Abstract
Background
In recent years, research on dysphagia has gained significant traction as one of the key topics of oral health research pertaining to the aged. Numerous academics have studied dysphagia in great detail and have produced numerous excellent scientific research findings.
Objective
To review the literature regarding dysphagia in community-dwelling older adults and identify the knowledge and trends using bibliometric methods.
Methods
The literature on dysphagia in older adults in the community was gathered from the Web of Science Core Collection (WoSCC), with inclusion criteria specifying English-language publications. The retrieval deadline was November 28, 2022. We extracted the following data: title, year, abstract, author, keywords, institution, and cited literature, and used CiteSpace (version 6.1.R3) to visualize the data through the knowledge map, burst keyword analysis, cluster analysis, and collaborative network analysis.
Results
A total of 979 articles and reviews were retrieved. Regarding productivity, the top 2 countries were the United States (n =239) and Japan (n =236). Hidetaka Wakabayashi (n =26) was one of the most prolific writers. The first paper in the frequency ranking of references cited was a white paper: European Society for Swallowing Disorders and European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome (n =53). “Prevalence” (n =173), “risk factor” (n =119), and “aspiration pneumonia” (n =108) were the most frequently occurring keywords (excluding defining nouns). The study identified reliability, tongue pressure, home discharge, and swallowing function as research hotspots from 2020 to 2022.
Conclusion
Prevalence, risk factors, and pneumonia are significant areas of study. Tongue pressure and sarcopenia are research hotspots and potential targets. In the future, research on dysphagia needs to refine strategies for prevention and control, as well as provide tertiary preventative services.
Introduction
In 2016, the FDI World Dental Federation introduced a revised description of oral health, stating that it encompasses various aspects such as communication, facial expressions, olfaction, gustation, tactile sensation, mastication, deglutition, and emotional expression, all performed effortlessly. These functions occur without pain, unease, or illness within the craniofacial structure.Citation1 Dysphagia is a specialized area within the field of oral health, specifically focusing on the impaired movement of food masses or liquids from the mouth to the stomach during swallowing. These challenges include oropharyngeal dysphagia, which can manifest as drooling, coughing, choking, nasal regurgitation, trouble starting to swallow, or needing to swallow several times to get food out of the mouth. There is also esophageal dysphagia, where the individual typically does not have difficulty swallowing but experiences a sensation of food being stuck after swallowing.Citation2,Citation3 Aging causes changes in swallowing that are physiological, structural, and neuromodulatory. Several factors, such as muscle loss, neurological dysfunction, decreased salivary secretion, and medication-induced dry mouth, contribute to reduced swallowing efficiency. Specific manifestations include reduced quality and strength of swallowing muscles, impaired movement ability of the tongue, lips, and throat, insufficient mixing of food with saliva, slow tongue movement of the food mass, and delayed laryngeal gag reflex.Citation4,Citation5 Consequently, older people are more likely to have dysphagia. According to data from previous studies, researchers have found that about 25 to 38% of older adults living alone have dysphagia.Citation6 About one-third of older adults live in the community and suffer from dysphagia. The prevalence of dysphagia is found to be 30.52% (95% CI = 21.75% to 40.07%, I2 = 68%).Citation7 It is more likely for older adults to exhibit symptoms such as decreased saliva production, atrophy of the pharynx and esophagus, loss of oral sensitivity, loss of muscle mass and strength, and worsening dental problems compared to younger and middle-aged people.Citation8 All of these things raise the risk of dysphagia. Previous studies have linked dysphagia to nutritional deficiencies, aspiration pneumonia, asphyxia, mortality, and prolonged hospital stays.Citation9,Citation10
In this study, community-dwelling older adults refer to members of a social group residing in a certain geographic area who are older than a specified age criterion, which may be 60 or 65 years old in different studies and years.Citation11 Community-dwelling older adults comprise a substantial proportion of the population affected by dysphagia. Many scholars have conducted in-depth research on swallowing problems and published numerous articles on this population. A substantial body of literature is available for bibliometric analysis. Through bibliometric analysis, it is possible to help understand the dynamic process of dysphagia through extensive data, identify future trends, aid treatment and nursing decisions, and enhance symptom management practices for community-dwelling senior citizens experiencing dysphagia.Citation12 There should be a greater focus on the bibliometric analysis of dysphagia in older adults living in the community.
Many scholars have reviewed the literature in this field, including reliable assessment, treatment, nutritional management, sarcopenia, aging, and other related but scattered topics. Therefore, to understand the research hotspots and frontiers of dysphagia among community-dwelling older adults and guide targeted research, we analyzed relevant scientific findings and conducted a visual review of the literature.
Bibliometrics is an interdisciplinary subject of quantitative analysis knowledge carrier, focusing on quantitative comprehensive knowledge systems. Bibliometrics assesses the volume of literature (including various publications, particularly journal articles), the number of contributors (including countries, institutions, groups, or individuals), and the number of terms (document identifiers, mostly keywords) to chart the course of a field, depict main trends, and highlight areas that require further investigation.Citation13 Such analyses are crucial for providing a comprehensive view of the advancements made thus far and identifying possible directions for further research. The implementation of bibliometrics relies on CiteSpace software. CiteSpace is a scientific analysis software package comprising co-countries or regions, co-authors, co-institutes, co-citations, and co-occurrence keywords used to analyze trends and identify research hotspots. It uses a combined compendium of information to analyze separate parts, applying similarity algorithms to create visual representations that cover various time dimensions.Citation14 This enables the clear observation of evolutionary paths and significant shifts within the academic domain. CiteSpace has been applied in areas such as regenerative medicine,Citation15 the identification of disruptive innovation, and emergent technology.Citation16 Nevertheless, there is an absence of a systematic evaluation and summary of the attributes, study fields, focal points of research, and collaboration related to dysphagia in older individuals residing in the community.
This study is designed to conduct a bibliometric analysis of dysphagia in community-dwelling older adults, with a focus on the subsequent four questions: (i) Which countries or regions, authors, institutions, and cited references have the highest impact in the field of dysphagia? (ii) Which keywords receive the most attention, and how are they clustered? (iii) Among community-dwelling older adults, what are the current research hotspots and prospective trends in the field of dysphagia? (iv) What recommendations can be provided for health managers?
Research Framework and Methods
Research Steps and Framework
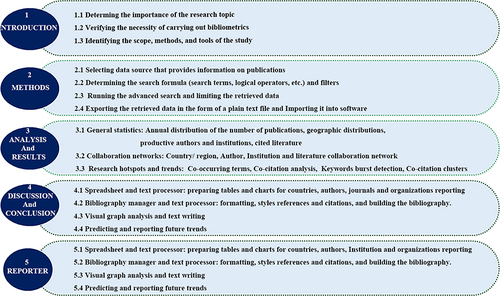
This report summarized the relevant articles published in the Web of Science Core Collection from 2002 to 2022 using bibliometrics and knowledge visualization techniques, providing a comprehensive research framework that can guide future research. The structured procedure is depicted in . After extensive Discussions, referencing other bibliometric articles, and consulting with experts, our research team finally determined the feasibility of this systematization process, which helps minimize the probability of making an error and allows for process feedback.Citation17 The following are detailed steps for putting our approach into action ().
Data Source
We used CiteSpace 6.1.R3 to analyze visualizations and bibliometrics. The publications were retrieved from the Web of Science Core Collection (WoSCC), including the Science Citation Index Expanded, Conference Proceedings Citation Index – Social Science & Humanities, Arts & Humanities Citation Index, Conference Proceedings Citation Index – Science, Emerging Sources Citation Index, Social Sciences Citation Index, Current Chemical Reactions, and Index Chemicus.
Search Strategy
The operator “or” was used in our retrieval to create three lists of all search terms, and the operator “and” was used to merge the three lists. The search structure for the first list was as follows: Topic = (aged OR aging OR age OR geriatric OR geriatrics OR old OR older OR elderly OR senior OR seniors). The following search structure was present in the second list: Topic = (deglutition disorders OR dysphagia OR swallowing disorder OR swallowing impairment OR swallowing dysfunction OR oropharyngeal dysphagia OR esophageal dysphagia). The search structure for the third list was as follows: Topic = (community OR communities OR communal OR reside OR residential OR home). Document type = article and review article; Timespan (custom year range) = 2002–2022; Language = English; Retrieval deadline: November 28, 2022. We exported the retrieved records to “Plain Text File”; the exported record content was “Full Record and Cited References”.
Since the data used in this study are secondary data available in the WoSCC database via open access, neither informed permission nor ethical approval is necessary.
Methods and Analysis
CiteSpace is a visualization tool for bibliometric analysis developed by Professor Chaomei Chen.Citation18 It integrates information visualization methods, data mining algorithms, and bibliometrics to assist academics in capturing the first-hand experience of changes in their respective fields.Citation19
Before importing the data, we created a new folder consisting of four subfolders named “data”, “input”, “output”, and “project”. The data retrieved from the Web of Science were imported into the “input” folder, and the imported data were named “download_1_500” and “download_501_979” in order to be correctly recognized by the software. The data were then imported into CiteSpace for deduplication (the data remained unchanged before and after deduplication) and visualization operations.
The parameters of CiteSpace were as follows: (1) time = January 2002 to December 2022; (2) years per slice = 1; (3) term source = Title/ Abstract/ Author/ Keywords/ Keywords plus. Only one node was selected at a time. The visualized network map consisted of nodes and links, with the size indicating the number of publications or frequency of citations and the colour showing the time of the first co-occurrence or co-citation, with warm hues indicating later times.Citation20 The lines connecting nodes represented the co-citation or co-occurrence relationships.Citation21 Nodes with a relatively high centrality may be the key or essential turning points in this field, as centrality represents the influence of a node on other nodes.Citation22 In order to achieve the best balance between the accuracy of node connections and the overall readability of the visual graph, the researchers finally generated the network graph after several debugging.
The growth rate of the number of publications was calculated according to the following formula:Citation23
Results
Annual Publications
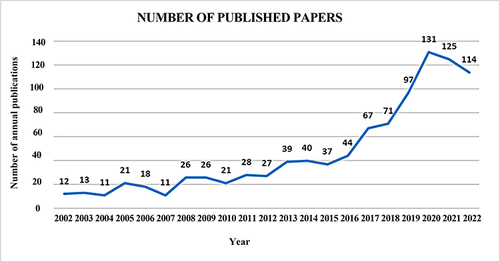
Nine hundred seventy-nine publications on dysphagia among community-dwelling older adults were retrieved, including 880 articles (90%) and 99 reviews (10%). shows the Results of the number of publications. While there were fluctuations in the number of publications during the study period, the overall growth rate was relatively rapid. The growth trend of the publications can be roughly divided into three stages: a fluctuating slow development from 2002 to 2015 with a growth rate of 9%. At this stage, 330 articles had been published, accounting for 34% of all publications; there had been an explosive growth from 2016 to 2020, with a growth rate of 31%, especially from 2018 to 2020. At this point, 410 articles had been published, making up 42% of the total, a growth rate of −9% between 2021 and 2022 with a slight fall. Two hundred thirty-nine articles had been published at this stage, comprising 24% of the total publications.
Co-Country
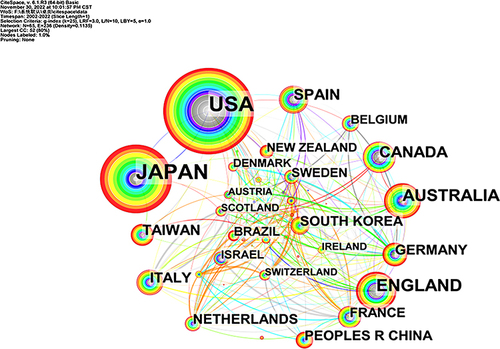
displays the locations of countries or regions that published dysphagia in the literature related to community-dwelling older adults from 2002 to 2022, based on WoSCC data. A colour-coded visual map of the distribution of relevant literature is shown in , which features the international cooperation network, and the top 10 productive countries or regions with many records on dysphagia in community-dwelling older adults are shown in .
Table 1 Top10 Productive Countries or Regions
illustrates the cooperative networks of the productive countries or regions; the merged network consists of 65 nodes and 236 links. The node size represents the number of publications, and the lines connecting the nodes reveal the cooperative relationships between countries or regions. The United States occupies the largest nodes and extends many links. Thus, it had the advantage of a large number of articles and abundant international cooperation. At the same time, we obtained the top 10 productive countries or regions from 2002 to 2022 (), of which the United States had the highest productivity, followed by Japan, the UK, Australia. The fourth column of the table presents information on national centrality, with the United States obtaining the highest centrality score of 0.38 points, followed by Australia (0.29 points). These results indicate that the United States and Australia played an intermediary role in the international cooperation network.
In a network, centrality is the degree of nodes that form a path between any two nodes; a node with a centrality of more than 0.1 is considered to be the key node.
Co-Authorship
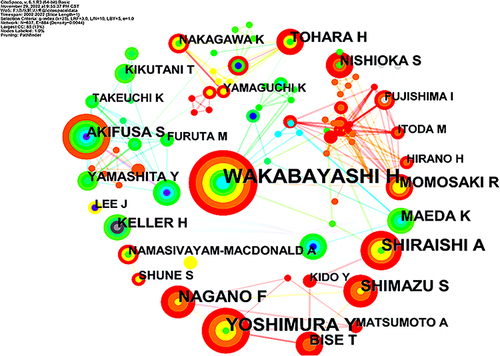
The authors’ cooperation network, which has 644 nodes and 956 links, is shown in . Each node represents one author, and the links between the nodes represent the collaborative relationship between the authors. The node size represents the number of articles published by the authors. shows data on the number of publications and the centrality of the top 10 authors for productivity. Even authors with large numbers of publications did not necessarily have a high centrality. There was a lack of a mature multilateral cooperation network among authors, and most academic cooperation was limited to two parties.
Table 2 Top10 Active Authors in Research of Dysphagia in Community-Dwelling Older Adults
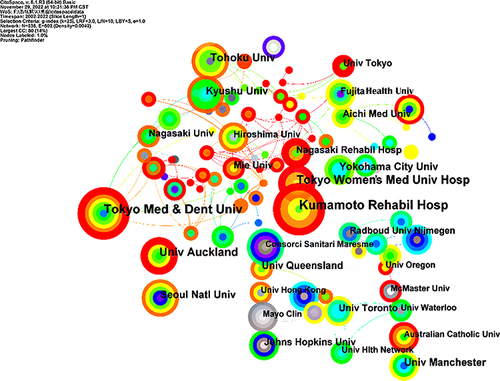
Co-Institute
We drew a diagram of institutional cooperation shown in , which consists of 536 nodes and 718 links. A total of 979 articles were published across 536 institutions. The top 10 institutions were: Kumamoto Rehabilitation Hospital, Tokyo Medical and Dental University, Tokyo Women’ s Medical University Hospital, The University of Auckland, Tohoku University, Yokohama City University, Seoul National University, Kyushu University, The University of Manchester, and The University of Queensland (). Six of these research institutions are in Japan, and seven are in East Asia. Overall, studies on dysphagia among community-dwelling older adults were more active in Japan, and the scope has been expanded to countries such as Korea and China. Most of the research institutions were universities, with a few hospitals. Thus, the university undertook the main task of scientific research.
Table 3 Top10 Productive Institutes in Research of Dysphagia in Community-Dwelling Older Adults
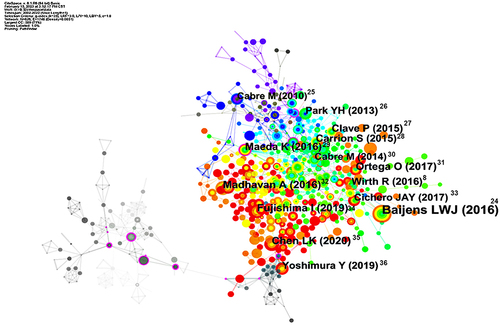
Cited Reference
The network diagram of the cited references includes 826 nodes and 2838 links (). References with more than twenty citations are presented on the map.Citation8,Citation24–36 The more references are cited, the larger the node. As can be seen, Baijens LWJ (2016) has the largest node, indicating that he has produced outstanding contributions in this area of study, which have significantly impacted the study of dysphagia research in community-dwelling older adults. In , there are multiple nodes with purple rings outside (for example, purple rings in the gray area at the lower left corner of the figure), representing literature with high centrality in this field. While centrality represents the structural attribute of scientific discovery, a node with high centrality may correspond to a transformative scientific discovery.
The top 10 cited references with the highest citation frequency and centrality are shown in and . In , the first-ranked cited reference was the European Society for Swallowing Disorders and European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome, published in Clinical Interventions in Aging.Citation24 Regarding the centrality of the cited reference (), Sellars C.’s cohort study of chest infections in stroke patientsCitation37 came first. By analyzing the cited literature, we found that studies on dysphagia in community-dwelling older adults focused on various domains such as pneumonia, stroke, dementia, sarcopenia, etc.Citation38–41
Table 4 Top10 High Cited References
Table 5 Top10 Cited References for the Highest Centrality
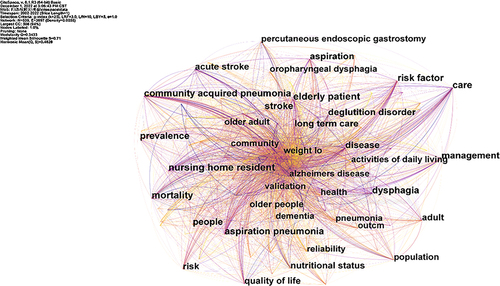
Co-Occurring Keywords Analysis
The keyword co-occurrence network has 539 nodes and 3697 links (). shows that the high-frequency keywords included the following related definitions and classifications: Oropharyngeal dysphagia, dysphagia, and deglutition disorder were common definitions, and stroke, dementia, Alzheimer’s disease, and older adult were linked risk factors. It also covered impacts and outcome measures such as prevalence, mortality, quality of life, nutritional status, activities of daily living, aspiration pneumonia, and community-acquired pneumonia. The content related to prognoses included management, percutaneous endoscopic gastrostomy, and long-term care.
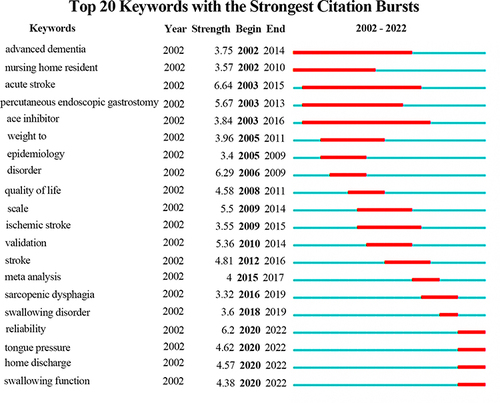
shows the top 10 keywords in research on dysphagia among community-dwelling older adults from 2002 to 2022. The keywords “dysphagia” held the highest attention. Furthermore, researchers can understand the change of dynamics in research hotspots preliminarily. shows the top 20 keywords with the most significant number of citation bursts and the lengths of each burst. From , the hot topics of the last three years were reliability, tongue pressure, home discharge, and swallowing function.
Table 6 Top10 Keywords in Research of Dysphagia in Community-Dwelling Older Adults
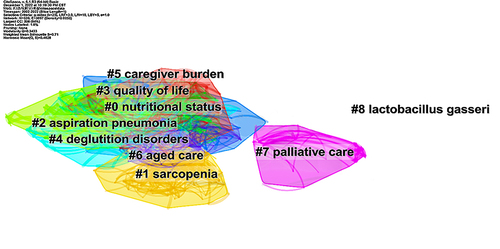
Keyword Clustering
CiteSpace generated nine clusters and drew a cluster map by analyzing the keywords. The modularity score Q is 0.3433 >0.3, and the mean silhouette score S is 0.71 >0.7. Therefore, the clustering network was highly consistent, and the result was convincing. In , there are nine labels representing 9 clusters. The labels of each cluster are keywords in the co-occurrence network, and the serial number of the cluster ranges from # 0 to # 8. The number of keywords in the cluster grows as the serial number decreases. Nutritional status was the most significant cluster. The remaining clusters in the top 5 clusters were sarcopenia, aspiration pneumonitis, quality of life, and deglutition disorder, including internal and external factors, which were the main content of this research area.
Discussion
Through visual analysis of 979 publicly published literature over the last 20 years, we showed the number of publications, countries/regions, high-productivity authors, institutions, co-cited literature, keywords, and other contents of dysphagia research among community-dwelling older adults. In general, dysphagia is relatively common in the community-dwelling older adult population and is found to reduce quality of life significantly.Citation50 The problem of dysphagia in community-dwelling older adults has drawn more attention over the past five years, and countries around the world have intensified their research on this topic.
Growth and Development of Publications
Research related to dysphagia among community-dwelling older adults has been growing slowly and floatingly between 2002 and 2015, a phase of problem identification and the accumulation of knowledge. During this phase of research (2002–2015), dysphagia was identified as one of the functional manifestations of neurodegenerative diseases such as Parkinson’s diseaseCitation51 and Alzheimer’s diseaseCitation52 and cerebrovascular diseases such as stroke,Citation53–55 and epidemiologic investigations such as the prevalence were carried out. Later in this period (2008–2011), research on the dysphagia-related quality of lifeCitation56 gained more attention, and the research framework began to be enriched. Between 2016 and 2020, which supplied 42% of all literature in just five years, was characterized by rapid expansion in the number of publications. Reviews, including meta-analyses, were conducted based on the results of previous studies to examine this topic from a comprehensive perspective. In addition, the study of sarcopenic dysphagia had begun to gain more attention at this time (2016–2020); for example, anabolic signals, catabolic signals, and age-related muscle fibrosis,Citation57 increasingly appeared in studies of swallowing muscles, and a breakthrough was achieved in the extensive research into the mechanism of dysphagia. Finally, there has been a negative trend in the number of publications in the last two years (2021–2022). Given the impact of the COVID-19 epidemic, the physical state of community-dwelling older adults is not well suited for participation in research studies, and attention to oral health is distracted. As a result, the number of relevant publications decreased but remained high during this period (2021–2022). The effect of tongue pressureCitation58 on dysphagia was also investigated. So far, the research framework for dysphagia in community-dwelling older adults includes prevalence, assessment, risk factors, disease mechanism, adverse outcomes, and intervention measures. Cohort studies and cross-sectional studies make up the majority of the study designs. Overall, there is a growing trend in the number of publications on dysphagia among older people living in communities, and the research’s focus is becoming more in-depth. There is reason to assume that the growth rate of publications will be higher in the future as the impact of the COVID-19 pandemic will be mitigated, as aging increases worldwide, and as interest in scientific research and oral health is rekindled.
Analysis of Publication Characteristics
Researchers from 65 countries and regions worldwide have been drawn to dysphagia in community-dwelling older adults. The top 5 most productive countries were all developed countries, with both the United States and Japan having absolute productivity advantages, and this result was consistent with the conclusion of Rech.Citation59 In addition, the data in the cooperative network and table show that all the authors and most of the high-productivity institutions were located in Japan. While the United States and Japan had similar numbers of publications, the United States produced the most significant number of publications and established more academic contacts due to its more prominent number of scholars and institutions. Therefore, it held a higher central position within the nation. Japan had more concentrated research resources (including research institutions and researchers) than the United States, making it better able to ensure the continuity and consistency of study and allowing it to deliver more mature research results continuously. However, Japan needed more cooperation with other countries. More global, multilateral academic cooperation is still required.
Hidetaka Wakabayashi ranked highest regarding the number of publications. He focused on the study of sarcopenic dysphagia. From 2014 to 2015, he was involved in a cross-sectional study that determined the connection between stroke-related sarcopenia and poor oral status.Citation60 In 2019, one of his retrospective cohort studies clearly stated that: Sarcopenia was associated with worse recovery of dysphagia,Citation36 and in 2021, his scoping review stated that the diagnostic algorithm for sarcopenic dysphagia was the only reliable method to diagnose sarcopenic dysphagia (in patients aged 65 years and older who could follow commands).Citation61,Citation62 In the same year, Hidetaka Wakabayashi participated in the construction and quality evaluation of the Japanese sarcopenic dysphagia database.Citation63 To date, his research has been focused on exploring the connection between sarcopenia and poor oral health, identifying the relationship between sarcopenia and dysphagia, defining the diagnostic criteria for sarcopenic dysphagia, and establishing the Japanese database of sarcopenic dysphagia. It was a well-structured study, with research ranging from shallow to profound. In addition, dysphagia-related assessment, diagnosis, sarcopenia, stroke, nutritional status, aspiration pneumonia, rehabilitation, and functional recovery were topics that the top 10 active authors focused on more often. In terms of countries and regions, all the top 10 active authors, including Hidetaka Wakabayashi, were affiliated with Japanese institutions. Japan had a significant advantage in conducting research on dysphagia among community-dwelling older adults. Japan’s super-aged society,Citation64 in which dysphagia was a prominent issue among community-dwelling older adults, enabled them to allocate more resources to research in this field. Finally, it was worth noting that even the authors with high publication counts did not have high degrees of centrality and failed to play a bridging role between co-authorship. In the visualization of networks ( and ), many authors and institutions preferred to form a stable cooperative group within a small scope of practice.
The most cited references are generally considered to form the basis of a research field.Citation19 We analyzed the most cited literature, the European Society for Swallowing Disorders and European Union Geriatric Medicine Society white paper:Citation24 Oropharyngeal dysphagia as a geriatric syndrome. In this study, the panel argued over whether dysphagia should be included in the spectrum of geriatric syndromes and came to the conclusion that it should. At the same time, we should also be clear that dysphagia without an obvious etiology requires proper attention if only to be imprecisely blamed on aging, as this may compromise older people’s entitlement to health care.Citation65 Furthermore, the document stated that oropharyngeal dysphagia (OD) was associated with multiple comorbidities and a poor prognosis, requiring multidimensional intervention. The top ten highly cited references focused on dysphagia’s pathophysiology, assessment and diagnosis, prevalence, risk factors, and relationship to sarcopenia and malnutrition. These themes essentially reflected the current trends in this field, highlighting the key concerns related to clinical diagnosis, care, and patient management. The majority of the top 10 citations were published in Clinical Interventions in Aging (two articles, IF = 3.829), Journal of the American Medical Directors Association (two articles, IF = 7.802), and Geriatrics & Gerontology International (two articles, IF = 3.387). Therefore, it is clear that the above periodicals played an essential role in disseminating and sharing related research on dysphagia in community-dwelling older individuals. Scholars can acquire related knowledge about it by reading the periodicals mentioned above. The literature with the highest centrality: Risk factors for chest infection in acute stroke: a prospective cohort study. In this cohort study, while dysphagia was a significant risk factor for the development of pneumonia, it was both a necessary and an insufficient condition for pneumonia, suggesting that some potential confounders enhanced the effect of dysphagia on the occurrence of pneumonia. The critical node connecting different topic structures is likely the turning point of knowledge or the inflection point.Citation66 This study expanded the pneumonia prevention and therapy concept by showing a link between dysphagia and pneumonia. Overall, the top 10 cited references of centrality played a significant mediating role in linking dysphagia to other diseases such as stroke, pneumonia, dementia, Parkinson’s disease, sarcopenia, and frailty.Citation27,Citation67–69
Research Hotspots and Emerging Trends
Co-occurring keywords and their frequency may reflect the main content and the core theme.Citation70 The analysis of and reveals that the research on dysphagia in community-dwelling older adults focused on the prevalence, etiologies (stroke, Alzheimer’s disease, etc). risk factors (sarcopenia, malnutrition, etc). and pneumonia (aspiration pneumonia, community-acquired pneumonia), which were the main research hotspots in this field.
In and , the hot topics switched from advanced dementia, acute stroke, and percutaneous endoscopic gastrostomy to epidemiology, disorder, quality of life, scale, and finally to meta-analysis, reliability, tongue pressure, home discharge, and swallowing function. There have been studies of dysphagia in community older adults who appear to have undergone the following processes. The issue of dysphagia was discovered in persons with particular conditions (dementia, stroke).Citation44,Citation54 After epidemiologic research and studies on the impact of dysphagia (quality of life, disorder),Citation71 it was understood that dysphagia could be measured (scale).Citation72 Finally, many advanced procedures were carried out, including a meta-analysis of primary data, research of the mechanism (sarcopenic dysphagia, tongue pressure),Citation58,Citation73 the validity of the assessment tools, the prognosis and functional recovery (swallowing function, home discharge).Citation36,Citation74
In the previous analysis, the “Aged Care” cluster involved the keywords “care”, “older adult”, and “nursing home resident”, along with the series and summary of the “nutritional status”, “quality of life”, “caregiver burden” and “palliative care” clusters. Therefore, in the cluster analysis, we conjecture that the implementation of scientific care and nutrition support (dysphagia, resulting in increased difficulty in eating, may result in patients having poor nutritional status).Citation75–77 for older adults with dysphagia and the management of dysphagia to reduce the incidence of complications remain the key trends. However, in this trend, we discovered that researchers mainly focused on managing and intervening in dysphagia after its occurrence and that less research involved primary prevention. In China, the first comprehensive management strategy for dysphagia in older adults based on the Delphi method was “SATIA”,Citation78 which included five components: screening, assessment, training, interventions, and management. It initially standardized the comprehensive management and provided theoretical support for improving the tertiary prevention system of dysphagia in older adults in China. However, the current evidence supporting comprehensive prevention and treatment strategies for dysphagia in community-dwelling older adults still needs to be improved. Moreover, the practical application value of the existing comprehensive strategies requires further research and the design of larger cohorts. Therefore, in the future, researchers should intensify their research on the primary prevention, including nutrition support, prospective oral health screening and maintenance, etc., of dysphagia among the comprehensive tertiary prevention strategies to give full play to the subjective initiative of older adults in preventing or delaying dysphagia and to enrich the evidence and validate their practical application value.
The studies of dysphagia continually deepened and refined from the study of general symptoms to the specific assessment; both conducted mechanism and detailed clinical research; and the content involved physiology, psychology, and society, but it could still be improved. For the study of dysphagia, it is necessary to explore the fundamental mechanisms and explain the occurrence and development of dysphagia at the cellular or molecular level. For example, aging leads to a decrease in satellite cell (mononuclear skeletal muscle precursor cells) content,Citation79 hindering satellite cell activation and thus impairing the regeneration of skeletal muscle fibers. Furthermore, as age advances, the skeletal muscle experiences an increase in oxidized proteins. This results in a poor accumulation of lipofuscin and cross-linking proteins, ultimately leading to a decrease in both the quality and quantity of skeletal muscle.Citation80 Currently, most of these studies focus on sarcopenia and were introduced into the field of dysphagia with the definition of sarcopenic dysphagia. Swallowing is a complex process involving over 30 muscles and numerous nerves in the oral cavity, pharynx, larynx, and esophagus.Citation81 Among these, the supraglottic and extrinsic muscles play a vital role in the upward movement of the hyoid bone to create pressure between the tongue and the hard palate.Citation82 This has a significant impact on tongue pressure. A series of degenerative changes in skeletal muscles mentioned above may also partly explain the changes in tongue pressure at the molecular and cellular levels. In future research, studies of muscle anabolism could target swallowing muscles and may also extend to areas such as neuromodulation, biomarkers, and fatty infiltration.
Hence, it is necessary to develop cellular and molecular research to achieve breakthroughs in the prediction, rapid identification, diagnostic staging, and prognostic evaluation of dysphagia in the future. Thus, according to the evolution law of keyword outbreak, the following hot trends can be inferred:
Research at the molecular and cellular level, as well as standardized testing for tongue pressure and dysphagia;
The development of new assessment tools;
Primary prevention, functional recovery and healthcare for older adults with dysphagia;
Limitations
Certain Limitations to our study need to be acknowledged. First, while we believe that the WoS database could provide a sufficient number of vital publications, the lack of proprietary publications in other databases might be detrimental to the completeness of the analysis results. Second, our analysis excluded non-English language publications and did not include gray literature such as conference articles, books, newspapers, and retracted papers, which may have missed some studies. Third, some high-quality publications in recent years have yet to achieve high citation counts due to the limitation of retrieval years because a higher citation count is time-consuming. Finally, because bibliometric analysis mainly relies on citation metrics, it cannot fully assess the inherent quality of individual papers. Therefore, future research can incorporate more databases, including the Google Database, Medline, PubMed, and Scopus. It is also advisable to increase the analysis of grey literature, consider studies in multiple languages, and maintain regular updates to mitigate the delay in exploring new scientific frontiers.
Conclusion
Overall, research on dysphagia in community-dwelling older adults has grown in range and depth. The United States and Japan had more significant influence and involvement in this field, but the cooperation still needed to be improved. A solid cooperative connection between countries, institutions, and authors must be established and maintained. In the realm of basic research, the mechanisms at the molecular and cellular levels that may involve tongue pressure, sarcopenia, and numerous other aspects still need to be complemented. As far as health care is concerned, aged care encompasses a multidimensional field of study characterized by a diverse set of keywords and keyword clusters. These include terms such as “care”, “older adult”, “nursing home resident”, “nutritional status”, “quality of life”, “caregiver burden”, and “palliative care”. Consequently, it necessitates greater attention. Furthermore, prevalence, risk factors, and pneumonia are important research topics, and they may have high potential in the future. Lastly, tertiary prevention strategies should be improved step by step to increase dysphagia prevention and control at the community level. Future studies on dysphagia in community-dwelling older adults will concentrate on promoting senior wellness and achieving healthy aging.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors affirm that the research was carried out without any commercial or financial affiliations that could be seen as a potential conflict of interest.
Acknowledgments
The authors would like to thank Prof. C. M. Chen for his theoretical and technical support for bibliometrics. We acknowledge the anonymous reviewers for their helpful remarks. This work was supported by the public welfare projects of Zhejiang Provincial Science and Technology Department, China (LGF21G010005).
Additional information
Funding
References
- Hescot P. The new definition of oral health and relationship between oral health and quality of life. Chin J Dent Res. 2017;20(4):189–192. doi:10.3290/j.cjdr.a39217
- Yang RY, Yang AY, Chen YC, et al. Association between dysphagia and frailty in older adults: a systematic review and meta-analysis. Nutrients. 2022;14(9):1812. doi:10.3390/nu14091812
- Wilkinson JM, Codipilly DC, Wilfahrt RP. Dysphagia: evaluation and collaborative management. Am Fam Physician. 2021;103(2):97–106.
- Barrera MAW, O’ Connor B. Presbyphagia versus dysphagia: normal versus abnormal swallowing symptoms in older adults with Parkinson disease and multiple sclerosis. Top Geriatr Rehabil. 2019;35(3):217–233. doi:10.1097/TGR.0000000000000237
- McCoy YM, Desai RV. Presbyphagia versus dysphagia: identifying age-related changes in swallow function. Perspective ASHA Spec Interest Groups. 2018;3(15):15–21. doi:10.1044/persp3.sig15.15
- Igarashi K, Kikutani T, Tamura F. Survey of suspected dysphagia prevalence in home-dwelling older people using the 10-item eating assessment tool (Eat-10). PLoS One. 2019;14(1):e0211040. doi:10.1371/journal.pone.0211040
- Doan TN, Ho WC, Wang LH, et al. Prevalence and methods for assessment of oropharyngeal dysphagia in older adults: a systematic review and meta-analysis. J Clin Med. 2022;11(9):2605. doi:10.3390/jcm11092605
- Wirth R, Dziewas R, Beck AM, et al. Oropharyngeal dysphagia in older persons-from pathophysiology to adequate intervention: a review and summary of an international expert meeting. Clin Interv Aging. 2016;11:189–208. doi:10.2147/CIA.S97481
- Morisaki N. Relationship between swallowing functions and health-related quality of life among community-dwelling dependent older individuals. Jpn J Nurs Sci. 2017;14(4):353–363. doi:10.1111/jjns.12168
- Thiyagalingam S, Kulinski AE, Thorsteinsdottir B, et al. Dysphagia in older adults. Mayo Clin Proc. 2021;96(2):488–497. doi:10.1016/j.mayocp.2020.08.001
- Huang CJ, Hsu NW, Chen HC. Prevalence, dimensions, and correlates of excessive daytime sleepiness in community-dwelling older adults: the Yilan study, Taiwan. Ann Med. 2024;56(1):2352028. doi:10.1080/07853890.2024.2352028
- Clancy TR, Gelinas L. Knowledge discovery and data mining: implications for nurse leaders. J Nurs Adm. 2016;46(9):422–424. doi:10.1097/NNA.0000000000000369
- Wang C, Zhu H, Li Y, et al. Bibliometric analysis of the gut microbiota and stroke from 2002 to 2022. Heliyon. 2024;10(9):e30424. doi:10.1016/j.heliyon.2024.e30424
- Chen C. CiteSpace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. 2005;57(3):359–377. doi:10.1002/asi.20317
- Chen C, Hu Z, Liu S, et al. Emerging trends in regenerative medicine: a scientometric analysis in citespace. Expert Opin Biol Ther. 2012;12(5):593–608. doi:10.1517/14712598.2012.674507
- Li M, Porter AL, Suominen A. Insights into relationships between disruptive technology/innovation and emerging technology: a bibliometric perspective. Technol Forecast Soc Change. 2018;129:285–296. doi:10.1016/j.techfore.2017.09.032
- Maia SC, de Benedicto GC, Do Prado JW, et al. Mapping the literature on credit unions: a bibliometric investigation grounded in Scopus and web of science. Scientometrics. 2019;120:929–960. doi:10.1007/s11192-019-03165-1
- Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101(Suppl):5303–5310. doi:10.1073/pnas.0307513100
- Wu MQ, Wu DQ, Hu CP, et al. Studies on children with developmental coordination disorder in the past 20 years: a bibliometric analysis via citespace. Front Psychiatry. 2021;12:776883. doi:10.3389/fpsyt.2021.776883
- Liang YD, Li Y, Zhao J, et al. Study of acupuncture for low back pain in recent 20 years: a bibliometric analysis via citespace. J Pain Res. 2017;10:951–964. doi:10.2147/JPR.S132808
- Zhang XL, Zheng Y, Xia ML, et al. Knowledge domain and emerging trends in vinegar research: a bibliometric review of the literature from woscc. Foods. 2020;9(2):166. doi:10.3390/foods9020166
- Chen C, Chen Y. Searching for clinical evidence in citespace. AMIA Annu Symp Proc. 2005;2005:121–125.
- Guo Y, Hao Z, Zhao S, et al. Artificial intelligence in health care: bibliometric analysis. J Med Internet Res. 2020;22(7):e18228. doi:10.2196/18228
- Baijens LW, Clavé P, Cras P, et al. European society for swallowing disorders and European Union geriatric medicine society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403–1428. doi:10.2147/cia.s107750
- Cabre M, Serra-Prat M, Palomera E, et al. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing. 2010;39(1):39–45. doi:10.1093/ageing/afp100
- Park YH, Han HR, Oh BM, et al. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs. 2013;34(3):212–217. doi:10.1016/j.gerinurse.2013.02.014
- Clavé P, Shaker R. Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol. 2015;12(5):259–270. doi:10.1038/nrgastro.2015.49
- Carrión S, Cabré M, Monteis R, et al. Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin Nutr. 2015;34(3):436–442. doi:10.1016/j.clnu.2014.04.014
- Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatr Gerontol Int. 2016;16(4):515–521. doi:10.1111/ggi.12486
- Cabré M, Serra-Prat M, Force L, et al. Oropharyngeal dysphagia is a risk factor for readmission for pneumonia in the very elderly persons: observational prospective study. J Gerontol a Biol Sci Med Sci. 2014;69(3):330–337. doi:10.1093/gerona/glt099
- Ortega O, Martín A, Clavé P. Diagnosis and management of oropharyngeal dysphagia among older persons, state of the art. J Am Med Dir Assoc. 2017;18(7):576–582. doi:10.1016/j.jamda.2017.02.015
- Madhavan A, LaGorio LA, Crary MA, et al. Prevalence of and risk factors for dysphagia in the community dwelling elderly: a systematic review. J Nutr Health Aging. 2016;20(8):806–815. doi:10.1007/s12603-016-0712-3
- Cichero JA, Lam P, Steele CM, et al. Development of International Terminology and Definitions for Texture-Modified Foods and Thickened Fluids Used in Dysphagia Management: the IDDSI Framework. Dysphagia. 2017;32(2):293–314. doi:10.1007/s00455-016-9758-y
- Fujishima I, Fujiu-Kurachi M, Arai H, et al. Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int. 2019;19(2):91–97. doi:10.1111/ggi.13591
- Chen LK, Woo J, Assantachai P, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–307. doi:10.1016/j.jamda.2019.12.012
- Yoshimura Y, Wakabayashi H, Bise T, et al. Sarcopenia is associated with worse recovery of physical function and dysphagia and a lower rate of home discharge in Japanese hospitalized adults undergoing convalescent rehabilitation. Nutrition. 2019;61:111–118. doi:10.1016/j.nut.2018.11.005
- Sellars C, Bowie L, Bagg J, et al. Risk factors for chest infection in acute stroke: a prospective cohort study. Stroke. 2007;38(8):2284–2291. doi:10.1161/strokeaha.106.478156
- Savas S, Yilmaz M. Self reported dysphagia is not associated with sarcopenia defined by the revised Ewgsop2 Criteria and regional thresholds at the hospital among ambulatory older patients. Mater Sociomed. 2019;31(4):253–257. doi:10.5455/msm.2019.31.253-257
- Wästfelt M, Cao Y, Ström JO. Predictors of post-stroke fever and infections: a systematic review and meta-analysis. BMC Neurol. 2018;18(1):49. doi:10.1186/s12883-018-1046-z
- Andrade PA, Santos CAD, Firmino HH, et al. The Importance of dysphagia screening and nutritional assessment in hospitalized patients. Einstein. 2018;16(2):eAO4189. doi:10.1590/s1679-45082018ao4189
- Fırat Ozer F, Akın S, Soysal T, et al. Relationship between dysphagia and sarcopenia with comprehensive geriatric evaluation. Dysphagia. 2021;36(1):140–146. doi:10.1007/s00455-020-10120-3
- Almirall J, Bolíbar I, Serra-Prat M, et al.; Community-Acquired Pneumonia in Catalan Countries (PACAP) Study Group. New evidence of risk factors for community-acquired pneumonia: a population-based study. Eur Respir J. 2008;31(6):1274–1284. doi:10.1183/09031936.00095807
- Almirall J, Cabré M, Clavé P. Neumonía aspirativa [Aspiration pneumonia]. Med Clin. 2007;129(11):424–432. doi:10.1157/13110467
- Logemann JA, Gensler G, Robbins J, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res. 2008;51(1):173–183. doi: 10.1044/1092-4388(2008/013)
- van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, et al. Risk factors for aspiration pneumonia in frail older people: a systematic literature review. J Am Med Dir Assoc. 2011;12(5):344–354. doi:10.1016/j.jamda.2010.12.099
- Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124(1):328–336. doi:10.1378/chest.124.1.328
- Reza Shariatzadeh M, Huang JQ, Marrie TJ. Differences in the features of aspiration pneumonia according to site of acquisition: community or continuing care facility. J Am Geriatr Soc. 2006;54(2):296–302. doi:10.1111/j.1532-5415.2005.00608.x
- Rosenvinge SK, Starke ID. Improving care for patients with dysphagia. Age Ageing. 2005;34(6):587–593. doi:10.1093/ageing/afi187
- Nogueira D, Reis E. Swallowing disorders in nursing home residents: how can the problem be explained? Clin Interv Aging. 2013;8:221–227. doi:10.2147/CIA.S39452
- Chen PH, Golub JS, Hapner ER, et al. Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia. 2009;24(1):1–6. doi:10.1007/s00455-008-9156-1
- Auyeung M, Tsoi TH, Mok V, et al. Ten year survival and outcomes in a prospective cohort of new onset Chinese Parkinson’s disease patients. J Neurol Neurosurg Psychiatry. 2012;83(6):607–611. doi:10.1136/jnnp-2011-301590
- Edahiro A, Hirano H, Yamada R, et al. Factors affecting independence in eating among elderly with alzheimer’s disease. Geriatr Gerontol Int. 2012;12(3):481–490. doi:10.1111/j.1447-0594.2011.00799.x
- Kopey SA, Chae J, Vargo MM. Does a 3-sip test detect dysphagia in acute stroke rehabilitation patients? Pm r. 2010;2(9):822–828. doi:10.1016/j.pmrj.2010.05.015
- Teasell R, Foley N, Fisher J, et al. The incidence, management, and complications of dysphagia in patients with medullary strokes admitted to a rehabilitation unit. Dysphagia. 2002;17(2):115–120. doi:10.1007/s00455-001-0110-8
- Turner-Lawrence DE, Peebles M, Price MF, et al. A feasibility study of the sensitivity of emergency physician dysphagia screening in acute stroke patients. Ann Emerg Med. 2009;54(3):344–348. doi:10.1016/j.annemergmed.2009.03.007
- Swan K, Speyer R, Heijnen BJ, et al. Living with oropharyngeal dysphagia: effects of bolus modification on health-related quality of life--a systematic review. Qual Life Res. 2015;24(10):2447–2456. doi:10.1007/s11136-015-0990-y
- Dellis S, Papadopoulou S, Krikonis K, et al. Sarcopenic Dysphagia. A narrative review. J Frailty Sarcopenia Falls. 2018;3(1):1–7. doi:10.22540/jfsf-03-001
- Nakao Y, Yamashita T, Honda K, et al. Association among age-related tongue muscle abnormality, tongue pressure, and presbyphagia: a 3d MRI Study. Dysphagia. 2021;36(3):483–491. doi:10.1007/s00455-020-10165-4
- Rech RS, de Goulart BNG, Dos Santos KW, et al. Frequency and associated factors for swallowing impairment in community-dwelling older persons: a systematic review and meta-analysis. Aging Clin Exp Res. 2022;34(12):2945–2961. doi:10.1007/s40520-022-02258-x
- Shiraishi A, Yoshimura Y, Wakabayashi H, et al. Prevalence of stroke-related sarcopenia and its association with poor oral status in post-acute stroke patients: implications for oral sarcopenia. Clin Nutr. 2018;37(1):204–207. doi:10.1016/j.clnu.2016.12.002
- Wakabayashi H, Kishima M, Itoda M, et al. Diagnosis and treatment of sarcopenic dysphagia: a scoping review. Dysphagia. 2021;36(3):523–531. doi:10.1007/s00455-021-10266-8
- Mori T, Fujishima I, Wakabayashi H, et al. Development, reliability, and validity of a diagnostic algorithm for sarcopenic dysphagia. JCSM Clin Rep. 2017;2(2):1–10. doi:10.17987/jcsm-cr.v2i2.17
- Mizuno S, Wakabayashi H, Fujishima I, et al. Construction and quality evaluation of the Japanese sarcopenic dysphagia database. J Nutr Health Aging. 2021;25(7):926–932. doi:10.1007/s12603-021-1646-y
- Honda M, Inoue N, Liverani M, et al. Lessons learned from the history of postgraduate medical training in Japan: from disease-centred care to patient-centred care in an aging society. Hum Resour Health. 2022;20(1):54. doi:10.1186/s12960-022-00752-x
- Adelman RD, Greene MG, Ory MG. Communication between Older Patients and Their Physicians. Clin Geriatr Med. 2000;16(1):1–24. doi:10.1016/s0749-0690(05)70004-5
- Zhong D, Li Y, Huang Y, et al. Molecular mechanisms of exercise on cancer: a bibliometrics study and visualization analysis via citespace. Front Mol Biosci. 2021;8:797902. doi:10.3389/fmolb.2021.797902
- Jones CA, Colletti CM, Ding MC. Post-stroke dysphagia: recent insights and unanswered questions. Curr Neurol Neurosci Rep. 2020;20(12):61. doi:10.1007/s11910-020-01081-z
- Ebihara T. Comprehensive approaches to aspiration pneumonia and dysphagia in the elderly on the disease time-axis. J Clin Med. 2022;11(18):5323. doi:10.3390/jcm11185323
- Sakai K, Nakayama E, Yoneoka D, et al. Association of oral function and dysphagia with frailty and sarcopenia in community-dwelling older adults: a systematic review and meta-analysis. Cells. 2022;11(14):2199. doi:10.3390/cells11142199
- Wang H, Shi J, Shi S, et al. Bibliometric analysis on the progress of chronic heart failure. Curr Probl Cardiol. 2022;47(9):101213. doi:10.1016/j.cpcardiol.2022.101213
- Eslick GD, Talley NJ. Dysphagia: epidemiology, risk factors and impact on quality of life--a population-based study. Aliment Pharmacol Ther. 2008;27(10):971–979. doi:10.1111/j.1365-2036.2008.03664.x
- Kunieda K, Ohno T, Fujishima I, et al. Reliability and validity of a tool to measure the severity of dysphagia: the food intake LEVEL scale. J Pain Symptom Manage. 2013;46(2):201–206. doi:10.1016/j.jpainsymman.2012.07.020
- Zhao WT, Yang M, Wu HM, et al. Systematic review and meta-analysis of the association between sarcopenia and dysphagia. J Nutr Health Aging. 2018;22(8):1003–1009. doi:10.1007/s12603-018-1055-z
- Todaro F, Pizzorni N, Scarponi L, et al. The Test of Masticating and Swallowing Solids (TOMASS): reliability and validity in patients with dysphagia. Int J Lang Commun Disord. 2021;56(3):558–566. doi:10.1111/1460-6984.12613
- Engelheart S, Brummer R. Assessment of nutritional status in the elderly: a proposed function-driven model. Food Nutr Res. 2018;62:1366. doi:10.29219/fnr.v62.1366
- Nishida T, Yamabe K, Honda S. The influence of dysphagia on nutritional and frailty status among community-dwelling older adults. Nutrients. 2021;13(2):512. doi:10.3390/nu13020512
- Cuomo F, Angelicola M, De Arcangelis E, et al. Rheological and nutritional assessment of dysphagia-oriented new food preparations. Foods. 2021;10(3):663. doi:10.3390/foods10030663
- Zhang H, Zheng L, Tang M, et al. Developing strategies ”satia”: how to manage dysphagia in older people? A delphi panel consensus. Nurs Open. 2023;10(4):2376–2391. doi:10.1002/nop2.1493
- Snijders T, Verdijk LB, van Loon LJ. The impact of sarcopenia and exercise training on skeletal muscle satellite cells. Ageing Res Rev. 2009;8(4):328–338. doi:10.1016/j.arr.2009.05.003
- Reeg S, Grune T. Protein oxidation in aging: does it play a role in aging progression? Antioxid Redox Signal. 2015;23(3):239–255. doi:10.1089/ars.2014.6062
- Shaw SM, Martino R. The normal swallow: muscular and neurophysiological control. Otolaryngol Clin North Am. 2013;46(6):937–956. doi:10.1016/j.otc.2013.09.006
- Oh JC. Changes in the activation level of the floor of the mouth muscles during pressing and swallowing tasks according to the degree of tongue pressure. Dysphagia. 2024. doi:10.1007/s00455-024-10691-5