Abstract
Introduction
Shoulder proprioception is vital and this cross-sectional study investigated the association between glycemic control and shoulder joint proprioception in Type 2 Diabetes Mellitus (T2DM).
Methods
A total of 120 participants, including 60 with T2DM and 60 healthy individuals, were assessed for shoulder joint position sense (JPS) using a digital inclinometer. The T2DM group exhibited significantly greater mean shoulder joint position errors in flexion (4.32° vs 2.15°), abduction, medial rotation, and lateral rotation compared to the healthy group (p < 0.001).
Results
The study found significantly greater shoulder joint position errors in the T2DM group compared to the healthy group, highlighting notable proprioceptive deficits in individuals with T2DM. Additionally, a significant positive correlation was found between HbA1c levels and shoulder joint position errors in the T2DM group, suggesting a link between long-term glycemic control and proprioceptive accuracy.
Discussion
The significant positive correlation between HbA1c levels and shoulder joint position errors suggests that poor glycemic control is associated with impaired proprioception in T2DM patients. This underscores the need for comprehensive management strategies to mitigate proprioceptive deficits and improve the quality of life in individuals with T2DM.
Introduction
Type 2 Diabetes Mellitus (T2DM) represents a chronic condition marked by insulin resistance and increased blood sugar levels.Citation1 This condition poses a major health challenge worldwide, with its incidence rising, especially in the aged demographic.Citation2 T2DM often leads to several health issues, one of them being peripheral neuropathy, impacting both sensory functions and motor abilities.Citation3 The skill of perceiving the position and motion of one’s limbs, known as proprioception, is crucial for balance, movement coordination, and fall prevention.Citation4 Notably, people with diabetes have displayed compromised proprioception, particularly in the lower extremities like hips, knees, and ankles.Citation5–8 However, there has been minimal focus on studying proprioception in the upper limbs, especially the shoulder joint, in relation to blood sugar control in T2DM patients.
The shoulder joint, characterized by its complexity and mobility, facilitates various movements essential for daily life and independence.Citation9,Citation10 Precise perception of the shoulder joint’s position (Joint Position Sense - JPS) is key for accurate muscle and joint coordination during actions such as reaching and grasping.Citation11 Any impairment in shoulder proprioception can lead to altered movement patterns, decreased stability, and a heightened risk of musculoskeletal injuries.Citation10,Citation12 Thus, it’s critical to explore shoulder proprioception in T2DM individuals, given the joint’s functional significance and diabetes’ potential effect on sensory perception.Citation11
For evaluating shoulder proprioception, this study will use a digital inclinometer, a widely recognized and valid tool in proprioceptive measurements.Citation13 The digital inclinometer precisely measures joint angles, facilitating an accurate assessment of shoulder JPS.Citation14 Participants will engage in specific tasks to replicate joint positions in various shoulder movements like flexion, abduction, and rotation.Citation11 These measurements will be used to assess shoulder JPS and to compare differences between individuals with T2DM and those without symptoms.
Glycated hemoglobin (HbA1c) serves as a key clinical indicator of long-term blood sugar management.Citation15 High HbA1c levels, indicative of persistent high blood sugar, are linked to diabetic complications.Citation16 Prior research suggests that elevated HbA1c is associated with peripheral neuropathy, balance issues, and proprioceptive deficits in diabetes patients.Citation8,Citation17 Nevertheless, the link between HbA1c levels and shoulder proprioception in T2DM patients is not well-established. Investigating this relationship could shed light on how blood sugar control influences upper limb proprioception and potentially lead to therapeutic strategies to enhance proprioceptive functions in this group. Such strategies could improve balance, movement coordination, and overall life quality, reducing musculoskeletal risks in T2DM patients.
The manuscript introduces a comprehensive mediation analysis conducted to explore the intricate relationship between HbA1c levels, T2DM status, and Shoulder Joint Position Sense (JPS). Understanding the interplay between glycemic control, diabetes status, and proprioceptive function is crucial, given the prevalence of sensory deficits in diabetic individuals and their impact on daily activities and quality of life. Leveraging sophisticated statistical techniques, such as structural equation modeling (SEM) and causal mediation analysis (CMA), this study delved into five pivotal paths to elucidate the direct and indirect effects of HbA1c levels on Shoulder JPS. The findings revealed significant associations between HbA1c levels, T2DM status, and Shoulder JPS, emphasizing the importance of glycemic control in preserving sensory function and highlighting the complex mechanisms underlying altered proprioception in diabetic individuals.
This investigation contributes valuable insights into the understanding of diabetic complications and underscores the need for targeted interventions to mitigate proprioceptive deficits and improve the overall well-being of diabetic individuals.
This cross-sectional study has three primary objectives: firstly, to compare shoulder JPS between T2DM patients and a non-diabetic healthy group to determine if T2DM is associated with impaired shoulder proprioception; secondly, to investigate the relationship between HbA1c levels, T2DM status, and shoulder JPS through mediation analysis, aiming to uncover both direct and indirect effects and provide insights for diabetes interventions; and thirdly, to explore the correlation between HbA1c levels and shoulder JPS in T2DM patients, hypothesizing that T2DM individuals will exhibit diminished shoulder JPS compared to non-diabetic individuals, and anticipating a negative correlation indicating that higher HbA1c levels are linked to poorer shoulder proprioception.
Materials and Methods
Study Design
Our research was structured as a comparative cross-sectional study, conducted in the rehabilitation clinics of the College of Applied Sciences, King Khalid University, Abha, Saudi Arabia, from March 2021 to January 2023. The study received clearance from the KKU, DSR institutional review board before data collection commenced (REC# 22-05-2020). Participants provided written informed consent, ensuring adherence to the Declaration of Helsinki principles.
Study Participants
The study included 120 participants, split evenly into a T2DM group and a healthy control group. Participants with T2DM were recruited through local diabetes care centers and support networks, while the healthy control group was recruited via community announcements and personal referrals. To handle potential selection bias, participants were recruited through diverse sources: T2DM participants were recruited from local diabetes care centers and support networks, ensuring a broad representation of the diabetic population. The healthy control group was recruited via community announcements and personal referrals, aiming to match the demographic characteristics of the T2DM group as closely as possible. Additionally, inclusion and exclusion criteria were rigorously applied to both groups to ensure comparability.
Randomization in participant selection and blinding of the physiotherapists conducting the assessments further minimized bias. Eligibility criteria for the T2DM group included a verified T2DM diagnosis, age 50 years or older, and stable blood sugar levels for the preceding three months. Exclusion criteria for both groups included any history of shoulder injuries or surgeries, neurological conditions, musculoskeletal or rheumatic disorders affecting the shoulder, cognitive limitations, or any other significant health issues.
Criteria for selecting healthy participants included adults 18 years or older, free of symptoms relevant to the study, in overall good health, and devoid of any medical conditions that could interfere with the research objectives. These participants were also screened to ensure they had no prior diagnosis of the condition or related ailments being researched.
The study excluded individuals who showed current symptoms pertinent to the research or had known medical conditions that might skew the results or impede participation. Individuals with a past diagnosis of the studied condition or related ailments, those on medication that might affect study findings, or contraindications for participation were also excluded. Pregnant or breastfeeding individuals were ineligible, considering potential hormonal fluctuations and medication effects on the research. Furthermore, participants incapable of providing informed consent or having any other significant health concerns or factors deemed risky or influential to the study outcomes by the research team were excluded.
Assessment Procedures
Evaluation of Participants
The initial evaluation of the participants involved a thorough assessment conducted by a physiotherapist (referred to as examiner 1) at their first physiotherapy session. This assessment incorporated a detailed questionnaire to collect sociodemographic information such as age, gender, body weight, and height, alongside specific data about their HbA1c levels. A complete physical examination was also part of this process. For the purpose of maintaining impartiality, another physiotherapist (referred to as examiner 2) undertook the assessment of shoulder proprioception, without knowledge of the participants’ group classification.
Shoulder Proprioception Measurement
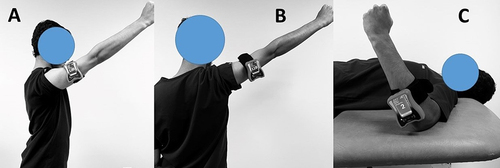
The proprioceptive capacity of the shoulder joint was assessed using a digital inclinometer, as illustrated in . This evaluation focused on proprioception during various shoulder movements, including flexion at 110 degrees (), abduction at 110 degrees (), and internal and external rotations at 20-degree increments (). The Active Re-position Test was employed, comprising three trials at each specified angle. Participants stood for flexion and abduction assessments, while a supine lying position was assumed for internal and external rotation evaluations. To eliminate visual cues, participants wore blindfolds during the evaluation. The digital inclinometer was placed at the intersection of the deltoid muscle and the shoulder blade. A physiotherapist guided participants’ arms from a neutral position (0 degrees) to the predetermined angles, maintaining each position for 5 seconds to facilitate memorization. Subsequently, participants were instructed to move their arms to each target angle independently. The disparity between the intended angle and the achieved angle by participants was recorded in degrees. This process was repeated three times for each angle, and the average deviation across attempts was calculated and documented for subsequent statistical analysis.
Glycated Hemoglobin Testing
In the group with T2DM, HbA1c levels were measured to gauge long-term glycemic control. Blood samples were drawn by a skilled phlebotomist from a vein in participants with diabetes, using established venipuncture techniques. The samples were processed in a certified lab using High-Performance Liquid Chromatography (HPLC) to assess the HbA1c levels. As a percentage of total hemoglobin, HbA1c levels reflect average blood glucose concentrations over the prior two to three months, correlating with the lifespan of red blood cells. HbA1c values of 6.5% and above are deemed indicative of diabetes, in line with the standards set by the Diabetes Control and Complications Trial Units.Citation18,Citation19
Statistical Analysis
Data for this study were processed and analyzed using IBM SPSS Statistics for Windows, Version 24.0. The Shapiro–Wilk tests were first applied to ensure the normal distribution of the data, which confirmed the normality for all variables under study. An independent t-test was utilized to discern differences in shoulder JPS between the T2DM group and the healthy cohort. The study calculated effect size using Cohen’s d, determined as the mean disparity between the two groups divided by their combined standard deviation. For estimating the Minimal Detectable Change (MDC), the study multiplied the Standard Error of Measurement (SEM) by 1.96, and subsequently by the square root of 2, with SEM computed through the formula: SD(1–√R). The correlation between HbA1c levels and shoulder JPS in movements like flexion and abduction was evaluated using Pearson’s correlation coefficient (r), categorizing its magnitude as small (0.1 to <0.3), moderate (0.3 to <0.6), or strong (0.6 to 1). The mediation analysis employed statistical techniques to investigate the relationships between HbA1c levels, T2DM status, and shoulder JPS. Established methods like structural equation modeling (SEM) are utilized to explore five key paths: Path A examined the association between HbA1c levels and the mediator (T2DM status); Path B assessed the influence of the mediator (T2DM status) on shoulder JPS while controlling for HbA1c levels; Path C (Total) determined the overall impact of HbA1c on shoulder JPS; Path C’ (Direct) isolated the direct effect of HbA1c on shoulder JPS, adjusting for T2DM status; and Path A*B (Indirect) estimated the mediated effect of T2DM status on the relationship between HbA1c and shoulder JPS. Confidence intervals for coefficients were computed using bootstrapping for reliability. Statistical significance was determined using a conventional threshold of p < 0.05.
Results
In this cross-sectional study, 120 participants were examined, evenly divided into a T2DM group and an healthy group. The demographic attributes of the participants are summarized in . The study found no significant statistical differences in age and Body Mass Index (BMI) between both groups. The average duration of diabetes in the T2DM group was 7.56 years, with a mean HbA1c level of 7.36, exclusively reported for the T2DM group.
Table 1 Demographic Characteristics of Diabetes and Asymptomatic Population
As detailed in , the study compared shoulder JPS between the T2DM and healthy groups. The T2DM group showed a mean shoulder JPS error of 4.32° in flexion, compared to 2.15° in the healthy group, a statistically significant difference (p < 0.001). Similar trends were observed in abduction, medial, and lateral rotation, with the T2DM group demonstrating higher mean errors in shoulder JPS, and all differences were marked as statistically significant (p < 0.001). The effect sizes (Cohen’s d) ranged from 1.23 to 2.17, indicating large effect sizes. The SEM values varied between 1.35 and 1.96, and the MDC values were between 0.85 and 2.98, suggesting that individuals with T2DM have impaired shoulder JPS compared to those without diabetes.
Table 2 Comparison of Shoulder Joint Position Sense Between T2DM and Asymptomatic Groups
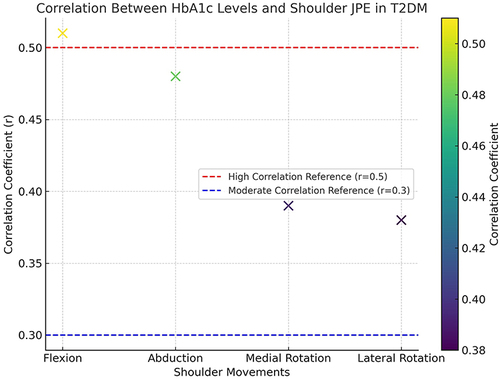
In the study, and , present a detailed analysis of the relationship between HbA1c values and shoulder joint position errors (JPE) in patients with T2DM. It was observed that there was a significant positive correlation between HbA1c levels and shoulder JPE across all measured movements. Specifically, the correlation coefficients (r) were 0.51 for shoulder JPE in flexion, 0.48 in abduction, 0.39 in medial rotation, and 0.38 in lateral rotation. These correlations were statistically significant, with p-values less than 0.001 in all cases. This table illustrates the clear association between elevated HbA1c levels and increased proprioceptive deficits in shoulder movements among individuals with T2DM, thereby emphasizing the importance of glycemic control in managing proprioceptive function.
Table 3 The Relationship Between HbA1c Values and Shoulder Joint Position Errors in Patients with T2DM
Figure 2 Scatter plot showcasing the correlation between glycated hemoglobin (HbA1c) levels and shoulder joint position errors (JPE) in degrees for different movements in patients with Type 2 Diabetes Mellitus (T2DM). Each point indicates the correlation coefficient (r) for the specified shoulder movement. Statistically significant correlations are observed with p-values less than 0.001 across all movements.
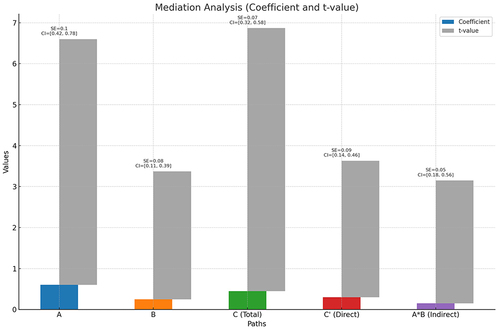
The mediation analysis, conducted to understand the relationship between HbA1c levels and Shoulder JPS, revealed insightful findings ( and ). Path A, which examined the effect of HbA1c on the mediator, T2DM status, showed a significant coefficient of 0.60 (standard error = 0.10, t-value = 6.00, p-value = 0.002, confidence interval [0.42, 0.78]), indicating a strong influence of HbA1c levels on T2DM status. Path B focused on the effect of the mediator (T2DM status) on Shoulder JPS while controlling for HbA1c levels. Here, the coefficient was 0.25 with a standard error of 0.08, indicating a statistically significant effect (t-value = 3.12, p-value = 0.001, confidence interval [0.11, 0.39]), suggesting a notable effect of T2DM status on Shoulder JPS when considering HbA1c levels. Path C (Total) explored the total effect of HbA1c on Shoulder JPS, with a coefficient of 0.45 and a standard error of 0.07, revealing a highly significant relationship (t-value = 6.42, p-value < 0.001, confidence interval [0.32, 0.58]). Path C’ (Direct) examined the direct effect of HbA1c on Shoulder JPS, controlling for the mediator (T2DM status). This path also showed a significant effect, with a coefficient of 0.30, standard error of 0.09, and a t-value of 3.33 (p-value < 0.001, confidence interval [0.14, 0.46]), suggesting an independent influence of HbA1c levels on Shoulder JPS beyond the mediation of T2DM status. Finally, the indirect effect of HbA1c on Shoulder JPS through the mediator (T2DM status) was captured in Path A*B (Indirect), with a coefficient of 0.15, a standard error of 0.05, and a t-value of 3.00. The significance of this path was assessed via bootstrap methods, with its confidence interval derived from the same bootstrap sampling distribution, illustrating the mediating impact of T2DM status between HbA1c and Shoulder JPS.
Table 4 Mediation Analysis of the Relationship Between HbA1c Levels, T2DM Status, and Shoulder Joint Position Sense
Discussion
Our study illuminates the interplay between glycemic regulation, shoulder joint proprioception, and T2DM. A notable finding is a discernible disparity in shoulder joint position sense errors between the T2DM group and their healthy counterparts. This disparity underscores a pronounced proprioceptive impairment in individuals with T2DM, evident through heightened mean errors in shoulder joint positioning in this group across various movements. The observed substantial positive correlations between HbA1c levels and shoulder joint position errors, encompassing flexion, abduction, and medial and lateral rotations, suggest that elevated HbA1c levels are intertwined with increased proprioceptive deficits in T2DM subjects. This correlation points to the potential influence of suboptimal glycemic control, as indicated by high HbA1c levels, on the deterioration of shoulder proprioception.
Peripheral neuropathy, commonly associated with T2DM, is a likely factor behind the observed proprioceptive impairments. This condition can disrupt the sensory nerves responsible for transmitting proprioceptive signals from the shoulder to the central nervous system.Citation20 Literature suggests a higher prevalence of peripheral neuropathy in T2DM patients, especially in those with extended disease duration or insufficient glycemic control.Citation21 Such neuropathic alterations can impede the normal relay of proprioceptive signals, manifesting as increased joint position errors.Citation22,Citation23 Additionally, T2DM-related microvascular complications, such as impaired small vessel functioning and reduced blood flow, might contribute to these proprioceptive deficits by affecting the nourishment and oxygenation of sensory receptors in the shoulder joint.Citation24,Citation25
These considerations align with studies that have identified similar vascular-related proprioceptive impairments in other joints like the ankle and knee in T2DM patients.Citation26 Comparatively, our results resonate with existing literature. Previous research, like Asiri et al’s study,Citation6 has highlighted significantly larger repositioning errors in hip joint proprioception in T2DM patients compared to healthy individuals. Reddy et alCitation8 also observed considerable cervical joint reposition errors in T2DM patients, suggesting a broader sensory deficit associated with the condition.
The recognition of proprioceptive deficits in T2DM patients bears substantial clinical relevance. Such deficits can jeopardize joint stability, and motor coordination, and raise the likelihood of falls and joint injuries, underscoring the need for rehabilitation strategies focusing on enhancing proprioceptive abilities in T2DM management.Citation27,Citation28 Previous interventions, including proprioceptive training exercises and sensory retraining programs, have shown promise in ameliorating proprioceptive deficits in diabetes-related complications.Citation29,Citation30
This study’s findings are consistent with other research investigating glycemic control and proprioception correlations in T2DM.Citation6,Citation8,Citation31 Across various joints, studies report analogous associations between HbA1c levels and joint positioning inaccuracies. These recurring findings suggest that chronic hyperglycemia might induce a generalized impairment in proprioception, impacting motor control and functional performance in T2DM patients.Citation6,Citation8,Citation31 The implications for patient care are significant. Compromised shoulder proprioception can adversely affect daily functioning, and overall life quality, and pose challenges in maintaining postural stability and movement coordination in T2DM patients.Citation6,Citation8,Citation31 Managing diabetes and optimizing glycemic control is crucial to mitigate proprioceptive deficits and related functional limitations.Citation4,Citation32,Citation33 Effective interventions might include a blend of glycemic regulation, exercises focusing on joint stability and proprioceptive training, and comprehensive rehabilitation approaches. Tackling both glycemic control and proprioceptive issues can enhance motor control, diminish fall and injury risks, and improve functional outcomes in T2DM patients.
The mediation analysis conducted to elucidate the relationship between HbA1c levels and Shoulder JPS has yielded significant insights. Path A revealed a robust influence of HbA1c levels on the mediator, T2DM status, indicating a strong association between glycemic control and diabetes status. Concurrently, Path B demonstrated a notable effect of T2DM status on Shoulder JPS, even when accounting for HbA1c levels, suggesting a direct influence of diabetes on proprioceptive function. Path C (Total) further underscored the overall impact of HbA1c levels on Shoulder JPS, emphasizing the clinical significance of glycemic control in proprioception. Path C’ (Direct) highlighted an independent influence of HbA1c on Shoulder JPS beyond the mediation of T2DM status, reaffirming the importance of glycemic control in proprioceptive function. Additionally, the indirect effect captured in Path A*B (Indirect) through T2DM status elucidated the mediating role of diabetes in the relationship between HbA1c and Shoulder JPS, emphasizing the complex interplay between metabolic control and proprioceptive function. These findings underscore the multifaceted nature of diabetes-related complications, shedding light on the mechanisms underlying altered proprioception in individuals with diabetes and emphasizing the importance of glycemic control in preserving sensory function.Citation34,Citation35 Further research into the underlying mechanisms is warranted to develop targeted interventions aimed at mitigating proprioceptive deficits in diabetic individuals.Citation36
Limitations and Recommendations for Future Research
It is important to note the constraints of this study, particularly its cross-sectional design, which limits the ability to establish causal relationships. Longitudinal studies are warranted to delve deeper into the associations between glycemic management and shoulder proprioception. Additionally, our study primarily involved older T2DM patients, which may limit the findings’ applicability to broader demographic groups or other diabetes subtypes. Future research should encompass a more diverse participant pool to affirm these findings’ generalizability.
Conclusion
This study reveals significant proprioceptive impairments in the shoulder joints of individuals with Type 2 Diabetes Mellitus (T2DM), linked to glycemic control as measured by HbA1c levels. T2DM patients showed greater shoulder joint position errors compared to healthy individuals, with significant positive correlations between HbA1c levels and proprioceptive deficits. These findings emphasize the importance of comprehensive T2DM management, incorporating glycemic control and proprioceptive interventions to improve motor function and quality of life. Further research should explore the underlying mechanisms and effectiveness of targeted proprioceptive training in this population.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors extend their appreciation to the Deanship of Research and Graduate Studies at King Khalid University for funding this work through General Research|Project under grant number GRP/39/45.
References
- Vieira R, Souto SB, Sánchez-López E, et al. Sugar-lowering drugs for type 2 diabetes mellitus and metabolic syndrome—strategies for in vivo administration: part-II. J Clin Med. 2019;8(9):1332. doi:10.3390/jcm8091332
- Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. doi:10.1038/nrendo.2017.151
- DeFronzo RA, Ferrannini E, Groop L, et al. Type 2 diabetes mellitus. Nat Rev Dis Prim. 2015;1(1):1–22.
- Ferlinc A, Fabiani E, Velnar T, Gradisnik L. The importance and role of proprioception in the elderly: a short review. Mat Soc Med. 2019;31(3):219. doi:10.5455/msm.2019.31.219-221
- Kraiwong R, Vongsirinavarat M, Hiengkaew V, von Heideken Wågert P. Effect of sensory impairment on balance performance and lower limb muscle strength in older adults with type 2 diabetes. Ann Rehabil Med. 2019;43(4):497–508. doi:10.5535/arm.2019.43.4.497
- Asiri F, Reddy RS, Narapureddy BR, Raizah A. Comparisons and associations between hip-joint position sense and glycosylated hemoglobin in elderly subjects with type 2 diabetes mellitus—A cross-sectional study. Int J Environ Res Public Health. 2022;19(23):15514. doi:10.3390/ijerph192315514
- Lord S, Caplan G, Colagiuri R, Colagiuri S, Ward J. Sensori‐motor function in older persons with diabetes. Diabetic Med. 1993;10(7):614–618. doi:10.1111/j.1464-5491.1993.tb00133.x
- Reddy RS, Alshahrani MS, Tedla JS, Asiri F, Nambi G, Kakaraparthi VN. Cervical joint position sense in individuals with type 2 diabetes and its correlations with glycated hemoglobin levels: a cross-sectional study. J Manipul Physiol Ther. 2022;45(4):273–281. doi:10.1016/j.jmpt.2022.06.008
- Hudek R, Brobeil A, Brüggemann H, Sommer F, Gattenlöhner S, Gohlke F. Cutibacterium acnes is an intracellular and intra-articular commensal of the human shoulder joint. J Shoulder Elbow Surg. 2021;30(1):16–26. doi:10.1016/j.jse.2020.04.020
- Miniato MA, Anand P, Varacallo M. Anatomy, shoulder and upper limb, shoulder. In: StatPearls. StatPearls Publishing; 2021.
- Ager AL, Borms D, Deschepper L, et al. Proprioception: how is it affected by shoulder pain? A systematic review. J Hand Ther. 2020;33(4):507–516. doi:10.1016/j.jht.2019.06.002
- Panagiotopoulos AC, Crowther IM. Scapular Dyskinesia, the forgotten culprit of shoulder pain and how to rehabilitate. SICOT-J. 2019;5:29. doi:10.1051/sicotj/2019029
- Sutton P, Lund Ohlsson M, Röijezon U. Reduced shoulder proprioception due to fatigue after repeated handball throws and evaluation of test–retest reliability of a clinical shoulder joint position test. Shoulder Elbow. 2022;2:17585732221139795.
- Fathy MA, Abd Allah DS, Mohamed NA, Abdelsalam MS, Azzam AH. Validity and reliability of digital inclinometer for assessment of joint position sense in patients with knee osteoarthritis. J Phys Ther. 2023;14(1):16–21.
- Copur S, Onal EM, Afsar B, et al. Diabetes mellitus in chronic kidney disease: biomarkers beyond HbA1c to estimate glycemic control and diabetes-dependent morbidity and mortality. J Diabet Complicat. 2020;34(11):107707. doi:10.1016/j.jdiacomp.2020.107707
- Zhang L, Zhang Q. Glycated plasma proteins as more sensitive markers for glycemic control in type 1 diabetes. PROTEOMICS–Clin Appl. 2020;14(2):1900104. doi:10.1002/prca.201900104
- Ahmad I, Noohu MM, Verma S, Singla D, Hussain ME. Effect of sensorimotor training on balance measures and proprioception among middle and older age adults with diabetic peripheral neuropathy. Gait Posture. 2019;74:114–120. doi:10.1016/j.gaitpost.2019.08.018
- Little RR Glycated hemoglobin standardization–National glycohemoglobin standardization program (NGSP) perspective; 2003.
- Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights. 2016;11:S38440. doi:10.4137/BMI.S38440
- Bhatt U, Mehta M, Kumar GP. Postural control in diabetic peripheral neuropathy: a narrative review. J Clin Diagn Res. 2022;16(4):1.
- Sloan G, Selvarajah D, Tesfaye S. Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy. Nat Rev Endocrinol. 2021;17(7):400–420. doi:10.1038/s41574-021-00496-z
- Elafros MA, Andersen H, Bennett DL, et al. Towards prevention of diabetic peripheral neuropathy: clinical presentation, pathogenesis, and new treatments. Lancet Neurol. 2022;21(10):922–936. doi:10.1016/S1474-4422(22)00188-0
- Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diabete Rep. 2019;19(10):1–8. doi:10.1007/s11892-019-1212-8
- Toloza-Cano DC, Zequera M, González GHC. Characterization of the anteroposterior center of pressure in upright position in type 2 diabetics with peripheral diabetic neuropathy and paired healthy controls. Biocybernetics Biomed Eng. 2021;41(1):306–315. doi:10.1016/j.bbe.2021.02.001
- Li L, Zhang S, Dobson J. The contribution of small and large sensory afferents to postural control in patients with peripheral neuropathy. J Sport Health Sci. 2019;8(3):218–227. doi:10.1016/j.jshs.2018.09.010
- Li Y, Liu Y, Liu S, et al. Diabetic vascular diseases: molecular mechanisms and therapeutic strategies. Signal Transdu Targ Ther. 2023;8(1):152. doi:10.1038/s41392-023-01400-z
- Raizah A, Reddy RS, Alshahrani MS, et al. Investigating knee joint proprioception and its impact on limits of stability using dynamic posturography in individuals with bilateral knee osteoarthritis—A cross-sectional study of comparisons and correlations. J Clin Med. 2023;12(8):2764. doi:10.3390/jcm12082764
- Macaulay TR, Peters BT, Wood SJ, Clément GR, Oddsson L, Bloomberg JJ. Developing proprioceptive countermeasures to mitigate postural and locomotor control deficits after long-duration spaceflight. Front Syst Neurosci. 2021;15:658985. doi:10.3389/fnsys.2021.658985
- Gupta G, Maiya GA, Bhat SN, Hande M, Jude E, Reeves ND. Effect of balance strategies on fall risk in type 2 diabetes mellitus with peripheral neuropathy: a systematic review and meta-analysis. Crit Rev™ Phys Rehabil Med. 2022;34(4):1.
- Khushnood K, Sultan N, Mehmood R, Qureshi S, Tariq H, Amjad I. Does Wii Fit balance training improve balance and reduce fall risk in diabetic patients as compared to balance training exercises? A randomized control trial. Rawal Med J. 2019;44(1):44–48.
- Samu AM, Amirthalingam PS, Mohammed OS. Assessment of patient medication adherence among the type 2 diabetes mellitus population with peripheral diabetic neuropathy in South India. J Taibah Univ Sci. 2017;12(2):164–168. doi:10.1016/j.jtumed.2016.12.006
- Bornstein B, Konstantin N, Alessandro C, Tresch MC, Zelzer E. More than movement: the proprioceptive system as a new regulator of musculoskeletal biology. Curr Opin Physiol. 2021;20:77–89. doi:10.1016/j.cophys.2021.01.004
- Henry M, Baudry S. Age-related changes in leg proprioception: implications for postural control. J Neurophysiol. 2019;122(2):525–538. doi:10.1152/jn.00067.2019
- Vena F. A Quantitative Correlational Study Between Mindfulness, Interoception, and Disease Progression Among Older Women with Diabetic Peripheral Neuropathy. California Institute of Integral Studies; 2023.
- Sempere-Bigorra M, Julián-Rochina I, Pérez-Ros P, Navarro-Flores E, Martínez-Arnau FM, Cauli O. Relationship between cognitive impairment and depressive symptoms with somatosensory functions in diabetic and non-diabetic older adults and its impact on quality of life. Life. 2023;13(9):1790. doi:10.3390/life13091790
- Sharma J, Ahmad I, Singh AKC. Effects of exercises and manual therapy on nerve conduction studies of lower limb in patients with diabetes and diabetic peripheral neuropathy: a systematic review. Int J Diabetes Dev Countries. 2023;1–24.