Abstract
Introduction
Drug and Food Interactions (DFI) arise when particular nutrients in food interact with drugs when consumed concurrently, consequently resulting in alterations in the pharmacokinetics, pharmacodynamics, and therapeutic effectiveness of the drug. This study aimed to evaluate the information and understanding of healthcare providers (HCPs) about common DFI.
Methods
A cross-sectional study was achieved by a self-administered online-based questionnaire to gather data from HCPs in eastern region of Saudi Arabia between Sep. to Oct. 2022. The questionnaire integrated questions related to HCP demographic features and knowledge of DFI. The DFI section included questions that assessed the general knowledge of DFI and knowledge of specific food and drug interactions.
Results
A total of 401 participants completed the study questionnaire; 41.4% were undergraduate students, 37.2% were pharmacists, 10.5% were nurses, and 9.5% were doctors. Unfortunately, HCPs are unable to recognize several food types that may interact with medications, which may lead to undesirable consequences associated with an enormous financial burden. For instance, only 27.9% of the HCPs stated that patients on monoamine oxidase inhibitors should avoid cheese. In addition, only approximately 11% of HCPs knew that patients on levothyroxine should avoid cauliflower, those taking digoxin should avoid wheat bran, those taking lithium should avoid cola, and those on heparin should avoid calcium-rich food. Overall knowledge was significantly higher among pharmacists and others HCPs with more than 5 years of experience.
Discussion and Conclusion
This study demonstrated a low level of knowledge regarding specific food and drug interactions among healthcare providers in the eastern region of Saudi Arabia.
Introduction
Drug and Food Interactions (DFI) arise when particular nutrients in food interact with drugs when consumed concurrently. The clinical significance varies for drug–drug interactions (DDIs), ie, major, moderate, minor, that are recognized as a vital factor for optimum healthcare provision. Similarly, the same can be applied for DFI which are even more complex issue.Citation1 DFI may influence pharmacokinetics, including the ADME process (absorption, distribution, metabolism, and excretion), as well as the pharmacodynamic properties of the medication.Citation2 Therefore, DFI may decrease or increase the bioavailability of medications, causing treatment failure and/or adverse events.Citation3 Additionally, DFI are not been specifically addressed during the drug development phase, except for the effects of whole meals and macronutrients on drug properties.Citation4 DFIs represent the foremost risk for harmless and effective pharmacotherapy; thus, identifying the fundamental mechanisms is essential to avoid these risks to the best extent.Citation5 The degree of drug-food interaction is influenced by the physical and chemical nature of the drug, formulation, food type, and time between the drug and food.Citation6 Clinically substantial DFI can be categorized into pharmaceutical, pharmacokinetic, and pharmacodynamic types, depending on the mechanisms of interaction.Citation7 Pharmaceutical interactions include physicochemical reactions that occur during drug delivery devices, such as enteral feeding tubes. Pharmacokinetic interactions occur when they are associated with drug absorption, distribution, metabolism, and excretion, which greatly fluctuate depending on the presence of food.Citation8 Examples of pharmacokinetic interactions include dairy products that contain divalent cations that form a chelate with ciprofloxacinCitation9 and grapefruit juice deterred CYP3A4 metabolism of simvastatin.Citation10,Citation11 Alternatively, pharmacodynamic interactions arise when food modifies the clinical effect of the drug, resulting in additive, synergistic, or antagonistic effects. For instance, a vitamin K-enriched diet antagonizes the anticoagulant therapeutic effects of warfarin.Citation12 The prevalence of DFI varies greatly between countries, ranging from 6% to 70%.Citation5 Due to the magnitude of the effect of food on oral drug bioavailability, the United States Food and Drug Administration (FDA), followed by the European Medicines Agency (EMA), issued a regulation for preforming bioavailability as well as bioequivalence experiments under fed conditions. Currently FDA and EMA guidelines necessitate the administration of a high-caloric and high-fat test meal for the inquiry of food actions on the oral medication bioavailability. Furthermore, elderly individuals taking several medications for chronic diseases are at an even higher risk of DFI; accordingly, geriatric patients should be scrutinized for DFI.Citation13,Citation14 The incidence and consequences of DFI have been verified by plenty of evidence; therefore, knowledge and understanding of DFI are indispensable for healthcare providers (HCPs) to deter these interactions.Citation15,Citation16
Healthcare providers play an important role in averting DFIsCitation17 via recognizing as well as offering sufficient information regarding probable DFIs. Therefore, the HCPs’ knowledge of DFIs is fundamental. However, studies performed in several parts of the world, such as Jordan,Citation18 Palestine,Citation19 and the United States of AmericaCitation20 reported that HCPs exhibit insufficient information about DFI. In the Kingdom of Saudi Arabia (KSA), a study evaluated the public’s level of knowledge and awareness of DFI in Jeddah. The Data showed that the contributors had poor to intermediate levels of knowledge and awareness of DFI.Citation15 Another study conducted a survey among Pharmacy College students in Al-Jouf Region and demonstrated that students had limited awareness of DFIs signifying the need for educating students and updating their knowledge about DFIs to improve therapeutic efficacy, drug compliance, and patients safety.Citation21 Regarding HCPs, there is a paucity of data about the HCPs’ knowledge and recognition of DFIs in KSA. Therefore, the current study designed to identify HCPs’ knowledge of DFIs and their concomitant factors in the eastern region of Saudi Arabia.
Materials and Methods
Study Design and Setting
This descriptive cross-sectional study aimed to evaluate the knowledge of HCPs regarding DFIs in the eastern region of KSA. The study participants were doctors, pharmacists, nurses, and healthcare students between Sep. to Oct. 2022.
Study Approval
This study was approved by the Institutional Review Board (IRB) of King Faisal University in the eastern region of Saudi Arabia (IRB approval number KFU-REC-2022-OCT-ETHICS211). Informed consent was obtained from each participant prior to data collection.
Sample Size Calculation
The sample size required for this study was estimated using a sample size calculator (www.raosoft.com), using a confidence interval of 95% and a margin of error of 5%.
Data Collection
A self-administered online questionnaire was used to collect data from the participants. The questionnaire was distributed on social media. The questionnaire was adapted and modified from a previous study that assessed the knowledge of HCPs towards DFIs.Citation7 The questionnaire integrated questions for HCPs concerning demographic features including gender, age, ethnic group, level of education, occupation, and years of work experience. The second section was the knowledge regarding DFIs section, which comprised 22 questions that evaluated the general knowledge of DFIs and knowledge of specific food and drug interactions.
Data Quality Control and Data Analysis
A pretest was performed on 5% of the total study population before the start of data collection. Any errors found during the pretest were corrected and modifications were made to the final version of the questionnaire. All the collected data were examined for completeness and consistency during data management, storage, and analysis.
Data were collected, reviewed, and fed into SSPS version 21. The statistical methods used were two-tailed with an alpha level of 0.05, considering significance if the p-value was less than or equal to 0.05. Regarding the HCPs’ knowledge, each correct answer was given 1-point score. The overall knowledge level regarding DFIs and specific food interactions was assessed by summing the discrete scores for the different correct knowledge items. The median score with range was calculated for each domain and the overall knowledge score. Descriptive analysis was performed by prescribing frequency distribution and percentage for study variables, including participants’ sociodemographic data and profession. In addition, participants’ knowledge regarding drug-food interaction was tabulated, while the overall knowledge score was graphed using a box-plot diagram displaying the median score with range. Associations between the overall knowledge scores and the collected sample covariates (age, sex, qualification, specialty, and years of experience) were inspected using the Mann–Whitney test, and the Kruskal–Wallis test was used to evaluate the association between the overall knowledge scores and the highest degree obtained by respondents.
Results
Socio-Demographic Characteristics of Study Participants
A total of 401 HCPs completed the questionnaires. Participants’ ages ranged from 18 to 45 years, with a mean age of 23.4 ± 11.9 years old. Regarding sex, 227 (56.6%) participants were female. Regarding qualifications, 230 (57.4%) were undergraduate students, 123 (30.7%) had a bachelor’s degree, 20 (5%) were residents, and 28 (7%) had a postgraduate degree. A total of 149 (37.2%) pharmacists, 42 (10.5%) nurses, and 38 (9.5%) physicians participated in this study. Considering years of experience, 216 (53.9%) had no work experience, 114 (28.4%) had work experience of 1–4 years while 14 (3.5%) had more than 20 years of experience ().
Table 1 Socio-Demographic Characteristics of Health Care Providers Participated
Knowledge of Healthcare Providers Regarding Drug–Food Interactions
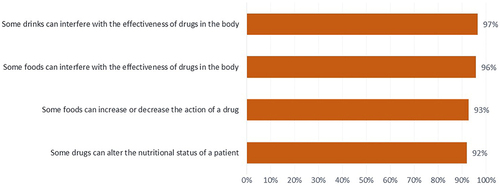
The HCPs’ knowledge was evaluated based on their responses to questions on DFIs. Regarding questions on general knowledge about DFIs, 97% and 96% of the study participants believed that drinking and food, respectively, can affect medication effectiveness. Approximately 93% of the HCP recognized that the effects of foods may intensify or decrease the action of medications. Additionally, 92% of the responders identified that some medications could modify the nutritional status of the patient ().
Knowledge of Healthcare Providers Regarding Specific Foods and Drugs Interactions
HCPs were unable to identify numerous specific food types that could potentially interact with certain medications. illustrates the low level of knowledge regarding specific DFIs among HCPs in eastern Saudi Arabia.
Table 2 General Knowledge of the HCPs About Drug-Food Interaction, Saudi Arabia
Furthermore, 36% of HCPs believed that they lacked sufficient knowledge of DFIs. Of the HCPs, 36% knew that DFIs are influenced by a person’s age, health status, drug dosages from (tablets and capsules) and taking many medications at the same time. In contrast, 53% identified that the geriatric population is the age group most susceptible to DFIs. In addition, 83% of HCPs believed that DFIs can occur when drugs interact with certain items, including diet, iron, vitamin supplements, alcohol, and fruit juices (). The overall score ranged from to 0–9 with a median score of 7 points ().
Figure 2 The overall knowledge score among HCPs regarding DFIs in the eastern region in Saudi Arabia.
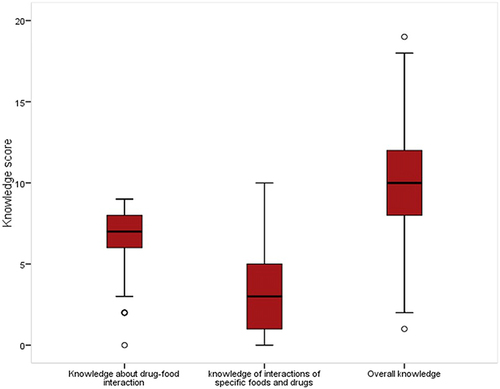
For instance, only 25.7% and 37.7% identified that patients taking theophylline should avoid drinking large amounts of beverages containing caffeine and patients on warfarin should avoid green leaf lettuce, respectively. In addition, 28.7% of HCPs recognized that patients on antibiotics such as tetracycline and fluoroquinolones should avoid dairy products. Simply put, 27.9% of the HCPs knew that patients on monoamine oxidase inhibitors should avoid cheese, which is a detrimental drug-food interaction. Approximately 45.6% of the study respondents correctly answered that acidic foods should be avoided in patients taking antibiotics. Only 15.2% recognized that griseofulvin should be consumed with a low-fat diet. Most HCPs cannot precisely recognize examples of food that interact with specific drugs. For instance, only approximately 11.0% of HCPs knew that patients on levothyroxine should avoid cauliflower, those taking digoxin should avoid wheat bran, those taking lithium should avoid cola, and those on heparin should avoid calcium-rich food. Furthermore, 44.4% correctly answered that foods should be avoided among patients taking antihypertensive drugs; for instance, patients taking spironolactone should avoid potassium-rich foods. The overall score for the knowledge level regarding specific DFIs ranged from to 0–10 with a median score of 3 points, signifying a low knowledge level regarding specific DFIs among HCPs in the eastern region of the KSA. The overall knowledge score ranged from 1 to 19, with a median score of 10 ().
Factors Associated with Knowledge of the Healthcare Providers
demonstrates the features connected with HCPs’ knowledge regarding DFIs in Saudi Arabia. Age had a significant relationship with knowledge about DFIs, knowledge of interactions of specific foods and drugs, and overall knowledge, where a higher knowledge level was detected among HCPs aged > 25 years (P < 0.05). Gender showed an insignificant relationship with any type of knowledge or the overall knowledge level. Regarding qualifications, HCPs with a bachelor’s degree and postgraduate degree showed the highest knowledge level for all domains. Knowledge of the interactions between specific foods and drugs was significantly higher among pharmacists and among those with years of experience than among those with no experience (P= 0.001). In addition, overall knowledge was significantly higher for pharmacists and others with experience exceeding 5 years (P=0.002), as shown in .
Table 3 Participants’ Personal Characteristics Affecting Their Knowledge Level Regarding Drug-Food Interaction, Saudi Arabia
Discussion
The existing study attempted to evaluate the knowledge of drug-food interactions (DFIs) among different groups of healthcare providers (HCPs), including physicians, nurses, pharmacists, dietitians, and undergraduate students, and to identify the factors affecting their knowledge and understanding. In KSA, the Saudi Food and Drug Administration (SFDA) established pharmacovigilance activities to oversee the risk–benefit balance of all registered products during their active marketing cycle in in Saudi Arabia.Citation22
An earlier study performed on 211 primary healthcare (PHC) physicians in three cities, Dammam, Al-Khobar, and Qatif, revealed that PHC had low knowledge of DFIs. This study suggested that the cause of this low knowledge was that PHC were not adequately trained in DFIs.Citation23
The existing study findings parallel those of earlier studies in which physicians, nurses, and pharmacists were described as having an inadequate understanding of DFIs in different places worldwide, such as Palestine,Citation19 EthiopiaCitation7 and South Africa.Citation13 Designed for general knowledge questions, the majority of HCPs identified that food and drinks may interact with drugs, which can alter the nutritional status of a patient. Unfortunately, only a few HCPs distinguished that elderly patients (> 60 years) were at a higher risk of drug-food interactions. Elderly patients are at an increased risk of developing DFIs owing to changes in physiological functions associated with aging, numerous disease conditions, and polypharmacy.Citation24,Citation25 Knowledge of the age group at risk for DFIs is indispensable to ensure that they are prioritized for counselling, scrutinized for any possible DFIs, and develop the correct drug prescription plan and nutritional intervention.Citation26
In the current study, HCPs exhibited inadequate knowledge of precise foods that may interact with certain medications. Approximately a quarter of the HCPs identified that theophylline could interact with caffeine. The use of caffeine while consuming theophylline can cause several adverse effects including nausea, vomiting, sleeplessness, tremors, restlessness, irregular heart rate, and seizures. Thus. Drinks or foods that contain caffeine, such as coffee, tea, cola, and chocolate.Citation27 Similarly, only 37.7% of participants knew that the efficacy of warfarin was affected by green leaf lettuce consumption. The anticoagulant efficacy could be deterred by foods containing high amounts of vitamin K or by consuming large amounts of avocado.Citation28 In addition, 28.7% of HCPs recognized that patients taking antibiotics such as tetracycline and fluoroquinolones should avoid dairy products. The chelation of drugs with certain food components is one of the most frequent drug-food interactions.Citation29 For instance, tetracycline bioavailability is reduced by 46–57% when taken with food, by 50–65% when taken with dairy products, and by up to 81% when taken with iron supplements because of chelation, resulting in treatment failure. Even the consumption of a small volume of milk in tea or coffee may reduce tetracycline bioavailability by 49%.Citation30 Similarly, the cation content (eg, calcium, iron, magnesium, and zinc) of certain enteral feeds may cause chelation with quinolones.Citation31 Another significant interaction is that the ingestion of tyramine-containing foods, especially cheese, by patients on monoamine oxidase inhibitors (MAOIs) is associated with a severe hypertensive crisis, characterized by throbbing headache, palpitations, stiff neck, and nausea, which leads to the development of strict dietary restrictions with MAOIs.Citation32,Citation33 However, only a few HCP knew that patients taking MAOIs should avoid cheese. Unfortunately, most HCPs cannot accurately identify specific examples of DFIs. For instance, levothyroxine with cauliflower, digoxin wheat bran, lithium with cola, and heparin with calcium-rich foods have not been recognized by HCPs. A high fiber content may reduce the bioavailability of certain drugs (eg, digoxin and lovastatin) because of drug binding to the fiber. The consumption of high dietary fiber-containing foods can reduce digoxin bioavailability by 16–32%. A high-fiber diet may cause digoxin treatment failure and necessitate dosage modification owing to the narrow therapeutic index.Citation34,Citation35
Knowledge of DFIs was considerably concomitant with the profession. Pharmacists had the highest knowledge scores for all segments when related to other HCPs. Comparable outcomes were described in which the pharmacists exhibited the highest overall knowledge score.Citation13,Citation36 The superior knowledge of pharmacists highlights the potential of pharmacists to educate HCP about DFIs. For instance, the frequency of DFIs decreased in an Iranian hospital when clinical pharmacists educated nurses on DFIs.Citation37 Another study conducted by Almazrou and AlaujanCitation38 assessed the influence of interprofessional education (IPE) on pharmacy and clinical nutrition students’ knowledge of DFIs and their willingness for interprofessional learning. The study concluded that pharmacy and clinical nutrition students’ knowledge regarding DFIs upgraded subsequent to executing the IPE. IPE in healthcare specialties is imperative to augment patient outcomes and shape professional images for coordination and collaboration among HCPs.Citation38 Furthermore, HCPs with postgraduate degrees were more likely to be knowledgeable than those with other degrees were. Presuming a postgraduate degree exposes HCPs to progressive knowledge, advocating the dynamic need for continued education among HCPs. Gender showed insignificant relation with any type of knowledge nor with the overall knowledge. Age showed a significant relationship with knowledge about DFIs, knowledge of interactions between specific foods and drugs, and overall knowledge, where higher knowledge levels were detected among HCPs aged > 25 years. In contrast to earlier studies, and concluded that the age of the HCPs, years of experience, and participation in training on DFIs were not significantly associated with knowledge of HCPs.Citation13 Knowledge of the interactions between specific foods and drugs was significantly higher among pharmacists with experience than among those with no experience. Overall knowledge was significantly higher among pharmacists and others HCPs with more than 5 years of experience.
Integration of knowledge about clinically significant DFIs among HCPs is essential for the effectiveness of the therapeutic process. Therefore, efforts should be made to improve HCPs’ knowledge about potential DFIs and to identify the reasons behind the knowledge gaps as well as to implement strategies for overcoming them. For instance, hospitals administration and the regional health bureau should give more attention and efforts to improve HCPs’ knowledge of DFIs by providing additional educational courses and training.
Conclusions
In conclusion, the current study demonstrated a low level of knowledge regarding specific food and drug interactions among HCPs in eastern Saudi Arabia. Lack of knowledge of nutrient drug interactions may lead to inappropriate drug efficacy and the occurrence of adverse effects. There is a need to improve the knowledge and to raise the level of awareness of HCPs about the potential food drug interactions that are clinically relevant.
Limitations of the Study
One limitation of the current study is that results are based mainly on undergraduate students. Another limitation is the selection bias due to online survey and small sample size relative to the total study population. Data were collected mainly from the eastern region of KSA, which limits the generalizability of the results. Further research with a larger sample size, covering more cities, using a random sampling method, and including other health professionals in educational interventions is recommended.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors took part in drafting, revising or critically reviewing the article. All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest.
Acknowledgments
The authors are grateful to Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University.
Additional information
Funding
References
- Péter S, Navis G, de Borst MH, et al. Public health relevance of drug–nutrition interactions. Eur J Nutr. 2017;56(2):23–36. doi:10.1007/s00394-017-1510-3
- Spanakis M, Patelarou E, Patelarou A. Drug-food interactions with a focus on Mediterranean diet. Applied Sci. 2022;12(20):10207. doi:10.3390/app122010207
- Genser D. Food and drug interaction: consequences for the nutrition/health status. Ann Nutr Metab. 2008;52(1):29–32. doi:10.1159/000115345
- Boullata JI, Hudson LM. Drug–nutrient interactions: a broad view with implications for practice. J Acad Nutr Diet. 2012;112(4):506–517. doi:10.1016/j.jada.2011.09.002
- Koziolek M, Alcaro S, Augustijns P, et al. The mechanisms of pharmacokinetic food-drug interactions – a perspective from the UNGAP group. Eur J Pharm Sci. 2019;134:31–59. doi:10.1016/j.ejps.2019.04.003
- Welling PG. Interactions affecting drug absorption. Clin Pharmacokinet. 1984;9(5):404–434. doi:10.2165/00003088-198409050-00002
- Degefu N, Getachew M, Amare F. Knowledge of drug-food interactions among healthcare professionals working in public hospitals in Ethiopia. J Multidiscip Healthc. 2022;15:2635–2645. doi:10.2147/JMDH.S389068
- Ased S, Wells J, Morrow LE, et al. Clinically significant food-drug interactions. Consult Pharm. 2018;33(11):649–657. doi:10.4140/TCP.n.2018.649.
- Eljaaly K, Helal A, Almandeel T, et al. Multivalent cations interactions with fluoroquinolones or tetracyclines: a cross-sectional study. Saudi J Biol Sci. 2021;28(12):6929–6932. doi:10.1016/j.sjbs.2021.07.065
- Huth F, Schiller H, Jin Y, et al. Novel bruton’s tyrosine kinase inhibitor remibrutinib: drug-drug interaction potential as a victim of CYP3A4 inhibitors based on clinical data and PBPK modeling. Clin Transl Sci. 2022;15(1):118–129. doi:10.1111/cts.13126
- Seden K, Dickinson L, Khoo S, et al. Grapefruit-drug interactions. Drugs. 2010;70(18):2373–2407. doi:10.2165/11585250-000000000-00000
- Jang SM, Bahjri K, Tran H. Safety and efficacy of direct oral anticoagulants for atrial fibrillation in patients with renal impairment. Pharmacy. 2020;8:1.
- Osuala EC, Tlou B, Ojewole EB. Assessment of knowledge of drug-food interactions among healthcare professionals in public sector hospitals in eThekwini. KwaZulu Natal PLoS One. 2021;16(11):e0259402. doi:10.1371/journal.pone.0259402
- Yıldırım AB, Kılınç AY. Yaşlı hastalarda polifarmasi ve ilaç etkileşimi [Polypharmacy and drug interactions in elderly patients]. Turk Kardiyol Dern Ars. 2017;45(Suppl 5):17–21. Turkish. doi:10.5543/tkda.2017.92770
- Zaidi SF, Mgarry R, Alsanea A, et al. A questionnaire-based survey to assess the level of knowledge and awareness about drug-food interactions among general public in Western Saudi Arabia. Pharmacy. 2021;9:2.
- Wiesner A, Gajewska D, Paśko P. levothyroxine interactions with food and dietary supplements-a systematic review. Pharmaceuticals. 2021;14(3):206. doi:10.3390/ph14030206
- Chiba T, Tanemura N, Nishijima C. 薬剤師および管理栄養士における医薬品と健康食品との相互作用に関する相談実態および情報源 [Consultation and information source of interaction between drugs and health foods among pharmacists and dietitians]. Shokuhin Eiseigaku Zasshi. 2022;63(1):27–33. Japanese. doi:10.3358/shokueishi.63.27
- Zawiah M, Yousef A-M, Khan AH, et al. Food-drug interactions: knowledge among pharmacists in Jordan. PLoS One. 2020;15(6):e0234779. doi:10.1371/journal.pone.0234779
- Radwan A, Sweileh A, Shraim W, et al. Evaluation of community pharmacists’ knowledge and awareness of food–drug interactions in Palestine. Int J Clin Pharm. 2018;40(3):668–675. doi:10.1007/s11096-018-0640-x
- Enwerem N, Okunji P. Knowledge, attitudes and awareness of food and drug interactions among nurses with different levels of experience. Int J Nurs. 2015;2015:2.
- Alasfour A. Food-drug interactions (FDI): a survey among students of pharmacy college in al-jouf region. Saudi Arab Inter J Med Dev Count. 2020;5:803–807.
- Bin Yousef N, Yenugadhati N, Alqahtani N, et al. Patterns of adverse drug reactions (ADRs) in Saudi Arabia. Saudi Pharm J. 2022;30(1):8–13. doi:10.1016/j.jsps.2021.08.014
- Al-Najim D, Al-Sahhaf H, Al-Bunaian N. Knowledge and attitude on common food and drug interactions among primary health care physicians in Dammam, Al-Khobar, and Qatif, Kingdom of Saudi Arabia. Int J Sci Res. 2018;7:37–40.
- Akamine D, Filho MK, Peres CM. Drug-nutrient interactions in elderly people. Curr Opin Clin Nutr Metab Care. 2007;10(3):304–310. doi:10.1097/MCO.0b013e3280d646ce
- Faught E, Szaflarski JP, Richman J, et al. Risk of pharmacokinetic interactions between antiepileptic and other drugs in older persons and factors associated with risk. Epilepsia. 2018;59(3):715–723. doi:10.1111/epi.14010
- Petrini E, Caviglia GP, Pellicano R, et al. Risk of drug interactions and prescription appropriateness in elderly patients. Ir J Med Sci. 2020;189(3):953–959. doi:10.1007/s11845-019-02148-8
- Ismail MYM, Yaheya M. Drug-food interactions and role of pharmacist. Asian J Pharm Clin Res. 2009;2(4):1–10.
- Wells PS, Holbrook AM, Crowther NR, Hirsh J. Interactions of warfarin with drugs and food. Ann Intern Med. 1994;121(9):676–683. doi:10.7326/0003-4819-121-9-199411010-00009
- Izzo AA, Ernst E. Interactions between herbal medicines and prescribed drugs: an updated systematic review. Drugs. 2009;69(13):1777–1798. doi:10.2165/11317010-000000000-00000
- Schmidt LE, Dalhoff K. Food-Drug Interactions. Drugs. 2002;62(10):1481–1502. doi:10.2165/00003495-200262100-00005
- Mueller BA, Brierton DG, Abel SR, et al. Effect of enteral feeding with ensure on oral bioavailabilities of ofloxacin and ciprofloxacin. Antimicrob Agents Chemother. 1994;38(9):2101–2105. doi:10.1128/AAC.38.9.2101
- Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004;10(4):239–248. doi:10.1097/00131746-200407000-00005
- Vuong M, González Aragón C, Montarroyos SS. Common food and drug interactions. Pediatr Rev. 2023;44(2):68–80. doi:10.1542/pir.2022-005641
- Nordström M, Melander A, Robertsson E, et al. Influence of wheat bran and of a bulk-forming ispaghula cathartic on the bioavailability of digoxin in geriatric in-patients. Drug Nutr Interact. 1987;5(2):67–69.
- Izzo AA, Di Carlo G, Borrelli F, et al. Cardiovascular pharmacotherapy and herbal medicines: the risk of drug interaction. Int J Cardiol. 2005;98(1):1–14. doi:10.1016/j.ijcard.2003.06.039
- Couris RR, Tataronis GR, Dallal GE, et al. Assessment of healthcare professionals’ knowledge about warfarin-vitamin K drug-nutrient interactions. J Am Coll Nutr. 2000;19(4):439–445. doi:10.1080/07315724.2000.10718944
- Abbasi Nazari M, Salamzadeh J, Hajebi G, et al. The role of clinical pharmacists in educating nurses to reduce drug-food interactions (absorption phase) in hospitalized patients. Iran J Pharm Res. 2011;10(1):173–177.
- Almazrou SH, Alaujan SS. Knowledge and readiness for interprofessional learning among pharmacy and clinical nutrition students at King Saud University. J Multidiscip Healthc. 2022;15:1965–1970. doi:10.2147/JMDH.S360608