Abstract
Background
Responding to inpatient deterioration is less favorable at night than during the day, and this may be related to barriers in collaboration between physicians and nurses. However, there had been no way to assess the problem. This study aimed to develop a scale for physicians to measure difficulties in nighttime collaboration with nurses in response to deteriorating inpatients and to identify factors associated with the developed scale scores.
Methods
We developed a draft scale of Nighttime Collaboration Difficulties between Nurses and Physicians for Physicians (NCDNP-P) based on key informant interviews with physicians. Psychometric validations, including structural validity, criterion-related validity, and reliability tests, were conducted among physicians who worked on night duty or on call in acute-care hospitals in Japan using a cross-sectional web-based questionnaire. Multiple linear regression analyses were performed using independent variables including individual backgrounds, style of working at night, and facility characteristics.
Results
By performing exploratory factor analysis, we confirmed the structural validity of the NCDNP-P, consisting of seven items and two domains (Domain 1: Dissatisfaction with reporting, Domain 2: Barriers to working with nurses). Cronbach’s alpha and McDonald’s omega coefficients were 0.81–0.84 and 0.81–0.89, respectively. The criterion-related validity for interprofessional collaboration was confirmed. Multiple regression analysis revealed that the variables employment status, number of night shifts, frequency of nighttime calls about patients under another physician’s charge, and handover between physicians before changing shifts were statistically significantly associated with NCDNP-P scores.
Conclusion
We developed the NCDNP-P, confirming its reliability and validity. Identified factors reflect physicians’ characteristics and the problems experienced working at night and may be associated with barriers in nighttime collaboration. The NCDNP-P can highlight issues in clinical settings and lead to the consideration of initiatives to address such issues.
Introduction
In hospitalized patients, clinical deterioration often occurs during usual care. If the patient is provided with inappropriate care, this increases the risk of adverse outcomes such as unanticipated disease progression, cardiac arrest, and death.Citation1–3 There has been increasing interest in an efficient response to clinical deterioration in hospitalized patients from a perspective of patient safety and improving the quality of care, and active measures such as rapid response systems (RRS) to respond to clinical deterioration have been implemented. Despite these measures, challenges remain related to care processes such as the occurrence of delays in RRS activation at night,Citation3,Citation4 and poorer clinical outcomes, including increased mortality rates, at night.Citation4–6
Appropriate escalation of care requires a series of efficient processes, including recognition of clinical deterioration, recording and reporting, and response. Physicians usually play a central leadership role and are required to have appropriate situation awareness and prompt responses or orders in responding to deteriorating patients.Citation7,Citation8 Nurses play a key role in executing the escalation of care process, from recognition to reporting, and require competencies to correctly assess and care for patients and make referrals of deteriorating patients to physicians.Citation9,Citation10 Many studies have documented challenges in communication or collaboration between physicians and nurses in this process; however, these barriers remain in clinical practice.Citation11–13 In addition, a previous scoping review regarding nighttime detection and response to clinical deterioration identified a gap in research concerning nighttime interprofessional communication and collaboration in response to deteriorating patients.Citation14 Accordingly, knowledge development that focuses on nighttime interprofessional collaboration may help address the challenges of responding to clinical deterioration at night.
Previous evidence showed that approximately 80% or more of the calls received by physicians during the night were from nurses,Citation15,Citation16 and more than half of the calls were deemed urgent in terms of the nature of the call.Citation17,Citation18 These characteristics emphasize the importance of the interaction between physicians and nurses in response to clinical deterioration at night. Barriers to nighttime communication between physicians and nurses have been reported as a theme of a general phenomenon, and cognitive differences between physicians and nurses were considered a factor in the barriers.Citation19 In the concept of interprofessional and physician–nurse collaboration, understanding and mutual respect for another role are key elements.Citation20–22 Having different perceptions about the problem between physicians and nurses may hinder effective collaboration. On the other hand, physicians and nurses have different roles, so they face different barriers and difficulties when collaborating; therefore, understanding each perspective is also necessary to address the nighttime collaboration problem. Focusing on the nighttime physician’s role, when dealing with clinical deterioration, physicians need to have appropriate comprehension of the situation and make therapeutic decisions, even if they are unfamiliar with the patient because of nighttime cross-coverage.Citation23 Focusing on the difficulties of collaborating with nurses during the night, based on the physician’s perspective, will not only help physicians to understand and deal with problems in their practice but also help nurses to understand another’s perspective.
Understanding the nighttime physician–nurse collaborative practice in an acute-care setting and identifying relevant barriers can lead to revealing the problem, as well as considering novel interventions that improve the quality of nighttime care. However, relevant research is currently limited to pursuing understanding through qualitative or descriptive methods. Improving understanding of the quantitative aspect and developing evaluation studies could help advance this area. Measuring instruments of difficulties during nighttime collaboration would facilitate the development of interventions to improve practice and would help evaluate the effectiveness of those interventions. Although some existing scales have been used to evaluate collaboration and cooperation between nurses and physicians,Citation24–27 the constructs and items of these scales do not reflect collaboration in the situation of responding to deteriorating patients at night. Therefore, we need a novel measure instrument to capture the concept of the difficulties physicians face in collaborating with nurses at night concerning responding to clinical deterioration.
The aims of this study were: (i) to develop a scale to measure physicians’ difficulties in nighttime collaboration with nurses in response to deteriorating inpatients; and (ii) to explore relevant factors including individual backgrounds, way of working at night (employment, number of night shifts, and cross-covering), and facility characteristics.
Materials and Methods
Design
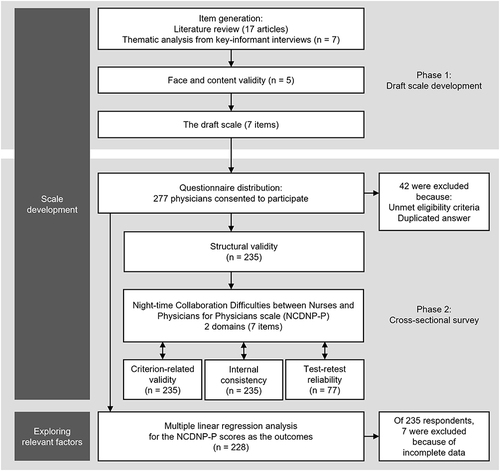
We undertook a two-phase research investigation to develop a novel scale. For Phase 1, we interviewed physicians working on night shifts to identify the pattern of physicians’ difficulties in nighttime collaboration with nurses and to develop a draft scale. Subsequently, for Phase 2, we conducted a cross-sectional questionnaire survey among physicians working night shifts to test the validity and reliability of the scale. In phase 2, the survey also included an analysis to explore factors relevant to the scale score. The process of the study is illustrated in .
Phase 1: Development of a Draft Scale
Item Generation
Initially, we conducted a preliminary literature review for item pooling. The review found 17 previous studies related to nighttime physician–nurse collaboration or communication (Supplementary 1), which provided us with some findings, but there were too few to pool the items. Thus, we conducted key informant interviews to generate the items by analyzing and synthesizing them.Citation28
We defined the key informant physician as (i) currently working at an acute-care hospital and (ii) working three or more night shifts in the past three months. We used snowball sampling to recruit physicians who were currently working night shifts. As a result, seven physicians participated and were interviewed individually. Participants included three internal medicine physicians and four surgeons from four different hospitals, and their experience ranged from 3 to 10 years.
The interview design was semi-structured. The first author (SH) conducted interviews using an interview guide (Supplementary 2). All interviews were conducted remotely using the video conferencing system Zoom (Zoom Video Communications, Inc., San Jose, CA, USA) and ranged in duration from 44 to 56 minutes. The interviews were conducted from August to November 2022. The data from each interview were transcribed and analyzed using Braun and Clarke’s reflexive thematic analysis.Citation29,Citation30 No new patterns emerged in the final few interviews, indicating that saturation had been reached. Thematic analysis found common patterns inductively by coding the physician’s narrative related to nighttime barriers to collaborating with nurses and categorizing them based on their similarities. Consequently, we developed two themes and seven subthemes via thematic analysis (). We determined to derive the subthemes as the questionnaire items by considering the abstraction level of the expressed concepts and generated seven items. Finally, we rechecked the previous studies regarding nighttime physician–nurse collaboration to confirm whether the items covered previously reported findings, and no additional items were added.
Table 1 Conceptual Themes and Subthemes Developed from Interviews with Physicians
Face and Content Validity
Before conducting the main survey, we assessed the clarity and content validity of the draft items by calculating the item-level content validity index (I-CVI) and the scale-level content validity index (S-CVI).Citation31 Physicians who had participated in the prior interviews were asked to assess the clarity and content validity. Participants rated each item in the draft scale on a four-point scale (1 = not relevant to 4 = relevant), to assess whether the item content adequately indicated the difficulty of nighttime collaboration and whether the text facilitated recall of the situation. Based on previous research an I-CVI value of 0.78 or higher was considered acceptable.Citation31 The S-CVI was computed using the mean of the I-CVIs, and an S-CVI value of 0.90 or higher was considered acceptable.Citation31 Five of the seven physicians who had participated in the individual interviews assessed the clarity and content validity, and all participants rated all items as 3 or 4 points; thus the I-CVIs and the S-CVI values were all 1.0. We also asked participants to add item content if they thought that additional items were needed; however, no item content was added. The draft scale of Nighttime Collaboration Difficulties between Nurses and Physicians for Physicians (NCDNP-P) thus consisted of the seven items identified in the original physician interviews.
Phase 2: Psychometric Testing and Exploring Relevant Factors
Participants and Data Collection
We conducted a nationwide cross-sectional questionnaire survey among physicians who were working on night duty or on call in acute-care hospitals in Japan. An acute-care hospital was defined as a hospital with intensive care units (ICUs) or high dependency units (HDUs). The inclusion criteria for participation were: (i) involvement in the care and management of patients in general wards during the night, and (ii) having worked night shifts within the past month. The exclusion criteria were physicians currently working with outpatients or in other departments such as obstetrics, psychiatry, intensive care or high dependency care, or end-of-life palliative care.
A total of 994 hospitals in Japan had ICUs or HDUs, of which 88 were special-functioning hospitals with large bed numbers, advanced medical care provision, or training facilities.Citation32,Citation33 We randomly selected 30 special-functioning hospitals and 80 hospitals other than special-functioning hospitals, which were generally relatively small-scale hospitals. A web-based survey was designed using Google Forms (Google LLC, Mountain View, CA, USA). We mailed flyers containing a Quick Response (QR) code to access the survey form to the hospital directors of the selected hospitals and requested that they distribute them to each clinical department in the hospital. Participants could read the QR code using digital devices such as smartphones, and then answered the questions on the web. We designed the survey so that the participants who accessed the form were first required to confirm their informed consent about this study before they began answering. The survey form also included an item requesting consent for retesting. The participants who consented to retesting were sent the retest survey form by email. The retest was administered two weeks after completion of the first test. We provided a reward (gift card of 500 JPY) to all survey participants; no additional reward was provided for participating in the retesting. The survey data were collected from July to September 2023. Data obtained from respondents were compiled on the Google Forms system. For analysis, a data set was downloaded from there, and cleansing was performed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA).
Instruments
The survey questionnaire included two instruments, one being the draft scale of the NCDNP-P. We understood from our interviews that difficulties in nighttime collaboration would be influenced by the frequency of encountering that event. For instance, there seemed to be differences in the intensity of feeling difficulties regarding similar difficulties or barriers between physicians who often experienced them and those who rarely experienced them. Therefore, we chose the unipolar adjectival scale and asked about the frequency. Each item of the NCDNP-P was scored on a five-point Likert-type scale (0 = never experienced, 1 = rarely experienced, 2 = sometimes experienced, 3 = often experienced, 4 = always experienced). The NCDNP-P is a physician-response scale that scores difficulties in collaborating with nurses at night. Scores for each item on the scale are summed, with higher scores indicating greater difficulty.
The other instrument, the Interprofessional Collaboration Scale (ICS), was used to test criterion-related validity. The ICS was developed and validated by Kenaszchuk et alCitation34 and was constructed so that any professional could rate other professional groups. The ICS consists of 13 items that are divided into three factors: (i) Communication, (ii) Accommodation, and (iii) Isolation. Items are rated on a 4-point agreement scale (1 = strongly disagree to 4 = strongly agree) including reverse-scored items. The mean score for items loading on each of the three factors was calculated, with higher scores indicating better interprofessional collaboration. Kenaszchuk et alCitation34 estimated the internal consistency of the ICS using Raycov’s composite reliability coefficient ρ, with ρ for physicians’ ratings of nurses being 0.80, 0.86, and 0.71 for Communication, Accommodation, and Isolation, respectively. Although there are some specific scales available for measuring physician–nurse or interprofessional collaboration, we decided to use the ICS because this scale can be rated subjectively from each professional perspective. Because no Japanese version of the ICS had been developed, we translated the ICS into Japanese with the permission of the original authors. The translated ICS was also back-translated by a third-party professional, and the back-translation was reviewed by the original authors before proceeding.
Independent Variables for Exploring Relevant Factors
To explore factors relevant to the difficulties of nighttime collaboration, independent variables of the multiple regression analysis were considered based on previous studies and discussions among the researchers.Citation15–19,Citation35–40 We finally selected and collected information on the following respondent characteristics: gender, years of experience as a physician, years of work in the current workplace, hospital type, employment, clinical specialty, number of night shifts per month, provision of night cover care for patients under another physician’s charge, frequency of nighttime calls about patients under another physician’s charge, handover before changing shifts, concurrent work in outpatient services, and the availability of RRS at night.
Statistical Analysis
Descriptive statistics were reported as means and standard deviations (SD) for continuous variables and as frequencies and percentages for categorical variables. All statistical tests were two-tailed and the significance level α was 0.05. All statistical analyses were performed using R version 4.2.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Assessing the Validity and Reliability of the NCDNP-P
The item analysis was performed to confirm the characteristics of the NCDNP-P items, checking the ceiling effect (mean + SD > 4), floor effect (mean − SD < 0), and item-total correlation coefficients (r < 0.3). We performed exploratory factor analysis (EFA) to determine the scale’s factor structure. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (MSA > 0.5) and Bartlett’s test of sphericity (p < 0.05) were used to confirm the adequacy of the EFA performance. The number of factors was determined based on the Kaiser-Guttman criterion of retaining factors with eigenvalues greater than 1.0, and parallel analysis. The EFA was performed using the maximum likelihood method with Harris-Kaiser independent cluster rotation, and items with factor loadings greater than 0.4 and with factor loadings contributing to only one factor were accepted. Criterion-related validity between the score of the NCDNP-P and the total score of the ICS was tested using Pearson’s correlation coefficient. We hypothesized that the scores of the two scales would be negatively correlated. Cronbach’s alpha and McDonald’s omega coefficients were calculated to estimate the internal consistency of the scale, and each value greater than 0.7 was considered acceptable Interrater reliability for the stability of rating the scale was validated using the test-retest method. The test-retest reliability was confirmed by calculating the intraclass correlation coefficients (ICCs).
Exploring Relevant Factors
Multiple linear regression analysis was performed to identify factors associated with the NCDNP-P score. Variables were entered into the model using the forced entry method with predetermined variables as independent variables. Data with missing values for any of the independent variables were removed before analysis using a listwise method. We checked the variance inflation factor (VIF) of the multiple regression model using a value greater than 10 as an indicator of multicollinearity. Categorical variables were converted to dummy variables and entered into the multiple regression analysis. The variables “frequency of nighttime calls about patients under another physician’s charge” and “frequency of handover before changing shifts” were dichotomized from the 4-point responses to “never and seldom” and “sometimes and often” categories and used in the analysis. To indicate the effect of the independent variables on the NCDNP-P, standardized partial regression coefficients, p values, coefficients of determination, and adjusted coefficients of determination were calculated for each variable in the multiple regression model.
Ethical Considerations
This study was conducted following the ethical principles of the Declaration of Helsinki, and with the approval of the ethics committee of Tokyo Medical and Dental University (approval numbers M2022-040 and M2023-011 for the key informant interviews and survey, respectively). All participants provided informed consent and their privacy and anonymity were protected.
Results
Characteristics of Participants
A total of 277 respondents consented to participate in the survey, but 41 were excluded because they did not match the eligibility criteria, and one was excluded because it was a duplicate response; therefore, the responses from 235 respondents were included in the analysis to assess the scale for validity and reliability. Of the 235 respondents, 77 participated in the test-retest survey. Data with missing values for independent variables were removed using the listwise method and 228 sets of responses (surveys) were analyzed using multiple linear regression.
The demographic characteristics of the respondents are shown in . Among the respondents, 86.1% (n = 199) were male, their mean years of experience as a physician were 13.4 years, 86.4% (n = 203) were full-time workers, 66.8% (n = 157) worked four or fewer night shifts per month, and 85.0% (n = 199) were working at special-functioning hospitals.
Table 2 Demographic Characteristics of Survey Respondents (N = 235)
Assessing the NCDNP-P
The item contents and summary of scores on the NCDNP-P scale are shown in . Mean scores of all seven items ranged in ±1 SD and there were no ceiling or floor effects. The total correlation coefficients of all items were greater than 0.3; therefore, no items were eliminated.
Table 3 Performance Metrics of the Nighttime Collaboration Difficulties Between Nurses and Physicians for Physicians (NCDNP-P) Scale (n = 235)
The EFA was conducted using all seven items. The overall MSA of the KMO test was 0.81 and the MSA ranged from 0.73 to 0.92 for each item. The Bartlett test of sphericity was statistically significant (χ2 = 694.05, df = 13, p < 0.001). Two eigenvalues were greater than 1.0 (3.64 and 1.17) and parallel analysis suggested that the number of factors was two, therefore we examined two factors. The EFA using the maximum likelihood method with the Harris-Kaiser independent cluster rotation indicated a scale structure with two factors and seven items. The two factors were named Domain 1: Dissatisfaction with reporting (four items), and Domain 2: Barriers to working with nurses (three items). The factor loading and the cumulative contribution ratio are shown in . The inter-factor correlation was 0.47 between the two domains. The Pearson’s correlation coefficients for the total score of the ICS compared with the total score, Domain 1 score, and Domain 2 score of the NCDNP-P were −0.59, −0.48, and −0.55, respectively.
The Cronbach’s alpha and the McDonald’s omega coefficients of the total score and two domains of the NCDNP-P were 0.81 to 0.84 and 0.81 to 0.89, respectively (). The ICC values of the total score, Domain 1 score, and Domain 2 score of the NCDNP-P were 0.78 (95% confidence interval [CI]: 0.68 to 0.86), 0.73 (95% CI: 0.61 to 0.82), and 0.60 (95% CI: 0.44 to 0.73), respectively.
Exploring the Relevant Factors
The results of the multiple regression analysis using the total score and each sub-scale score of the NCDNP-P as the outcomes are shown in . The VIF values of each variable ranged from 1.05 to 2.43, indicating a lack of multicollinearity. The variable “frequency of handover before changing shifts” was statistically significant for all outcomes (standardized partial regression coefficient [β] = −0.187 to −0.220, p < 0.01). The variables “employment”, “number of night shifts”, and “frequency of nighttime calls about patients under another physician’s charge” were statistically significant for the total score (β = 0.155 to 0.197, p < 0.05) and Domain 1 score (β = 0.173 to 0.227, p < 0.05). No other variables were significantly associated with the Domain 2 score. The adjusted coefficients of determination for each multiple regression model ranged from 0.041 to 0.101.
Table 4 Results of Multiple Linear Regression Analysis of Factors Associated with the Nighttime Collaboration Difficulties Between Nurses and Physicians for Physicians (NCDNP-P) Score (n = 228)
Discussion
In this study, we developed the NCDNP-P, which evaluates physicians’ difficulties of nighttime collaboration with nurses in responding to deteriorating patients. We also identified the respondent characteristics associated with the NCDNP-P scores and confirmed that these results have implications for future research.
Scale Development
We developed the NCDNP-P and confirmed reliability and validity by analyzing the psychometric validation. The item–domain structure was confirmed to have interpretable structural validity by EFA and coincided with the relationship between themes and subthemes presumed by thematic analysis in the key informant interviews. The Cronbach’s alpha and McDonald’s omega coefficient values were greater than 0.8; therefore, the NCDNP-P has high internal consistency. The results of the test-retest, ICC values over 0.5 indicated at least moderate stability of the responses.Citation41 In addition, there were moderate negative correlations between the NCDNP-P and the ICS, supporting our predetermined hypothesis; thus the NCDNP-P has adequate criterion-related validity for assessing collaboration between physicians and nurses.
Domain 1 (Dissatisfaction with reporting) represented the content of physicians’ dissatisfaction with the difficulty in understanding and the appropriateness of reports from nurses at night about deteriorating patients. As included in the existing physician–nurse collaboration scales such as Collaboration and Satisfaction with Care Decisions (CSACD)Citation24 and Nurses’ Opinion Questionnaire (NOQ),Citation42 “satisfaction” with collaboration is an important measurement domain for the scale. Physicians who rate higher scores in this domain may feel difficulty because they are dissatisfied with reporting from night nurses. A possible cause of dissatisfaction with nurse reports may be related to the characteristics of night work. It is common for physicians on night duty to cross-cover patients who are under another physician’s charge,Citation43 and they need to rely on nurses’ information and reports in order to assess and manage deteriorating patients who are unfamiliar to them.Citation44 On the other hand, previous qualitative exploration of physician–nurse collaboration indicated that physicians feel nurses’ communication is unclear, redundant, and does not accurately explain patient problems, which is especially problematic for the on-call physicians who cover patients other than their own.Citation45 This suggests an association with the nighttime call frequency about patients under another physician’s charge, which is discussed below. In addition, the impact of night shifts on cognitive performance may also affect the process of shared situation awareness for both physicians and nurses. A recent study assessing the cognitive performance of clinicians after each shift suggested that cognitive performance worsens for both physicians and nurses after night shiftsCitation46 The cognitive impact during the night shift may affect the ability of nurses to organize and convey information and of physicians to be aware of the situation based on reports from the nurse.
Domain 2 (Barriers to working with nurses) represented the content of perceiving difficulties in working with nurses due to a lack of support or nurses’ attitudes and usual relationships when managing patients with clinical deterioration. Psychological burdens, mood swings, and negative attitudes have been identified as barriers to communication between physicians and nurses during the night.Citation19,Citation47 Previous research investigated the mood states of residents who work night shifts administrating the Profile of Mood States (POMS) and suggested that the “anger–hostility” factor was potentially high among internal medicine residents who participated as physicians primarily performing clinical activities.Citation48 In addition, physicians and nurses absorb emotions from their colleagues, and absorbed anger was associated with cynicism in both physicians and nurses.Citation49 High levels of anger and hostility states among physicians who work the night shift may have negative impacts on both parties in their interactions with nurses. Apart from that, the usual relationship and organizational culture between physicians and nurses are also important factors in communication and collaboration during the night.Citation11,Citation19,Citation50 Nighttime nurse staffing levels are lower than those during the day, which may make it more difficult for physicians to collaborate with nurses when dealing with deteriorating patients during the night. Physicians who are cross-covering also sometimes require collaboration with nurses in other wards who are not involved during the day, and this lack of familiarity may affect the quality of collaboration. The usual relationship may be affected by hierarchies among professionals or individuals. A systematic review of interprofessional practice in responding to clinical deterioration suggested that hierarchy in reporting is a factor that inhibits practice.Citation11 Although this appeared to be particularly problematic for nurses, developing flattened relationships may help remove barriers to physician–nurse collaboration.Citation51
We expect that the NCDNP-P will be used to evaluate the effectiveness of interventions to reduce difficulties during nighttime collaboration. This scale could also be used to identify issues in clinical practice and to consider interventions by interpreting the scores of each domain and item. Furthermore, this scale could be used as a resource to help nurses understand physicians’ difficulties, to enable nurses to improve their practices for working with physicians.
Relevant Factors
Part-time physicians, physicians working more than five-night shifts per month, and physicians with a relatively high frequency of calls about patients under another physician’s charge had higher NCDNP-P scores. In contrast, physicians who relatively often received handovers from other physicians before the night shift tended to have lower NCDNP-P scores.
Part-time physicians tended to have higher NCDNP-P scores, especially for Domain 1 (Dissatisfaction with reporting). This may be because part-time physicians have fewer opportunities to be in charge of inpatients and have little information on how to deal with patients encountered during the night shift. In Japan, more than 90% of medical facilities employ part-time physicians,Citation52 with approximately 18% of all physicians working part-time.Citation53 Although it is common for physicians to work part-time, this may have a negative effect on patient outcomes. A study showing an association between the number of days physicians work clinically and patient outcomes found that patients treated by physicians with fewer clinical days per year had higher 30-day mortality rates than patients treated by physicians in full-time clinical practice.Citation54 Kato et al pointed out that one of the reasons was that part-time physicians may be less familiar than full-time physicians with working with nurses, and other hospital staff, leading to poorer teamwork and worse patient outcomes.Citation54 Our results suggest that part-time physicians tend to experience greater difficulties in collaborating with nurses at night. Further research is needed from the perspective of nurses to gain a deeper understanding of the difficulties they encounter working with part-time physicians.
Respondents who worked more night shifts per month tended to have higher NCDNP-P scores. In Japan, 86.2% of physicians working night shifts reported that they worked five or fewer night shifts per month.Citation55 In other countries, the average number of monthly night shifts was reported as 4.8 ± 1.4 shifts in France,Citation56 5.9 ± 2.4 shifts in Korea,Citation57 and 2.5 ± 1.4 shifts in the United States.Citation58 Even on a global scale, physicians who work night shifts five or more times per month are considered to be working a relatively high number of night shifts. A previous study suggested that the number of monthly night shift days was associated with an increased risk of physicians’ excessive daytime sleepiness by multivariate logistic regression analysis (OR: 1.106, 95% CI: 1.028–1.191).Citation57 Regarding the relationship between sleep and physicians’ performance, recent research suggests that the amount of sleep before a night shift is associated with physicians’ physical and cognitive performance.Citation59 In addition, Malmberg et al concluded that it takes at least two days to recover from a night shift by their study.Citation60 An increased number of night shifts poses risks to adequate physical and mental recovery through sleep, and these effects may impact effective collaboration and communication with other healthcare professionals for patient safety.Citation61 Our result may be explained by these previous findings; however, to further understand the association between the number of night shifts and physician–nurse collaboration, we need to analyze other variables including night work hours, sleep hours, and some performance indicators.
The relative frequency of receiving nighttime calls about patients who were under another physician’s charge tended to increase the difficulties of nighttime collaboration with nurses, particularly with respect to Domain 1. The relatively high mean scores for Items 1 and 2 on the scale suggest difficulty in sharing information about unfamiliar patients who are under another physician’s charge during nighttime collaboration with nurses. This highlights the importance of difficulties in situational awareness related to the cross-coverage system when responding to clinical deterioration of patients during the night. We can suggest several methods to facilitate information sharing and communication regarding cross-cover patients who are not familiar. For instance, one Delphi study provided recommendations for residents who cross-cover at night to communicate in a respectful and closed-loop manner in physician–nurse collaboration.Citation23 In addition to the physician-to-physician handover described below, the implementation of a consultation system and the use of communication tools to enhance situational awareness may serve as intervention strategies to reduce such difficulties during nighttime collaboration. The Situation, Background, Assessment, Recommendation (SBAR) tool is one example of a communication tool for improving physician–nurse communication. In a previous study, widespread use of the SBAR tool as part of RRS implementation resulted in improvements in physician–nurse communication and collaboration, as well as a reduction in unexpected deaths among hospitalized patients after the intervention (RRR: −227%, 95% CI: −793 to −20, p <0.001).Citation62 Even with the impact of RRS, this could contribute to improved communication.
Conducting handovers between physicians before the night shift was identified as a relevant factor associated with lower NCDNP-P scores. This variable showed significant associations not only with the total scores but also with Domains 1 and 2, suggesting that it influences physicians’ overall practice in working with nurses at night and is a significant factor in reducing the difficulties in nighttime collaboration. Screening and sharing information about patients who potentially develop clinical deterioration during the night was suggested as an important component of interventional measures in detecting and responding to nighttime deterioration.Citation14 Sharing patient information among physicians might affect Domain 1 by increasing situational awareness when responding to patients with clinical deterioration. The use of structured communication tools or the organizational change of the handover system could help improve the sharing of information between clinicians. Appropriate information sharing among physicians may enhance understanding of reports by nurses about deteriorating patients and contribute to building trust with nurses due to improved communication. Mutual trust affects physician–nurse collaborative interactions,Citation20 which may influence nurses’ trust in physicians and their collaborative attitudes, as reflected in the Domain 2 score. Organizational changes in addition to education and intervention to change individuals’ attitudes are required to address difficulties in physician–nurse nighttime collaboration.
Limitations
Our study has several limitations. First, there may be sampling bias. Despite randomly selecting and surveying eligible facilities from all over Japan, more than 80% of the respondents were physicians affiliated with special-functioning hospitals. There was also a gender bias in the sample. Of the respondents in this study, only 14% were female, which equates to fewer women than the gender ratio in the Japanese physician population.Citation63 In addition, the respondents in this study participated of their own free will and may also have been biased by having an interest in the research topic. Given these considerations, the influence of sampling bias cannot be eliminated, and this may have affected our results. The second limitation is that this study was based on subjective data from respondents. The response to the number of night shifts may have deviated from the actual working state, and the call frequency was subjectively rated, so the accuracy of responses cannot be verified. To establish more robust evidence in the future, it would be useful to use more objective indicators such as employment and work data or electronic data on call frequency as variables. Finally, there is a limitation to generalizability. This study excluded physicians working in several specific settings, and validation will be needed when the NCDNP-P is utilized in other clinical settings. The generalizability of the NCDNP-P to other cultures and countries is also unknown because it was developed based on current nighttime management of hospital inpatients in Japan. Further research is required to assess the effects of different physicians from different countries and with different backgrounds on the performance of the NCDNP-P scale.
Relevance to Clinical Practice and Future Research
We expect that the NCDNP-P will be used to evaluate the effectiveness of interventions to reduce difficulties during nighttime collaboration. This scale could also be used to identify issues in clinical practice and to consider interventions by interpreting the scores of each domain and item. Furthermore, examining the relationship between the NCDNP-P and other objective data, such as clinical outcomes and aspects of patient safety, would lead to a more accurate evaluation of the effectiveness of interventions to improve the quality of nighttime collaboration. Despite exploring and assessing the difficulties from physicians’ perspectives in this study, gaining insight into the nighttime collaboration between physicians and nurses would greatly benefit from the perspectives of both nurses and physicians. The NCDNP-P could be used as a resource to help nurses understand physicians’ difficulties, which may lead to improving nurses’ practices for working with physicians. Future research from a more comprehensive perspective, including that of nurses, is required.
Conclusion
In this study, we developed the NCDNP-P and confirmed high reliability and validity through psychometric validation. The NCDNP-P can identify problems related to nighttime collaboration in clinical settings and can also be used to evaluate physicians’ difficulties as an outcome in intervention studies to improve the quality of nighttime collaboration. In addition, we found that factors related to employment status, number of night shifts, frequency of night calls regarding patients under another physician’s charge, and handover between physicians before night shifts were associated with physicians’ difficulties in working with nurses during the night. The results of this study suggest the need for future research, including interventions related to improving nighttime communication with nurses and organizational changes regarding the way of sharing information in nighttime cross-coverage situations to reduce collaboration difficulties and provide more effective care for patients who deteriorate during the night.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Makoto Tanaka reports grants from JSPS KAKEN, grants from Takeda Pharmaceutical Company Limited, grants from Nakatani Foundation for Advancement of Measuring Technologies in Biomedical Engineering, grants from Pfizer Health Research Foundation, outside the submitted work. The authors report no other conflicts of interest in this work.
Acknowledgments
We thank all the participants who cooperated in this research.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, SH, on reasonable request.
Additional information
Funding
References
- Johnston MJ, Arora S, King D, et al. A systematic review to identify the factors that affect failure to rescue and escalation of care in surgery. Surgery. 2015;157(4):752–763. doi:10.1016/j.surg.2014.10.017
- Kause J, Smith G, Prytherch D, Parr M, Flabouris A, Hillman K. A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom–the ACADEMIA study. Resuscitation. 2004;62(3):275–282. doi:10.1016/j.resuscitation.2004.05.016
- Chen J, Bellomo R, Flabouris A, Hillman K, Assareh H, Ou L. Delayed emergency team calls and associated hospital mortality: a multicenter study. Crit Care Med. 2015;43(10):2059–2065. doi:10.1097/CCM.0000000000001192
- Fernando SM, Reardon PM, Bagshaw SM, et al. Impact of nighttime Rapid Response Team activation on outcomes of hospitalized patients with acute deterioration. Crit Care. 2018;22(1):67. doi:10.1186/s13054-018-2005-1
- Churpek MM, Edelson DP, Lee JY, Carey K, Snyder A. American heart association’s get with the guidelines-resuscitation investigators. association between survival and time of day for rapid response team calls in a national registry. Crit Care Med. 2017;45(10):1677–1682. doi:10.1097/ccm.0000000000002620
- Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792. doi:10.1001/jama.299.7.785
- DiazGranados D, Dow AW, Appelbaum N, Mazmanian PE, Retchin SM. Interprofessional practice in different patient care settings: a qualitative exploration. J Interprof Care. 2018;32(2):151–159. doi:10.1080/13561820.2017.1383886
- Retchin SM. A conceptual framework for interprofessional and co-managed care. Acad Med. 2008;83(10):929–933. doi:10.1097/ACM.0b013e3181850b4b
- Jensen JK, Skår R, Tveit B. The impact of early warning score and rapid response systems on nurses’ competence: an integrative literature review and synthesis. J Clin Nurs. 2018;27(7–8):e1256–e1274. doi:10.1111/jocn.14239
- Odell M, Victor C, Oliver D. Nurses’ role in detecting deterioration in ward patients: systematic literature review. J Adv Nurs. 2009;65(10):1992–2006. doi:10.1111/j.1365-2648.2009.05109.x
- Allen E, Elliott D, Jackson D. Recognising and responding to in-hospital clinical deterioration: an integrative review of interprofessional practice issues. J Clin Nurs. 2017;26(23–24):3990–4012. doi:10.1111/jocn.13839
- Douglas C, Osborne S, Windsor C, et al. Nursing and medical perceptions of a hospital rapid response system: new process but same old game? J Nurs Care Qual. 2016;31(2):E1–E10. doi:10.1097/NCQ.0000000000000139
- Gonzalo JD, Moser E, Lehman E, Kuperman E. Quality and safety during the off hours in medicine units: a mixed methods study of front-line provider perspectives. J Hosp Med. 2014;9(12):756–763. doi:10.1002/jhm.2261
- Hotta S, Ashida K, Tanaka M. Night-time detection and response in relation to deteriorating inpatients: a scoping review. Nurs Crit Care. 2023;29:178–190. doi:10.1111/nicc.12917
- Hanson JT, Leykum LK, Pugh JA, McDaniel RR. Nighttime clinical encounters: how residents perceive and respond to calls at night. J Hosp Med. 2015;10(3):142–146. doi:10.1002/jhm.2315
- Parrado RH, Notrica DM, Molitor MS. Nighttime calls, pages, and interruptions to the on-call surgery resident. Am Surg. 2022;88(6):1181–1186. doi:10.1177/0003134821991987
- Sun AJ, Wang L, Go M, et al. Night-time communication at Stanford University Hospital: perceptions, reality and solutions. BMJ Qual Saf. 2018;27(2):156–162. doi:10.1136/bmjqs-2017-006727
- Young JB, Baker AC, Boehmer JK, et al. Using NNAPPS (Nighttime Nurse and Physician Paging System) to maximize resident call efficiency within 2011 accreditation council for graduate medical education (ACGME) work hour restrictions. J Surg Educ. 2012;69(6):819–825. doi:10.1016/j.jsurg.2012.08.010
- Li L, Hou Y, Kang F, Li S, Zhao J. General phenomenon and communication experience of physician and nurse in night shift communication: a qualitative study. J Nurs Manag. 2020;28(4):903–911. doi:10.1111/jonm.13018
- Corser WD.A conceptual model of collaborative nurse-physician interactions: the management of traditional influences and personal tendencies. Sch Inq Nurs Pract. 1998;12(4):325–341.
- Stutsky BJ, Laschinger HKS. Development and testing of a conceptual framework for interprofessional collaborative practice. Health Interprof Pract. 2014;2(2):eP1066. doi:10.7772/2159-1253.1066
- Tan TC, Zhou H, Kelly M. Nurse–physician communication – an integrated review. J Clin Nurs. 2017;26(23–24):3974–3989. doi:10.1111/jocn.13832
- Heidemann LA, Fitzgerald JT, Hughes DT, Hartley S. Inpatient cross-cover consensus recommendations for medical and surgical residents: a delphi analysis. J Grad Med Educ. 2019;11(3):277–283. doi:10.4300/jgme-d-18-00707.1
- Baggs JG. Development of an instrument to measure collaboration and satisfaction about care decisions. J Adv Nurs. 1994;20(1):176–182. doi:10.1046/j.1365-2648.1994.20010176.x
- Hojat M, Fields SK, Veloski JJ, Griffiths M, Cohen MJ, Plumb JD. Psychometric properties of an attitude scale measuring physician-nurse collaboration. Eval Health Prof. 1999;22(2):208–220. doi:10.1177/01632789922034275
- Ushiro R. Nurse-Physician Collaboration Scale: development and psychometric testing. J Adv Nurs. 2009;65(7):1497–1508. doi:10.1111/j.1365-2648.2009.05011.x
- Weiss SJ, Davis HP. Validity and reliability of the Collaborative Practice Scales. Nurs Res. 1985;34(5):299–305. doi:10.1097/00006199-198509000-00010
- Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A Practical Guide to Their Development and Use. Oxford University Press; 2014; doi:10.1093/med/9780199685219.001.0001
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exer Health. 2019;11(4):589–597. doi:10.1080/2159676X.2019.1628806
- Polit D, Beck C. Nursing Research: Generating and Assessing Evidence for Nursing Practice. Wolters Kluwer Health; 2019.
- Ministry of Health, Labour and Welfare of Japan. Regional Bureau of Health and Welfare; 2023. Available from: https://kouseikyoku.mhlw.go.jp/. Accessed September 12, 2023.
- Ministry of Health, Labour and Welfare of Japan. About special functioning hospitals; 2023. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000137801.html. Accessed September 12, 2023.
- Kenaszchuk C, Reeves S, Nicholas D, Zwarenstein M. Validity and reliability of a multiple-group measurement scale for interprofessional collaboration. BMC Health Serv Res. 2010;10:83. doi:10.1186/1472-6963-10-83
- Schröder A, Farhat WA, Bägli DJ, Lorenzo AJ, Koyle MA. Turning a new “page”: ways to decrease the number of pages after hours without compromising patient care. Can J Surg. 2020;63(2):E155–E160. doi:10.1503/cjs.009119
- Zhu J, Stadeli KM, Pandit K, et al. Standardizing nightly huddles with surgical residents and nurses to improve interdisciplinary communication and teamwork. Am J Surg. 2020;219(5):769–775. doi:10.1016/j.amjsurg.2020.03.002
- Harvey R, Jarrett PG, Peltekian KM. Patterns of paging medical interns during night calls at two teaching hospitals. CMAJ. 1994;151(3):307–311.
- Storino A, Polanco-Santana JC, Allar BG, et al. Paging patterns among junior surgery residents in a tertiary care center. J Surg Educ. 2021;78(5):1483–1491. doi:10.1016/j.jsurg.2021.02.009
- Lauffenburger JC, Coll MD, Kim E, et al. Prescribing decision making by medical residents on night shifts: a qualitative study. Med Educ. 2022;56(10):1032–1041. doi:10.1111/medu.14845
- White C, Del Rey JG. Decreasing adverse events through night talks: an interdisciplinary, hospital-based quality improvement project. Perm J. 2009;13(4):16–22. doi:10.7812/TPP/09-076
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
- Adams A, Bond S, Arber S. Development and validation of scales to measure organisational features of acute hospital wards. Internat J Nurs Stud. 1995;32(6):612–627. doi:10.1016/0020-7489(95)00041-1
- Atlas KR, Forbes M, Riches J, et al. The scope of hospital medicine practice at night: a national survey of night shift hospitalists. Hosp Pract. 2021;49(4):292–297. doi:10.1080/21548331.2021.1932507
- Tang CJ, Zhou WT, Chan SWC, Liaw SY. Interprofessional collaboration between junior doctors and nurses in the general ward setting: a qualitative exploratory study. J Nurs Manag. 2018;26(1):11–18. doi:10.1111/jonm.12503
- Chua WL, Legido-Quigley H, Jones D, Hassan NB, Tee A, Liaw SY. A call for better doctor-nurse collaboration: a qualitative study of the experiences of junior doctors and nurses in escalating care for deteriorating ward patients. Aust Crit Care. 2020;33(1):54–61. doi:10.1016/j.aucc.2019.01.006
- Sun J, Stewart P, Chiew A, et al. Association between shift work and cognitive performance on the Trail Making Test in emergency department health officers. Emergency Med Australasia. 2021;33(4):711–717. doi:10.1111/1742-6723.13753
- Lyndon A, Zlatnik MG, Wachter RM. Effective physician-nurse communication: a patient safety essential for labor and delivery. Am J Clin Exp Obstet Gynecol. 2011;205(2):91–96. doi:10.1016/j.ajog.2011.04.021
- Costa C, Mondello S, Micali E, et al. Night shift work in resident physicians: does it affect mood states and cognitive levels? J Affective Disorders. 2020;272:289–294. doi:10.1016/j.jad.2020.03.139
- Petitta L, Jiang L, Härtel CEJ. Emotional contagion and burnout among nurses and doctors: do joy and anger from different sources of stakeholders matter? Stress Health. 2017;33(4):358–369. doi:10.1002/smi.2724
- Walker RM, Boorman RJ, Vaux A, Cooke M, Aitken LM, Marshall AP. Identifying barriers and facilitators to recognition and response to patient clinical deterioration by clinicians using a behaviour change approach: a qualitative study. J Clin Nurs. 2021;30(5–6):803–818. doi:10.1111/jocn.15620
- Fernandopulle N. To what extent does hierarchical leadership affect health care outcomes? Med J Islam Repub Iran. 2021;35:117. doi:10.47176/mjiri.35.117
- Maeda Y, Japan Medical Association. Results of the survey on the number of physicians needed in hospitals [Nihon Ishi Kai: byoin ni okeru hitsuyo ishi-su chosa kekka]. Japan Medical Association Research Institute. Japanese; 2015. Available from: https://www.jmari.med.or.jp/result/working/post-897/. Accessed November 28, 2023.
- Ministry of Health, Labour and Welfare of Japan. The necessary doctor number survey. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryou/hitsuyouishisuu/index.html. Accessed November 19, 2023.
- Kato H, Jena AB, Figueroa JF, Tsugawa Y. Association between physician part-time clinical work and patient outcomes. JAMA Intern Med. 2021;181(11):1461–1469. doi:10.1001/jamainternmed.2021.5247
- Ishimaru T, Okawara M, Yoshikawa T, et al. Trends in physician work schedules in Japan: employed physician surveys of the Japan medical association in 2009, 2015, and 2021. JMA J. 2023;6(3):339–341. doi:10.31662/jmaj.2023-0013
- Maltese F, Adda M, Bablon A, et al. Night shift decreases cognitive performance of ICU physicians. Intensive Care Med. 2016;42(3):393–400. doi:10.1007/s00134-015-4115-4
- Park SY, Lee HM, Kim J. The number of monthly night shift days and depression were associated with an increased risk of excessive daytime sleepiness in emergency physicians in South Korea. Behav Sci. 2022;12(8):279. doi:10.3390/bs12080279
- Machi MS, Staum M, Callaway CW, et al. The relationship between shift work, sleep, and cognition in career emergency physicians. Acad Emergency Med. 2012;19(1):85–91. doi:10.1111/j.1553-2712.2011.01254.x
- Cushman P, Samuel SH, Cushman J, Markert RJ. Improving performance on night shift: a study of resident sleep strategies. J Clin Sleep Med. 2023;19(5):935–940. doi:10.5664/jcsm.10480
- Malmberg B, Kecklund G, Karlson B, Persson R, Flisberg P, Ørbaek P. Sleep and recovery in physicians on night call: a longitudinal field study. BMC Health Serv Res. 2010;10(1):239. doi:10.1186/1472-6963-10-239
- Saadat H. Effect of inadequate sleep on clinician performance. Anesth Analg. 2021;132(5):1338–1343. doi:10.1213/ANE.0000000000005369
- De Meester K, Verspuy M, Monsieurs KG, Van Bogaert P. SBAR improves nurse–physician communication and reduces unexpected death: a pre and post intervention study. Resuscitation. 2013;84(9):1192–1196. doi:10.1016/j.resuscitation.2013.03.016
- Ministry of Health, Labour and Welfare of Japan. Statistics of physicians, dentists and pharmacists; 2020. Available from: https://www.mhlw.go.jp/english/database/db-hss/spdp.html. Accessed March 20, 2024.