Abstract
Objective
In the USA, the American Cleft Palate Association-Craniofacial Association (ACPA-CPF) specifies guidelines to ensure craniofacial teams function in a multidisciplinary fashion to provide care in a sequence that mirrors the patient’s needs. Among these guidelines is the expectation that teams hold regular multidisciplinary team meetings to discuss patient care. The purpose of this study was to identify factors that contribute to optimal team functioning during these meetings. The impact of the virtual format on meetings was also evaluated.
Design
One-hour semi-structured interviews of craniofacial team members, queried on current and ideal team meetings, were conducted from December 2020 – January 2021. Interviews were recorded, transcribed, and coded to identify common themes until thematic saturation was achieved.
Setting/Participants
Sixteen team members from three major American craniofacial centers were interviewed virtually.
Results
Three major categories were identified as integral to successful meetings: (1) meeting content, (2) meeting processes, and (3) team dynamics. Within these categories are several factors that participants reported as important to optimize their multidisciplinary meetings: key content for discussions, integration of patient perspective, recognition of collaboration in determining proper sequence of treatments, an attentive discussion leader promoting equitable discussions, managing absences, and team diversity. Participants also identified benefits and pitfalls of hosting meetings in the virtual setting, including lack of engagement and awkward communication.
Conclusion
Diverse groups of disciplines are expected to come together during craniofacial multidisciplinary meetings to formulate intricate care plans for complex patients. In this study, craniofacial team members have identified several key factors to optimize these meetings. The research group used these factors to propose a self-evaluation instrument for meeting quality improvement, provided in printable format. Further studies should evaluate how implementation of these factors affects meetings and ultimately guides patient care.
Introduction
The care of patients with craniofacial differences requires the expertise of providers from multiple disciplines – plastic surgery, otolaryngology, dentistry, audiology, speech pathology, psychology, etc. The need for multidisciplinary care of patients with craniofacial differences has long been recognized, with the first interdisciplinary meeting of the American Cleft Palate Association, now the American Cleft Palate Association-Craniofacial Association (ACPA-CPF), being held in 1943.Citation1 Multidisciplinary care of patients with craniofacial differences, most commonly cleft-lip and palate, is widely recognized as standard of care among medical, dental, and allied health professionals.Citation2 An estimated 7000 individuals are born with cleft lip and/or palate in the United States each year, and they, in addition to patients with other craniofacial differences, require the care of multidisciplinary craniofacial teams from infancy to adulthood.Citation3 Multidisciplinary team meetings (MDT meetings) often serve as the primary time point during which a patient’s case is discussed and complex treatment plans are developed in quorum.
The ACPA-CPF publishes standards for craniofacial team care including the statement that the team must have a “mechanism for regular meetings among core team members to provide coordination and collaboration on patient care”.Citation4 Despite this, few studies have been performed to evaluate how multidisciplinary craniofacial teams function during team meetings. It is at these meetings that many teams decide how they can best address the medical, surgical, dental, or psychosocial needs of their patients. MDT meetings outside of craniofacial care, most notably tumor boards for cancer patients, have been evaluated extensively and standardized tools for their evaluation have been developed.Citation5,Citation6 However, the unique patient population, diversity of disciplines represented, and the ACPA-CPF requirement for regular team meetings warrant the assessment of craniofacial MDT meetings specifically.
The virtual setting provides a unique set of challenges for team dynamics and functionality during multidisciplinary meetings. The COVID-19 pandemic necessitated a temporary shift to virtual meetings due to physical distancing requirements and some opt to continue virtual meetings for a myriad of reasons. The impact of attending multidisciplinary meetings virtually on the effectiveness of team meetings has been researched in other fields but is still limited in craniofacial team care.Citation7–10 At the time of this study, many meetings are conducted in a virtual or hybrid in-person and virtual format. Therefore, this study also queried participants on how the virtual format influenced their team functioning during meetings.
Given the importance of the craniofacial team meetings in determining treatment plans, the time and effort put into these frequent meetings, and the lack of standardized guidance for optimization, it is important to study craniofacial team meetings specifically. The purpose of this study was to identify factors that contribute to optimal craniofacial multidisciplinary team meetings, including virtual meetings, by interviewing craniofacial team members. An assessment of craniofacial team meetings is an important step in identifying measures to improve team functioning and thereby improve the quality of the care of patients with craniofacial differences.
Materials and Methods
General Study Design
A series of one-hour interviews were held via web-conferencing platform, Zoom, with members from multiple disciplines of craniofacial teams. Participants were informed of the nature of the interview and gave their consent to be interviewed, recorded, and publication of anonymized responses. The subject of the interviews was to ascertain the participant’s opinions on the effectiveness of their team meetings and what factors contribute to optimal meetings. Participants were asked to provide their views on how their team meetings functioned and how they could be improved. Video recordings were transcribed and underwent qualitative analysis to find common themes on effective team functioning.
Participants
Sixteen craniofacial center team members, clinical and administrative, across the United States expressed willingness to participate and were interviewed. Participants were recruited via Email if they were a team member of one of the three craniofacial centers chosen for study. Centers were chosen based on their varied geography and perceived patient volume. Of the multiple centers contacted for participation, three expressed interest. The final three centers varied in team size, disciplines represented, patient volume, and team meeting structure. The research group continued recruitment efforts until participants from several different fields were included in the study. However, additional participants were not pursued once thematic saturation was achieved.
Instruments and Technologies
The interview guide was created by the research team by modifying questions from previous studies of multidisciplinary team functioning.Citation5,Citation6,Citation11,Citation12 Researchers were instructed to read the questions as written in the interview guide; however, interviews were semi-structured to allow for the flexibility to clarify and further explore participant responses (Appendix 1). Interviews were video-recorded using the web-conferencing platform. Each recorded interview was then transcribed using an automated transcription program and checked for accuracy by the research team. Interview transcripts were then uploaded, de-identified, and coded using Atlas.ti software.
Description of Data Analysis
A preliminary theory-driven codebook was created by the research team based on literature review and prior observation of team meetings. Three members of the research team coded interviews. ANON1, an MD candidate, ANON2, a research technician, and ANON3, a graduate student with training in qualitative research methods. The coders received guidance from a mentor who had formal training in qualitative research methods and extensive experience with thematic analysis. ANON1 coded half of the interviews, while ANON2 & ANON3 worked jointly to code the remaining interviews. A circular process was used to introduce data-driven codes and revise the initial theory-driven codes as the researchers progressed through interview transcripts. All three coders met periodically to reach a consensus regarding the revision of codes. The coded transcripts were checked by the opposite coder to ensure accuracy. Thematic saturation was achieved when the team did not need additional codes or revisions to code the remaining interview transcripts. Anonymized data may be requested from the primary author. The recorded interviews will not be made available to protect the anonymity of participants.
Reporting Data
Quotations were de-identified by removing names of participants and specific mention of their institution. Some alterations are made within reported quotes to provide additional context and maintain anonymity. These alterations are denoted by brackets (ie, “[she] enjoys team meetings”). Additional alterations of reported quotations were made to shorten quotes with repetition that occurs in conversational speech. The discipline attached to each quote is provided as it adds important context but has been generalized as much as possible to provide further anonymity (ie, surgeon vs plastic surgeon).
Ethics Statement
A review and approval were provided by the University of North Carolina at Chapel Hill Institutional Review Board (study #20-3297). Participants provided informed consent verbally, including consent to publicize de-identified responses.
Results
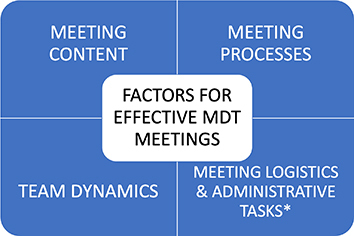
Analysis revealed several themes related to effective craniofacial MDT meetings. These themes have been separated into three major categories: (1) meeting content, (2) meeting processes, and (3) team dynamics (). Interviewees also provided insights on the impact of the virtual format on team meetings. Meeting logistics and administrative tasks integral to successful meetings were described by interviewees, but details are omitted here due to the lack of generalizability.
Figure 1 The four key factors for effective craniofacial multidisciplinary team meetings identified by participants: meeting content, meeting processes, team dynamics, and meeting logistics and administrative tasks. *Logistics and administrative tasks expected to vary widely among different institutions and thus, are not detailed in this study.
Meeting Content
Themes related to meeting content were identified by interviewees as important to facilitate thorough yet efficient discussion of patient cases. The purpose and benefits of MDT meetings were provided by interviewees in addition to important content for the initial case presentation and case discussion, input from local care providers, and community ort reflected in team meetings.
MDT Meeting Purpose and Benefits
Nearly all participants reported that the primary purpose of MDT meetings is to reach a consensus on the best treatment plan for the patient with special attention to the sequence and timing of procedures. The second most frequently mentioned purpose was coordinating that care. Participants also reported several other functions of meetings: gathering expert opinion in the absence of clear guidelines -
In our field, there are certainly treatments and aspects of care for which there is no evidence and where we do rely on consensus. And having multiple people from each specialty allows us to provide the highest quality and safest care to complex patients (md1),
discuss patient needs and psychosocial concerns, clarify plans for effective communication with family and to learn from other disciplines.
Interviewees mentioned several benefits of holding MDT meetings: improves cohesiveness and ensures proper sequence of care, streamlines the treatment plan, provides structured time to gather expert opinion in absence of clear guidelines for the best treatment pathway, provides a unified message to the family, and improves provider confidence in the treatment plan.
Several participants commented on how the team meeting ensures delivery of the proper sequence of treatments -
some recommendations can impact other disciplines…The plastics guys want to know when the kids can be ready for something, and the dental people will give a rough idea of timing. And it’s all pending (the) eruption of the third molars, or the canines…. (surgeon3)
The reported benefits to patients in streamlining the treatment plan included reducing financial burden, unnecessary visits, surgical trauma, anesthesia exposure, etc.
One of the ways we were very cost and morbidity conscious is to try and combine procedures so that if they need to have a surgical procedure, we can do the dental procedures at the same time. You have one operation, one hospitalization, one work loss for the parents… We try to cut the number of surgeries and keep our eye on the prize. What is the result that we’re aiming for, how can we do it with the least treatment possible?. (dds2)
Important Content for the Initial Case Presentation
All participants commented on the importance of a clear and concise patient presentation to set the tone for the remainder of the case discussion. Interviewees offered a number of topics that contribute to an ideal patient presentation. The authors divided these topics into three categories: history, current context, and a specific goal or question to guide the discussion ().
Figure 2 Key components of a thorough case presentation that sets the stage for a patient-centered discussion, as identified by participants. *Reported as a pleasant addition to case presentations by some participants but not regarded as essential to a thorough case presentation.
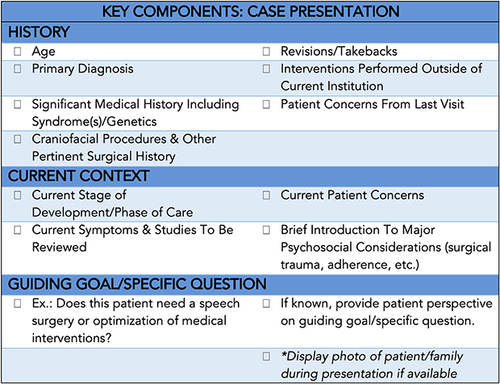
History: patient age, primary diagnosis and significant medical history including underlying syndrome(s)/genetics, surgical history to include all craniofacial procedures, if a surgical intervention has failed and requires revision/take back, if procedures have been performed outside of current institution and concerns from their last visit –
I feel we should be presenting all of the craniofacial procedures, which is easy to run through. It’s like lip, palate, p flap, pe tubes, tonsils, but then if there’s anything significant in their health, so if the child had a cardiac reconstruction procedure…. (surgeon4)
Current context: patient’s current stage of development/phase of care, current patient/family concerns, any pertinent symptoms and related studies to be reviewed, and a brief introduction to major psychosocial considerations (ie, financial hardship, geographic, difficulty with treatment adherence).
Specific guiding goal or question: stating a specific goal or question to guide discussion, if present, can assist disciplines in knowing what information is most important to discuss to keep meetings efficient-
do we need to figure out if this patient needs a trach before their monoblock? (md1).
Important Content for the Case Discussion
In addition to expanding upon the topics described in the initial case presentation section, interviewees reported the following topics as important for team discussion: patient/family preferences, values, concerns, and their opinion on progress and treatments, upcoming significant life events, care received since last team meeting, review of relevant labs and imaging, optimization of allied health and medical therapies (speech therapy, feeding therapy, preventive dental measures, etc.), medical, dental, and surgical plan including the sequence and timing of treatments, potential resource needs, and occasionally, local provider progress or recommendations.
The Patient Perspective: Patient and Family Preferences, Values, Concerns, and Opinion on Progress and Treatments
The authors of this study differentiated the patient perspective from the psychosocial context in questions regarding how patient-centered participants’ team meetings are. Interviewees were asked how the patient’s preferences and opinions on progress and treatments were reflected in their meetings. No interviewees reported a formalized discussion of the patient perspective during their team meetings. That is not to say this information was absent in meetings,
any of us can pull in what we perceive to be patient goals, hopes, and preferences (md1).
the goal is so that they feel better about where they are in their life, it’s not my expectations. It’s theirs… They make the decisions. It’s their life. It’s their face (dds1),
and just because it is not verbalized during the team meeting does not mean providers are not considering the patient perspective. However, some respondents welcomed a more explicit and comprehensive presentation of the patient perspective.
Many benefits of discussing the patient perspective were cited: ensuring the proposed treatment plan is in line with patient/family desires –
I think that kids grow up having every single one of their vacation holidays for some surgery… they put their whole lives on hold, sometimes in order to get surgery completed (socialwork1),
obtaining patient’s satisfaction with treatment thus far, understanding how the family is receiving information and setting realistic expectations, providing clarity when family says contradictory statements to different providers -
one person will say, Oh, I truly believe that this family is not interested in surgery and another person will come in and say, oh, they’re definitely interested in surgery (slp1),
reviewing families’ questions, and resolving team member disagreements on the treatment plan.
Eliciting the Patient Perspective
Most interviewees stated that their team has an informal method of eliciting the patient perspective as these matters tend to come up organically in discussion during clinic visits with providers. Some interviewees mentioned patient satisfaction surveys, but it was unclear to what extent those address the patient perspective and if responses are used in discussion of the individual during team meetings. Others identified a team member who serves as a de facto patient advocate and as they often do not provide direct medical or surgical care, patients may feel more comfortable confiding in them (ie, clinic coordinator, nurse, social worker, etc). Some respondents feel that the informal method of obtaining the patient perspective works well for their team and are open to a formalized method but do not feel it is entirely necessary. Other interviewees felt that more explicitly obtaining and presenting the patient perspective would be prudent.
Input from Local Care Providers
When asked about implementing local care provider input into team meetings, most were ambivalent. The primary arguments for inclusion of input from local providers during meetings were obtaining a more holistic view of the patient, better understanding ort systems and community provider capabilities, and avoiding confusion regarding the treatment plan. Arguments against inclusion of input from local care providers included: time constraints, information is better suited for a specific specialty and unnecessary for the entire team, increased administrative burden, and lack of an existing process to regularly elicit information from local care providers.
Meeting Processes
Several themes emerged regarding processes that contribute to effective multidisciplinary team meetings. There was more variation of themes within this category compared to others, which is likely due to varied infrastructure at different institutions. Interviewees found that the following processes determine whether meetings are successful: discussion leader’s role and responsibilities, order of discussing patient cases, flow of each case discussion, managing absences, general meeting inefficiencies, and display of important media (patient photograph, radiographs, recorded speech sample, etc).
Discussion Leader’s Role & Responsibilities
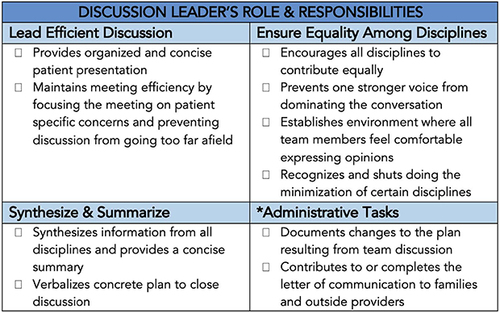
The teams interviewed varied somewhat in both who serves as the discussion leader and their responsibilities. Team members reported having participated in several iterations of discussion leader structures during their careers, which informed their commentary on both real and ideal leader responsibilities. Three major themes emerged regarding the perceived responsibilities of the discussion leader: lead an efficient group discussion, ensure equality among disciplines, and synthesize and summarize information to verbalize a concrete plan. A fourth theme emerged regarding the expected administrative tasks for a discussion leader. It is important for teams to recognize the administrative tasks expected of their discussion leader and the institution infrastructure (ie care coordinator, administrative staff, etc.) to ort these expectations. These themes are detailed further in the figure below ().
Order of Discussing Patient Cases and Flow of Each Case Discussion
Each institution represented had a different structure for the order in which they discussed cases during team meetings. Most interviewees reported that within each meeting, cases are discussed either alphabetically, by the clinic schedule, or randomly with some consideration for provider availability.
One respondent discussed the impact of a recent change to ordering case presentations by complexity -
With the complex patients going first we were able to concentrate our focus on them, and then quickly run through the patients who really didn’t need a great deal of discussion (admin1)
- indicating that the order of patient cases can affect efficiency.
The general structure of case discussions is as follows: case presentation, team discussion, followed by verbalization of a clear recommendation or treatment plan. The flow within that structure varied by institution. Respondents from two institutions reported a standard order of discussion by order of discipline with organic discussion interspersed throughout. One institution appears to have been intentional in the order in which disciplines offer their perspective -
…you’re starting out at 30,000 feet, it’s the rest of the community and the child and the family and what’s their ort mechanisms and then what are the health issues and then eventually you get down to what do their teeth or bite is like. (dds1)
Most respondents seemed pleased with their institution’s current method; however, some recommended changing the flow of discussions to make them more patient-centered –
I guess, I’m a humanist in that I would prefer that psychology and social work set the stage. here’s the family we’re treating versus here’s the condition and then we’re going to kind of retrofit the information about the family into the condition. (dds3)
Meeting “Speed Bumps”
Participants reported the primary meeting inefficiencies as technological issues, discussions not directly relevant to decision making, provider absences, and inadequate chart review prior to meetings. Additionally, discussing complex patients and resolving disagreements were reported to slow meetings but not regarded as inefficiencies.
Technological mishaps were thought to be the primary cause of meeting inefficiency (discussed further in Virtual Format section). Discussing administrative issues and academic or social minutia, often referred to as “getting into the weeds” by interviewees, were both considered to decrease meeting efficiency. One interviewee offered both an illustrative example and a solution to avoid “getting into the weeds”,
we’re interested in the whole patient but sometimes we get into the weeds a little bit too much within our own profession… we are so excited to learn all this information that’s so fascinating to us about this child, because it’s all about [our discipline] but during the team meeting, it may not be the best time to reiterate your entire report to the team. So, when you consider your audience, that is, is the orthodontist going to care about the linguistic complexity of XYZ? Probably not. What the orthodontist is interested in is are the teeth affecting the way the child is producing their sounds?. (slp1)
There is a delicate balance between providing a holistic picture, educating colleagues, and being concise; an optimal balance that likely looks a little different for everyone. And of course, it takes time to learn how to “consider your audience”. The new craniofacial team member may not know exactly what is relevant from their assessment for others to know. Or perhaps, there is a colleague who consistently overshares. According to interviewees, learning what is meaningful to other craniofacial team members and presenting only that information is a skill worth honing.
The Absent Team Member
Attendance was regarded as a key factor for successful meetings by many interviewees. Interviewees reported that having an absent team member negatively affects the meeting in the following ways: slows down the meeting, creates additional administrative work, requires utilization of second-hand knowledge, discipline-specific knowledge absent during meeting, and postponement of decision making.
The primary method utilized to handle absences was to find a substitute to relay a provider’s assessment and plan and to communicate meeting details back to the absent provider. This was reported to be carried out by having a proxy from within the same discipline, a different but similar discipline, an entirely different discipline, or an administrative team member. An alternative method, adopted by some, was to postpone the discussion of a patient’s case until all the relevant providers are present –
We pick the dates for these conferences, making sure that the key players are there, and we wouldn’t have a conference without a key player. (surgeon2)
Team Dynamics
Interviewees reported having a good team dynamic as important in conducting optimal team meetings. Several behaviors contributing to positive team dynamics were identified: creating a welcoming environment by encouraging all to participate, remaining engaged, and demonstrating some enjoyment in participating, exhibiting respectful communication, practicing equality among disciplines, comfortable handling criticisms and disagreements in a professional manner, respecting others’ time by maintaining efficiency, seeking diverse opinions for group discussion, and demonstrating understanding of and gratefulness for the roles fulfilled by colleagues –
I really think it’s the value of each discipline and what people have to offer. The group wants to hear from each specialty. It’s true. there’s value of every person on that team. (surgeon2)
Interviewees also reported that the team dynamic during meetings is heavily influenced by the team leader and by behaviors in clinic.
Interviewees also identified several behaviors, which contribute to poor team dynamics: inequality among the disciplines –
I think there’s still a kind of a traditional aura about what the pecking order is. I think it’s not just on our team, I think it’s just in medicine (socialwork1)
discussing administrative concerns during team meetings, multitasking during patient presentations and team discussion, lacking understanding of roles and responsibilities of colleagues, and inability to concede to others.
Handling Disagreements
Respondents stated their teams most often demonstrated respectful debate to resolve disagreements, which was regarded as the optimal method. Teams reported utilizing several tactics to ort reaching a consensus including active consideration of the patient perspective, team leader eliciting input from other members, scheduling a
follow up conversation amongst a smaller group outside of the [meeting] (md1),
Interviewees also reported experiencing a few maladaptive responses to disagreements including allowing big egos to dismantle healthy discussion –
I think people would back down pretty quickly to the surgeon if he said this is what it is, then, we were all just like all right that’s what it is (audio1)
deferring to disciplines traditionally thought to hold more authority, and lack of decision-making to avoid conflict -
It gets pacified… and then we move on (surgeon4).
I believe that [multidisciplinary meetings] improve the quality because of the integrated range of perspectives. We frequently don’t agree. Then we have a chance to iron that disagreement out and come to a common plan. (dds2)
Impact of Team Diversity
Diversity of specialty, gender, ethnicity, culture, socioeconomic background, duration of practice, training location, and clinical practice patterns among team members were all reported to positively impact team functioning. Interviewees indicated that having a diverse team increased the likelihood of eliciting subtle information from and about patients, allowing for the formation of a more holistic and comprehensive treatment plan -
I think the more diverse our workforces, the more likely we’re going to be able to capture a lot of the subtleties of the clinical encounter… a lot of that best information comes when there’s really good rapport with families, and having a diverse group of providers only enhances the probability of improving rapport with that individual or with the whole team. (surgeon1)
Interviewees also reported diversity enhanced their patient case discussions by bringing in alternative viewpoints and experiences to the discussion.
Virtual Format
The COVID-19 pandemic necessitated an unprecedented shift to a virtual format for patient care and team meetings. Interviewees were asked several questions regarding their experience of attending virtual MDT meetings. It is worthwhile to note that interviewees had several months of experience with the virtual setting prior to being interviewed and that virtual meetings were still the norm at the time of interview.
Most interviewees expressed a preference for in person meetings over the virtual setting, which was largely regarded as a nuisance born of the COVID-19 pandemic. Interviewees provided several cons of the virtual format including lack of engagement, poorer communication, slower meetings, technical issues, and fewer opportunities for team bonding and social niceties. Responses were mixed, even within teams, regarding the effect of the virtual setting on efficiency. Overall, participants were satisfied with their web conferencing platforms and commented on few technical issues.
Lack of Engagement & Awkward Communication in the Virtual Setting
Many of the responses regarding lack of engagement implicated the large number of participants leaving their cameras off as a contributing factor. Other reported contributors included participants multitasking during meetings and awkward communication via web conferencing. Irrespective of the cause, several interviewees reported that discourse suffered somewhat in the virtual setting.
Communication in the virtual setting was reportedly weakened due to awkward mechanics of having multiple speakers, perceived higher threshold to contribute to the conversation-
It’s not challenging to mute and unmute. But you know, it just seems like well, ‘maybe what I have to say is not as important. Because it gets so choppy, and how do I get my voice out there? (ncc1),
and decreased ability to read nonverbal cues.
Advantages to the Virtual Setting
Although it was not the preferred setting, interviewees offered several advantages to holding virtual team meetings: decreased COVID-19 exposure risk, increased efficiency with fewer side conversations, facilitates appropriate multitaskings such as reviewing imaging and charts, and increased attendance.
Discussion
Interviewees discussed several factors that influence the quality of their multidisciplinary team meetings. Through thematic analysis of their interview transcripts, the research team was able to categorize key factors into three major categories: meeting content, meeting processes, and team dynamics.
Meeting Content
Interviewees made recommendations to optimize meeting content to ensure the team efficiently reaches a consensus on a treatment plan that honors the patient’s desires and streamlines interventions. Integral to achieving this aim is ensuring a clear and concise patient-centered case presentation to set the stage for a patient-centered discussion. In addition to making several specific recommendations for presenting the history, current context, and a guiding goal for discussion, participants recommended presenting patients instead of conditions. For example,
This is [patient Y], he’s [15] years old and likes to play football and he’s been on the junior varsity team and he has a diagnosis of hemifacial microsomia, and this is what he does. That versus [patient Y] is a [15] year old with hemifacial microsomia, here are his deficiencies, here is the surgical plan here’s how we’re going to move forward let’s get everyone’s opinion. So, there’s a different way of presenting it like a person versus a condition. (dds3)
Patient-centered presentations and discussions are discussed further in the following patient perspective section. Given the ambivalence of interviewees, teams may consider inclusion of input from local care providers and community orts (ie, teachers, counselors, spiritual networks, ort groups, etc.) on a case-by-case basis. A summary of the recommendations for an optimal case presentation and case discussion can be found in Appendix 2.1. Craniofacial teams may use these recommendations to find their own optimal balance of having comprehensive patient-centered discussions within a realistic timeframe.
The Patient Perspective: Patient and Family Preferences, Values, Concerns, and Opinion on Progress and Treatments
Integral to both the case presentation and discussion is the patient perspective. While the two are intimately intertwined, it is important to distinguish the patient perspective from the psychosocial context. The authors of this study propose a comprehensive definition of the patient perspective to include both the patient and family’s preferences, values, concerns, and opinions on progress and treatments. Understanding that a patient has certain barriers to care does not inform the team that the patient finds competing in their soccer tournament more important than undergoing a flap revision this summer. Craniofacial providers understand the importance of making this distinction as most posited that the patient should “drive” treatment planning; however, several interviewees stated that the patient perspective is not adequately addressed during their multidisciplinary team meetings.
Ensuring a patient-centered meeting begins with an explicit elicitation of a more complete patient perspective on their care. Interviewees reported largely informal methods of gathering the patient perspective (asking for concerns during clinic visit, satisfaction surveys, de facto patient advocates), which could create an opportunity for inequity. For example, a young patient may not feel they have the agency to offer unprompted negative feedback to their surgeon. And what happens if the patient advocate is out of the clinic that day? Is their response on their patient satisfaction survey used to guide their individual care or only to look at institution-level metrics? The discussion of this patient might not be as patient-centered compared to a family that feels more empowered to share their thoughts on treatment thus far. Families may feel reluctant to share displeasure with their care for several reasons (ie, low health literacy, desire to please providers, only comfortable with certain providers) and may require more pointed questions to gather their comprehensive perspective. To reduce potential bias and inequities, teams should consider a standardized method of eliciting the patient perspective to ensure this important information is gathered and discussed for all patients. Standardized forms for patient-reported outcome measures (PROMs) have been created previously, such as the CLEFT-Q questionnaires, and may assist in eliciting the patient perspective and in aiding quality improvement efforts.Citation13–16 Ultimately, the balance teams strike between collecting patient perspectives through informal and standardized feedback will vary based on institution infrastructure and resources.
Once the patient perspective is obtained, it should be discussed and steer decision-making during MDT meetings. All of the participants in this study recognized the patient perspective as the ultimate factor in final decision-making; however, most reported a lack of formalized discussion of the patient perspective during team meetings. To hold truly patient-centered meetings, the authors of this study recommend standardizing case presentations and discussions to explicitly state the patient perspective. While some may find this unnecessary, previous studies on multidisciplinary team meetings have found that providers do not spend significant time discussing the patient’s perspective and overestimate their time discussing the patient’s values and concerns during team meetings.Citation11,Citation17–20
As recommended by a participant, teams may try restructuring the flow of their case discussions to start from the “30,000 feet” view provided by the psychosocial disciplines and work their way down to the surgical and medical details to make discussions more patient-centered. Several interviewees reported a noticeable decline in patient-centered discussion without the presence of their social work or psychosocial colleagues so craniofacial teams may consider allowing these disciplines to lead the effort in obtaining and presenting this information. Teams should consider whether they reliably gather, present, and integrate the patient perspective of all of their patients to ensure equitable patient-centered discussions and decision-making.
Meeting Processes
Interviewees proposed that several processes are influential in the success of their MDT meetings. These include the skill of the discussion leader, structure of discussing patient cases, management of absences and meeting inefficiencies, and the display of important media. This study demonstrated that team members clearly have expectations of their discussion leader beyond presenting the patient history and calling on disciplines to contribute. General expectations include leading an efficient discussion, synthesizing information from all disciplines to verbally summarize a concrete plan, ensuring equality among disciplines during discussions, and various administrative tasks depending upon institution infrastructure (). Discussion leaders should be aware of their team members’ expectations and recognize their importance in contributing to optimal team meetings.
Teams may find it beneficial to review the structure of discussing their cases. The order in which cases are discussed may impact meeting efficiency, with an expected greater impact as the number of patients discussed per meeting increases. Teams should anticipate their lengthier cases, due to medical or social complexity, and prioritize discussing these cases earlier in the meeting. Furthermore, it is often during these complex cases that resolving “healthy dissent” prolongs discussion (surgeon4). Similarly, attempting to discuss a patient’s case when a key provider is absent can unnecessarily lengthen a meeting and create duplicative work outside of the meeting. When utilizing a proxy, the absent team member should consider the proxy’s familiarity with the patient and their knowledge of the absentee’s discipline and provide an appropriate level briefing. Absences are unavoidable; therefore, individual teams should identify the method of managing anticipated and unanticipated absences that works best for their team. Discussing the most medically or socially complex patients first while balancing provider availability may serve as an effective meeting structure for institutions discussing many cases per meeting.
Many of the meeting inefficiencies (irrelevant discussions, inadequate preparation, technological mishaps) cited by interviewees can be managed by an engaged discussion leader, prior preparation, and administrative ort. Teams should strongly consider holding separate meetings with dedicated time to discuss issues that do not directly pertain to individual patient care. This will prevent issues that are not immediately relevant from detracting from patient case discussions. Teams should query their members if they are satisfied with the way in which important media (radiographs, speech recordings, etc.) is displayed during meetings. Some team members may prefer using personal devices to click through the EMR to visualize media as needed while others may prefer that all important media is collected ahead of the meeting and displayed on a shared screen.
Optimization of the meeting processes presented here will depend heavily upon a center’s case volume, resources, and defined roles of team members; therefore, the authors of this study encourage individual craniofacial teams to decide how to best address these factors in a manner that is realistic for their center.
Team Dynamics
Interviewees described their multidisciplinary team meetings as welcoming, collaborative, and equitable; strengthened by their diversity of discipline, experience, and background. Participants overwhelmingly described the team meeting environment as positive using descriptors such as “collegial”, “an atmosphere of exploring”, and “respectful”. Interviewees not only demonstrated an understanding of the roles their colleagues play in the management of their patients but expressed gratitude for the functions their team members perform. It is, perhaps, this gratitude for colleagues and for the ability to serve on a craniofacial team that motivates team members to contribute to positive team dynamics.Citation21,Citation22 Participants also remarked that team diversity improved their meetings by enriching discussions and formulating treatment plans that truly align with patients’ desires. However, some expressed that their teams could do more to increase diversity across several dimensions (ie, race, ethnicity, gender); an action that may improve health outcomes, patient compliance, productivity, and patient satisfaction.Citation23,Citation24
The primary behaviors reported to contribute to poor team dynamics included instances of inequality among disciplines and poor conflict resolution. Interdisciplinary team-based care encourages all members of the team being valued as equals as they collaborate to form treatment plans, a practice that craniofacial teams adopted long ago.Citation21,Citation25,Citation26 However, craniofacial teams are not immune to reverting to traditional hierarchical decision-making and suboptimal team functioning.Citation27 Participants reported witnessing some instances of minimizing allied health disciplines, allowing louder team members to dominate discussions and deferring decision-making to avoid conflict during their team meetings. Teams should aim to achieve equality among disciplines and
not to dismiss difference, but to elevate it and harmonize it so that we make that part of the decision-making process (dds2)
Achieving this aim is important for all medical teams but perhaps even more critical for craniofacial teams, whose patients’ outcomes depend so heavily upon input from a diverse group of disciplines to determine the optimal sequence of treatments. A summary of the beneficial and detrimental behaviors cited by participants in this study can be found in Appendix 2.2 and may be used by craniofacial teams to assess the overall team dynamic during their multidisciplinary team meetings (Appendix 2.2).
Virtual Format
Despite acknowledgment of the virtual setting as a viable alternative with some reported benefits, interviewees preferred in-person meetings overall. The lack of personal engagement and communication difficulties were cited far more than technological mishaps as the reason for the in-person preference; a finding that is in line with previous studies on virtual multidisciplinary team meetings.Citation8,Citation10,Citation28 However, it is difficult to tease apart how much of the perceived lack of engagement is attributable to the virtual forum itself versus the “Zoom fatigue” that many experienced throughout the height of the pandemic.Citation29 The feeling of camaraderie that comes with in-person meetings cannot be entirely replicated in the virtual setting but it can be improved. Teams should set the expectation that cameras must be turned on with the participant’s face in clear view. Team members can optimize their screen to see as many team members as possible while also looking at what is being presented. Team members may then scroll through pages of participants’ screens periodically to gauge engagement through the nonverbal cues that can be obtained via web conferencing.
In addition to optimizing the view, teams can make a few changes to improve the rhythm of their virtual discussions. The virtual setting can disrupt the usual patterns of conversation due to having simultaneous speakers, not realizing one is unmuted, distracting background noise, inappropriate speaking volume, increased waiting time between speakers and hesitancy to unmute or contribute to the conversation.Citation29,Citation30 Much of this can be overcome with practice and some procedural adjustments: designating a team member to monitor the chat, using icons to indicate a need to speak or provide a non-verbal response and remaining on mute when not speaking (additional recommendations in Appendix 2.2). Teams should familiarize themselves with the features of their specific web-conferencing format and may consider hosting intermittent tutorials to remind team members how to best utilize those features.
Limitations
This study faces several limitations that impact the generalizability and reliability of its findings. Firstly, the selection of only three large craniofacial centers for participation may introduce selection bias and hinder the extrapolation of results to a wider range of institutions. Centers selected were all in the United States, which further limits generalizability to teams caring for patients with craniofacial differences outside of the US. Moreover, the reliance on a limited sample size of centers may not adequately capture the diversity of perspectives and practices within the field, thus limiting the broader applicability of the study’s conclusions. Additionally, while a codebook and two-researcher coding guided the qualitative analysis process, the subjective interpretation by coders introduces the potential for bias and inconsistency in identifying themes. These limitations underscore the need for caution when interpreting and applying the study findings to other contexts. This study did not include participants from all disciplines that make up craniofacial teams (ie no geneticists interviewed) so there is the possibility of missing important discipline-specific information despite achieving thematic saturation. Other important limitations include that participants may have been reluctant to share negative feedback with interviewers and, as this study was descriptive in nature, we did not demonstrate that altering the identified factors definitively impacts team meetings.
Conclusion
In conclusion, craniofacial MDT meetings represent a significant time point in the formulation of treatment plans for patients with craniofacial differences. Interviews of craniofacial team members revealed several important factors related to the meeting content, meeting processes, and team dynamics that contribute to successful team meetings. Among these key factors are recommendations to optimize patient presentations, case discussions, role of discussion leaders, communication during meetings, and the virtual format. Teams should also be mindful of potential changes they can make to ensure their meetings are patient-centered including presenting the patient instead of the condition, explicitly discussing the patient perspective, and allowing psychosocial disciplines to initiate case discussion.
This study detailed several factors for successful craniofacial MDT meetings as described by craniofacial team members. The authors of this study have transformed these factors into a meeting self-evaluation instrument, which may be printed, to help teams evaluate their own meetings and case discussions for points of improvement (Appendix 2.1 and 2.2). Teams may consider using this instrument to standardize their presentations and discussions, as they see fit, to ensure equitable discourse for all of their patients. Alternate methods of evaluating the effectiveness of multidisciplinary team meetings, both specific and non-specific to craniofacial teams, have also been published elsewhere.Citation5,Citation12,Citation21 An assessment of craniofacial team meetings is an important step in identifying measures to improve team functioning and thereby improve the quality of care patients with craniofacial differences receive. Future studies should seek to include broader representation of craniofacial team disciplines and evaluate how optimization of these factors impact multidisciplinary team meetings and patient care. The findings of this study are an important first step in better understanding multidisciplinary craniofacial team meeting content, structure, and member dynamics.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors of this study would like to acknowledge Dr. Gary Beck Dallaghan, PhD, for guidance on the thematic analysis of this study.
References
- Richman LC. Presidents’ perceptions: an historic review of fifty years of the American cleft palate-craniofacial association. Cleft Palate Craniofac J. 1993;30(6):521–527. doi:10.1597/1545-1569_1993_030_0521_ppahro_2.3.co_2
- American Cleft Palate-Craniofacial Association. Parameters for the evaluation and treatment of patients with cleft lip/palate or other craniofacial differences; 2018. Available from: https://acpa-cpf.org/team-care/standardscat/parameters-of-care/. Accessed August, 2021.
- Parker SE, Mai CT, Canfield MA, et al. Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res a Clin Mol Teratol. 2010;88(12):1008–1016. doi:10.1002/bdra.20735
- American Cleft Palate-Craniofacial Association. Standards for Approval of Cleft Palate and Craniofacial Teams; 2022. Available from: https://acpa-cpf.org/wp-content/uploads/2019/04/Standards-2019-Update.pdf. Accessed April, 2023.
- Harris J, Taylor C, Sevdalis N, Jalil R, Green JS. Development and testing of the cancer multidisciplinary team meeting observational tool (MDT-MOT). Int J Qual Health Care. 2016;28(3):332–338. doi:10.1093/intqhc/mzw030
- Raine R, Wallace I, Nic A’ Bháird C, et al. Improving the Effectiveness of Multidisciplinary Team Meetings for Patients with Chronic Diseases: A Prospective Observational Study. Southampton (UK): NIHR Journals Library; 2014.
- Aghdam MRF, Vodovnik A, Hameed RA. Role of telemedicine in multidisciplinary team meetings. J Pathol Inform. 2019;10(1):35. doi:10.4103/jpi.jpi_20_19
- Dharmarajan H, Anderson JL, Kim S, et al. Transition to a virtual multidisciplinary tumor board during the COVID-19 pandemic: University of Pittsburgh experience. Head Neck. 2020;42(6):1310–1316. doi:10.1002/hed.26195
- Janssen A, Brunner M, Keep M, et al. Interdisciplinary eHealth practice in cancer care: a review of the literature. Int J Environ Res Public Health. 2017;14(11):1289. doi:10.3390/ijerph14111289
- Sidpra J, Chhabda S, Gaier C, Alwis A, Kumar N, Mankad K. Virtual multidisciplinary team meetings in the age of COVID-19: an effective and pragmatic alternative. Quant Imaging Med Surg. 2020;10(6):1204–1207. doi:10.21037/qims-20-638
- Jalil R, Ahmed M, Green JS, Sevdalis N. Factors that can make an impact on decision-making and decision implementation in cancer multidisciplinary teams: an interview study of the provider perspective. Int J Surg. 2013;11(5):389–394. doi:10.1016/j.ijsu.2013.02.026
- Lamb BW, Wong HW, Vincent C, Green JS, Sevdalis N. Teamwork and team performance in multidisciplinary cancer teams: development and evaluation of an observational assessment tool. BMJ Qual Saf. 2011;20(10):849–856. doi:10.1136/bmjqs.2010.048660
- Allori AC, Kelley T, Meara JG, et al. A standard set of outcome measures for the comprehensive appraisal of cleft care. Cleft Palate Craniofac J. 2017;54(5):540–554. doi:10.1597/15-292
- Denadai R, Lo LJ. Patient-reported outcome measures as driving elements toward value-based patient-centered care for cleft-craniofacial conditions: a call for multidisciplinary-based action. J Formos Med Assoc. 2020;119(12):1728–1730. doi:10.1016/j.jfma.2020.05.034
- Klassen A, Wong Riff K, McMaster University and the hospital for sick children. CLEFT-Q; 2018. Available from: https://qportfolio.org/cleft-q/. Accessed December, 2021.
- ICHOM. Patient-centered outcome measures: cleft lip & palate. Available from: https://connect.ichom.org/patient-centered-outcome-measures/cleft-lip-palate/. Accessed July 10, 2024.
- Bokhour BG. Communication in interdisciplinary team meetings: what are we talking about? J Interprof Care. 2006;20(4):349–363. doi:10.1080/13561820600727205
- Hahlweg P, Didi S, Kriston L, Härter M, Nestoriuc Y, Scholl I. Process quality of decision-making in multidisciplinary cancer team meetings: a structured observational study. BMC Cancer. 2017;17(1):772. doi:10.1186/s12885-017-3768-5
- Wihl J, Rosell L, Carlsson T, Kinhult S, Lindell G, Nilbert M. Medical and nonmedical information during multidisciplinary team meetings in cancer care. Curr Oncol. 2021;28(1):1008–1016. doi:10.3390/curroncol28010098
- Rosell L, Wihl J, Hagberg O, Ohlsson B, Nilbert M. Function, information, and contributions: an evaluation of national multidisciplinary team meetings for rare cancers. Rare Tumors. 2019;11:2036361319841696. doi:10.1177/2036361319841696
- Fox LM, Stone PA. Examining the team process: developing and sustaining effective craniofacial team care. In: Berkowitz S, editor. Cleft Lip and Palate. Berlin, Heidelberg: Springer; 2013:885–906.
- Shaw A, de Lusignan S, Rowlands G. Do primary care professionals work as a team: a qualitative study. J Interprof Care. 2005;19(4):396–405. doi:10.1080/13561820500053454
- Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc. 2019;111(4):383–392. doi:10.1016/j.jnma.2019.01.006
- LaVeist TA, Pierre G. Integrating the 3Ds--social determinants, health disparities, and health-care workforce diversity. Public Health Rep. 2014;129(Suppl 2):9–14. doi:10.1177/00333549141291S204
- Slavkin HC, Sanchez-Lara PA, Chai Y, Urata M. A model for interprofessional health care: lessons learned from craniofacial teams. J Calif Dent Assoc. 2014;42(9):637–644.
- Strauss RP, Broder H. Interdisciplinary team care of cleft lip and palate: social and psychological aspects. Clin Plast Surg. 1985;12(4):543–551. doi:10.1016/S0094-1298(20)31638-2
- Hlongwa P, Rispel LC. Interprofessional collaboration among health professionals in cleft lip and palate treatment and care in the public health sector of South Africa. Hum Resour Health. 2021;19(1):25. doi:10.1186/s12960-021-00566-3
- Mohamedbhai H, Fernando S, Ubhi H, Chana S, Visavadia B. Advent of the virtual multidisciplinary team meeting: do remote meetings work? Br J Oral Maxillofac Surg. 2021;59(10):1248–1252. doi:10.1016/j.bjoms.2021.05.015
- Bennett AA, Campion ED, Keeler KR, Keener SK. Videoconference fatigue? Exploring changes in fatigue after videoconference meetings during COVID-19. J Appl Psychol. 2021;106(3):330–344. doi:10.1037/apl0000906
- Andrews M, Allen G, Alexander A, French B, Wilkinson C, Mason A. Evolution of a virtual multidisciplinary cleft and craniofacial team clinic during the COVID-19 pandemic: children’s hospital Colorado experience. Cleft Palate Craniofac J. 2021;58(5):653–657. doi:10.1177/1055665620961904