Abstract
The global pandemic of coronavirus disease 2019 (COVID 19) is reported to have started in Wuhan City, Hebei Province, China. It has spread rapidly all over the world, including Saudi Arabia, having a severe health emergency. This new virus was named as the 2019 novel coronavirus (2019-nCoV), and now severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) based on previous practice and phylogenetic and taxonomic investigations. SARS-CoV-2 belongs to the family of Coronaviridae, Betacoronavirus, Sarbecovirus subgenus, genome β. Throughout the COVID 19 pandemic, several strains of SARS-CoV-2 have been recognized around the world. The SARS-CoV-2 variants have caused significant morbidity and mortality worldwide and in Saudi Arabia as well. The rate at which COVID-19 spread across borders and affected countries has highlighted the significance of health care systems to nations and global operations. This review focuses on the origin, epidemiology, pathophysiology, transmission, and the impact of this disease, while highlighting the knowledge about SARS-CoV-2 variants.
Introduction
The coronavirusdisease 2019 (COVID-19), the fifth pandemic following the 1918 Spanish flu pandemic (H1N1), has spread worldwide.Citation1 A widespread outbreak of COVID-19 began in China in December 2019 for the first time. The World Health Organization (WHO) called the virus; the infectious disease coronavirus disease 2019 (COVID-19).Citation2 SARS-CoV-2 (acute respiratory syndrome coronavirus 2) is likely to have been transmitted from animal hosts into humans and then adapted to become transmissible between humans. The disease caused by SARS-CoV-2 has turned out to be an unprecedented global health problem in the history of humanity; it has caused the disturbance of social life for billions of human population and also causing mortality of more than 2.5 million people within one year.Citation1 The COVID-19 virus is highly infectious, contributing to its rapid widespread, reaching pandemic levels. The most common symptoms exhibited by COVID-19 patients include high fever, chills, cough, and shortness of breath or difficulty in breathing. The infected people may also present with other symptoms such as diarrhea, myalgia, fatigue, expectoration, and hemoptysis.Citation3
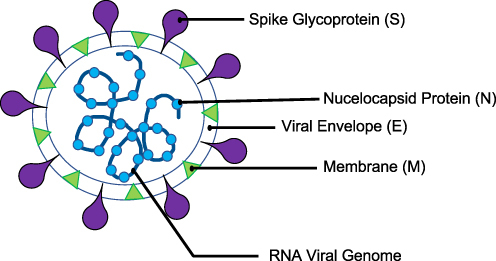
COVID-19 virus or SARS-CoV-2 is a positive-stranded RNA virus with an envelope and glycoprotein spikes, and its particles are elliptic or rounded. SARS-CoV-2 recorded diameter ranges between 60nm to 140nm with spikes of 9nm to 12nm ().Citation4 COVID-19 adds to six coronaviruses that have previously infected humans, which are HCoV-229E, SARS-CoV, HCoV-NL63, HCoV-OC43, HCoV-HKU1, and MERS-CoV. Research has established that COVID-19 has an 88–89% resemblance to two severe acute respiratory syndrome- (SARS-) coronaviruses with bat origins, namely bat-SL-CoVZXC21 and bat-SL-CoVZC45. SARS-CoV-2 has a 79% resemblance with SARS-CoV and 50% similarity with MERS-CoV.Citation2
Pathogenic Mechanism
The SARS-CoV-2 virus penetrates a host cell via the S spike protein after attaching to the host receptor, the angiotensin converting enzyme 2 (ACE2), to prepare for internalization with the help of TMPRSS2 protease.Citation5–7 The virus has high infectivity due to the numerous mutations in its receptor-binding domain and the development of a furan cleavage site in its S spike protein. Once After the virus comes into contact with the ACE2, it inhibits the anti-inflammatory function and increases angiotensin II properties.Citation8 When the virus invades the myocytes, lung cells, and endothelial cells (found in the vascular system), it causes inflammatory alterations such as necrotic, oedema, and degeneration changes. The inflammatory changes are mostly associated with proinflammatory cytokines such as granulocyte colony-stimulating factor (G-CSF), macrophage inflammatory protein 1α (MIP-1α/CCL3), T-cell immunoglobulin (Tim), interleukin (IL)-6 and IL-10, mucin domain 3 (Tim-3), tumor necrosis factor α (TNF-α), monocyte chemoattractant protein 1 (MCP-1/CCL2), and increased expression of programmed cell death 1 (PD-1).Citation9 The alterations caused hypoxia-related myocyte injury, increased damage of myocardial cells, lung injury pathogenesis, body immune response, and cardiopulmonary and intestinal alterations. These changes cause accumulation of lactic acid, changes in intracellular pH, the buildup of oxygen free radicals, cellular damage, and electrolyte changes.
SARS-CoV-2 Variants
Viruses mutate with time, and SARS-CoV-2 is no exception. Since the outbreak of COVID-19, variants of the virus have been responsible for abnormal health incidents.Citation10 WHO closely monitors variants of COVID-19 to determine if there are significant changes in the severity of symptoms, transmission rates, clinical presentation, and possible effects on control measures such as therapeutics, diagnostics, and vaccines. Notable variations include the earlier D614G mutation and more recent variants reported in Denmark, United Kingdom (UK), South Africa, and Northern Ireland.
The D614G (glycine for aspartic acid substitution) variant of the SARS-CoV-2 was first reported around February 2020. This D614G variant became the prevalent version of the virus globally and it was linked to increased severity of the disease and higher mortalities across Europe.Citation11–13 There are no findings to support changes in the efficiency of diagnostics, therapeutics, public health-protective measures, and vaccines for the D614G strain in relation to the SARS-CoV-2. Between August and September 2020 in Jutland, Denmark, Danish authorities discovered a SARS-CoV-2 variant originating from farmed minks named “Cluster 5”.Citation14 Cluster 5 variant is thought to exhibit lower virus neutralization and cause low immune protection after infection or vaccination. The Cluster 5 variant did not spread much due to drastic containment measures, and there were only 12 confirmed human infections reported in Denmark.
SARS-CoV-2 variant of concern (VOC) 202012/01 or 20I/501Y.V variant, (also known as SARS-CoV-2 variant B.1.1.7), was reported in the UK on 14 December 2020. This variant has 23 nucleotide substitutions, and it has phylogenetic differences with the initial SARS-CoV-2 virus dominant in the country at the time and was temporally associated with an increase in regional infections.Citation15,Citation16 Its origins are still undetermined. SARS-CoV-2 variant B.1.1.7 was first reported in South East England but rapidly became dominant in London.Citation17,Citation18 This variant has been detected in samples from the UK. SARS-CoV-2 VOC 202012/01 has been found to poses higher transmissibility, with 50–75 more transmissible over wild-type strain.Citation15–17,Citation19 However, the underlying mechanism for the enhanced transmissibility is unclear. In addition, there are no changes in the severity of the disease or reinfection rate compared to other variants found in the UK.
More than a dozen mutations compared with other circulating strains have been reported in the SARS-CoV-2 variant B.1.1.7. B.1.1.7 features multiple mutations in the spike protein receptor-binding domain,Citation20 that may enhance ACE2 binding 2.Citation21 One of the mutations in this variant, N501Y, is in the receptor-binding region of the spike protein and increased SARS-CoV-2 infectivity in a mouse model.Citation22,Citation23 A further spike protein mutation in the variant, P618H, is immediately adjacent to the furin cleavage site in spike, which seems to have a role in SARS-CoV-2 cell entry.Citation24 Another mutation of this variant is a deletion in the spike protein at amino acid positions 69–70 (deletion ∆H69/∆V70), which is linked to immune escape in immunocompromised patients, and enhances viral infectivity in vitro.Citation25,Citation26 This deletion variant is noted to affect the results from PCR assays targeting the S gene (which encodes the spike protein), although this challenge will be insignificant. These molecular tests would still be able to detect viral RNA since they include more than one gene target and thus would not result in false-negative results. Additional genomic analysis of the SARS-CoV-2 VOC 202012/01 circulating in the UK has reported mutation E484K in the spike protein in some sequences.Citation27 This mutation is present in the SARS-CoV-2 B.1.351 and P.1 variants. As of 05 February 2021, the COVID-19 Genomics UK Consortium (COG-UK) has determined and sequenced over 236,000 variants from UK patients’ samples. By the end of 2020, has confirmed the VOC 202012/01 variant in 31 different countries, including the US, Italy, Australia, Canada, Iceland, Netherlands, and Denmark. This VOC 202012/01 variant exhibited mutations that are linked to the attenuation of other variants.
South African health authorities reported VOC 202012/02 variant, (also known as SARS-CoV-2 variant B.1.351), on 18 December 2020.Citation18 This variant was fast spreading across South Africa. The South African variant was locally referred to as 20H/501Y.V2 because it has the spike protein N501Y mutation.Citation18 Although the UK variant VOC 202012/01 has N501Y mutation, the South African 501Y.V2 is a completely different variant. By 16 November 2020, sequencing data indicated that the VOC 202012/02 variant has displaced other SARS-CoV-2 viruses in the KwaZulu-Natal, Eastern Cape Western Cape provinces.Citation18 Initial research shows that the 501Y.V2 variant is linked to increased viral load indicating higher transmissibility risk, but there is no increased severity of disease or deaths.Citation28 More research is necessary to understand further the changes in transmission, lab diagnostics, clinical severity of infections, vaccines, therapeutics, and public health containment measures. The South African 501Y.V2 variant has spread out of South Africa to four other countries including the United States. In addition, this variant contains also mutation E484K in the spike protein, and some studies have suggested that it may represent the antigenic evolution of SARS-CoV-2.Citation29
In Japan, the VOC 202101/02 variant, (also known as SARS-CoV-2 variant P.; descendent of B.1.1.28 or 20J/501Y.V3), was first discovered in four Brazilian travelers,Citation18 and then was subsequently reported to account for 42% of 31 sequenced samples (RT-PCR positive samples collected between 15 to 23 December 2020) in the Amazonas state of Brazil.Citation30 It has subsequently been reported in other countries, including the United States. This variant was found to have undergone mutations at the spike protein receptor-binding domain, including N501Y, E484K, and K417T.Citation30 It is suggested to influence antigenic behavior and transmissibility; more research is necessary to determine its impact altogether. Global analysis considering over 12,000 other SARS-CoV-2 virus mutations did not get any evidence showing any of the variants to poses higher transmissibility.
Moreover, as SARS-CoV-2 continues to spread and cause diseases, emerging variants of the virus are being identified worldwide. Because of their capacity to significantly alter the properties of the virus, some variants have been designated “Variants of Concerns (VOCs)“or”Variants of Interests (VOIs)” by the World Health Organization (WHO) for easier and more practical discussion of the variants. The WHO has recently has renamed the dominantly circulating variants by Greek alphabets, ie Alpha (α) for B.1.1.7 (UK variant), Beta (β) for B.1.351 (South Africa), Gamma (γ) for P.1 (Brazil), Delta (γ) for B.1.617.2 (India), and so on. The highly contagious Delta variant has displaced Alpha as the most prevalent variant ever since the SARS-CoV-2 Delta outbreak in India in April 2021.Citation31
After the World Health Organization reported on its rapid spread in South American nations such as Peru, Ecuador, Argentina, and Brazil, another variant of Lambda (C.37) has been emerged. The World Health Organization (WHO) stated that “lambda has been associated with substantive rates of community transmission in multiple countries, with rising prevalence over time concurrent with increased COVID-19 incidence” and that additional studies into the variant would be conducted.Citation31
Origin and Spread of COVID-19
COVID-19 pandemic is reported to have started in Huanan South China Seafood Market, in Wuhan City, Hebei Province, China, in December 2019. The market is a center for live animals’ trade, and therefore, the virus is suspected to be of zoonotic origin.Citation32 SARS-CoV-2 is likely to be a recombinant virus due to bat coronavirus and a coronavirus of unknown origins. Minks and pangolins are suspected to be the potential intermediate hosts for the virus. However, no evidence has shown how the virus was transmitted from a bat reservoir to intermediary animals and then humans.
The virus spread into other parts of China through human-to-human transmission (humans became a secondary source of the COVID-19 virus). The virus spread very rapidly from Hubei to Mainland China in just 30 days.Citation33 COVID-19 infection occurs when an individual comes into close contact with infected persons and exposure to the virus. COVID-19 outbreak was rapid in China, and when to other nations across the world, transmission rates were still high. Global transmission saw peaks in transmission rate in Italy, Spain, Germany, Korea, France, the United States, Iran, and Brazil. As at 31 May 2020, there were 5,934,936 confirmed COVID-19 cases and 367,166 deaths globally.Citation34 The WHO has acknowledged that COVID-19 continues to spread and is still a challenge to global public health.
Epidemiology of COVID-19
Much research has been conducted since the outbreak began to understand its transmissibility, severity, mutation, and other virus attributes. Researchers found that individuals aged ≥60 years and people with a background of low immunity (due to cancer, diabetes, renal dysfunction, cardiovascular disease, hepatic dysfunction, and chronic respiratory disease) were likely to suffer from severe COVID-19. Younger people may not get infected or may have mild symptoms, or may be asymptomatic. Findings report the chances of getting COVID-19 infection among children and adolescents to be 0.56 susceptibility than adults. Data from China indicated that 87% of the reported cases were in the age bracket of 30 to 79 years and men accounted for 51% of the confirmed cases.Citation2 According to the CDC COVID-19 Response Team et al,Citation35 in the US, individuals over 65 years of age accounted for about 31% of the confirmed cases, 45% of hospital admissions, 53% of intensive care needs, and 80% of confirmed COVID-19 deaths, but individuals ages ≥85 years had the highest worse outcomes. An increase in confirmed cases in children, teens, and young adults was noted in the US in late 2020, but hospitalization was 2.5%, critical care admittances were 0.8%, and deaths were <0.1%. The confirmed cases among children were linked to familial clusters or those who interacted with infected persons.
According to Khalil et al,Citation36 a meta-analysis of 2500 pregnant women with COVID-19 established that 73.9% were in the third trimester; 50.8% were ethnic minorities such as Black, Asian and Hispanic; 38.2% were suffering from obesity, and 32.5% were suffering from chronic comorbidities. Admission rates for pregnant women due to confirmed COVID-19 in the UK are 4.9 per 1000 maternities. The majority of the women were in the second and third trimesters; 41% were aged ≥35, 56% were Blacks or ethnic minorities, 69% were suffering from obesity, and 34% had chronic comorbidities.
According to the WHO, healthcare workers account for about 14% of the reported COVID-19 cases, a variation of 2% to 35%. The prevalence of infection for health workers varied from 0% to 49.6% and the incidence of COVID-19 seropositivity ranged from 1.6% to 31.6%. The vast variations can be associated with the differences in exposure, settings, symptom status, community transmission rates, adherence to transmission control measures, and other elements. A meta-analysis of 130,000 healthcare workers approximated the total seroprevalence of COVID-19 antibodies at 8.7%, and North America had 12.7% seroprevalence compared to Europe’s 8.5%, Africa’s 8.2%, and Asia’s 4%. The main risk factors for seropositivity among health workers were male sex; patient-facing work; COVID-19 unit roles; Asian, Black, or Hispanic ethnicity; and frontline healthcare roles. According to WHO Situation Report 82,Citation13 as of 08 April 2020, 52 countries had reported a total of 22,073 cases of COVID-19 infections in healthcare workers. According to, out of 9000 confirmed cases among healthcare officers in the US, exposure to COVID-19 in the healthcare setting was 55%, households at 27%, community 13%, and multiple settings at 5%. Nurses account for the more significant percentage of health workers affected by COVID-19. About 5% of healthcare workers suffered severe effects, and mortality was at 0.5%. Healthcare workers with preexisting conditions such as diabetes, obesity, and hypertension were prevalent, seem to be at a higher risk of suffering severe COVID-19 infections.
Pathophysiology
The SARS-CoV-2 virus attaches itself to the angiotensin-converting enzyme 2 (ACE2) receptor using its spike glycoprotein-S and fuses with the host cell’s membrane.Citation37 The virus then infects its target cell by utilizing its serine proteases TMPRSS2 (transmembrane protease serine 2) to achieve S protein priming. SARS-CoV-2 has two subunits in its protein spike: the S1 receptor binding subunit and S2 fusion subunit that facilitate virion binding with receptor protein to start membrane fusion. For successful virion attachment to receptor and fusion to the cell membrane, the spike protein has to contain a cleavage caused by the cellular proteases of the S1/S2 cleavage site.Citation38 Molecular investigations of S proteins revealed an insertion at S1/S2 site that is missing in other SARS-CoV. This insertion is linked to increased efficiency in cell infection and spread within the human body. The RNA of the virus inhibits a host cell’s ability to start polypeptides chain synthesis and viral genome replication to create the replication-transcription complex (RCT) that helps produce the structural proteins (nucleocapsid and envelope) and sub-genomic RNAs. The viral envelope is responsible for viral assembly, release, and enhancing viral pathogenesis. Researchers should focus more efforts on determining the structural properties of COVID-19 that are responsible for the different pathogenic mechanisms.
Clinical Manifestation
According to Lauer et al,Citation39 COVID-19 has a mean or interquartile range of about 5.1 (2–7) days incubation window (the period between exposure and the beginning of symptoms). In about 97.5% of persons infected, the symptoms develop 12 days from infection. A median interval of 7 (3–9) days has been noted between the onset of symptoms to the point of hospitalization. Hospitalized patients’ median age differs between 47 and 73 years, but there was about 60% male preponderance in most cohorts. COVID-19 patients who are ≥50 years account for 74% to 86% of the hospitalized patients.
There are numerous clinical manifestations for COVID-19. A COVID-19 study on 44,672 patients in China reported mild clinical manifestations at 81%, severe manifestations at 14%, and critical manifestations at 5% (described by respiratory failure, multiple organ dysfunctions, or septic shock.Citation40 According to Docherty et al,Citation41 research on 20,133 hospitalized COVID-19 patients in the UK revealed that 17.1% had been admitted to intensive care units (ICUs) or high dependency units (HDUs). About 25% of the infected persons had comorbidities but hospitalized COVID-19 patients with comorbidities accounted for about 60% to 90%. In the hospitalized patients, the most prevalent comorbidities are chronic liver disease (found in <5%), malignancy (6–8%), chronic kidney disease (3–13%), chronic pulmonary disease (4–10%), cardiovascular disease (21–28%), diabetes (17–34%), and hypertension (48–57%) of the patients). The most dominant symptoms in admitted patients include fever (about 90% of the hospitalized patients), shortness of breath (53–80%), dry cough (60–86%), vomiting or nausea or diarrhea (15–39%), fatigue (38%), and myalgia (15–44%). Some patients may have unusual symptoms like isolated gastrointestinal symptoms. Approximately 64% to 80% of the admitted patients had gustatory or olfactory dysfunctions.
COVID-19 patients may develop complications such as reduced lung, kidney, liver, heart, brain, and coagulation systems. Infection may cause ventricular arrhythmias, myocarditis, cardiomyopathy, and hemodynamic instability. In patients with severe COVID-19 conditions, encephalitis and acute cerebrovascular illness are common. About 10% to 25% of the hospitalized individuals with COVID-19 suffer arterial and venous thromboembolic events, but this percentage can range from 31% to 59% in patients admitted to the ICU.Citation42 ICU admissions accounted for 17% to 35% of all COVID-19 hospitalizations linked to hypoxemic respiratory failure.Citation43 ICU patients requiring the use of invasive mechanical ventilation were about 29% to 91%. Other conditions that may develop in hospitalized individuals are coagulation and bleeding dysfunction (10–25%), liver dysfunction (19%), kidney complications (9%), and septic shock (6%).Citation43 Children who contract COVID-19 exhibit mild symptoms that are mainly restricted to the upper respiratory tract and have lower hospitalization rates. It is still unclear why children are at a lesser risk of contracting COVID-19, although it’s suggested that this may be due to lower rates of contact with the virus, part immunity caused by contact with other viruses, and less complicated immune reactions. Less than 7% of the children hospitalized with COVID-19 reach severe conditions necessitating mechanical ventilation.
Source and Reservoir for COVID-19
The coronaviruses that infect humans originate from animals. Bats are thought to be the natural hosts of SARS-CoV, MERS-CoV, HCoV-NL63, and HCoV-229E. Bats are the reservoirs of the β (beta-coronavirus) and α (alpha-coronaviruses). Domestic animals can act as intermediate hosts enabling the transmission of the virus from its natural host into humans. Camels served as intermediate hosts for MERS-CoV.Citation44 Masked palm civets were the intermediate hosts for SARS-CoV.Citation45 In the early stages of the SARS-CoV-2 outbreak, sequencing revealed that the virus had 96.2% resemblance to the Bat-CoV RaTG13 that had been earlier discovered in Rhinolophus affinis in Yunnan Province, China. Bats are thought to be the reservoir for SARS-CoV-2, but it is still unclear if Bat-CoV RaTG13 was directly transmitted to humans or an intermediate host (animal). COVID-19 is claimed to be a zoonotic infection, but no findings have hinted to the Huanan Seafood and Wildlife Market in Wuhan as the virus’s source. Research on Malayan pangolins from Guangdong and Guangxi, China, indicated that pangolins could be the intermediate hosts for SARS-CoV-2 between bats and humans due to the high similarity of the SARS-CoV-2 to the pangolin coronavirus.Citation46 More research is still necessary to clarify the actual source of COVID-19. The rate at which COVID-19 spreads is at a serial interval (the mean period between an infected individual spreading the infection to others) of about 4.4–7.5 days.Citation47
Rate and Mode of Transmission
SARS-CoV-2 is mainly transmitted in humans through respiratory transmission. This type of transmission occurs when a person comes into proximity with a positive person in places with little ventilation. The proximity that can result in the transmission of the virus is below 6 feet. After a COVID-19 positive individual sneeze, breathes, speaks, sings, or coughs, they release droplets infested with the virus into their surroundings.Citation48 When an individual without the virus comes into contact with these droplets, the droplets enter them through the nose or mouth, leading to COVID-19 infection. The droplets infested with the virus may settle on surfaces or objects around the infected person. When other individuals contact the objects or surfaces, they can be transferred to the eyes, nose, or mouth through touch before disinfecting or cleaning hands. The virus is highly contagious when the symptoms in an infected person are at their peak. It has been observed that the virus mainly spreads through respiratory droplets when individuals are close to one another.
Airborne transmission mainly takes place in healthcare settings, particularly in aerosol-generating procedures. Airborne transmission is possible between people under specific settings, mostly indoors, spaces with limited ventilation, and crowded places where an infected individual(s) inhabits for extended periods such as planes, restaurants, offices, worship centers, nightclubs.Citation49 Air samples collected from ICUs have been found to contain SARS-CoV-2 RNA, but this could be controlled with the use of protective gear.Citation50 Further research is being conducted to increase knowledge on how airborne transmission happens outside medical centers in which aerosol producing procedures take place.
Other forms of COVID-19 transmission that may be possible but lack or have limited evidence include fomite transmission, fecal-oral transmission, vertical transmission, nosocomial transmission, and transmission through other body fluids. Fomite transmission can happen when a person directly comes into contact with fomites, but it is yet to be supported by research. Fecal-oral transmission or respiratory transmission is possible via aerosolized feces, but very little evidence is available.Citation51 Vertical transmission is seldom, and there is little evidence on it, but findings support transplacental transmission. At birth, about 6.3% of the infants whose mothers were COVID-19 positive also tested positive, while COVID-19 negative infants born to positive mothers were found to have antibodies against the virus.Citation52 Vertical transmission of COVID-19 is preventable using proper hygiene measures. Transmission through body fluids such as blood and sexual fluids is still not confirmed. COVID-19 virus has been found in saliva, blood, urine, tears, semen, cerebrospinal fluid, pleural fluid, pericardial fluid, and cornea, but this does not translate into infectivity. COVID-19 cannot be transmitted sexually. Nosocomial transmission has been linked to infections acquired after more than seven days of hospitalization.
The Impact of COVID-19
Efforts to curb and treat non-communicable diseases (NCDs) have significantly been interrupted by COVID-19 in 155 countries, but the most significant disruptions were witnessed in low-income countries.Citation53 Individuals suffering from NCDs face a greater risk of developing adverse COVID-19 related complications and death. There has been a reluctance to visit hospitals or seek medical attention out of the fear of contracting COVID-19 in healthcare facilities, creating a backlog of healthcare procedures. More and more NCDs are not getting the necessary health care services and medication during the current pandemic. France has recorded a 40% decline in consultations with general health practitioners and a 50% decline in specialist consultations from the beginning of COVID-19, although teleconsultation has increased. Chronic disease management has been affected by cancer centers’ adjourned consultations and procedures that are not that urgent. A survey by WHO conducted in May 2020 revealed that 53% of the 155 countries had disrupted treatment services for hypertension care (partly or entirely); diabetes and diabetes complications (49%); cancer (42%); and cardiovascular problems (31%). Rehabilitation programs following recovery from severe COVID-19 illness have been interrupted in 63% of the 155 countries.
Health care staff in 94% of the 155 countries who were previously assigned to NCDs had been partly or entirely reallocated to focus on COVID-19. It was crucial to reassign staff working in less urgent hospitalized care units to help fight the pandemic. COVID-19 and its containment measures led to public transportation disruption, lack of diagnostics, medicines, and technology. It appears that as the rate of COVID-19 transmission increased, disruption of NCDs treatment also increased. COVID-19 has stretched health care systems worldwide and has forced both global leaders and national governments to institute emergency COVID-19 protocols and reconsider measures to manage the pandemic. Health care systems are overstretched in the majority of the countries. The high infection rates and need for hospitalization have caused physical and mental fatigue in healthcare workers and overloaded hospital infrastructure. Containment measures such as curfews and lockdowns and economic recession are negatively impacting mental health and physical health.
COVID 19 in Saudi Arabia
The variants of SAR-CoV-2 have affected most countries globally, including Saudi Arabia.Citation54 By 7 June 2020, the number of infected individuals by the virus in the country has reached more than 100,000 and Saudi authorities have reported 283 deaths from the virus, most of which were in the main cities including Mecca, Riyadh, Jeddah, and Medina.Citation55 The general seroprevalence of SAR-CoV-2 or Covid 19 in Saudi Arabia is at 11% in July; the prevalence ranges from 1.78% to 24.45% in different regions of Saudi Arabia.Citation56 The incidence of the prevalence of COVID 19 varies in different regions or areas in Saudi Arabia.Citation56 Despite the increase in the number of COVID-19 cases that have been confirmed, the number of reported daily active cases started to stabilize two months after the pandemic began in the country, and the overall recovery rate was 71.4%. Moreover, the mortality rate decreased by 6.4%.Citation57 Several nationwide studies have been conducted in Saudi Arabia concerning COVID-19 in Saudi Arabia. One of them focused on the demographic and clinical characteristics of COVID-19 cases in various Saudi Arabian regions;Citation58 Another looked at how prepared Saudi Arabia was to deal with COVID-19;Citation59 The status of COVID-19 and management practices in Gulf Cooperation Council nations were also discussed in another study.Citation60 More recent study has described the prevalence of COVID-19 in Saudi Arabia throughout the various phases of prevention strategies and evaluates their impact on limiting the disease’s spread.Citation61
Saudi Arabia was among the first countries to respond to COVID 19 by employing useful strategies, prevention measures to reduce the spread of COVID 19 Pandemic.Citation59 The Saudi government, together with the ministry of health, put forward a great effort at all levels of the government to control Covid 19 such as the household quarantine, public awareness campaigns, and the international travel restrictions.Citation59 Saudi Arabian Ministry of Health (MOH) has carried out intensive awareness campaigns, making communication through its website, and televisions among other social media in passing out information on how to prevent the spread of SAR-CoV-2.Citation62 The Ministry of Health worked with other civil servants in the public sector and the media, particularly by using social media platforms.Citation62 These early actions involving public participation in prevention measures helped combat the spread of Covid 19 and its variant in Saudi Arabia.
In addition, as the cases of Covid 19 increased in Saudi Arabia, new regulations were initiated and legislated and put in place with immediate effect. As all the live classes in schools, nurseries, and universities were suspended and replaced with e-learning by online platforms.Citation63 Several organizations were stopped from receiving or serving clients in their offices and switch to online ways to deliver their services. The authorities of every administration or province were allowed to take further measures appropriate to the circumstances. For example, the government of Saudi Arabia stopped issuing Umrah visas to all foreign visitors, which was later followed by suspending Umrah to everyone to combat the spread of Covid 19.Citation63,Citation64 Theses preventive and control measures together with the implementation of successful healthcare and COVID-19 vaccines/treatment protocols were effective ways to control the epidemic of COVID-19 in Saudi Arabia.
In conclusion, COVID-19 pandemic has been widespread across the world and has led to severe respiratory infections and deaths. The rate at which COVID-19 spread across borders and affected countries has highlighted the significance of health care systems to nations and global operations.Citation53 As the case of Covid 19 increased, the Saudi Arabia government was prompted to put on strict measures to curb the spread of the virus from its early stage. These measures were evidence-based, which was in line with the international recommendation by WHO. More emphasis should be put on investments in sustainable healthcare systems, ensuring the abundance of skilled workers, a conducive working environment, and modern equipment.
Disclosure
No conflict of interest related to this work.
Additional information
Funding
References
- World Health Organization. Director-General’s remarks at the media briefing on 2019-nCoV; 2020. Available from:http://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020. Accessed January 21, 2023.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA. 2020;323(13):1239. doi:10.1001/jama.2020.2648
- Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. JAMA. 2020;323(8):707. doi:10.1001/jama.2020.0757
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Eng J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
- Chambers JP, Yu J, Valdes JJ, Arulanandam BP. SARS-CoV-2, early entry events. J Pathog. 2020;2020:1–11. doi:10.1155/2020/9238696
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi:10.1038/s41586-020-2012-7
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280.e8. doi:10.1016/j.cell.2020.02.052
- Ni W, Yang X, Yang D, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24(1):422. doi:10.1186/s13054-020-03120-0
- Costela-Ruiz VJ, Illescas-Montes R, Puerta-Puerta JM, Ruiz C, Melguizo-Rodríguez L. SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. 2020;54:62–75. doi:10.1016/j.cytogfr.2020.06.001
- Duong D. What’s important to know about the new COVID-19 variants? Can Med Assoc J. 2021;193(4):E141–E142. doi:10.1503/cmaj.1095915
- Eaaswarkhanth M, Al Madhoun A, Al-Mulla F. Could the D614G substitution in the SARS-CoV-2 spike (S) protein be associated with higher COVID-19 mortality? Int J Infect Dis. 2020;96:459–460. doi:10.1016/j.ijid.2020.05.071
- Korber B, Fischer WM, Gnanakaran S, et al. Tracking Changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182(4):812–827.e19. doi:10.1016/j.cell.2020.06.043
- World Health Organization. Coronavirus disease 2019 (COVID-19) situation report – 82. data as received by WHO from national authorities by 10:00 CET; 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200411-sitrep-82-covid-19.pdf?sfvrsn=74a5d15_2. Accessed January 21, 2023.
- Bazykin GA, So DD. Emergence of Y453F and Δ69-70HV mutations in a lymphoma patient with long-term COVID-19. Available from: https://virological.org/t/emergence-of-y453f-and-69-70hv-mutations-in-a-lymphoma-patient-with-long-term-covid-19/580.
- European Centre for Disease Prevention and Control. Rapid increase of a SARS- CoV-2 variant with multiple spike protein mutations observed in the United Kingdom; 2020. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/SARS-CoV-2-variant-multiple-spike-protein-mutations-United-Kingdom.pdf. Accessed January 21, 2023.
- NERVTAG meeting. SARS-CoV-2 variant under investigation VUI-202012/01. Avaliable from: https://app.box.com/s/3lkcbxepqixkg4mv640dpvvg978ixjtf/file/756963730457. Accessed January 21, 2023.
- Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. 2021;372(6538). doi:10.1126/science.abg3055
- World Health Organization. SARS-CoV-2 Variants. World Health Organization. Available from:https://www.who.int/csr/don/31-december-2020-sars-cov2-variants/en/. Accessed January 21, 2023.
- Volz E, Mishra S, Chand M, et al. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature. 2021;593(7858):266–269. doi:10.1038/s41586-021-03470-x
- Galloway SE, Paul P, MacCannell DR, et al. Emergence of SARS-CoV-2 B.1.1.7 Lineage — United States, December 29, 2020–January 12, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(3):95–99. doi:10.15585/mmwr.mm7003e2
- Yi C, Sun X, Ye J, et al. Key residues of the receptor binding motif in the spike protein of SARS-CoV-2 that interact with ACE2 and neutralizing antibodies. Cell Mol Immunol. 2020;17(6):621–630. doi:10.1038/s41423-020-0458-z
- Gu H, Chen Q, Yang G, et al. Adaptation of SARS-CoV-2 in BALB/c mice for testing vaccine efficacy. Science. 2020;369(6511):1603–1607. doi:10.1126/science.abc4730
- Starr TN, Greaney AJ, Hilton SK, et al. Deep mutational scanning of SARS-CoV-2 receptor binding domain reveals constraints on folding and ACE2 binding. Cell. 2020;182(5):1295–1310.e20. doi:10.1016/j.cell.2020.08.012
- Hoffmann M, Kleine-Weber H, Pöhlmann S. A multibasic cleavage site in the spike protein of SARS-CoV-2 is essential for infection of human lung cells. Mol Cell. 2020;78(4):779–784.e5. doi:10.1016/j.molcel.2020.04.022
- Kemp SA, Collier DA, Datir RP, et al. SARS-CoV-2 evolution during treatment of chronic infection. Nature. 2021;592(7853):277–282. doi:10.1038/s41586-021-03291-y
- Meng B, Kemp SA, Papa G, et al. Recurrent emergence of SARS-CoV-2 spike deletion H69/V70 and its role in the Alpha variant B.1.1.7. Cell Rep. 2021;35(13):109292. doi:10.1016/j.celrep.2021.109292
- Public Health England. Investigation of novel SARS-CoV-2 variant: variant of concern. Technical briefing 5; 2020. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/957504/Variant_of_Concern_VOC_202012_01_Technical_Briefing_5_England.pdf. Accessed January 21, 2023.
- Mahase E. Covid-19: what new variants are emerging and how are they being investigated? BMJ. 2021;2021:n158. doi:10.1136/bmj.n158
- Greaney AJ, Loes AN, Crawford KHD, et al. Comprehensive mapping of mutations in the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human plasma antibodies. Cell Host Microbe. 2021;29(3):463–476.e6. doi:10.1016/j.chom.2021.02.003
- Nuno R. Genomic characterisation of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings. Available from: https://virological.org/t/genomic-characterisation-of-an-emergent-sars-cov-2-lineage-in-manaus-preliminary-findings/586. Accessed January 21, 2023.
- World Health Organization. Tracking SARS-CoV-2 variants. World Health Organization. Available from:https://www.who.int/activities/tracking-SARS-CoV-2-variants. Accessed January 21, 2023.
- Kingsbury JLR. Potential for foodborne transmission of Covid-19:: literature review update. Available from: https://www.unitedfresh.co.nz/assets/COVID-19/United-Fresh---Potential-for-Foodborne-Transmission-of-Covid-19---Literature-Review-Update-19-May-20.pdf. Accessed January 21, 2023.
- Team E. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. China CDC Wkly. 2020;41(2):145–151. doi:10.3760/cma.j.issn0254-6450202002003
- PNG National Department of Health (NDoH). Coronavirus disease 2019 (COVID-19). Available from: http://mail.health.gov.pg/covid19/PNGSR23PCOVID-19(2020-05-31).pdf. Accessed January 21, 2023.
- CDC COVID-19 Response Team, Bialek S. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States; 2020. Available from: https://stacks.cdc.gov/view/cdc/99478. Accessed January 21, 2023.
- Khalil A, Kalafat E, Benlioglu C, et al. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinicalMedicine. 2020;25:100446. doi:10.1016/j.eclinm.2020.100446
- Astuti I, Srafil Y. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): an overview of viral structure and host response. Diabetes Metab Syndr. 2020;14(4):407–412. doi:10.1016/j.dsx.2020.04.020
- Simmons G, Zmora P, Gierer S, Heurich A, Pöhlmann S. Proteolytic activation of the SARS-coronavirus spike protein: cutting enzymes at the cutting edge of antiviral research. Antiviral Res. 2013;100(3):605–614. doi:10.1016/j.antiviral.2013.09.028
- Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. doi:10.7326/M20-0504
- Pan American Health Organization. Technical specifications of medical devices for the case management of COVID-19 in healthcare settings. Interim recommendations; 2020. Available from: https://iris.paho.org/handle/10665.2/51979. Accessed January 21, 2023.
- Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. BMJ. 2020:m1985. doi:10.1136/bmj.m1985
- Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. EClinicalMedicine. 2020;29–30:100639. doi:10.1016/j.eclinm.2020.100639
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19). JAMA. 2020;324(8):782. doi:10.1001/jama.2020.12839
- Azhar EI, El-Kafrawy SA, Farraj SA, et al. Evidence for camel-to-human transmission of MERS coronavirus. N Eng J Med. 2014;370(26):2499–2505. doi:10.1056/NEJMoa1401505
- Wang LF, Shi Z, Zhang S, Field H, Daszak P, Eaton B. Review of bats and SARS. Emerg Infect Dis. 2006;12(12):1834–1840. doi:10.3201/eid1212.060401
- Lam TTY, Jia N, Zhang YW, et al. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature. 2020;583(7815):282–285. doi:10.1038/s41586-020-2169-0
- Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi:10.1016/S0140-6736(20)30567-5
- Dhand R, Li J. Coughs and sneezes: their role in transmission of respiratory viral infections, including SARS-CoV-2. Am J Respir Crit Care Med. 2020;202(5):651–659. doi:10.1164/rccm.202004-1263PP
- National Academies of Sciences E and M. Airborne Transmission of SARS-Cov-2. Shelton-Davenport M, Pavlin J, Saunders J, Staudt A, eds. National Academies Press; 2020.
- Guo ZD, Wang ZY, Zhang SF, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26(7):1583–1591. doi:10.3201/eid2607.200885
- Arslan M, Xu B, Gamal El-Din M. Transmission of SARS-CoV-2 via fecal-oral and aerosols–borne routes: environmental dynamics and implications for wastewater management in underprivileged societies. Sci Total Environ. 2020;743:140709. doi:10.1016/j.scitotenv.2020.140709
- Bwire GM, Njiro BJ, Mwakawanga DL, Sabas D, Sunguya BF. Possible vertical transmission and antibodies against SARS‐CoV‐2 among infants born to mothers with COVID‐19: a living systematic review. J Med Virol. 2021;93(3):1361–1369. doi:10.1002/jmv.26622
- Chriscaden K. Impact of COVID-19 on people’s livelihoods, their health and our food systems. World Health Organization; 2020. Available from: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people’s-livelihoods-their-health-and-our-food-systems#:~:Text=The%20economic%20and%20social%20disruption,the%20end%20of%20the%20year. Accessed January 21, 2023.
- Alahmari AA, Khan AA, Elganainy A, et al. Epidemiological and clinical features of COVID-19 patients in Saudi Arabia. J Infect Public Health. 2021;14(4):437–443. doi:10.1016/j.jiph.2021.01.003
- Al-Rabiaah A, Temsah MH, Al-Eyadhy AA, et al. Middle east respiratory syndrome-corona virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J Infect Public Health. 2020;13(5):687–691. doi:10.1016/j.jiph.2020.01.005
- Alharbi NK, Alghnam S, Algaissi A, et al. Nationwide seroprevalence of SARS-CoV-2 in Saudi Arabia. J Infect Public Health. 2021;14(7):832–838. doi:10.1016/j.jiph.2021.04.006
- Alyami MH, Naser AY, Orabi MAA, Alwafi H, Alyami HS. Epidemiology of COVID-19 in the Kingdom of Saudi Arabia: an ecological study. Front Public Health. 2020;8. doi:10.3389/fpubh.2020.00506
- Alsofayan YM, Althunayyan SM, Khan AA, Hakawi AM, Assiri AM. Clinical characteristics of COVID-19 in Saudi Arabia: a national retrospective study. J Infect Public Health. 2020;13(7):920–925. doi:10.1016/j.jiph.2020.05.026
- Algaissi AA, Alharbi NK, Hassanain M, Hashem AM. Preparedness and response to COVID-19 in Saudi Arabia: building on MERS experience. J Infect Public Health. 2020;13(6):834–838. doi:10.1016/j.jiph.2020.04.016
- Alandijany TA, Faizo AA, Azhar EI. Coronavirus disease of 2019 (COVID-19) in the Gulf Cooperation Council (GCC) countries: current status and management practices. J Infect Public Health. 2020;13(6):839–842. doi:10.1016/j.jiph.2020.05.020
- Javed N, Zuber M, Amin S, Bugis B, Al-Mohaithef M. COVID-19 cases and deaths after implementation of prevention strategies, Saudi Arabia. East Mediterr Health J. 2022;28(2):95–107. doi:10.26719/emhj.21.067
- Khan A, Alahmari A, Almuzaini Y, et al. The role of digital technology in responding to COVID-19 pandemic: Saudi Arabia’s experience. Risk Manag Healthc Policy. 2021;14:3923–3934. doi:10.2147/RMHP.S317511
- Sayed AA. The progressive public measures of Saudi Arabia to tackle covid-19 and limit its spread. Int J Environ Res Public Health. 2021;18(2):783. doi:10.3390/ijerph18020783
- Al-Tawfiq JA, Memish ZA. COVID-19 in the Eastern Mediterranean Region and Saudi Arabia: prevention and therapeutic strategies. Int J Antimicrob Agents. 2020;55(5):105968. doi:10.1016/j.ijantimicag.2020.105968