Abstract
Background
Globally, oral health training has shown positive influence on knowledge, competency and practices for both oral and non-oral health-care workers towards integration of oral health into primary health care (PHC). Sub-Saharan Africa has very divergent social-cultural-political-economic settings. Since healthcare is contextual, it is necessary to review oral health training programs in this region to establish if their formulation, implementation and evaluation are context-reliant.
Objective
To assess if oral health trainings aimed at integrating oral health into PHC in sub-Saharan Africa were context-reliant.
Methodology
The reviewers searched five electronic databases and WHO sites. Selection of publications was done using the PRISMA framework. Oral health training programs for oral and non-oral health-care workers in sub-Saharan Africa published in English language between year 2001 and 2020 were included in the study.
Findings
Only 4 (0.8%) of the original 512 publications for oral health-care workers and 9 (1.5%) of the 613 for non-oral health-care workers publications met the inclusion criteria. Countries established and/or increased number of dental schools, 1 university adopted competency-based curriculum and 2 introduced community rotations. Dental auxiliaries varied by cadre, training duration and scope of practice. Non-oral health-care workers training programs used diverse approaches like pre-service, workshops and printed materials. Target groups for the trainings varied from nurses, traditional healers, health promotion officers to community health volunteers. Evaluations were done mainly using pre-post or quasi-experimental studies. Outcomes of interest varied from level of knowledge, services provision, early childhood caries, oral health seeking behavior and oral hygiene practices.
Conclusion
Oral health training for integration of oral health into PHC in sub-Saharan Africa varied by targeted cadre, training methods and evaluation method and scope. It was thus context-reliant. More programs are necessary to accommodate other training approaches, evaluation methods and other health-care cadres in the region.
Introduction
The number of trained oral health-care personnel in sub-Saharan Africa is very low.Citation1 They are also maldistributed with the rural populations being highly underserved.Citation2 Reliance on these oral health personnel to provide services in the whole spectrum of health-care levels is therefore not feasible. Using the common risk factors approach with both oral and non-oral health-care workers is a more cost effective and efficient way to achieve population- wide and patient centered solutions.Citation2 One of the prongs in the common risk factors approach is increasing the number of oral health-care workers trained so as to increase the pool of workers available for service delivery. Oral health workers training curriculum can also be modified to include behavioral science, public health and other health actions to facilitate their involvement in the integration process. Similarly, to equip the non-oral health-care workers on service provision, the WHO Regional Office for Africa recommends the inclusion of aspects of oral health in the curriculum of basic health training programs and, within in-service training of existing doctors, nurses, clinical officers and other health-care workers.Citation2 The training approach, scope and outcomes have, however, been as diverse as the permutations of the training elements. The purpose of this review is to therefore to appraise oral health training programs aimed at integration of oral health into PHC with the aim of synthesizing evidence in the formulation, implementation and evaluation of oral health training programs in sub-Saharan Africa. It will present knowledge to policy makers that would inform planning of future oral health training programs and further the policy debate on the integration of oral health into PHC.
Materials and Methods
The original search was done through various electronic databases: Biomed Central, MEDLINE, Cochrane, NCBI, Google Scholar and WHO sites. Additional articles were identified by reviewing the reference lists and bibliographies of the articles obtained by database searching.
The key words used were: “integration of oral health into primary health care”, “oral health in primary health care”, “oral health training”, “primary oral health care” and other related terms like “dental curriculum”. The titles from the search were scrutinized by the authors to select relevant abstracts which were reviewed for relevant articles to be downloaded. Oral health training programs for oral and non-oral health-care workers in sub-Saharan Africa published in English language between year 2001 and 2020 were included.
All processes that lead to an increase in the number of oral health-care workers were considered as an opportunity to add to the pool available for the integration process. Thus, all publications on training processes aiding in such was considered in the review. Conversely, only training that was aimed at improving oral health-care delivery for non-oral health-care workers was included in the review. This difference in focus necessitated the use of two different pathways for oral and non-oral health-care workers.
Results
The process of source selection and exclusion was based on the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) framework as shown in . The original search on the training for oral health-care workers had 512 publications. Of these, 27 were duplicates and were therefore removed. After screening the titles and the abstracts, a further 385 and 84 publications were eliminated, respectively. A further 27 publications were eliminated after application of the systematic review criteria. Only 4 publications met the inclusion criteria.
Figure 1 Source selection process using PRISMA framework.
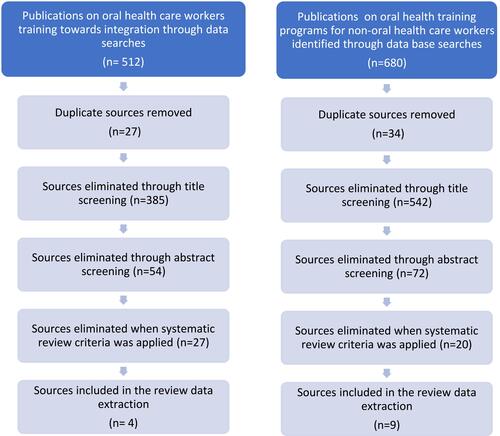
For the non-oral health-care providers training programs, the database searches yielded 680 publications. There were 34 duplicates which were removed. Screening of titles and abstracts eliminated a further 542 and 72 publications, respectively. Of the remaining 29 publications, only 9 met the final criteria for inclusion for data extraction in the systematic review.
Dentists Training
Dentists are trained at undergraduate and post graduate levels at Universities globally, including the sub-Saharan region. It takes an average of six years in undergraduate school and four years in post-graduate school for clinical studies.Citation3 As at the year 2000, only 11 sub-Saharan African countries with 23 dental schools were offering dental training at undergraduate level.Citation4 Currently, there are 16 countries with 35 dental schools in the region. The increased number of dentists has, however, been paralleled by population growth stagnating the net effect on access to oral health care. This is more so with increasing number of underserved populations.Citation2,Citation5
To restructure oral health training to prepare graduates for services in the underserved populations, universities have adopted community-based training for their students.Citation6–Citation9 As outlined in , this has resulted in students having more contact hours in the community and the dental curriculums have been broadened to include behavioral science, public health and other health actions.Citation8,Citation9 The net effect has been an increased willingness by oral health workers to work in the PHC programs; graduates are also better placed to join the PHC team following exposure during training.Citation8,Citation9 The overall aim to increase the dentist to population ratio is, however, not yet achieved.Citation13
Table 1 Oral Health Training Programs for Oral Health Workers
Auxiliary Dental Personnel Training
The need to shift some tasks from the already overstretched dentist workforce prompted the training of auxiliary dental personnel. As at the year 2000, 14 sub-Saharan African countries were training ten different cadres of dental auxiliary personnel.Citation10 These included dental therapist, dental technicians, dental assistants, community oral health officers, dental hygienist, chair side assistants, dental nurses, assistant dental officers, public health dental assistants and dental technologists.Citation10 Training of these auxiliary cadres has continued to date with countries increasing the number of cadres trained as well as the absolute numbers trained.
The auxiliary dental personnel training and roles in oral health care is however country dependent as regulation vary between countries.Citation10 The number of auxiliary oral health personnel is equally low and their distribution is also predominantly urban.Citation2 The need to work with the dentist and referral means the challenge faced by the dentist is mirrored in the auxiliary oral health personnel.
Non-Oral Health Care Workers Training
The aim for training non-oral health-care workers is to enable them offer oral health services as part of their package of care to their clients. outlines oral health training programs in sub-Saharan Africa that were included in the systematic review. Among the non-oral healthcare targeted were the community health workers,Citation11–Citation13 nurses,Citation14–Citation16 clinical officers,Citation16 nutritionistsCitation17 and health promotion officers.Citation18
Table 2 Oral Health Training Programs for Non-Oral Health Workers
Oral health modules were included in training curriculums at pre-service, in-service and other forms of interprofessional education resulting in better understanding of each professionals’ role in provision of oral health services.Citation14,Citation15,Citation18 Educational meetings and workshops that offered both didactic and interactive sessions were also deployed for training the non-oral health-care workers.Citation12,Citation16,Citation19 In two of the programs,Citation16,Citation20 trainers met the health-care workers in their work place in scheduled educational outreaches. Both approaches nonetheless resulted in improved professional practice and health outcomes.Citation16,Citation20 Printed educational materials inform of oral health education materials like flipcharts, posters and clinical guidelines were used to improve health services provision and outcomes in different settingsCitation13,Citation14,Citation16 and, although no study evaluated them independently, the improvement when used in combination with other interventions was significant.Citation13,Citation16 Three programs did not, however, indicate the training interventions used.Citation15,Citation17,Citation21
All but oneCitation18 of the studies included in the systematic review achieved their expected outcomes. Increase level of knowledge in oral health among the non-oral health-care workers was the most reported outcome.Citation14,Citation16,Citation19,Citation22 Other reported outcomes were oral health examination, diagnosis and referral by the non-oral health-care workers.Citation12,Citation14–Citation16 One of the studiesCitation15 reported oral health education being offered as part of routine health education. Placement of atraumatic restorative therapy was also reported in a primary oral health-care program in Gambia.Citation14
Downstream effects of oral health training programs were assessed in only three programs.Citation12,Citation17,Citation21 Improved oral hygiene practices among the targeted population were reported in the three studies. Other outcomes reported were reduced incidences of early childhood cariesCitation17 and, decrease in harmful practices like tooth bud mutilation.Citation17
Discussion
Integration of oral health into PHC is still suboptimal globally.Citation2,Citation5 A large majority of disadvantaged communities have thus been unable to benefit from the aspirations of PHC.Citation2,Citation5 Instead, the vertical system of oral health-care delivery continues to create an even larger disparity in the oral health-care access.Citation2,Citation5 The poorly funded public health systemCitation5,Citation23 creates inadequacy in access to oral health care which inadvertently push the marginalized to seek the more expensive privately oral health care. Poor oral health seeking behavior may then be linked to the poor access and high cost. Patients may also opt to remain with untreated dental diseases affecting their oral health-related quality of life.
Maldistribution of already inadequate oral health providers with urban skew diminishes further the desired oral health care for all.Citation2,Citation24–Citation26 The emerging trend in lifestyle in the rural setups and the increasing prevalence of dental diseases and conditionsCitation27 further highlights the growing need to serve the rural community. More needs to be done therefore to train, attract and retain oral health personnel in integrated programs that seek to alter the imbalance in access.
Oral health training for dentists continues to be insufficient to meet the demand of the growing population.Citation1 The dentist to population ratio is poorer in the rural areas.Citation25,Citation28 Compounded with poor infrastructure, the majority who rely on public health system are left underserved. The effortsCitation4,Citation8 to align the dentist training to the principles of PHCCitation1 have resulted only in marginal success. The dentist is still clinical and peripheral within the PHC system.Citation2 Dental schools thus need to do more to inculcate the promotive and preventive actions in dental training.
Training of auxiliary dental staff is getting global acceptance as sub-Saharan African countries train different auxiliary cadres in oral health.Citation10 Whereas their contribution is irrefutable, their inherent incapacity to function in the absence of the dentist makes it impossible to significantly reduce the absolute workload of the dentist.Citation10 The limited and blurred line in the scope of practice as indicated in for different cadres could also be easily abused especially in settings with poor regulatory and governance structures. Their continued deployment in clinical setupCitation23 could also negate the purpose for which the programs were designed which is to achieve promotive and preventive oral health.
Non-oral health-care workers’ role in oral health care has remained untapped due to structural barriers including training, licensing and practice. Despite the willingness to offer oral health services, insufficient oral health training has led to poor knowledge on oral health and ultimately poor integration of oral health services.Citation27 To mitigate this, training for non-oral health-care workers on their roles in integration is advocated.Citation2 The approaches to oral health training in the region have been diverse.Citation4,Citation14–Citation16,Citation18,Citation19,Citation21,Citation29 While no single approach has failed to offer some positive level of desired outcome, some approaches like printed materials have only been used as supplementary to amplify desired outcomes.Citation16,Citation21 This illustrates that permutations in training approaches application can be used to enhance the effectiveness of a training program. Other combination of approaches, as shown in , demonstrates the multiplicity of option available in training. The difference in targeted groups for training, beneficiaries and the choice of host program depicts the heterogenicity in health-care systems. This further speaks to the contextual nature of health care, and the need to not only adopt but adapt training for the intended group and desired outcomes.
Conclusion
Oral health training is a key component of the integration process of oral health into PHC. Positive outcomes of the hitherto training programs points to the infinite possibilities. Diversity in the structure of the programs underscores the heterogenicity of health-care delivery and confirms that oral health training aimed at integration in sub-Saharan Africa is context-reliant. More programs are necessary to accommodate other training approaches, expand evaluation methods and scope and target other health-care cadres in the region to continue providing new knowledge on integration as well as enrich the policy debates on integration.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
- World Health Organization. Global health workforce statistics database; 2019. Available from: https://www.who.int/data/gho/data/themes/topics/health-workforce. Accessed June 16, 2022.
- World Health Organization. Promoting oral health in Africa; 2016.
- Adeola HA, Adefuye A, Soyele O, Butali A. The dentist-scientist career pathway in Africa: opportunities and obstacles. Korean J Med Educ. 2018;30(3):189–198. doi:10.3946/kjme.2018.93
- Achembong LN, Ashu AM, Hagopian A, Downer A, Barnhart S. Cameroon mid-level providers offer a promising public health dentistry model. Hum Resour Health. 2012;10. doi:10.1186/1478-4491-10-46
- World Health Organization. Oral health services in Europe; 2020. Available from: https://www.euro.who.int/en/health-topics/disease-prevention/oral-health/policy/oral-health-services. Accessed June 16, 2022.
- Morales DV. Las concepciones de curriculum y su importancia en la elaboración de un doctorado curricular en estomatología [The curriculum concepts and its significance in designing of a curricular doctorate in stomatology]. Rev Cubana Estomatol. 2011;48(3). Spanish.
- Bailit HL. Organization and management of community-based dental education programs: an overview from the dental pipeline program. J Dent Educ. 2010;74:S9–S16. doi:10.1002/j.0022-0337.2010.74.10_suppl.tb04976.x
- Ibiyemi O, Taiwo JO, Oke GA. Dental education in the rural community: a Nigerian experience. Rural Remote Health. 2013;13(1). doi:10.22605/rrh2241
- Ngassapa OD, Kaaya EE, Fyfe MV, et al. Curricular transformation of health professions education in Tanzania: the process at Muhimbili University of health and allied sciences (2008–2011). J Public Health Policy. 2012;33(SUPPL.1):S64–S91. doi:10.1057/jphp.2012.43
- Thorpe S. Oral health issues in the African region: current situation and future perspectives. J Dent Educ. 2006;70:8–15. doi:10.1002/j.0022-0337.2006.70.11_suppl.tb04209.x
- Agbor AM, Naidoo S. Knowledge and practice of traditional healers in oral health in the Bui Division, Cameroon. J Ethnobiol Ethnomed. 2011;7. doi:10.1186/1746-4269-7-6
- Rudolph MJ, Ogunbodede EO, Mistry M. Management of the oral manifestations of HIV/AIDS by traditional healers and care givers. Curationis. 2007;30(1). doi:10.4102/curationis.v30i1.1051
- Adeniyi AA, Sofola OO, Kalliecharan R. An appraisal of the oral health care system in Nigeria. Int Dent J. 2012;62(6):292–300. doi:10.1111/j.1875-595X.2012.00122.x
- Jordan AR, Pottbrock M, Gängler P, Zimmer S. [GambiaDentCare - evaluation of a primary oral health-care programme in West Africa]. TT - GambiaDentCare - Evaluierung eines zahnmedizinischen Grundversorgungsprogramms in Westafrika. Gesundheitswesen. 2011;73(12):849–852. doi:10.1055/s-0030-1267944
- Kolisa Y. Assessment of oral health promotion services offered as part of maternal and child health services in the Tshwane Health District, Pretoria, South Africa. Afr J Prim Health Care Fam Med. 2016;8(1). doi:10.4102/phcfm.v8i1.794
- Koyio LN, Van Der Sanden WJM, Dimba E, et al. Oral health training programs for community and professional health care workers in Nairobi East District increases identification of HIV-infected patients. PLoS One. 2014;9(3):e90927. doi:10.1371/journal.pone.0090927
- Muhoozi GKM, Atukunda P, Skaare AB, et al. Effects of nutrition and hygiene education on oral health and growth among toddlers in rural Uganda: follow-up of a cluster-randomised controlled trial. Trop Med Int Health. 2018;23(4):391–404. doi:10.1111/tmi.13036
- Molete MP, Daly B, Hlungwani TM. Oral health promotion in Gauteng: a qualitative study. Glob Health Promot. 2013;20(1):50–58. doi:10.1177/1757975913476906
- Olatosi OO, Oladugba A, Oyapero A, et al. A preexperimental study to assess the impact of an interdisciplinary educational intervention on nurses’ knowledge of perinatal and infant oral health care. J Int Soc Prev Community Dent. 2019;9(6). doi:10.4103/jispcd.JISPCD_144_19
- Jordan RA, Gaengler P, Markovic L, Zimmer S. Performance of Atraumatic Restorative Treatment (ART) depending on operator-experience. J Public Health Dent. 2010;70(3):176–180. doi:10.1111/j.1752-7325.2009.00159.x
- Adeniyi AA, Oyapero A, Ajieroh V, Sofola O, Asiyanbi O. Effect of health education intervention conducted by primary health care workers on oral health knowledge and practices of nursing mothers in Lagos State. J Public Health Africa. 2018. doi:10.4081/jphia.2018.833
- Agbor AM, Naidoo S. A review of the role of African traditional medicine in the management of oral diseases. Afr J Tradit Complement Altern Med. 2016;13(2):133. doi:10.4314/ajtcam.v13i2.16
- Ahluwalia K, Mutave R, Gianfrancesco C, Nicholas S. Summit to address oral health in East Africa: a framework to integrate oral health and health. Columbia University; 2018.
- Ramphoma K. Oral health in South Africa: exploring the role of dental public health specialists. S Afr Dent J. 2016;71(9):402–403.
- Fatusi O, Ogunbodede E, Sowole C, Folayan M. Gaps in oral health-care service provision systems for children in Nigeria: a case study of a tertiary health institution. Indian J Dent Res. 2018;29(5):622. doi:10.4103/ijdr.IJDR_734_16
- Agbor AM, Azodo CC, Naidoo S. The oral health workforce in Cameroon; the past, the present and the future. Afr J Oral Health Sci. 2018;7(2):11. doi:10.4314/ajoh.v7i2.172404
- Okoye L, Ekwueme O. Prevalence of dental caries in a Nigerian rural community: a preliminary local survey. Ann Med Health Sci Res. 2011;1(2):187–196.
- World Health Organization. Oral health services; 2016.
- Ogunbodede EO, Rudolph MJ, Tsotsi NM, Lewis HA, Iloya JI. An oral health promotion module for the primary health care nursing course in Acornhoek, South Africa. Public Health Nurs. 1999;16(5):351–358. doi:10.1046/j.1525-1446.1999.00351.x
- Mumghamba EG. Integrating a primary oral health care approach in the dental curriculum: a Tanzanian experience. Med Princ Pract. 2014;23(1):69–77. doi:10.1159/000355520
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
