Abstract
Objective
This study aimed to develop the Chinese version of the totally implantable venous access port (TIVAP) self-management behavior scale for patients with cancer to provide a reliable tool for medical staff to judge patients with TIVAP self-management behavior.
Methods
This study employed a mixed-method exploratory design. The initial scale was developed through a literature review, expert meetings, and two-round Delphi expert consultation. The reliability indicators included retest reliability and Cronbach’s alpha coefficients. The validity indicators included content, construct, convergent, discriminant, and criterion validity. Exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) were employed for the validity analysis; 22 venous therapy experts participated in the Delphi expert consultation. A total of 500 patients were recruited from two third-class A hospitals in Guangdong Province, China, between July 2020 and January 2021 to test reliability and validity. A convenience sampling method was adopted.
Results
The final scale comprised seven dimensions and 29 items. The content validity index (S-CVI) was 0.990. Cronbach’s alpha coefficient and retest reliability of the scale were 0.931 and 0.900, respectively. The EFA results indicated a seven-factor structure, accounting for 65.68% of the total data variance. The results of the CFA showed that the CMIN/DF value was 2.348; the root mean square error of approximation value was 0.06; and the values of comparative fit index, incremental fit index, and Tucker–Lewis index were all >0.90. The factor loadings for all the items were >0.50, the composite reliability value was >0.70, and the average variance extracted (AVE) value was >0.50. Moreover, all absolute values of the correlation coefficients were less than the square root of the AVE for the seven dimensions. The total scores between the health promoting lifestyle profile-II revise (HPLP-IIR) and CPTSMBS were positively correlated (r = 0.465, p < 0.01).
Conclusion
The scale demonstrated good reliability and validity and can be applied in clinical practice to evaluate self-management behavior among patients using a TIVAP.
Background
A totally implantable venous access port (TIVAP) is a closed intravenous infusion system that is completely implanted under the skin. This use of TIVAP was first reported in 1982.Citation1 Compared with peripherally inserted central catheters (PICC) and nontunneled central venous catheters, TIVAP has fewer complications, higher levels of patient satisfaction, and ensures a higher quality of life for the patient.Citation2 However, several unavoidable TIVAP-related complications remain and include catheter rupture, infection, and thrombosis, which can increase the financial and health burdens on patients.Citation3
The TIVAP is completely implanted under the skin and has a minimal impact on the daily lives and work of the patients, which could cause a lack of observation of complications and the protection of the TIVAP. Multiple studies have shown port-related complications are closely associated with self-management behaviors, and poor compliance with TIVAP maintenance, lack of knowledge regarding TIVAP-related maintenance, and inadequate self-management behaviors, which can cause complications such as catheter occlusion and infection.Citation4–7 Therefore, a reliable assessment tool is needed for TIVAP self-management behaviors. Researchers have developed a self-management ability assessment scale for PICCs, which has been widely used in clinical practice. However, a comprehensive and reliable evaluation tool for the self-management behavior of TIVAP remains lacking. This study aimed to develop a self-management behavior assessment scale for TIVAP and to provide an effective assessment instrument for evaluating and monitoring self-management behaviors in patients with cancer who used TIVAP.
Methods
Study Design
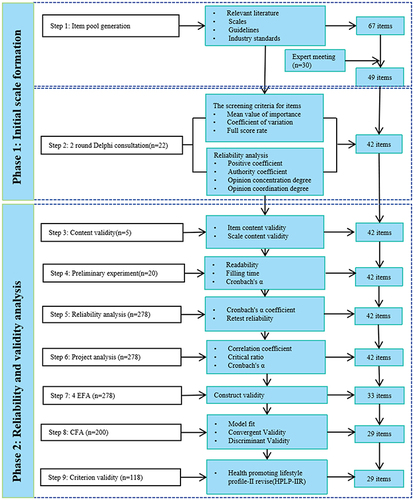
This study used a mixed-method exploratory design comprising two phases: initial scale generation and reliability and validity analyses of the initial scale. A flowchart of scale formation is shown in . We followed the eight-step scale development guidelines proposed by DeVellis and Thorpe to develop this scale and verified the reliability and validity through a questionnaire survey.Citation8 All participants signed an informed consent form. This study was reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Shantou University Medical College (Approval Number: 035). Our study complied with Declaration of Helsinki.
Phase 1: Initial Scale Formation
Conceptual Framework
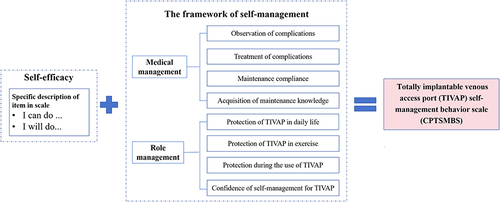
The development of the TIVAP self-management behavior assessment scale was based on self-efficacy,Citation9 which was reflected as “I can do it, or I will do it” in the specific description of the scale. Self-management refers to the ability to effectively manage symptoms, treatments, physical and psychosocial changes, and lifestyle adjustments.Citation10 The scale was designed using three self-management tasks proposed by Corbin et al.Citation11 These tasks included role, medical, and abnormal-emotion management. Although emotional management is one of the three major tasks of self-management, the scale developed in this study was mainly used for the self-management behavior of the TIVAP, emphasizing the management of the catheter rather than the management of the disease. Hence, no emotional management was present under the preset framework. The conceptual framework of this scale is illustrated in . The predesigned dimension represented medical management, including observation of complications, treatment of complications, maintenance compliance, and confidence in the self-management of TIVAP. The predesigned dimension represented role management, including the acquisition of maintenance knowledge, protection of TIVAP in daily life, protection of TIVAP during exercise, and protection during the period with the TIVAP needle.
Item Pool Generation
We reviewed the self-management-related scale, TIVAP-related guidelines, industry standards, and analyzed the causes of TIVAP complications. The Chinese and English databases searched included CNKI, VIP, Wan Fang, PubMed, Cochrane Library, Web of Science, EMBASE, CINAHL, and OVID. The 67 initial items were formulated from the retrieved literature. We then conducted an expert meeting with 30 specialist nurses in intravenous therapy at the First Affiliated Hospital of Shantou University Medical College to assess, revise, and delete redundant items. Finally, 49 preliminary items were selected for the Delphi experts.
Delphi Expert Consultation
The criteria for the inclusion of experts in this study were as follows: (1) specialist nurses in intravenous therapy from the provincial nursing association or Chinese Nursing Association; (2) professional title of supervisor or above; and (3) >5 years of experience in intravenous therapy. We recruited 26 experts based on their published recommendations.Citation12 The expert consultation questionnaire comprised four parts. (1) Introduction: Explain the background, purpose, method, and significance of the research and questionnaire filling requirements; (2) General information of Delphi experts, including age, educational background, professional title, and working years. (3) The assessment of scale indicators consisted of eight first-level indicators and 49 second-level indicators, and the Likert five-level method was used to assess the importance of the indicators (1 = very unimportant to 5 = very important). Each item establishes a modified opinion column, and experts can put forward suggestions for modifying, deleting, and adding items to enrich the scale. (4) Familiarity with expert indicators and the basis of judgment. Questionnaires were distributed to experts via email. The second round of the questionnaire, which was formed according to the importance score and revised opinions from the first round of expert consultation, was fed back to the experts until they gradually agreed.
Phase 2: Reliability and Validity Analysis
Sample Size
DeVellis and Thorpe recommended that, in exploratory factor analysis (EFA), the sample size should be at least five- to ten-fold the number of items to obtain reliable factors for tool development.Citation8 Hair et al suggested that a minimum sample size of 100–150 is required for confirmatory factor analysis (CFA).Citation13 The initial scale comprised 42 items after two rounds of expert consultation in Phase 1. Hence, the required theoretical sample size ranged from 310 to 570 patients. In addition, a 10% invalid questionnaire response rate was considered. The final sample size was 500.
Questionnaire Distribution
After two rounds of expert consultation in Phase 1, the initial scale consisted of seven dimensions and 42 items. The initial scale, which is commonly used to measure attitudes, was scored on a Likert scale ranging from 1 (never) to 5 (always).Citation14 All questionnaires were distributed by the researchers and immediately collected to ensure that real data could be obtained. Convenience sampling was also used. In total, 500 patients were recruited from two third-class A hospitals in Guangdong Province, China, between July 2020 and February 2021.
Inclusion and Exclusion Criteria
The inclusion criteria for this study were: (1) implantation of TIVAP for at least 1 month, (2) age range of 18–80, (3) ability to read and comprehend the questionnaire, (4) completion of the questionnaire independently or with the assistance of the researcher, and (5) willingness to sign informed consent. The exclusion criteria were as follows: (1) patients with serious illnesses or complications related to their disease, and (2) patients with cognitive, psychiatric, speech, or hearing impairments.
Preliminary Experiment
Before distributing questionnaires, we conducted a preliminary experiment with 20 patients in the First Affiliated Hospital of Shantou University Medical College to test whether the questions are easy to understand, measure the required time for completing the entire questionnaire, and calculate the Cronbach’s α coefficient of scale. The result of preliminary experiment showed that the questionnaire completion time was 7–9 min, and the Cronbach’s α coefficient was 9.458.
Criterion Validity
We used the health promoting lifestyle profile-II revise (HPLP-IIR) suitable for Chinese people to assess the criterion validity of the scale developed in this study.Citation15 The scale was revised by Cao et al based on the health-promoting lifestyle profile II (HPLP-II) developed by Walker et al.Citation16 The HPLP-IIR includes six dimensions and 40 items, including interpersonal relationships (5 items), nutrition (6 items), health responsibility (11 items), physical exercise (8 items), stress management (5 items), and spiritual growth (5 items). The Cronbach’s α coefficient of the scale measured in the preliminary experiment was 0.952 in this study. A total of 118 patients with TIVAP completed both the CPTSMBS and the HPLP-IIR.
Data Analysis
SPSS 23.0 and AMOS 23.0 were used for statistical analysis.
Delphi Expert Consultation
The screening criteria for items in Delphi are a mean value of importance assignment ≥3.5, coefficient of variation ≤0.25, and full score rate ≥20%. When items do not meet any of the above criteria, the research team discussed whether to retain or delete the item.Citation17 The indicators to evaluate the reliability of Delphi expert consultation included expert positive coefficient, expert authority coefficient (Cr), expert opinion concentration degree, and expert opinion coordination degree (Kendall coefficient W).Citation18,Citation19
Content Validity
Five experts were invited to evaluate the content validity. The relevance of the items was scored using a Likert four-level method (1 = very irrelevant to 4 = very relevant). The calculation method of content validity was as follows: I-CVI = Ne / N (Ne: the number of experts who selected “3” and “4”; N: the total number of experts); S-CVI = (sum of I-CVI scores) / (number of items). The I-CVI was 0.78 or above, indicating that the content validity of the item was good. The S-CVI was 0.90, indicating very good content validity of the scale.Citation20,Citation21
Reliability Analysis
(1) Internal consistency: Cronbach’s α coefficient was used to evaluate the internal consistency of the scale.Citation22 Cronbach’s α coefficient >0.7 was generally considered to indicate good internal consistency.Citation23 (2) External stability: Fourteen patients completed the scale again after a one-month interval to assess its retest reliability.Citation24 ICC ≥ 0.7 was considered good retest reliability.Citation25
Project Analysis
Before exploring the factor analysis, a project analysis was performed to filter the items. Items that met the following criteria were retained: (1) items with an item-total correlation coefficient of >0.4, and a correlation coefficient between items of less than 0.8;Citation8,Citation26 (2) items with a critical ratio > 4.00, with significant differences (P < 0.05); and (3) items did not lead to a decrease in the total Cronbach’s α coefficient.Citation27
EFA
The Kaiser–Meyer–Olkin (KMO) value >0.8, and Bartlett’s spherical test (p < 0.05) indicated that the items were suitable for EFA.Citation28 A cumulative variation rate >60% and a factor loading of each item >0.4 indicated good construct validity for the scale.Citation26 The deletion methods of the items and common factors in the EFA were as follows: (1) Items appeared under two common factors simultaneously, (2) items with only two or one common factors, (3) common factors without any items, and (4) items with factor loadings of <0.4.Citation29
Confirmatory Factor Analysis
(1) Model fit: The indicator goodness of fit which checks the fitting degree of scale theoretical framework formed by EFA, was tested by analyzing the chi-square (χ2)/degrees of freedom (df) (CMIN/DF), standardized residual mean root (SRMR), root mean square error of approximation (RMSEA), comparative fit index (CFI), incremental fit index (IFI) and Tucker–Lewis index (TLI).Citation30,Citation31 (2) Convergent Validity(CV): Convergent validity was used to distinguish the degree of item aggregation in each dimension. Factor loading values >0.5, average variance extraction (AVE) >0.5, and composite reliability (CR)>0.7 indicated good convergent validity.Citation32 (3) Discriminant Validity (DV): DV was used to check whether the factors measured the different concepts. An AVE > r2 indicates good DV of the scale.Citation33 If the fitting degree, convergent validity, and DV were unsatisfactory, the model could be modified by removing items with low factor loading values or by establishing covariance relationships between the residuals of the variables.Citation26
Criterion Validity
Pearson correlation coefficient method was used to analyze the correlation between the total scores of the two scales to assess criterion validity.
Results
Phase 1: Initial Scale Formation
Characteristics of Delphi Experts
Twenty-two experts from Guangdong, Shanghai, Tianjin, and Xinjiang provinces were invited to participate in expert consultation for this study. These experts were specialist intravenous therapy nurses with an average age of 46.18 ± 5.61 years and had 6–33 years of experience in intravenous therapy. The current occupations of these experts included nursing education (nine experts), nursing management (17 experts), clinical nursing (22 experts), and nursing scientific research (nine experts) ().
Table 1 The General Characteristics of Consult Expert (n=22)
The Results of Delphi Expert Consultation
The positive coefficient of experts in the two rounds was 84.62% (22/26) and 86.36% (19/22) respectively, exceeding 70%, which indicated the experts showed a high level of knowledge. The authority coefficient of the experts in the two rounds was 0.94 and 0.98 respectively, exceeding 0.7, which indicated the experts had a high level of authority and the results of their consultation were reliable.Citation19 The mean value of importance assignment in the second round was higher than the first round [(4.69 ± 0.28) vs (4.81 ± 0.20)], the coefficient of variation and the rate of expert opinion presentation in the second round was lower than the first round [Coefficient of variation: (0.13 ± 0.08) vs (0.09 0.08); Opinion: 68.18% (15/22) and 47.37% (9/19)], indicating that expert opinions were gradually consistent.Citation34 The Kendall coordination coefficient W in the two rounds was 0.26 and 0.50, respectively, showing an improvement in the coordination of expert opinions.Citation35,Citation36 After two rounds of consultation with a Delphi expert, an initial scale with seven preset dimensions and 42 items was developed (). The 42 items were shown in . The detailed information regarding the modification of the initial item pool has been presented in the previously published master’s thesis by Xiao-Hong Wu.Citation37
Table 2 The Results of Delphi Expert Consultation
Table 3 The Project Analysis of Initial Scale with 42 Items(n=278)
Phase 2: Reliability and Validity Analysis
The Characteristics of Patients
A total of 500 questionnaires were distributed to patients with cancer who used TIVAP. A total of 478 cases were available for analysis, with a questionnaire recovery rate of 95.60%. Among the 478 cases, 278 were randomly selected for EFA and 200 were used for CFA. The mean age of the study subjects was (48.38 ± 11.35) years. In 299 cases, the use of TIVAP exceeded 90 days ().
Table 4 Demographic Characteristics of the Participants (n=478)
Content Validity
Five experts were invited to evaluate the content validity. Only the I-CVI of item D1 was 0.8, and the I-CVI values of the other items were 1. The mean S-CVI/AVE scale score was 0.995. Five experts were both specialist nurses in intravenous therapy, and the characteristics of experts was shown in .
Table 5 The Characteristics of Five Experts
Reliability Analysis
The Cronbach’s α coefficient of the scale in this study was 0.931. Each dimension ranged from 0.733 to 0.877. The retest reliability of the scale was 0.900, and each dimension ranged from 0.515 to 0.911. Therefore, the scale has good reliability ().
Table 6 The Results of Reliability
Project Analysis
The items with item-total correlation coefficients ranged from 0.401 to 0.663, and the items with item-total correlation coefficients ranged from 0.005 to 0.770. The critical ratio was 9.864–10.108, with a significant difference (P < 0.05). The Cronbach’s α of the initial scale was 0.931. After deleting items individually, Cronbach’s α of the scale was 0.928–0.931. All items were retained after the project analysis in this study. The results of the project analyses are presented in .
Construct Validity by EFA
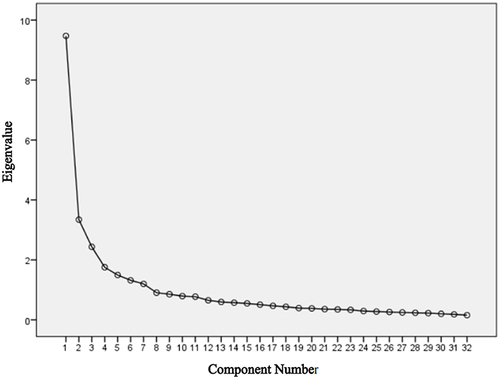
We conducted four EFAs with the 42 items to test construct validity. In the first three EFAs, we deleted nine items for the following reasons: six items that did not appear in any common factors (f2, f3, f4, e10, f8, and f9), one item that appeared in two common factors simultaneously (f1), and only two items that had the same common factor (c3 and c4). The results of four EFAs were shown in . In the fourth EFA, the KMO value was 0.881, and the Bartlett’s spherical test was statistically significant (X2 = 4732.439, P < 0.001), indicating that data were suitable for EFA. The results of the fourth EFA showed that seven common factors with eigenvalues >1 accounted for 65.68% of the total variance. The factor loading of remaining 33 items were >0.50 (). All items were successfully classified into the seven common factors, and each common factor had three or more items. The scree plot also supported the seven-factor structure (). Based on the results of the fourth EFA, the dimensions of the scale were renamed and redivided. After the fourth exploring factor analysis, the scale consisted of seven dimensions and 33 items, and the renamed dimensions and items are shown in .
Table 7 The Results of Four EFA
Table 8 The Results of Fourth EFA
Model Fit Degree in the CFA
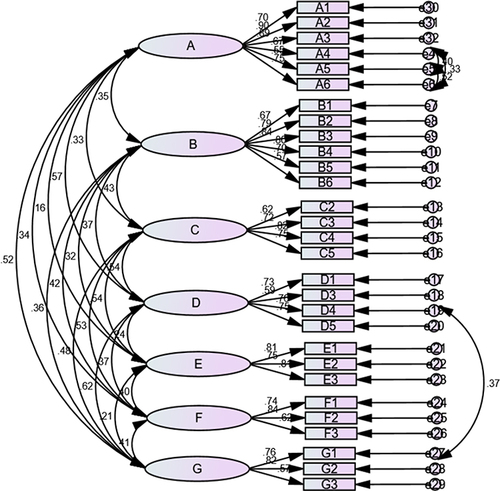
A total of 200 samples was used for the CFA, excluding those used in the EFA. The model fit was CMIN/DF = 2.909, RMSEA = 0.072, GFI = 0.809, CF I =0.854, and IFI = 0.855. The model fit was acceptable but could be improved. Hence, the model was modified by removing items B7, C1, D2, and F4 because of their low factor loadings after discussion by the research group and establishing covariance relationships between the variable residuals of items D4 and G1, A4 and A5, A5 and A6, and A4 and A6. The results of the CFA after model modification showed that the CMIN/DF value was 2.348, the RMSEA value was 0.06, and the CFI, IFI, and TLI values were all >0.90. The modified model fit was sufficient for acceptance ().
Table 9 The Fitness Results in CFA
Convergent Validity in the CFA
The AVE values of dimensions B (0.498), C (0.481), D (0.480), and F (0.491) were all <0.5, and the convergent validity was unideal (). After model modification, all factor loadings ranged from 0.552 to 0.896 and were >0.50 (), the AVE value ranged from 0.5231 to 0.6258, and the CR value ranged from 0.763 to 0.885, which met the criteria of AVE>0.50 and CR values >0.7. This scale had good convergent validity ().
Table 10 Convergent Validity
Discriminant Validity (DV) in the CFA
The absolute value of the correlation coefficients between the dimensions was smaller than the square root of the AVE for each dimension in both the premodification and postmodification models ().
Table 11 Discriminant Validity
Criterion Validity
The total scores between the HPLP-IIR and CPTSMBS were positively correlated (r = 0.465, <0.01), with a moderate-strength association, and the difference was statistically significant.
Discussion
The CPTSMBS comprising seven dimensions and 29 items was developed in this study to evaluate TIVAP self-management behaviors among patients with cancer. The scale is scored on a Likert five-level, with a total score ranging from 29 to 145. Higher scores indicate better self-management ability. The scale was divided into three levels: <87, low; 87–116, medium; and >116, good. The scale structure included two stages of TIVAP self-management in hospitals and at home, covering various aspects of the self-management of TIVAP by patients with cancer, such as complication observation, treatment, protection, and maintenance compliance. This scale can help medical staff identify patients with poor TIVAP self-management behavior and formulate targeted intervention measures to reduce TIVAP-related complications. The development of the scale followed the methodology proposed by Rattray and Jones to ensure scientific rigor.Citation38
The reliability of the scale was assessed by Cronbach’s α coefficient and retest reliability. Overall, the scale demonstrates excellent reliability. The Cronbach’s α coefficient of the scale and each dimension exceed 0.7, indicating a good internal consistency.Citation23,Citation39,Citation40 Additionally, the retest reliability of the scale was 0.900, which exceeded 0.7, suggesting good stability over time.Citation25 The retest reliability of each dimension ranges ranged from 0.515 to 0.911. However, the retest reliabilities of the dimensions of maintenance compliance, acquisition of maintenance knowledge, and confidence in self-management were <0.7. This indicates that these dimensions had poor stability, which may be attributed to the four-week interval between the retests.Citation25 The best time interval for retest reliability was 10–14 days.Citation41 Since our scale is issued on-site and the TIVAP maintenance interval in China is one month, most patients return to the hospital after a month. Hence, our retest interval was 1 month. Therefore, we suggest that the retest reliability of the scale used in this study was acceptable.
Woo suggested that in EFA, highly statistically correlated variables can be grouped together.Citation42 In the fourth EFA, the five items under the dimension b all described ”seeking medical help timely for different abnormal situations” and the items c1 and c2 both described “seeking medical help timely for maintenance.” A close relationship is present between items b1 to b5 and between c1 and c2. Hence, these items were classified under the same common factors as in the fourth EFA. The dimension E describes “The protection of TIVAP under different circumstances in the daily routine of exercise and life.” The items e4 to e8 all describes “protection of skin around TIVAP.” Hence, these items were classified into the same common factors. The fourth EFA identified seven common factors with eigenvalues >1, explaining 65.68% of the total variance, indicating that the scale had good construct validity.Citation26
The model fit was checked using CMIN/DF, GFI, CFI, and IFI, all of which had values within acceptable ranges (). We used a minimum sample size of 100–150 for CFA, following the criteria of Hair et al.Citation13 However, the small sample size might have affected model fit. Therefore, future studies using this scale should include a sufficient sample size to perform a CFA. For a model fit that may have problems because of a small sample size, the RMSEA, which is less affected by sample size, should be checked.Citation42 Therefore, we also calculated the RMSEA value, which was 0.072 (< 0.08) and within the excellent range.Citation43 Although a better model fit is desirable, building a research model based solely on a good model-fitting criterion is undesirable.Citation42 Therefore, based on the RMSEA values and the small sample size in the CFA, the fit of scale of the model was considered to be acceptable Moreover, the fit indicator in the revised model was better than before, and the GFI, CFI, and IFI of the model fit indicators had ideal values.
Convergent validity refers to the correlation of items within the same dimension, which is evaluated using composite reliability and average variance extraction (AVE).Citation32 Composite reliability reflects the consistency of items in the same dimension. A higher composite reliability value indicates a stronger association between the items and dimensions. A value >0.70 indicates better composite reliability.Citation44 In this study, the composite reliability values for all dimensions were >0.7, indicating a good combination reliability. The AVE represents the comprehensive interpretation ability of the items under the dimension. The greater the AVE value, the stronger the ability of the dimension to explain items, and the better the convergence validity. Generally, the AVE value was >0.5 indicating good convergent validity.Citation45 In this study, The AVE values of dimensions B, C, D, and F were all <0.5, indicating that convergence validity was not ideal. The factor load reflects the standardized regression coefficient from the dimension to item; the larger the factor load, the higher the AVE value. When the degree of fit, convergent validity, and DV were unsatisfactory, a common method is to delete items with low factor-loading values and establish covariance relationships between the residuals of mutually explainable variables.Citation26 Based on the clinical importance of the items, those with the smallest factor loads in dimensions B(B7), C(C1), D(D2), and F(F4) for model modification were deleted. Moreover, since items A4, A5 and A6 all describe “observed complications”, and items D4 and G1 all describe “acquisition of TIVAP information”, these variables can be interpreted by each other. Hence, we established covariance relationships between the variable residuals of A4 and A5, A5 and A6, A4 and A6, and D4, and G1 (). Chen et al adopted the same model modification method in their study.Citation46 All factor loadings of all items were >0.50 (), the CR value of all dimensions was >0.70, and the AVE value of all dimensions >0.50 after model modification, indicating good convergent validity.
Discriminant validity emphasizes the degree of differentiation among different dimensions.Citation33 The correlation coefficient between latent variables (ie, dimensions) was smaller than the square root of the AVE, suggesting that all dimensions had a certain degree of differentiation and that the scale had good discriminant validity.
The Chinese version of the Health Promotion Lifestyle Scale II Revision (HPLP-IR) is widely used clinically in China, with good reliability and validity.Citation15 A health-promoting lifestyle refers to the adoption of spontaneous, multilayered behaviors to maintain or have better health.Citation47 Self-management behavior refers to the initiative to perform preventive or therapeutic healthcare activities related to one’s own diseases under the guidance or assistance of medical personnel.Citation48 These two scales are closely related and exhibit synergistic effects. Due to the lack of an existing validated scale for the CPTSMBS, we used the HPLP-IIR to measure the criterion validity of this scale. This tool has also been used in other studies on health behaviors.Citation49 In this study, the total scores of both instruments were positively correlated (r = 0.465, P < 0.01), with a moderate-strength association.Citation50
Limitations
This study had some limitations. First, data collection took place during the COVID-19 pandemic when China was in a critical situation, which caused difficulties in the distribution of the questionnaire. Hence, we only included 500 patients with TIVAP from two hospitals in China, which may have led to regional bias and limited the promotion of the scale. Second, patients with cancer are physically weak. The scale is completed at an intravenous catheter clinic, and their schedule is very busy, which may have affected their answers to the questions. Finally, the scale was developed in China, and its items might have been influenced by Chinese culture. Hence, it is necessary to examine different cultural backgrounds in the future to improve the applicability of the scale.
Conclusions
The CPTSMBS developed in this study, comprising seven dimensions and 29 items, demonstrated good reliability and validity. The scale provides an effective evaluation tool for the prevention, monitoring, and intervention of TIVAP self-management in patients with cancer. Nevertheless, further validation and adjustments using multicenter and large-sample studies are necessary.
Disclosure
All authors declare that they have no conflicts of interest. Data acquisition was approved by the hospital ethics committee.
Acknowledgments
Xiao-Hong Wu and Yu Xiao are co-first authors for this study. We are grateful to the Affiliated Cancer Hospital of Sun Yat-sen University and the First Affiliated Hospital of Shantou University Medical School for providing the study site support. We are indebted to all consultation experts who contributed their time, knowledge, and energy to developing this scale.
Additional information
Funding
References
- Niederhuber JE, Ensminger W, Gyves JW, et al. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery. 1982;92(4):706–712. doi:10.1016/s0022-3468(83)80256-5
- Fang S, Yang J, Song L, et al. Comparison of three types of central venous catheters in patients with malignant tumor receiving chemotherapy. Patient Prefer Adher. 2017;11:1197–1204. doi:10.2147/PPA.S142556
- Shiono M, Takahashi S, Kakudo Y, et al. Upper arm central venous port implantation: a 6-year single institutional retrospective analysis and pictorial essay of procedures for insertion. PLoS One. 2014;9(3):e91335. doi:10.1371/journal.pone.0091335
- Zhang YH, Zhang J, Cao SS, et al. The survey analysis on outpatients’ nursing status of implanted venous port. Nurs Pract Res. 2014;11(12):96–98. Chinese. doi:10.3969/j.issn.1672-9676.2014.11.052
- Wu CJ. Evidence-Based Practice for Maintenance of Implantable Venous Access Port in Adult Patients [ Master’s thesis]. Nanjing Medical University; 2018. Chinese. Available from: http://med.wanfangdata.com.cn. Accessed June 26, 2024.
- Shen YH, Xu JM, Zhang XP, et al. Analysis of the intervention significance of the health education in totally implantable venous access ports. Chin J Clin Med. 2016;23(3):365–367. Chinese.
- Kong QH, Chen YJ, Shi SM, et al. Cause analysis and nursing care of 6 cases of inverted injection seat in infusion port counter plan. Chin Gen Pract Nurs. 2019;17(27):3402–3404. doi:10.12104/j.issn.1674-4748.2019.27.021
- DeVellis RF, Thorpe CT. Scale Development: Theory and Applications. Thousand Oaks (CA): Sage Publications; 2021.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi:10.1037/0033-295X.84.2.191
- Richard AA, Shea K. Delineation of self‐care and associated concepts. J Nurs Scholarship. 2011;43(3):255–264. doi:10.1111/j.1547-5069.2011.01404.x
- Corbin JM, Strauss A. Unending Work and Care: Managing Chronic Illness at Home. Jossey-bass; 1988.
- Shi C, Zhang Y, Li C, et al. Using the delphi method to identify risk factors contributing to adverse events in residential aged care facilities. Risk Manag Healthc Policy. 2020;13:523–537. doi:10.2147/RMHP.S243929
- Hair JF, Black WC, Babin BJ, et al. Multivariate Data Analysis. 6th ed. Upper Saddle River (NJ): Pearson Prentice Hall; 2006.
- Jang D, Cho SK. Is the mid-point of a Likert-type scale necessary? Comparison between the scales with or without the mid-point. Survey Res. 2017;18(4):1–24. doi:10.20997/SR.18.4.1
- Cao WJ, Guo Y, Ping WW, et al. Development and psychometric tests of a Chinese version of the HPLP-II scales. Chin J Dis Control Prev. 2016;20(3):286–289. doi:10.16462/j.cnki.zhjbkz.2016.03.018
- Walker SN, Sechrist KR, Pender NJ. Health Promotion Model-Instruments to Measure Health Promoting Lifestyle: Health-Promoting Lifestyle Profile [HPLP II] (Adult Version). Omaha (NE): University of Nebraska Medical Center; 1995.
- Shen L, Yang J, Jin X, et al. Based on Delphi method and Analytic Hierarchy process to construct the evaluation index system of nursing simulation teaching quality. Nurse Educ Today. 2019;79:67–73. doi:10.1016/j.nedt.2018.09.021
- Dai F, Wei K, Chen Y, et al. Construction of an index system for qualitative evaluation of undergraduate nursing students innovative ability: a delphi study. J Clin Nurs. 2019;28(23–24):4379–4388. doi:10.1111/jocn.15020
- Wu C, Wu P, Li P, et al. Construction of an index system of core competence assessment for infectious disease specialist nurse in China: a delphi study. Bmc Infect Dis. 2021;21(1):1–10. doi:10.1186/s12879-021-06402-2
- Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–467. doi:10.1002/nur.20199
- Mujlli G, Al-Ghosen A, Alrabah R, et al. Development and validation of simulation scenario quality instrument (SSQI). BMC Med Educ. 2023;23(1):972. doi:10.1186/s12909-023-04935-5
- Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. doi:10.5116/ijme.4dfb.8dfd
- Li ZH, Luo P. PASW/SPSS Statistics Chinese Edition Statistical Analysis Course. 3rd ed. Beijing: Publishing House of Electronics Industry; 2010. Chinese.
- Peng Q, Wu WY. Development and validation of oral chemotherapy self-management scale. BMC Cancer. 2020;20(1):890. doi:10.1186/s12885-020-07404-0
- Fayers PM, Machin D. Quality of Life: Assessment, Analysis and Interpretation. Wiley Press; 2007.
- Wu ML. Statistical Analysis Practices in Questionnaire Development. Chongqing: Chongqing University Press; 2010.
- Qiu HZ. Quantitative Research and Statistical Analysis: Analysis of Data Analysis Examples in SPSS Chinese Window Version. Chongqing: Chongqing University Press; 2009.
- Hutcheson GD, Sofroniou N. The Multivariate Social Scientist: Introductory Statistics Using Generalized Linear Models. Sage; 1999.
- Kaiser HF. Coefficient alpha for a principal component and the Kaiser-Guttman rule. Psychol Rep. 1991;68(3):855–858. doi:10.2466/pr0.1991.69.1.111
- Parker KM, Harrington A, Smith CM, et al. Creating a nurse-led culture to minimize horizontal violence in the acute care setting: a multi-interventional approach. J Nurses Prof Dev. 2016;32(2):56–63. doi:10.1097/NND.0000000000000224
- Sando D, Ratcliffe H, McDonald K, et al. The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. Bmc Pregnancy Childb. 2016;16:236. doi:10.1186/s12884-016-1019-4
- Quigley L, Wright CA, Dobson KS, et al. Measuring attentional control ability or beliefs? Evaluation of the factor structure and convergent validity of the attentional control scale. J Psychopathol Behav Assess. 2017;39(4):742–754. doi:10.1007/s10862-017-9617-7
- Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Market Sci. 2015;43(1):115–135. doi:10.1007/s11747-014-04
- Guo XH. Techniques and Statistical Analysis of Medical Field Investigation. Beijing: People’s Medical Publishing Press; 2009.
- Kilner T. Desirable attributes of the ambulance technician, paramedic, and clinical supervisor: findings from a Delphi study. Emerg Med J. 2004;21(3):374–378. doi:10.1136/emj.2003.008243
- Xiao SZ. Nursing Research. Beijing: People’s Medical Publishing Press; 2006.
- Wu XH. Study on Current Status and Analysis of Influencing Factors about Self-Management Behavior of TIVAP among Cancer Patients [ Master’s thesis]. Shantou University; 2021. Chinese. Available from: http://med.wanfangdata.com.cn. Accessed June 26, 2024.
- Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. 2007;16(2):234–243. doi:10.1111/j.1365-2702.2006.01573.x
- Taber K. The use of cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2017;48(6):1273–1296. doi:10.1007/s11165-016-9602-2
- Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11(Suppl 1):S80. doi:10.4103/sja.SJA_203_17
- Lynn M. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–386. doi:10.1097/00006199-198611000-00017
- Woo J. The Concept and Understanding of Structural Equation Model. Seoul: Hannarae Academy; 2012.
- Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Elecron J Bus Res Methods. 2008;6(6):53–60.
- Mirzaei N, Dehdari T, Taghdisi MH, et al. Development of an instrument based on the theory of planned behavior variables to measure factors influencing Iranian adults’ intention to quit waterpipe tobacco smoking. Psychol Res Behav Manag. 2019;12:901–912. doi:10.2147/PRBM.S196417
- Ou-Yang ZY, Feng Y, Xie DD, et al. Development, validation and psychometric evaluation of the Chinese version of the biopsychosocial impact scale in orofacial pain patients. Front Psychol. 2023;14:1101383. doi:10.3389/fpsyg.2023.1101383
- Chen J, Song Y, Ou L, et al. Development and psychometric evaluation of a self-management behaviours scale in rheumatoid arthritis patients (RA-SMBS). BMC Nurs. 2023;22(1):40. doi:10.1186/s12912-023-01173-4
- Chen MY. The effectiveness of health promotion counseling to family caregivers. Public Health Nurs. 1999;16(2):125–132. doi:10.1046/j.1525-1446.1999.00125.x
- Kenneth A, Thomas Holroyd L, Creer. Self-Management of Chronic Disease: Handbook of Clinical Interventions and Research. Orlando; 2010.
- Kim H, Oh M, Kwon H, et al. Development of the Korean health behavior for dementia prevention scale for older adults. J Korean Acad Fundam Nurs. 2022;29(3):363–374. doi:10.7739/jkafn.2022.29.3.363
- Zhi L, Qiaojun L, Yanbo Z. Development and validation of patient-reported outcomes scale for hypertension. Int J Qual Health Care. 2015;27(5):369–376. doi:10.1093/intqhc/mzv060