Abstract
Purpose
Malnutrition and sarcopenia require dietetic and physiotherapy interventions. In this study, we aimed to compare interprofessional identity of dietitians and physiotherapists, as well as attitudes towards, facilitators and barriers for, and occurrence of interprofessional treatment of malnutrition and sarcopenia by both professions.
Methods
A cross-sectional online survey was distributed from December 4, 2021 until January 31, 2022 through an international online network platform for professionals (LinkedIn). Practitioners working as dietitian or physiotherapist in a healthcare setting were eligible for participation. Outcome measures concerned perceptions regarding shared problem domains, interprofessional treatment, attitudes towards interprofessional treatment, interprofessional identity, facilitators, and barriers. A Chi2-test, Mann–Whitney U-test, and Spearman’s Rho correlation were calculated.
Results
Data from 53 physiotherapists and 48 dietitians were included. Malnutrition is considered a shared problem domain by both professions (U = 1248.000; p = 0.858). While sarcopenia is treated by both professions (U = 1260.000; p = 0.927), physiotherapists consider sarcopenia more often a shared problem domain compared to dietitians (U = 1003.000; p = 0.044). Attitudes towards interprofessional treatment were mostly positive (73%, n = 35 and 87%, n = 46 respectively). Interprofessional identity of dietitians was lower compared to physiotherapists (median = 4.0 versus median = 4.3 respectively; U = 875.000, p = 0.007). This was explained by lower interprofessional belonging (median = 4.0 versus median = 4.8 respectively; U = 771.000, p < 0.001) and lower interprofessional commitment (median = 4.0 versus median = 4.3 respectively; U = 942.500, p = 0.023). Interprofessional identity was correlated with efficient means of communication (r = 0.30, p = 0.003) and bureaucracy (r = −0.21, p = 0.034). Other barriers reported included available time, financial compensation, interprofessional knowledge, and obtaining extra care. Most reported facilitators concerned role clarity, clarity of expertise, and willingness of others to collaborate.
Conclusion
Dietitians and physiotherapists have different interprofessional identities, but both are advocates of interprofessional treatment. Both professions mostly treat malnutrition and sarcopenia individually and have different perceptions regarding sarcopenia as shared problem domain. Facilitators were mainly related to clarity and commitment while barriers were mainly related to resources.
Introduction
In hospital settings, professionals perceive interprofessional collaboration as an important way to link between professions and believe it to be beneficial to patients and to other professions besides their own.Citation1 Home-based care can also be interprofessional but requires different prerequisites.Citation2 Some conditions need early identification to prevent rapid deterioration like malnutrition and sarcopenia. Interprofessional collaboration can lead to sensitization of decision-makers and enables new measures to improve nutritional management.Citation3 However, hardly any research has been conducted on interprofessional practice and nutritional management. Only one paperCitation4 reported on the effectiveness of interprofessional collaboration and practice implementation for older adults with malnutrition compared to usual care. In that study, a collaborative team of primary health care providers consisting of a physician, dentist, nurse, dietitian and pharmacist who provided interprofessional care of malnutrition among older adults, were compared with an untreated control group design. However, this study did not include physical therapists nor combined nutritional and physical exercise interventions. They found that nutritional status of older adults improved significantly better after interprofessional collaboration than after usual care.
Both malnutrition and sarcopenia are conditions commonly present in various health care settings. Malnutrition has been defined as a state resulting from lack of intake or uptake of nutrition that leads to altered body composition (decreased fat-free mass) and body cell mass, leading to diminished physical and mental function and impaired clinical outcome from disease.Citation5 Sarcopenia has been defined as a progressive and generalized skeletal muscle disorder that is associated with increased likelihood of adverse outcomes including falls, fractures, physical disability and mortality.Citation6 Prevalence of malnutrition is estimated to range between 10% and 40% in the hospital setting,Citation7 nearly 10% in community-dwelling older people, and up to 30% in women and 51% in men in nursing homes.Citation8,Citation9 However, prevalence of malnutrition may even be higher in specific patient populations like patients with cancer.Citation10 Prevalence of sarcopenia is estimated to be around 10%.Citation11 With the increasing age that is accompanied by an increase in comorbidities, prevalence rates of malnutrition and sarcopenia are expected to further increase in the upcoming years.
While malnutrition and sarcopenia are distinct conditions,Citation12 both conditions are characterized by deterioration of muscle status. Low muscle mass is an important criterion to diagnose malnutrition,Citation13 while low muscle strength is the primary criterion to diagnose sarcopenia.Citation6 Therefore, both conditions are best treated by combining nutritional and exercise interventions.Citation14 Theoretically, this makes malnutrition and sarcopenia a problem domain shared by dietitians and physiotherapists and the starting point of interprofessional collaboration. A shared problem domain is considered inherent to any kind of collaboration.Citation15 Interprofessional treatment of malnutrition and sarcopenia may prevent delay of care and improve diagnosing and managing these conditions.
Interprofessional collaboration is a policy spearhead of the International Confederation of Dietetic Associations.Citation16 This international confederation states: The more interprofessional education that occurs between medical students, other health professional students, and RDNs (registered dietitian nutritionists), the more likely all health care professionals will understand and value the role of RDNs in improving the quality of care provided to patients.Citation17 Moreover, the World Physiotherapy states: Promote greater interprofessional exchange among health professionals across all stages of patient/client management, namely, examination, evaluation, diagnosis, prognosis, intervention, and follow-up to promote effective streamlined health services delivery.Citation18 Based on definitions of interprofessional work, six factors are important for interprofessional treatment of malnutrition and sarcopenia: 1) shared commitment; 2) shared identity; 3) clear goals; 4) clear team roles and responsibilities; 5) interdependence between team members; and 6) integration between work practices.Citation19 This integration also includes setting interprofessional team goals around achieving equitable care outcomes for, and with, vulnerable populations.Citation20
An approach that recognizes the interaction between infrastructure and human behavior in the practice setting is the Sociotechnical Systems (STS) approach. The Meta-Model of Interprofessional Development is a sociotechnical systems approach to interprofessional collaboration.Citation21–Citation23 This meta-model functions as a theory and evidence-based roadmap that describes the nature, sequence, and interrelatedness of several interprofessional factors when solving a shared problem together. One factor during the preparation for interprofessional work is acquaintance between professions. This can clarify mutual expectations and beliefs. Expectations and beliefs about interprofessional collaboration between dietitians and physiotherapists can, in turn, affect trust,Citation24 respectCitation25,Citation26 and perceptions on added value of interprofessional collaboration.Citation27 Different interprofessional experiences enhance interprofessional identity formation, and teams with high interprofessional identities generate more solutions to shared problems.Citation23 Other factors besides involvement of different disciplines are as follows: role clarity, communication, and information sharing.Citation28 Additional examples of facilitators and barriers are available time, accessibility,Citation27 financial compensation,Citation29 and interprofessional knowledge.Citation30 So far, facilitators and barriers of interprofessional treatment of malnutrition and sarcopenia have not been investigated. Therefore, in this study, we aimed to compare interprofessional identity of dietitians and physiotherapists, as well as their attitudes towards, perceived facilitators and barriers for, and occurrence of interprofessional treatment of malnutrition and sarcopenia by both professions.
Materials and Methods
A cross-sectional online survey was distributed from December 4, 2021 until January 31, 2022, through an international online network platform for professionals (LinkedIn). Network pages of the following organizations were used for survey distribution: Dutch Professional Association of Dietetics (NVD), Dutch Professional Association of Geriatric Physiotherapy (NVFG), FAITH research, a SIA SPRONG public–private network (www.faithresearch.nl), and the Center of Expertise Urban Vitality of the Amsterdam University of Applied Sciences.
Sample and Recruitment
In the Netherlands, about 2.303 dietitiansCitation31 and 35.065 physiotherapistsCitation32 are registered. A convenience sample was obtained through the use of social media. A link to an online survey was placed on websites, together with an explanatory introduction. Potential participants were informed about the inclusion criteria, ie, working as a dietitian or physiotherapist in a healthcare setting. No particular exclusion criteria were formulated. The purpose of the study, ie, interprofessional collaboration between dietitians and physiotherapists to treat malnutrition and sarcopenia, was clarified beforehand. All data were collected through Qualtrics as a survey tool.Citation33
Ethics Approval and Consent to Participate
Since respondents to the survey were not subject to procedures or required to follow rules of behavior, the study was not subject to the Dutch law Medical Research Involving Human Subjects Act (WMO), and therefore, approval by a Medical Ethical Committee was not required. This study was conducted according to the Helsinki Declarations. Participants were informed about the nature of this study by an introduction attached to the online survey, and were asked to participate anonymously, ie, survey links were anonymous. Informed consent was obtained from all respondents before completion of the survey. The answers to all questions were irreducible to personal identities.
Measurement
Demographics
Demographic variables were gender, age, and work setting. Work setting was categorized as follows: primary care (home care setting), secondary care (hospital care), nursing home and rehabilitation, and others.Citation34,Citation35 Nursing home and rehabilitation care was defined as residential or outpatient care of elderly or disabled people aimed at optimizing functioning and reduce disability in individuals with health conditions in interaction with their environment. Also, respondents were asked whether they collaborate with professionals of other work settings. Sample size calculation indicated that 330 responses from dietitians and 381 responses from physiotherapists were needed to have a confidence level of 95% that the real value is within ±5% of the measured/surveyed value.Citation36
Measures
Interprofessional treatment of malnutrition and sarcopenia by dietitians and physiotherapists was measured by several interrelated outcome measures: perceptions regarding shared problem domains (interprofessional) treatment, attitudes towards interprofessional treatment, interprofessional identity, facilitators, and barriers. As visualized in , perceptions of problem domains precede considering initiation of interprofessional treatment. To enable interprofessional treatment, experiences and expectations lead to several attitudes that affect interprofessional identity which, in turn, will predict interprofessional treatment. Interprofessional treatment can be enhanced by facilitators and decreased or even absent when obstructed by barriers.
Figure 1 Overview of measurement outcomes: problem domain, attitudes, interprofessional identity, facilitators, barriers and interprofessional treatment of malnutrition and sarcopenia.
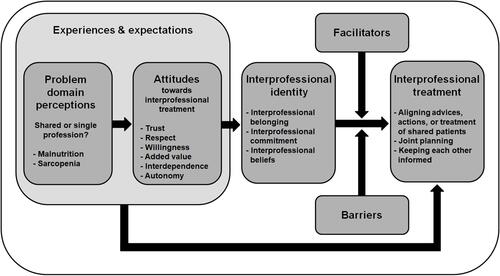
- Interprofessional treatment of malnutrition or sarcopenia was measured by three items: 1) Treatment and interprofessional treatment of each condition, 2) Considering each condition as shared problem domain, and 3) Degree of involvement in dietitian-physiotherapist collaboration with regard to malnutrition or sarcopenia. All items were scored on a 5-point Likert scale: 1 = never; 2 = seldom; 3 = sometimes; 4 = relatively often; 5 = often. Three additional items were added to explore specific actions regarding collaborative treatment of malnutrition and/or sarcopenia. These items were based on the interprofessional work cycle described by the Meta-Model of Interprofessional Development: 1) aligning advices, actions, or treatments of shared patients with malnutrition and/or sarcopenia; 2) degree of joint planning between different professions; and 3) keeping each other informed regarding the progress of a shared patient.Citation21–Citation23
Attitudes towards interprofessional collaboration between dietitians and physiotherapists regarding treatment of malnutrition and sarcopenia were measured with six items. All items concerned trust in expertise of other, respect for the other, willingness to collaborate interprofessional, perceived added value of interprofessional collaboration, perceived interdependence and perceived autonomy. The response format consists of a 5-point Likert scale: 1 = very unimportant; 2 = unimportant; 3 = neutral/no opinion; 4 = important; 5 = very important.
- Interprofessional identity was measured using the Extended Professional Identity Scale (EPIS). This measurement instrument consists of 12 items, three subscales and four items per subscale. In another study, the explained variance of this instrument was 65%. Internal consistency of the overall scale was 0.89, and 0.79, 0.81, and 0.80 of the subscales, respectively. A confirmatory factor analysis confirmed its three-dimensionality and several goodness-of-fit indexes showed positive results.Citation37 Examples of items are as follows: “I like learning about other health professions” (interprofessional belonging), “I prefer working with others in an interprofessional team” (interprofessional commitment), and “All members of an interprofessional team should be involved in goal setting for each patient” (interprofessional beliefs). The response format consists of a 5-point Likert scale: 1 = strongly disagree; 2 = disagree; 3 = neutral/no opinion; 4 = agree; 5 = strongly agree.
- Facilitators and barriers to interprofessional collaboration between dietitians and physiotherapists were measured by asking participants to identify 16 topics derived from an exploratory literature search and informal interviews with four experts on treatment of malnutrition and sarcopenia: role clarity, clarity other expertise, intergroup hierarchy, willingness of others to collaborate interprofessional, efficient means of communication, available time, accessibility, financial compensation, differences in liability, differences in payment and remuneration, interprofessional knowledge, interprofessional skills, interprofessional experience, bureaucratic procedures, clarity about clinical responsibility, obtaining extra care for patient. All items were scored on a 5-point Likert scale ranging from 1 (strong barrier) to 3 (neutral) to 5 (strong facilitator). For analytical purposes, barriers and facilitators were also dichotomized per topic afterwards. Topics were based on a literature exploration.
Data Analysis
All analyses were performed using SPSS Version 23 (IBM). Normal distribution was tested by Kolmogorov–Smirnov test. Descriptive statistics were reported as frequencies (relative frequency: %) for categorical data, mean and standard deviation (SD) for normally distributed data, and median and interquartile range (IQR; Q1–Q3) for not normally distributed data, respectively. Cronbach’s alpha (α) was used to assess the internal consistency of the overall scale and separate subscales of the EPIS. The internal consistency of the scale and subscales is considered sufficient if α > 0.70.Citation38,Citation39 A Chi2-test or Mann–Whitney U-test was used to explore differences between groups (profession, gender, work setting, and low versus high interprofessional identity). Spearman’s Rho correlation was used to investigate the relationship between interprofessional treatment of malnutrition and sarcopenia, interprofessional identity (including its three dimensions), attitudes, facilitators and barriers. In all analyses, statistical significance was set at p<0.05.
Results
In total, 101 practitioners, ie, 53 (53%) Dutch physiotherapist and 48 (48%) Dutch dietitians, responded. All respondents that started filling in the questionnaire fully completed the questionnaire. More dietitians (n = 46; 96%) compared to physiotherapists (n = 42; 79%) were female (Chi2 = 6.180; df = 1, p = 0.013). The average age of dietitians was 42.9 years (SD = 13.1 years) compared to 38.4 years (SD = 10.7 years) of physiotherapists. The majority of both professions worked in primary care (67%; n = 32 and 62%; n = 33, respectively). The two largest subgroups were practitioners working in both primary and secondary care and practitioners working in a nursing home and rehabilitation setting (). Malnutrition is more often treated in nursing homes and rehabilitation centers than in other work settings (U = 517.5, p = 0.043).
Table 1 Demographic Characteristics of Respondents (n = 101)
Interprofessional Treatment of Malnutrition and Sarcopenia
More dietitians than physiotherapists treat patients with malnutrition (U=621.000; p <0.001) even though both dietitians and physiotherapists perceive malnutrition as a shared problem domain (; U=1248.000; p=0.858). Of all professionals from both professions, interprofessional treatment of malnutrition is reported by a minority (Chi2 = 0.001; df = 1; p = 0.981). Half of the dietitians and a majority of physiotherapists often treat patients with sarcopenia (Chi2 = 0.442; df = 1; p = 0.506). Also, a majority of these practitioners perceive sarcopenia as a shared problem domain (Chi2 = 0.638; df = 1; p = 0.424). A minority of dietitians and physiotherapists report frequent interprofessional treatment of sarcopenia (Chi2 = 1.625; df = 1; p = 0.202).
Table 2 Comparing Interprofessional Treatment of Malnutrition and Sarcopenia by Dietitians and Physiotherapists (n = 101)
Attitudes
shows attitudes towards interprofessional collaboration related to treatment of malnutrition and sarcopenia among dietitians and physiotherapists. No significant differences were found in attitudes between dietitians and physiotherapists. A majority of dietitians and physiotherapists felt mutual trust (85% and 91% respectively) and respect (90% and 93% respectively). Moreover, a majority of dietitians (87%) and physiotherapists (89%) held positive attitudes towards interprofessional collaboration. Perceived interdependence was hardly perceived as a barrier nor a facilitator by dietitians and physiotherapists. Perceived autonomy was perceived as a facilitator by a majority of dietitians (54%).
Table 3 Attitudes of Dietitians and Physiotherapists Towards Interprofessional Treatment of Malnutrition and/or Sarcopenia (n = 101)
Interprofessional Identity
The internal consistency of the EPIS in this study was α = 0.86. In addition, the internal consistency of its subscales interprofessional belonging, interprofessional commitment, and interprofessional beliefs was α = 0.90, α = 0.90, and α = 0.80, respectively. No differences were found between overall scale and subscales of interprofessional identity and gender. shows results on interprofessional identity of dietitians and physiotherapists per work setting and per profession. Interprofessional identity of dietitians was lower compared to physiotherapists (U=875.000, p=0.007). The dimension of interprofessional belonging (U=771.000, p<0.001) and interprofessional commitment (U=942.500, p=0.023) were both lower among dietitians compared to physiotherapists. Interprofessional commitment was lower in primary care compared to other work settings (U=885.000; p = 0.040). In professionals working in secondary care, however, interprofessional commitment was higher (U=880.500; p = 0.037) compared to those not working in that setting. For professionals working both in primary and secondary care (U=458.500; p = 0.009) and for those working in a nursing home or rehabilitation work setting (U=436.000; p = 0.010), interprofessional commitment was also higher compared to those not working in those settings. Professionals working in both primary and secondary care had a higher interprofessional identity compared to others (U=516.000; p=0.040).
Table 4 Interprofessional Identity of Dietitians and Physiotherapists per Profession and per Work Setting (n = 101)
Facilitators and Barriers
shows barriers and facilitators of extrinsic antecedents of interprofessional treatment of malnutrition and sarcopenia among dietitians and physiotherapists. Six barriers were identified by a majority of both dietitians and physiotherapists: efficient means of communication, available time, financial compensation, interprofessional knowledge, bureaucratic procedures, and obtaining extra care for the patient. Role clarity, clarity of expertise, and willingness of others to collaborate interprofessional were perceived as three facilitators by the majority of both professions. Physiotherapists perceived role clarity more often as a facilitator than dietitians (Chi2 = 5.102; df = 1; p = 0.024). Even more so, relatively more dietitians perceived this as a barrier (Chi2 = 6.779; df = 1; p = 0.009).
Table 5 Reported Barriers and Facilitators of Interprofessional Treatment of Malnutrition and/or Sarcopenia (n = 101)
Relationships Between Treatment, Identity, Attitudes and Facilitators and Barriers
Being involved in collaborative treatment of malnutrition is strongly associated with being involved in collaborative treatment of sarcopenia (r = 0.69, p < 0.001). This collaborative involvement is associated with aligning advices, actions, or treatment of shared patients with malnutrition or sarcopenia (r = 0.53, p < 0.001 and r = 0.54, p < 0.001 respectively). In addition, collaborative involvement in treatment of malnutrition or sarcopenia is associated with joint planning (r = 0.35, p < 0.001 and r = 0.45, p < 0.001 respectively), and keeping each other informed regarding the progress of a shared patient (r = 0.41, p < 0.001 and r= 0.40, p < 0.001 respectively).
As reported above, dietitians have slightly lower interprofessional identities compared to physiotherapists. Of all three dimensions of interprofessional identity, interprofessional belonging and interprofessional commitment were lower. For this reason, low and high interprofessional belonging were compared to explore differences with regard to interprofessional treatment to analyse potential relevance of this former finding. Professionals with low interprofessional belonging reported less alignment of advices, actions, or treatments of shared patients with malnutrition and/or sarcopenia (U = 927.000; p = 0.014). This is also the case for the degree of joint planning (U = 897.500; p = 0.009) and keeping each other informed (U = 911.000; p = 0.011). Yet, no differences were found with regard to low versus high interprofessional commitment and these same aspects of interprofessional treatment of malnutrition and sarcopenia.
Professionals with a high interprofessional identity reported more facilitators (M = 7.9; SD = 2.9) than barriers compared to professionals with a low interprofessional identity (M = 6.5; SD = 2.8; t (99) = −2.407, p = 0.018). No difference was found with regard to high versus low interprofessional identity and number of reported barriers (M = 7.4; SD = 3.3 versus 6.8; SD = 2.7 respectively; t (99) = −1.066; p = 0.289). Even though the number of reported facilitators are associated with interprofessional identity, only the number of reported barriers are associated with involvement in dietitian-physiotherapist collaboration (r = −0.29, p = 0.003). The efficiency of the means of communication was positively associated with interprofessional identity (r = 0.30, p = 0.003). Efficient means of communication was also associated with two dimensions of interprofessional identity: interprofessional belonging (r = 0.21, p = 0.035) and interprofessional commitment (r = 0.31, p = 0.001). Interprofessional skills was negatively associated with interprofessional identity (r = −0.23, p = 0.19) and with interprofessional beliefs (ie, a dimension of interprofessional identity) (r = −0.21, p = 0.31). Bureaucracy was associated with interprofessional identity (r = −0.21, p = 0.034) and associated with the dimension interprofessional belonging (ie, a dimension of interprofessional identity; r = −0.33, p = 0.001). Interprofessional identity was somewhat associated with interprofessional treatment of malnutrition and sarcopenia: the degree of aligning advices, actions, or treatment of shared patients with malnutrition and/or sarcopenia (r = 0.22, p = 0.030), joint planning (r = 0.21; p = 0.035) and keeping each other informed (r = 0.22; p = 0.31).
Discussion
This is the first study exploring interprofessional treatment of malnutrition and sarcopenia by dietitians and physiotherapists. The results of this study show that perceptions regarding shared problem domains can differ between these professions. However, dietitians and physiotherapists are both advocates of interprofessional collaboration. The same facilitators and barriers for interprofessional treatment of malnutrition and sarcopenia were reported by the majority of both professions, except for role clarity.
Our findings show that malnutrition is mostly treated by dietitians, while sarcopenia is more often treated by physiotherapists. Perhaps some dietitians and physiotherapists, other professions and/or patients are inclined to associate malnutrition more with dietetics and sarcopenia more with physiotherapy. While health care professionals understand the etiology of malnutrition, screening for malnutrition is not routine in many practices.Citation40 The Meta-Model of Interprofessional DevelopmentCitation21–Citation23 theorizes that professional identity also includes perceptions on professional relevance of problem domains and determines professional engagement as well as the application of relevant professional competencies. In other words, professional identity is a meta-competence and a prerequisite of interprofessional collaboration, which guides professional contributions.Citation41–Citation44 Therefore, the professional identities of both professions regarding treatment of malnutrition and sarcopenia need further investigation.
The results of this study suggest that the willingness of dietitians and physiotherapists towards interprofessional collaboration and interprofessional treatment of malnutrition and sarcopenia is strong. Both attitudes and interprofessional identity were generally positive and high among a majority of the participants in this study. Yet, most of these respondents were hardly involved in interprofessional collaboration. It is not likely that the relatively lower interprofessional identity of dietitians can fully explain this. First, the interprofessional identities of dietitians and physiotherapists were both high. Second, even though the lower interprofessional identity of dietitians can be explained by a lower interprofessional belonging, its relationship with alignment of advices, actions, or treatments of shared patients with malnutrition and/or sarcopenia was not very strong. Therefore, the lack of interprofessional treatment is likely to be explained by several factors. Third, no differences were found between dietitians and physiotherapists with regard to interprofessional beliefs, and both seem high. On the other hand, interprofessional commitment of dietitians was relatively lower compared to physiotherapists, but was still high. Commitment is a stronger predictor of behavior compared to attitude and both are different constructs.Citation45 So far, it is not clear what specific interprofessional behaviors interprofessional identity can predict with regard to interprofessional treatment of malnutrition and sarcopenia. Nevertheless, attitude can change quickly and refers to a favorable or unfavorable evaluation of an entity,Citation46 while commitment can influence behavior in the long term and even in the absence of positive attitudes.Citation47,Citation48 The importance of commitment is also reported in other studies on interprofessional collaboration.Citation20 A shared commitment and shared identity are reported as two of six important enablers of interprofessional collaboration. However, based on several psychological theories and evidence, commitment is a dimension of a social identity.Citation49–Citation52 Thus, interprofessional commitment is part of interprofessional identity and determines the relatively sustainable willingness to work or learn interprofessional.Citation53
The finding that interprofessional identity is related to reporting more facilitators rather than barriers to interprofessional treatment of malnutrition and sarcopenia could be explained by the effect of positive attitudes derived from success experiences. Even more so, attitudes play an important role in the process of identity formation.Citation54 Thus, facilitators could enhance interprofessional collaboration indirectly through interprofessional identity formation. Role clarity, clarity of expertise, and perceived added value of interprofessional treatment of malnutrition and sarcopenia should be facilitated.
According to our findings, interprofessional treatment of malnutrition and sarcopenia is positively associated with interprofessional identity and negatively with the number of reported barriers, but not with number of reported facilitators. Based on this and the findings mentioned above, clues are provided on the roles of facilitators and barriers in the occurrence of interprofessional treatment of malnutrition and sarcopenia. Facilitators seem to enhance interprofessional treatment indirectly through interprofessional identity, while barriers seem to reduce interprofessional treatment directly.
In our study, dietitians and physiotherapists reported their degree of involvement in dietitian-physiotherapist collaboration. However, collaboration between professions does not always concern interprofessional collaboration.Citation55 Yet, it seems this involvement did concern interprofessional collaboration, since moderate to strong correlations were found between involvement in dietitian-physiotherapist collaboration and specific actions related to alignment of different professional services.
Based on the findings of this study, several recommendations can be made. First, it is recommended to increase interprofessional knowledge of dietitians and physiotherapists. This can be increased by using a model that can complement the regular infrastructure, clarifies procedural implications, and aligns priorities for development of collaborative practice.Citation16 The Meta-Model of Interprofessional DevelopmentCitation21–Citation23 was specifically designed to support development of interprofessional practice and education by professionals. It provides a prioritization of interrelated factors that are subject of co-creation by all to whom this may concern. Second, efficient means of communication and improved coping with bureaucracy are likely to positively affect available time and obtaining extra care, possibilities to improve these aspects need to be further explored. Third, possibilities for financial compensation of interprofessional work should be explored and tested in practice. When the urgency of interprofessional treatment of malnutrition and sarcopenia is recognized by health insurers and other institutions that allocate funding, an interprofessional financial infrastructure can be designed to stimulate and improve health through interprofessional collaboration. Finally, interprofessional identity formation should be facilitated by enabling more interpersonal contact between dietitians and physiotherapists. Both a sense of belonging as well as commitment are predicted by interpersonal contactCitation56 A sense of belonging affects team member participation in terms of intentions to exchange knowledge.Citation57 Also, facilitating social processes can increase commitment to interprofessional collaboration. The willingness of others to collaborate is conditional on commitment balance. Commitment balance occurs when individual commitment to a group or social category is perceived to be reciprocated by the commitment of others.Citation58 This may further enhance individual commitment. Interpersonal contact between dietitians and physiotherapists should also be organized in such a way that they will get more acquainted with each other’s roles (role clarityCitation16,Citation59,Citation60) and expertise (clarity of expertiseCitation16,Citation59,Citation61). This can simultaneously clarify role overlap and common ground.Citation62,Citation63
Limitations
The current study has some limitations. Firstly, the sample size was relatively small. This makes it more difficult to generalize findings to the populations of dietitians and physiotherapists. Yet, a sample size of 20 to 150 participants may suffice for an exploratory study.Citation64 Nevertheless, the findings of this study provide clues on how interprofessional treatments of malnutrition and sarcopenia are facilitated or obstructed. Also, the facilitators and barriers explored were derived from studies performed among other professions and work settings. Thus, it seems some of these antecedents do have a more general relevance. The latter is also supported by the finding that the majority of dietitians and physiotherapists report similar facilitators and barriers.
Secondly, a convenience sample was used. A disadvantage of a convenience sample is that the findings of this study cannot be generalized to the target populations of dietitians and physiotherapists. Some subgroups of dietitians and physiotherapists might be under-represented. To investigate potential generalizability of findings to the two professional populations, it would be interesting to also include other demographic measures like qualification and years of experience. On the other hand, it is useful to gain more understanding of interprofessional treatment of malnutrition and sarcopenia by both professions. In addition, participants in this study did work in several work settings and did report similar facilitators and barriers. Also, our findings do reveal interesting relationships that are consistent with other findings regarding interprofessional identity of dietitians. A study regarding interprofessional identity among Lithuanian dietetic students and practitioners reported that their interprofessional identity was also lower compared to members of other disciplines. Just like the findings in this study, that difference was also explained by a lower interprofessional belonging.Citation65 This lower interprofessional belonging might be related to the professional identity of the dietitian, but this has never been investigated. Professional beliefs of dietitians could be based on social positioning outside the health professions category. If so, this could explain why their interprofessional belonging is lower compared to other dimensions of their interprofessional identity.
Thirdly, in this study, we did not analyse perceptions of professionals who do and do not work interprofessionally. Comparing this would be highly informative. However, the subgroup of those involved in interprofessional collaboration was too small for analysis. Comparison of perceptions and outcomes related to interprofessional versus non-interprofessional treatment of malnutrition or sarcopenia by dietitians and physiotherapists are not investigated yet. For this reason, we would recommend more research to specifically explore this.
Fourthly, a limitation of this study is that attitudes, barriers and facilitators were related to both malnutrition and sarcopenia without making a specific distinction between both conditions. This may have affected responses to the questions. Since physiotherapists perceive sarcopenia more as a shared problem domain compared to dietitians, this would make attitudes of dietitians towards interprofessional treatment of sarcopenia potentially less positive compared to physiotherapists making it also less likely they would be open to interprofessional treatment in collaboration with physiotherapists.
Fifthly, this study was limited to investigating the interprofessional treatment of two specific conditions treated by dietitians and physiotherapists. However, these disciplines do share more problem domains than just malnutrition and sarcopenia. Other examples of shared problem domains are chronic congestive heart failureCitation66 and cystic fibrosis‐related diabetes.Citation67
Conclusions
The results of this study show that dietitians and physiotherapists have different interprofessional identities, but both are advocates of interprofessional treatment. Both professions mostly treat malnutrition and sarcopenia individually and have different perceptions regarding sarcopenia as shared problem domain. Facilitators were mainly related to clarity and commitment while barriers were mainly related to resources. Most reported facilitators of interprofessional treatment of malnutrition and sarcopenia concerned role clarity, clarity of expertise, and willingness of others to collaborate. The most reported barriers were inefficient means of communication, bureaucracy, available time, financial compensation, interprofessional knowledge, and obtaining extra care.
The findings of this study are of clinical importance to clinicians and patients. Even though different clinicians and health professionals can treat the same conditions like malnutrition and sarcopenia, perceptions on shared problem domains might differ between professions. This is also relevant to patients who might not always be aware that interprofessional treatment of malnutrition and sarcopenia is likely to improve their health. To researchers it is interesting that interprofessional identity of different professionals is not always the same and that this might be related to factors typical for a particular profession. It should be explored how professional identity of dietitians might be related to such differences that are possibly culture independent. Finally, identified facilitators and barriers can provide handles for both health professions as well as researchers to enhance interprofessional collaboration and decrease factors that obstruct this.
Disclosure
The authors report no conflicts of interest in this work.
References
- Webster F, Bremner S, Jackson M, Bansal V, Sale J. The impact of a hospitalist on role boundaries in an orthopedic environment. J Multidiscip Healthc. 2012;5:249–256. doi:10.2147/JMDH.S36316
- Moe A, Brataas HV. Interdisciplinary collaboration experiences in creating an everyday rehabilitation model: a pilot study. J Multidiscip Healthc. 2016;9:173–182. doi:10.2147/JMDH.S103696
- Braun B, Grünewald M, Adam-Paffrath R, et al. Impact of interprofessional education for medical and nursing students on the nutritional management of in-patients. GMS J Med Educ. 2019;36(2):Doc11. doi:10.3205/zma001219
- Mawardi F, Lestari AS, Kusnanto H, Sasongko EPS, Hilmanto D. Effectiveness of collaboration in older adults: do interprofessional teams improve nutritional status more compared to usual care? Fam Prac. 2022;39(1):32–37. doi:10.1093/fampra/cmab052
- Cederholm T, Barazzoni R, Austin P, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr ESPEN. 2017;36(1):49–64. doi:10.1016/j.clnu.2016.09.004
- Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Writing group for the European working group on sarcopenia in older people 2 (EWGSOP2), and the extended group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi:10.1093/ageing/afy169
- Kruizenga H, van Keeken S, Weijs P, et al. Undernutrition screening survey in 564,063 patients: patients with a positive undernutrition screening score stay in hospital 1.4 d longer. Am J Clin Nutr. 2016;103(4):1026–1032. doi:10.3945/ajcn.115.126615
- Leij-Halfwerk S, Verwijs MH, van Houdt S, et al. MaNuEL Consortium. Prevalence of protein-energy malnutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults ≥65 years: a systematic review and meta-analysis. Maturitas. 2019;126:80–89. doi:10.1016/j.maturitas.2019.05.006
- Papadopoulou SK, Tsintavis P, Potsaki G, Papandreou D. Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. a systematic review and meta-analysis. J Nutr Health Aging. 2020;24(1):83–90. doi:10.1007/s12603-019-1267-x
- Arends J, Baracos V, Bertz H, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr ESPEN. 2017;36(5):1187–1196. doi:10.1016/j.clnu.2017.06.017
- Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. 2017;16(1):21. doi:10.1186/s40200-017-0302-x
- Cao L, Morley JE. Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM). J Am Med Dir Assoc. 2016;17(8):675–677. doi:10.1016/j.jamda.2016.06.001
- Cederholm T, Jensen GL, Correia MITD. et al; GLIM core leadership committee; GLIM working group. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. Clin Nutr ESPEN. 2019;38(1):1–9. doi:10.1016/j.clnu.2018.08.002
- Damanti S, Azzolino D, Roncaglione C, Arosio B, Rossi P, Cesari M. Efficacy of nutritional interventions as stand-alone or synergistic treatments with exercise for the management of sarcopenia. Nutrients. 2019;11(9):1991. doi:10.3390/nu11091991
- Wood DJ, Gray B. Toward a comprehensive theory of collaboration. J Appl Behav Sci. 1991;27(2):139–162. doi:10.1177/0021886391272001
- Hark LA, Deen D. Position of the academy of nutrition and dietetics: interprofessional education in nutrition as an essential component of medical education. J Acad Nutr Diet. 2017;117(7):1104–1113. doi:10.1016/j.jand.2017.04.019
- Kris-Etherton PM, Akabas SR, Bales CW, et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutr. 2014;99(suppl):1153S–1166S. doi:10.3945/ajcn.113.073502
- Dean E, Al-Obaidi S, De Andrade AD, et al. The first physical therapy summit on global health: implications and recommendations for the 21st century. Physiother Theory Pract. 2011;27(8):531–547. doi:10.3109/09593985.2010.544052
- Xyrichis A, Reeves S, Zwarenstein M. Examining the nature of interprofessional practice: an initial framework validation and creation of the InterProfessional Activity Classification Tool (InterPACT). J Interprof Care. 2018;32(4):416–425. doi:10.1080/13561820.2017.1408576
- Carey MJ, Taylor M. The impact of interprofessional practice models on health service inequity: an integrative systematic review. J Health Organ Manag. 2021;35(6):682–700. doi:10.1108/JHOM-04-2020-0165
- Reinders JJ Task shifting, interprofessional collaboration and education in Oral Health Care. PhD thesis. Groningen: University of Groningen; 2018.
- Reinders JJ, Pesut DJ, Brocklehurst P, Paans W, van der Schans CP. Meta-model of interprofessional development. An overarching model that connects requirements for interprofessional practice and education. In: Utley J, Mathena C, Gunaldo T, editors. Interprofessional Education and Collaboration. An Evidence-Based Approach to Optimizing Healthcare. Champaign, USA: Human Kinetics; 2020:177–178.
- Reinders JJ, Pesut DJ. A meta-model for transforming interprofessional practice, education, and research. In: Joosten-Hagye D, Khalili H, editors. Interprofessional Education and Collaborative Practice – International Approaches at the Micro, Meso, and Macro Levels. San Diego, USA: Cognella Academic Publishing; 2022.
- Evans JL, Henderson A, Johnson NW. Interprofessional learning enhances knowledge of roles but is less able to shift attitudes: a case study from dental education. Eur J Dent Educ. 2012;16(4):239–245. doi:10.1111/j.1600-0579.2012.00749.x
- Siegler E, Whitney FW.What is collaboration? In: Siegler E, Whitney FW, editors. Nurse - Physician Collaboration: Care of Adults and the Elderly. Springer: 3–10.
- Jones L, Way DO. Is there room for both NPs and MDs. In a community health centre. In: Patterson C, editor. Visions and Voices: The Nurse Practitioner Today. Troy, Ontario: New Grange Press; 1999:112–28.
- Reymond L, Mitchell G, McGrath B, Welch D. Research into the educational, training and support needs of general practitioners in palliative care. Report to the Department of Health and Ageing. Brisbane: Mt Olivet Health Services; 2003.
- Yinusa G, Scammell J, Murphy J, Ford G, Baron S. Multidisciplinary provision of food and nutritional care to hospitalized adult in-patients: a scoping review. J Multidiscip Healthc. 2021;14:459–491. doi:10.2147/JMDH.S255256
- Tsakitzidis G, Van Royen P. Leren Interprofessioneel Samenwerken in de Praktijk. Antwerpen: Standaard uitgeverij; 2008.
- Rhee JJ, Zwar N, Vagholkar S, Dennis S, Broadbent AM, Mitchell G. Attitudes and barriers to involvement in palliative care by Australian urban general practitioners. J Palliat Med. 2008;11(7):980–985. doi:10.1089/jpm.2007.0251
- ZorgkaartNederland. Available from: https://www.zorgkaartnederland.nl. Accessed April 12, 2022.
- FysioFacts; 2021. Available from: https://www.kngf.nl. Accessed April 12, 2022.
- Sue VM, Ritter LA. Conducting Online Surveys. 2nd ed. Thousand Oaks, CA: Sage Publications; 2012.
- World Health Organization/Europe. Available from: https://www.euro.who.int/. Accessed March 31, 2022.
- National Caregivers Library. Available from: http://www.caregiverslibrary.org/. Accessed March 31, 2022.
- Kadam P, Bhalerao S. Sample size calculation. Int J Ayurveda Res. 2010;1(1):55–57. doi:10.4103/0974-7788.59946
- Reinders JJ, Lycklama À, Nijeholt M, Van Der Schans CP, Krijnen WP. The development and psychometric evaluation of an interprofessional identity measure: extended Professional Identity Scale (EPIS). J Interprof Care. 2020;1–13. doi:10.1080/13561820.2020.1713064
- Nunnally J. Psychometric Theory. New York, USA: McGraw-Hill; 1978.
- Nunnally J, Bernstein JC. Psychometric Theory. McGraw-Hill; 1994.
- Mawardi F, Lestari AS, Kusnanto H, Sasongko EPS, Hilmanto D. Malnutrition in older adults: how interprofessional teams see it? A systematic review of the qualitative research. Fam Pract. 2021;38(1):43–48. doi:10.1093/fampra/cmaa091
- Savickas ML. Career Counseling. Washington DC: American Psychological Association; 2011.
- Owens TJ, Robinson DT, Smith-Lovin L. Three faces of identity. Annu Rev Sociol. 2010;36(1):477–499. doi:10.1146/annurev.soc.34.040507.134725
- Ashforth BE, Kreiner GE. “How can you do it?”: dirty work and the challenge of constructing a positive identity. Acad Manage Rev. 1999;24:413–434.
- Kelly C. Group identification, intergroup perceptions and collective action. Eur Rev Soc Psychol. 1993;4(1):59–83. doi:10.1080/14792779343000022
- Meyer JP, Herscovitch L. Commitment in the workplace: towards a general model. Hum Resour Manag Rev. 2001;1:299–326.
- Eagly AH, Chaiken S. The Psychology of Attitudes. Fort Worth, TX: Harcourt Brace Jovanovich; 1993.
- Hertweck ML, Hawkins SR, Bednarek ML, Goreczny AJ, Schreiber JL, Sterrett SE. Attitudes toward interprofessional education: comparing physician assistant and other health care professions students. J Physician Assist Educ. 2012;23:8–15. doi:10.1097/01367895-201223020-00003
- Matziou V, Vlahioti E, Perdikaris P, Matziou T, Megapanou E, Petsios K. Physician and nursing perceptions concerning interprofessional communication and collaboration. J Interprof Care. 2014;28(6):526–533. doi:10.3109/13561820.2014.934338
- Turner JC. A self-categorization theory. In: Turner JC, Hogg MA, Oakes PJ, Reicher SD, Wetherell MS, editors. Rediscovering the Social Group: A Self-Categorization Theory. Oxford, England: Blackwell; 1987:42–67.
- Turner JC. Some current issues in research on social identity and self-categorization theories. In: Ellemers N, Spears R, Doosje B, editors. Social Identity. Oxford, England: Blackwell; 1999:6–34.
- Barbour JB, Lammers JC. Measuring professional identity: a review of the literature and a multilevel confirmatory factor analysis of professional identity constructs. J Prof Organ. 2015;2:38–60.
- Beal DJ, Cohen R, Burke MJ, McLendon CL. Cohesion and performance in groups: a meta-analytic clarification of construct relation. J Appl Psychol. 2003;88:989–1004. doi:10.1037/0021-9010.88.6.989
- Reinders JJ, Krijnen WP, Goldschmidt AM, van Offenbeek MAG, Stegenga B, van der Schans CP. Changing dominance in mixed profession groups: putting theory into practice. Eur J Work Organ. 2018;27(3):375–386. doi:10.1080/1359432X.2018.1458712
- Brown RB. Organizational commitment: clarifying the concept and simplifying the existing construct typology. J Vocat Behav. 1996;49(3):230–251. doi:10.1006/jvbe.1996.0042
- Headrick LA, Wilcock M, Batalden B. Interprofessional working and continuing medical education. BMJ. 1998;316(7133):771–774. doi:10.1136/bmj.316.7133.771
- Dávila MC, García GJ. Organizational identification and commitment: correlates of sense of belonging and affective commitment. Span J Psychol. 2012;15(1):244–255. doi:10.5209/rev_SJOP.2012.v15.n1.37316
- Zhao L, Lu Y, Wang B, Chau PYK, Zhang L. Cultivating the sense of belonging and motivating user participation in virtual communities: a social capital perspective. Int J Inf Manage. 2012;32(6):574–588. doi:10.1016/j.ijinfomgt.2012.02.006
- Cownie F. What drives students’ affective commitment towards their university? J Furth High Educ. 2019;43(5):674–691. doi:10.1080/0309877X.2017.1394988
- Martin D, Weeres A. Building nursing role clarity on a foundation of knowledge and knowledge application. Healthc Manage Forum. 2016;29(3):107–110. doi:10.1177/0840470416633237
- Allen J, Ottmann G, Roberts G. Multi-professional communication for older people in transitional care: a review of the literature. Int J Older People Nurs. 2013;8(4):253–269. doi:10.1111/j.1748-3743.2012.00314.x
- Eley DS, McAllister L, Chipchase L, Strong J, Allen S, Davidson B. Health professions as distinct cultures in interprofessional, intercultural clinical placements: a pilot study exploring implications for interprofessional supervision. Int J Pract Based Learn Health Soc Care. 3(1):108–118.
- Julkunen IHG, Willumsen E. Professional boundary crossing and interprofessional knowledge development. In: Blom B, Evertsson L, Perlinski M, editors. Social and Caring Professions in European Welfare States: Policies, Services, and Professional Practices. Bristol: Policy Press; 2017:115–13053.
- Teräs M. Inter-professional working and learning: instructional actions and boundary crossing or boundary making in oral healthcare. J Educ Work. 2016;29(5):614–636. doi:10.1080/13639080.2014.997680
- Daniel J. Choosing the size of the sample. In: Daniel J, editor. Practical Guidelines for Making Sampling Choices. Thousand Oaks: SAGE Publications; 2012:236–253.
- Reinders JJ, Tamulienė T, Krijnen WP, Piščalkienė V, Navickienė L, Krasuckienė D. Enabling worldwide research on interprofessional identity: Lithuanian translation and psychometric evaluation of an interprofessional identity scale: EPIS-LT. Health, Interprofessional Practice and Education; 2022.
- Colonna P, Sorino M, D’Agostino C, et al. Nonpharmacologic care of heart failure: counseling, dietary restriction, rehabilitation, treatment of sleep apnea, and ultrafiltration. Am J Cardiol. 2003;91(9A):41F–50F. doi:10.1016/S0002-9149(02)03337-4
- Middleton PG, Wagenaar M, Matson AG, et al. Australian standards of care for cystic fibrosis‐related diabetes. Respirology. 2014;19(2):185–192. doi:10.1111/resp.12227
