was invited from the SC to determine whether or not the committee’s objectives had been met.
Figure 1 Average change in Interdisciplinary Education Perception Scale scores, from baseline to 6 weeks (n = 8; *n = 7).
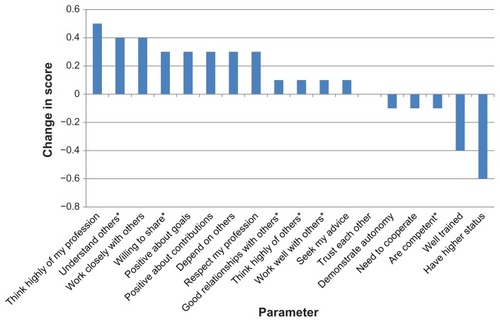
Figure 2 Average change in Interdisciplinary Education Perception Scale scores, from baseline to 6 months (baseline and 6 weeks: n = 8 [except *n = 7]; 6 months: n = 4).
![Figure 2 Average change in Interdisciplinary Education Perception Scale scores, from baseline to 6 months (baseline and 6 weeks: n = 8 [except *n = 7]; 6 months: n = 4).](/cms/asset/5198e3e7-c016-4dc5-97e1-fbae48b8487a/djmd_a_34527_f0002_b.jpg)
Figure 3 Average change in Attitudes to Health Professions Questionnaire scores, baseline to 6 weeks (n = 8).
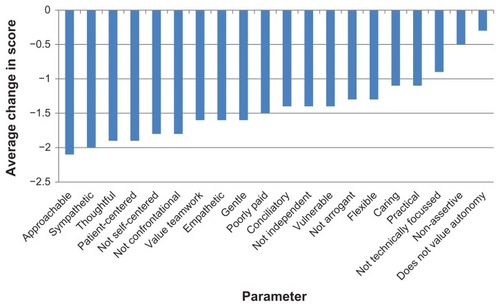
Figure 4 Average change in Attitudes to Health Professions Questionnaire scores, baseline to 6 months (baseline and 6 weeks: n = 8; 6 months: n = 4).
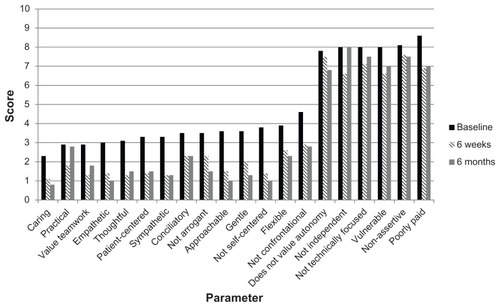
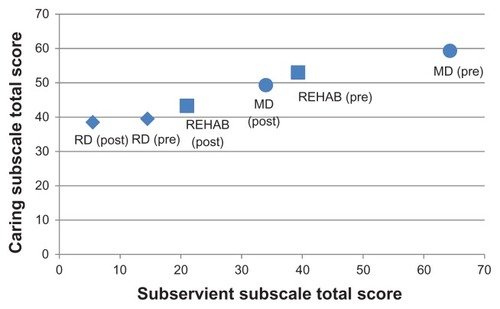
Figure 5 Average change in scores of the caring and subservient subscales of the Attitudes to Health Professions Questionnaire, baseline (pre) to week 6 (post), demonstrating the degree to which physicians (MD), registered dietitians (RD), and rehabilitation (Rehab) (speech-language pathology, physiotherapy, occupational therapy) professionals are viewed as caring and subservient by others.
IPE program evaluation
Eight students from the MD, CN, OT, PT, and SLP disciplines have participated in the IPE program. Students had completed an average of 16 weeks of clinical placements prior to the studentship in areas as diverse as radiology, intensive care, and pediatrics. Previous MDT experience varied as a result of those placements, undergraduate education, mandatory didactic courses, and extracurricular activities.
For the IEPS, larger scores were indicative of a more positive view of the student’s own profession. The average change in scores from baseline to week 6 ranged from 0.5 to −0.6. Of the 18 items in the IEPS, scores for 12 items increased, reflecting an improved outlook (). Average absolute scores over time are shown in , with 6 months of data available for four students. Scores usually decreased at week 6 in comparison with baseline, with some attitudinal changes maintained to 6 months, some returning to baseline, and still others increasing past baseline values ().
For the AHPQ, smaller scores were indicative of a more positive view of other professionals. Changes in average scores from baseline to week 6 ranged from −0.3 to −2.1 (). Average absolute scores over time are shown in , with 6 months of data again available for four students. All scores decreased at week 6 in comparison with baseline, with many changes in perception still present at 6 months but some returning to baseline. Few increased past baseline values at 6 months (). At the end of the elective, each participating profession was perceived as both more caring and more subservient than at baseline ().
At the end of the elective, students generally described a more positive view of MDT practice and a better appreciation of the cancer journey, with some expressing personal growth and an aspect of transformation from their experiences ().Citation9
Table 3 Examples of qualitative student feedback (n = 8)
On average, clinical mentors spent between half a day to 1 day with each student on various activities, which seven of the eight students (87.5%) felt was appropriate and one felt was too little. Six of the eight students (75%) did not support changing the time of year of the studentship, one wanted to switch from summer, and one was neutral. In comparing these students with other students supervised, faculty considered the depth of reflection was much more significant; they noted advantages of two students being placed together and they considered the focus on MDT practice was a significant added benefit. All SC members who attended the final presentations considered that both the exploratory investigation and the presentation positively affected students’ learning. All eight SC members agreed that objectives were met and agreed to continue their participation.
Discussion
Through the new CCI Multidisciplinary Summer Studentship in Supportive and Palliative Care in Oncology, prelicensure students were introduced to the art of supportive care throughout the cancer journey, from diagnosis to end of life, by a broad spectrum of health care professionals. Participating senior health care trainees gained experience in team-based skills and compassionate care, became familiar with other disciplines, and formed collaborative partnerships. The studentship attempted to encompass the features of best practice cooperative learning. Various types of multidisciplinary learning were utilized, such as working with illustrative cases, learning from experience, and in-service learning.Citation2 It was not intended to replace a discipline-specific mandatory clinical placement. In the present study, the students’ scores on the IEPS and AHPQ at week 6 (and, to a lesser extent, at month 6) suggest internalization of their experiences resulting in attitudinal and perceptual change. The authors propose that this blueprint is transferable to other settings, with minor modifications.
Assumptions underpinning the push for multi- or transdisciplinary collaboration include advantages surrounding quality and individualization of care, access to providers, effective use of scarce resources, patient and practitioner satisfaction, and cost-effectiveness.Citation10 Complex health care presentations, such as are commonplace in oncology, often exceed the capacity of any one individual to support. Formal teams provide a structure for coordinating the efforts of independent disciplines, and team practice results in pooling of knowledge, skills, and attitudes for the benefit of the patient and his or her family.Citation11 By making the best use of the competencies of all health professionals, collaboration should provide timely quality care, potentially in a more cost-effective manner.Citation11
Two of the main barriers to teaching an interdisciplinary approach are (1) lack of existing IPE and (2) a dearth of role models in undergraduate clinical placements.Citation11 Unfortunately, most health care professionals are first introduced to team practice “on-the-job.”Citation1 However, learning must prepare students for the real world in which they will work, especially in emotionally charged areas.Citation2
In view of … changing trends, corresponding changes must be made in the way health care providers are educated … If health care providers are expected to work together and share expertise in a team environment, it makes sense that their education … should prepare them for this.Citation12
If current best practices dictate a paradigm shift toward MDTs, then undergraduate student learning must model these teams in increasingly realistic and complex situations.Citation2 Changing the way health provider students are educated and socialized is key to entrenching system change.Citation3,Citation10,Citation11
It is important to objectively measure the impact of the approach used in the present study. The authors considered that the IEPS was appropriate, given its validation on a cross-disciplinary sample (n = 143) of students from OT (60%), medical office assistant (27%), SLP (9%), and therapeutic recreation (4%) programs, of whom 83% were undergraduates and 86% were female. The Cronbach’s alpha coefficient of reliability for all items was 0.87, and construct validity has been established.Citation7
Unlike the IEPS, the AHPQ measures attitudes around specific health professions and is applicable to a wide range of disciplines. The AHPQ was developed by staff from a range of different health care backgrounds, and, after revision, was validated on first-year trainees from the MD, RN, OT, PT, midwifery, and pharm disciplines (n = 160).Citation8 In that study, pharm trainees were viewed as significantly less caring than MD trainees, who were in turn viewed as less caring than PT trainees. Professions seen as the most caring were OT, RN, and midwifery. Nurses were perceived as being the most subservient and MDs as being the least, with other professions perceived as intermediate between the two. Internal consistency overall was 0.86 (0.91 for the caring and 0.59 for the subservient subscales). Test–retest intraclass correlation coefficients ranged from 0.34 to 0.85.Citation8 To the authors’ knowledge, there have been no reports of similar questionnaires either constructed or validated using CN students.
The CCI Multidisciplinary Summer Studentship in Supportive and Palliative Care in Oncology was loosely based on a similar interprofessional elective at the Toronto Rehabilitation Institute (Ontario, Canada), which began in 2004.Citation1 In the Toronto interprofessional elective, representatives from the RN, OT, pharm, PT, social work, MD, and SLP disciplines are placed together on the same clinical unit, as a team unto themselves. The student team attends group orientation sessions followed by weekly tutorials, clinical shadowing of discipline-specific mentors, and a group presentation at the completion of the rotation.Citation6
Benefits of hosting IPE clinical placements have been reported by other institutions to include the following: improved recruitment and retention of health care providers, recommitment to collaboration and teamwork, increased teaching activity, increased number and breadth of students completing rotations, and an increase in research dollars.Citation6 Additionally, clinical faculty themselves learn more about the professions they work with; student feedback can be used for quality improvement in the teams they shadow; the development of, for example, education materials by students is beneficial for current and future patients; enhanced awareness of collaborative opportunities and challenges occurs; and team education through the final presentations takes place.Citation6 Furthermore, facilitating and modeling MDT best practices for the benefit of students strengthens current partnerships.
Conclusion
In conclusion, the CCI Multidisciplinary Summer Studentship in Palliative and Supportive Care in Oncology is feasible, successful, and potentially transferable to other academic settings. The results of this study suggest that even over as short a period as 6 weeks, objective attitudinal and perceptual change is seen. Trainees practice team process and clinical skills that are transferable to future clinical placements and, ultimately, post-licensure practice. Further studies are required that describe the integration of students within established MDTs, which must be accompanied by an evaluation component proving presumptive outcomes.
Acknowledgments
This study was presented in part at the 22nd International Symposium of the Multinational Association of Supportive Care in Cancer, June 25–27, 2009, in Rome, Italy. The authors acknowledge generous support received through the Alberta Cancer Research Institute (Edmonton, Alberta, Canada), an unrestricted educational grant from Ortho Biotech, and the Alberta Cancer Foundation (Edmonton, Alberta, Canada). The authors also with to acknowledge all participating clinical mentors and students.
Disclosure
The authors report no conflicts of interest in this work. The authors alone are responsible for the content and writing of this article.
References
- LumagueMMorganAMakDInterprofessional education: the student perspectiveJ Interprof Care200620324625316777792
- D’EonMA blueprint for interprofessional learningJ Interprof Care200519Suppl 1495916096145
- HerbertCPChanging the culture: interprofessional education for collaborative patient-centred practice in CanadaJ Interprof Care200519Suppl 11416096140
- LefresneSFairchildABistritzAVennerPYeeDA case of indirect cauda equina syndrome from metastatic prostate cancerCan Urol Assoc J200934E31E3519672434
- LefresneSFairchildAJohnsonRDeschenesJRussellLPedersonJGenitourinary malignancy presenting as an ocular metastasis: a case report and review of the literatureCan Urol Assoc J201262E67E7122511437
- SinclairLLoweMPaulenkoTWalczakAFacilitating Interprofessional Clinical Learning: Interprofessional Education Placements and Other OpportunitiesToronto, CanadaUniversity of Toronto, Office of Interprofessional Education2007
- LuechtRMMadsenMKTaugherMPPettersonBJAssessing professional perceptions: design and validation of an interdisciplinary education perception scaleJ Allied Health19901921811912365636
- LindqvistSDuncanAShepstoneLWattsFPearceSDevelopment of the “Attitudes to Health Professionals Questionnaire” (AHPQ): a measure to assess interprofessional attitudesJ Interprof Care200519326927916029980
- LefresneSNielsenDFairchildAThe Cross Cancer Institute Multidisciplinary Summer Studentship in Palliative and Supportive Care in Oncology: teaching students to see through patients’ eyesSupport Care Cancer201119340340820204420
- IveySLBrownKSTeskeYSilvermanDA model for teaching about interdisciplinary practice in health care settingsJ Allied Health19881731891953192484
- RayMDShared borders: achieving the goals of interdisciplinary patient careAm J Health Syst Pharm19985513136913749659964
- RomanowRJBuilding on Values: The Future of Health Care in Canada; Final ReportSaskatoon, CanadaCommission on the Future of Health Care in Canada2002