Abstract
Aim
Incontinence-associated dermatitis is a common health problem among older clinical patients, causing related severe skin damage such as pressure ulcers, secondary infection, and long length of hospital stay. This pilot study aimed to develop and examine the effects of nursing programs in preventing incontinence-associated dermatitis (IAD) among older patients. Ten older patients at high risk of incontinence-associated dermatitis were included in this study: five patients received a nursing program combined with mixed products, and another five received a nursing program combined with separate use of products. The program was evaluated using a perianal assessment tool (PAT-T) for risk assessment, the incontinence-associated dermatitis invention tool (IADIT-T) for severity assessment, the skin surface pH, and skin surface moisture. The results revealed that the nursing program and skin products are usable and acceptable, provide step-by-step details, and are simple and easy to follow. The nursing program combined with using zinc oxide products followed by petroleum jelly can prevent and decrease the severity of incontinence-associated dermatitis in older patients. Moreover, it can also improve the skin surface pH to a mild acidity appropriate for the skin condition and increase the skin’s moisture better the nursing program with mixed skin products. This pilot study confirmed that the developed program can be applied in practice. Moreover, the program could be used to decrease the incidence of IAD and skin surface pH but increase skin moisture. However, future study with a larger sample size and applying a more substantial research design for more accuracy and generalization is needed.
Clinical Trial Registration Number
OSF https://osf.io/8gj3d.
Introduction
Incontinence-associated dermatitis (IAD) is a serious skin condition resulting from moisture damage and chemical reactions, leading to skin irritation and damage.Citation1 This skin damage is typical among older patients who experience both urinary and fecal incontinence. Based on a statistical survey of older patients, the prevalence of urinary incontinence is approximately 16–28%, with rates in the community ranging from 15% to 30%. However, the prevalence can be as high as 60–70% among hospitalized older patients, which is twice in women compared to men.Citation2 A systematic review revealed that the prevalence of incontinence-associated dermatitis was 44% in patients residing in nursing homes and ranged from 33% to 73% among older patients admitted to hospitals.Citation2 The primary factor contributing to this condition is the inability to control bowel movements due to the deterioration of smooth muscles in the urinary and fecal sphincters among older patients. This factor leads to two main types of inability to control excretion in the acute and chronic phases.Citation3 A literature review also identified a higher prevalence of incontinence in semi-intensive/intensive care units (semi-ICU/ICU)Citation4 due to critical and severe illnesses and high-risk medical procedures. These serious factors render older patients incapable of self-care due to constraints such as intubation, anesthesia, and dialysis.Citation5 Finally, these factors contribute to serious skin complications, defining IAD.
Additionally, it has been revealed that older people undergo skin changes, including thinning of the epidermis and dermis.Citation6 There is a reduction in the number of blood vessels supplying the skin, accompanied by a loss of subcutaneous fat. The skin tends to become dry and rough due to a decrease in the number of sweat glands, along with reduced production of fat by the sebaceous glands and a decrease in the inflammatory response.Citation3 As a result, the skin of older people becomes more fragile, prone to easy tearing, and susceptible to damage and causing wounds. In addition, it has been found that ten risk factors for incontinence-associated dermatitis in older patients include excessive moisture, elevated skin pH (alkaline), presence of bacteria or fungus, friction, age, malnutrition, loose stools, obesity, lack of oxygen and blood flow, and the use of disposable diapers.Citation7 These factors place critically ill older patients receiving treatment in intensive or semi-intensive care units at a higher risk of developing IAD.
From the survey among older patients admitted to the hospital, it was discovered that up to 70% of them experience fecal incontinence.Citation8 This incapacity to control excretion stands as a significant factor contributing to dermatitis. Upon assessing the risk of IAD, up to 60% of older patients in the intensive care unit (ICU) were at a high risk. In comparison, IAD in the semi-intensive care unit (Semi-ICU) reached as high as 20.67%.Citation8 The development of IAD in older patients can lead to complications such as secondary infections and pressure injuries. A literature review found that individuals with IAD are ten times more likely to develop pressure ulcers than those with normal skin.Citation9 The conditions damage older patients’ skin, leading to physical and mental distress, higher risk of secondary infection, increased care costs, and longer hospital stays.Citation10 The researcher reviewed the literature on IAD prevention and care, identifying eight key activities: knowledge and skill training, risk assessment, incontinence management, cleaning, medical product application, body positioning, nutrition promotion, and outcome evaluation.Citation2 These activities were integrated into the five nursing processes: health assessment, nursing diagnosis, care planning, implementation, and evaluation.
A literature review categorized skin protection products into two groups: moisturizing and skin protection. Moisturizers, containing fats like lanolin and dimethicone, prevent water loss and promote skin hydration. Glycerin draws water to the skin’s surface. Skin protection products, containing petrolatum, zinc oxide, dimethicone, and acrylic polymer, prevent irritation from feces and urine. Phuengsiri found that a combination of petroleum jelly and zinc oxide effectively prevented IAD, though their different functions were noted.Citation11 Zinc oxide reduces inflammation, promotes healing, and protects against heat, wetness, and infection,Citation12 while petroleum jelly forms a protective layer but may affect the absorption of other moisturizing substances.Citation13 The effectiveness of separate or combined use of these products needs further exploration.
Working in a semi-ICU, we observed that older patients with diminished or altered consciousness, limited movement, and hesitancy to ask for help are at high risk of developing IAD. The staff is new to IAD care, and no guidelines exist. Traditional use of alkaline soap, a cause of IAD, is still practiced. Therefore, the researcher aimed to develop and study a nursing program using zinc oxide and petroleum jelly to prevent IAD in older patients in the semi-ICU. This pilot study explored the program’s feasibility and initial effectiveness.
Objective
This study aimed to develop a nursing program by applying separated and mixed zinc oxide and petroleum jelly to prevent IAD in older patients. We also aimed to study the feasibility of a nursing program and its effectiveness.
Conceptual Framework
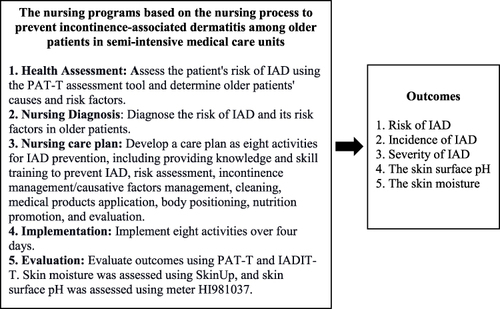
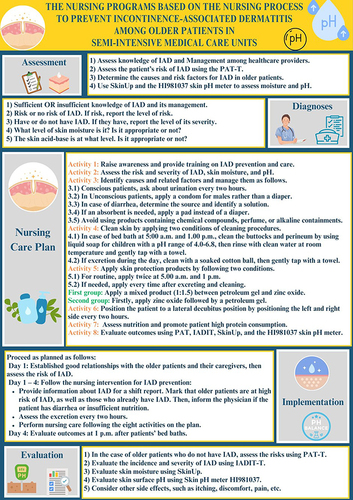
The researcher reviewed the related literature of Banharak et al,Citation2 a systematic literature review on the prevention and care of IAD in older patients. There were eight activities: providing knowledge and skill training to prevent IAD, risk assessment, incontinence management/causative factors management, cleaning, medical products application, body positioning, nutrition promotion, and evaluation activities. These activities were integrated into the 5-step nursing process, consisting of health assessment, nursing diagnosis, nursing care plan, implementation, and evaluation ().
Method
Design
A pilot study applied a quasi-experimental design and case study. This pilot study used a case study and nonparametric statistical analysis to explore feasibility and internal effectiveness. Quantitative and qualitative data were collected to provide comprehensive findings. Moreover, it can reflect the feasibility of applying the program and measure its results.
Setting
This study was conducted at the semi-intensive care units (Semi-ICUs) at the super tertiary hospital at the northeast region of Thailand. There were three Semi-ICUs which similar context of service taking part in the study.
Sample
The population and sample are new cases of older patients aged 60 years who were admitted to the medical semi-ICU in the super tertiary hospital. Ten patients were at high risk of IAD, and purposive sampling was used for this study. To prevent bias, the research assistants who did not work in the semi-ICU where the study was conducted and did not know what kind of nursing program the patient received measured the study outcomes. The research assistants earned master’s degrees in gerontological nursing practitioner and were prepared regarding the assessment of IAD risk, severity levels, and skin biomarkers before participating in this research. The times of outcomes evaluation were the first day of admission before attending the program and the fourth day after receiving the program.
Research Instruments
The search instruments were divided into two parts. Part one was a research instrument for conducting research (program intervention), and part two was a research instrument for outcome evaluation. Both parts were provided as follows.
Part 1: The nursing programs prevent IAD among older patients in the semi-ICU. After developing the program, the researcher sent it to the five experts, including a doctor specializing in dermatology, two nursing instructors who are experts in caring for older patients, a pharmacist specializing in skincare, and a nurse who is an expert in caring for patients with IAD. The program structures were presented in two ways to make the program clear and easy to follow.
The program is based on the nursing process: The program was structured around five nursing processes, starting with assessment and continuing through outcome evaluation. The content validity index (CVI) was 1.00, and the index of item objective congruence (IOC) of the program was 0.87 ().
The program is based on a daily schedule: The daily activities for nursing programs preventing IAD were prepared for four days following the day’s schedule. The CVI was 1.00, and the IOC was 0.95 ().
Table 1 The Nursing Programs Based on the Daily Activities Schedule to Prevent Incontinence-Associated Dermatitis Among Older Patients in Semi-Intensive Medical Care Units
Part 2: The research instruments for data collection. The researcher developed only general information records, illness records, and activity checklists based on the literature review; others were adopted from the instrument developer. The same expert group above evaluated the CVI for these research instruments. We found that the CVI for every tool was 1.00. The content of each tool was provided as follows:
The general information recording form included seven items: gender, age, weight, height, BMI, education, and occupation.
The illness record form included 19 items: the date of admission to the hospital, the date of admission to medical semi-ICU, the date of joining this study, diagnosis, chronic diseases, APACHE-II, antibiotics, laxative drugs, anesthesia drugs, levels of consciousness, albumin levels, malnutrition screening using nutrition screening tool – SPENT and Nutrition Alert Form (NAF), Barthel Activities of Daily Living (ADL), incontinence status, incontinence management, oxygen therapy, vasopressor drugs, equipment for direct and indirect restraining, muscle power and daily excretion record form.
The outcomes recording form to record the care results after receiving a nursing program to prevent IAD in older patients. This recording form included risk and severity levels, skin pH surface, and skin moisture. More details are as follows.
The perineal assessment tool Thai Version (PAT-T) was translated and examined for its validity and reliability by Simim.Citation8 The CVI was 0.90, and the IOC was 0.75. The percent agreement with the nurses’ opinions analyzed using a Pearson correlation coefficient was 0.94. Interrater reliability using a Pearson correlation coefficient was 0.99, and using the Kappa coefficient was 0.99. Moreover, intra-rater reliability using a Pearson correlation coefficient was 0.97, and using the kappa coefficient was 0.97. For this instrument, the four factors were assessed, including intensity of irritant (type and intensity of irritant), duration of irritant (amount of time that skin was exposed to irritant), perineal skin condition (skin integrity), and contributing factors (low albumin, antibiotics, tube feeding, clostridium difficile, other). The score ranged from 4 to 12 points. The levels of risk were divided into two: A score of 4–7 points means low risk, and 8–12 points means high risk of IAD.
Incontinence-Associated Dermatitis Intervention Tool Thai Version, IADIT-T, was translated and examined for validity and reliability by Simim.Citation8 The CVI was 1.00, and the IOC was 1.00. The percent agreement with the nurses’ opinions was analyzed using a Pearson correlation coefficient of 0.86. Interrater reliability using a Pearson correlation coefficient was 0.96, and using the kappa coefficient was 0.94. Moreover, intra-rater reliability using a Pearson correlation coefficient was 1.00, and using the kappa coefficient was 1.00. The evaluation of this instrument was five levels based on the definition and characteristics of the assessed skin: high risk of developing IAD, early IAD, moderate IAD, severe IAD, and fungal appearing rash.
The skin surface pH was measured using the Skin pH Meter Tool HI981037: The pH rank is between 0.00 and 12.00, the sensitivity is 0.01, and the accuracy value of pH ± 0.05.Citation14 The pH is divided into three levels: A pH lower than 7 indicates acidic skin pH, A pH of 7 is neutral, and a pH higher than 7 indicates base skin pH.
The skin moisture was measured using the SkinUp: The SkinUp measured moisture values lower than the Corneometer, but there was a good correlation between the SkinUp measure and the Corneometer (r < 0.804). Skin moisture estimates for the SkinUp and Craniometer forearm devices were similar to those measured when Corneometer instruments were compared, with a correlation between 0.759 and 0.981.Citation15 For interpreting results, 0–39% indicates dry skin, 40–60% indicates normal skin moisture, and 61–100% indicates too much moisture.
An activities checklist was used to ensure all activities/interventions were implemented for the older patients: Because the researcher wants to know the program’s effectiveness, it requires that the participants must receive at least 75% of activities/interventions indicated in the planned program, or at least 6 out of 8 activities, to be considered and included for data analysis.
Pilot Methods
The Center for Ethics in Human Research; Khon Kaen University committee approved this study before a pilot study. The approval date was December 19, 2023, and the approval number was HE661469. All methods or procedures related to this study complied with the Declaration of Helsinki. Before conducting this research, the protocol was developed and registered at the OSF https://osf.io/8gj3d. After getting approval, the researcher explained the objectives, procedures, and duration of data collection to the participants. They had the right to decide without any effects and could quit this study at any time. All information was kept confidential. The researcher presented the research results anonymously, and consent from patients for publication of the case details was introduced to the patients and their family members. Moreover, nurse feedback to be published anonymously was introduced. After explaining and giving all participants time to decide, all participants from this study signed the consent form before the researcher started collecting data. In cases where the patient is unconscious, a family member with decision-making authority signed consent forms instead of the patient before starting the data collection process.
Data Analysis
Both quantitative and qualitative data were collected for this pilot study. The quantitative data were analyzed using descriptive statistics such as percentages, means, standard deviations, medians, minimums, and maximums, along with inferential statistics such as the Chi-square test. However, the incidence of IAD, the severity of IAD, pH level, and skin moisture were analyzed using the Mann–Whitney U-test and Fisher’s exact test. Qualitative data were analyzed using a case report with various health conditions. Finally, the ten case studies with different characteristics and a discussion were provided.
Results
Possibility of Using the Program
The results revealed that a nursing program demonstrated a comprehensive set of activities that effectively prevent the occurrence of IAD. This program proved suitable for older patients admitted to the ICU/semi-ICU. The evaluation results from five experts indicated that the program provided comprehensive, accurate, and sufficient content of care for older patients with IAD that was easy to understand and follow. The program-based nursing process demonstrated a CVI of 1.00 and an IOC of 0.87. In the same way, the program-based daily schedule had a CVI of 1.00 and an IOC of 0.95, indicating a high level of alignment. Furthermore, the program adhered to the nursing process, a framework familiar to nurses. Including daily activity details, specified tasks, and their designated times made it easily executable and followable.
The program provides details on both the broader aspects of the nursing process and the more specific steps of a time-based, step-by-step practice, leading to easy understanding and follow-through RN0302202401.
Many nursing activities are routine tasks that have been performed before. The program introduces a few additional steps, such as selecting products for cleaning, blotting, and applying skin protection. Remembering what and when to do it is not difficult, as the program provides clear instructions and a schedule to guide us. Therefore, these activities are not complicated, making them easy to follow. RN0502202402.
General Information of the Sample
A sample of ten was divided into two groups: The nursing program with mixed products and a nursing program with separate product use. The first five older patients received a nursing program and skin protection products (zinc oxide mixed with petroleum gel). Most were males (4 cases) with an average age of 70.49±11.65 years and an average BMI of 21.55±2.81 kg/m2. Most older patients reported respiratory (2 cases) and gastrointestinal problems (2 cases). Four cases had a low disease severity level (APACHE II score of 0–19 points). In five cases, albumin protein levels were less than 3.8 g/dl, with an average albumin protein value of 2.36±0.36. The ability to perform daily activities was less than 12 points (dependency) for five cases, with an average ability to perform daily activities at 2.20±2.17. Five were at high risk of malnutrition. Most patients received oxygen, with two cases using an endotracheal tube and two using a high-flow nasal cannula. Additionally, three cases received Lactulose ().
Table 2 General Information Older Patients (n=10)
Another five patients received a nursing program by applying zinc oxide followed by petroleum gel. Primarily was female, with an average age of 71.41±10.09 years and an average BMI of 23.04±5.62 kg/m2. The majority of older patients presented with respiratory (2 cases) and cardiovascular problems (2 cases), with low disease severity levels (APACHE II score) in five cases. In five cases, albumin was less than 3.8 g/dl, with an average value of 15.60±3.13. The ability to perform daily activities was less than 12 points for five cases, indicating dependency and the average ability to carry out daily activities was 3.60±2.19. Five cases were at high risk of malnutrition. Three older patients received oxygen cannula, and two cases received Senokot ().
Quantitative Data Results
For improvement within the group, we found that for the participants who received the nursing process with mixed products, the improvement was found only for skin moisture (p = 0.4) (). However, the participants who received the nursing process with separate products used got improvements in skin surface pH (p = 0.043), skin moisture (p = 0.043), suitable skin surface pH (p = 0.049), and suitable skin moisture (p = 0.03) ().
Table 3 The Comparison of IAD Risks and Biomarkers Before and After Applying Nursing Programs in Preventing Incontinence-Associated Dermatitis (IAD) Among Older Patients (n=10) (Wilcoxon Signed Rank Test)
Table 4 The Comparison of the Number of IAD Cases and Suitable Biomarkers Before and After Applying Nursing Programs in Preventing Incontinence-Associated Dermatitis (IAD) Among Older Patients (n=10) (Fisher's Exact Test)
In the comparison between groups after attending the program, we found that the group that received a nursing program with separate products used had a lower risk score (p = 0.049), lower skin surface pH (p = 0.009), higher skin moisture (p = 0.009) (), suitable skin moisture (p = 0.049), and lower incidence of IAD (p = 0.004) than the group receiving nursing program with mixed products used ().
Table 5 The Comparison of IAD Risks and Biomarkers Before and After Applying Nursing Programs in Preventing Incontinence-Associated Dermatitis Among Older Patients Between the Two Groups (n=10) (Mann–Whitney U-Test)
Table 6 The Comparison of the Number of IAD Cases and Suitable Biomarkers Before and After Applying Nursing Programs in Preventing Incontinence-Associated Dermatitis Among Older Patients Between the Two Groups (n=10) (Fisher's Exact Test)
Qualitative Study Results
A Nursing Program Combined with the Use of a Zinc Oxide Skin Protection Product Mixed with Petroleum Jelly, Totaling 5 Cases
Case 1
The older male patient was 63 years old with good conscience, 53 kg, 160 cm, 19.53 kg/m2 of BMI, high risk of malnutrition (SPENT= 3), and 15 points of Nutrition Alert Form (NAF). He was admitted to the hospital due to drowsy for five hours with underlying disease of hepatic encephalopathy, cirrhosis child B, and hepatitis B virus (HBV) infection, treated by laxative Lactulose and the antibiotic ceftriaxone. The patient received a high-flow nasal cannula of 40 LPM and FiO2 0.4. The severity of the disease was assessed using the APACHE II score of 15 points. The older patient had urinary incontinence and was retained a urinary catheter and worn diaper. The pre-PAT-T score was 9, indicating a high risk of IAD with no pressure injury. The skin around the buttocks is clean. The skin surface pH was 6.32, indicating weakly acidic skin pH. The skin moisture was 10.00, indicating a dry skin. During the program, the older patient has feces 4–6 times a day and is liquid/watery. After completing the program, the older patient experienced IAD on the third day of admission. There was red skin and a burning sensation, and there was much burning when wiping the skin during cleaning. The skin surface pH was 7.95, indicating a neutral to the base. The skin moisture was 9.80, indicating the skin was drier than before the experiment.
Case 2
The older female patient was 65 years old with good consciousness, 63 kg, 160 cm, 24.61 kg/m2 of BMI, high risk of malnutrition (SPENT = 2), and 9 points of Nutrition Alert Form (NAF). The older patient was admitted to the hospital due to panting, tired, swollen legs for three hours. The underlying diseases were congestive heart failure and hepatitis B virus (HBV) cirrhosis, treated by expelling waste with the laxative lactulose and the antibiotic ceftriaxone. She received an oxygen nasal cannula 3 LPM. The severity of the disease was assessed using the APACHE II score of 13 points. The older patient had urinary incontinence and retained a urinary catheter and worn diaper. Before joining the program, the PAT-T was 10, indicating a high risk of IAD with no pressure injury. The skin around the buttocks was clean. The skin surface pH was 6.45, indicating a weakly acidic skin pH. The skin moisture was 10.10, indicating dry skin. During the program, the older patient had feces 2–4 times a day and was liquid/watery. After completing the program, the older patient had clean skin around the buttocks. However, the skin surface pH was 6.93, indicating a neutral value to the base. The skin moisture was 10.30, indicating the skin began to retain more moisture before the experiment.
Case 3
The older male patient was 75 years old with good consciousness, 50 kg, 165 cm, 18.37 kg/m2 of BMI, high risk of malnutrition (SPENT = 3), and 15 points of Nutrition Alert Form (NAF). The older patient was admitted to the hospital due to panting, tired for six hours; diagnosed with Acute Liver Failure, and underlying diseases were ischemic stroke, diabetes mellitus type 2, and hyperlipidemia, treated by laxative lactulose and the antibiotic Tazocin. The patient received a high-flow nasal cannula with 40 LPM and FiO2 0.4. The severity of the disease was assessed using the APACHE II score of nine points. The older patient had urinary incontinence and urinated with a urinary catheter and diaper. Before joining the program, the PAT-T was eight, indicating a high risk of IAD with no pressure injury. The skin around the buttocks was clean. The skin surface pH was 6.52, indicating weakly acidic skin pH. The skin moisture was 10.00, indicating dry skin. During the program, the older patient had liquid/watery feces 2–3 times a day. After completing the program, the skin around the buttocks was also clean. The skin surface pH was 6.94, indicating a neutral value to the base. The skin moisture was 10.70, indicating that the skin began to retain more moisture before the experiment.
Case 4
The older male patient was 65 years old with good conscience, 53 kg, 176 cm, 18.00 kg/m2 of BMI, high risk of malnutrition (SPENT = 3), and 16 points of Nutrition Alert Form (NAF). The older patient was admitted to the hospital due to fever, panting, and tiredness for three hours. He was diagnosed with pneumonia with septic shock and his underlying diseases were diabetes mellitus type 2 and hyperlipidemia, treated by the antibiotic Meropenem. The patient was on an endotracheal tube with a ventilator. The severity of the disease was assessed using the APACHE II score of 18 points. This patient had urinary incontinence and urinated using a urinary catheter and diaper. Before joining the program, PAT was nine, which results in a high risk of IAD with no pressure injury. The skin around the buttocks was clean. The skin surface pH was 6.85, indicating a weakly acidic skin pH. The skin moisture was 10.50, indicating dry skin. During the program, the older patient had liquid/watery feces 3–6 times a day. After completing the program, the skin around the buttocks was still clean. The skin surface pH was 6.90, indicating a neutral value to the base. The skin moisture was 10.20, indicating that skin moisture decreased after attending the program.
Case 5
The older male patient male was 91 years old with good conscience, 50 kg, 150 cm, 19.53 kg/m2 of BMI, high risk of malnutrition (SPENT = 3), and 15 points of Nutrition Alert Form (NAF). He was admitted to the hospital due to chest pain for an hour; he was diagnosed with non-ST elevation myocardial infarction (NSTEMI), and his underlying diseases were hypertension, diabetes mellitus type 2, and hyperlipidemia, treated by coronary artery angiography with the antibiotic Meropenem. The patient received oxygen via an endotracheal tube with a ventilator. The severity of the disease was assessed using the APACHE II score of 22 points. The older patient had urinary incontinence, which was urinated using a urinary catheter and diaper. Before joining the program, PAT was 8, resulting in a high risk of IAD but no pressure injury. The skin around the buttocks was clean. The skin surface pH was 6.78, indicating weakly acidic skin pH. The skin moisture was 10.20, indicating dry skin. During the program, the older patient has liquid/watery feces 2–4 times daily. After completing the program, the skin around the buttocks was clean. The skin surface pH was 6.89, indicating a neutral value to the base. The skin moisture was 11.20, indicating that the skin began to retain its moisture more before attending the program.
A Nursing Program Combined with the Use of Zinc Oxide Product Followed by Petroleum Jelly, Totaling 5 Cases
Case 6
The older male patient male was 65 years old with good consciousness, 85 kg, 165 cm, 31.22 kg/m2 of BMI, three scores of Nutrition Screening Tool (SPENT) indicating high risk of malnutrition, and Nutrition Alert Form (NAF) was 14 points. The older patient was admitted to the hospital due to panting and being tired for three hours and was diagnosed with congestive heart failure. His underlying diseases were hypertension, diabetes mellitus type 2, chronic kidney disease, and hyperlipidemia, treated by using diuretics drugs with the antibiotic Tazocin. The patient received a high-flow nasal cannula of 40 LPM and FiO2 of 0.4. The severity of the disease was assessed using the APACHE II score of 18 points. The older patient had urinary incontinence, which urinated using a urinary catheter and diaper. Before joining the program, PAT was eight, resulting in a high risk of IAD but no pressure injury. The skin around the buttocks was clean, with the skin surface pH at 6.98, indicating a neutral value to the base skin pH. The skin moisture was 10.10, indicating dry skin. During the program, the older patient has liquid/watery feces 2–4 times daily. After completing the program, the skin around the buttocks was clean, with the skin surface pH at 6.40, indicating a weakly acidic skin pH. The skin moisture was 12.90, indicating the skin began to retain moisture more than before attending the program.
Case 7
The older female patient was 62 years old with good consciousness, 48 kg, 150 cm, 21.33 kg/m2 of BMI, four scores of Nutrition Screening Tool (SPENT) indicating high risk of malnutrition, and Nutrition Alert Form (NAF) was 16. The older patient was admitted to the hospital due to a high fever and tiredness for a day. She was diagnosed with septic shock and his underlying diseases were hypertension and diabetes mellitus type 2, treated by diuretics drugs with the antibiotic Tazocin. The patient received an oxygen nasal cannula 5 LPM. The severity of the disease was assessed using the APACHE II score of 15 points. She had urinary incontinence, which was urinated by retraining a urinary catheter and wearing a diaper. Assessment of the PAT-T before joining the program was eight, indicating a high risk of IAD but no pressure injury. The skin around the buttocks was clean, with a skin surface pH of 7.20, indicating a neutral value to the base skin pH. The skin moisture was 10.00, indicating dry skin. During the program, the older patient had liquid/watery feces 3–5 times a day. After completing the program, the skin around the buttocks was still clean, with a skin surface pH of 6.38, indicating a weakly acidic skin pH. The skin moisture was 12.90, indicating the skin began to retain moisture more than before attending the program.
Case 8
The older male patient was 72 years old with good consciousness, 75 kg, 176 cm, 24.21 kg/m2 of BMI, SPENT Nutrition Screening Tool was three, indicating high risk of malnutrition, and Nutrition Alert Form (NAF) was 16. He was admitted to the hospital due to diarrhea for a day and was diagnosed with acute diarrhea and had no underlying disease. Then, he was treated using antibiotics, including Tazocin, Metronidazole, and Vancomycin. This patient received oxygen nasal cannula 3 LPM. The severity of the disease was assessed using the APACHE II score of 15 points. He had urinary incontinence and urinated using a urinary catheter and wore a diaper. The PAT before joining the program was nine, resulting in a high risk of IAD with no pressure injury. The skin around the buttocks was clean, with a skin surface pH of 6.87, indicating a weakly acidic skin pH. The skin moisture was 10.00, indicating dry skin. During the program, the older patient had liquid/watery feces 4–6 times a day. After completing the program, the skin around the buttocks was still clean, with a skin surface pH of 6.67, indicating a weakly acidic skin pH. The skin moisture was 11.50, indicating the skin began to retain moisture more than before attending the program.
Case 9
The older female patient was 70 years old with good consciousness, 52 kg, 151 cm, 22.81 kg/m2 of BMI, SPENT Nutrition Screening Tool was three, indicating high risk of malnutrition, and Nutrition Alert Form (NAF) was 16. She was admitted to the hospital due to a high fever and being tired for a day and was diagnosed with septic shock; her underlying diseases were hypertension, diabetes mellitus type 2, and lymphoma. She was treated with an antibiotic using Meropenem. This patient received oxygen via an endotracheal tube with a ventilator. The severity of the disease was assessed using an APACHE II score of 19 points. She had urinary incontinence and managed using a urinary catheter and diaper. The PAT before joining the program was nine, indicating a high risk of IAD with no pressure injury. The skin around the buttocks was clean, with a skin surface pH of 6.68, indicating a weakly acidic skin pH. The skin moisture was 10.50, indicating dry skin. During the program, the older patient had liquid/watery feces 4–6 times a day. After completing the program, the skin around the buttocks was clean, with the skin surface pH at 6.32, indicating a weakly acidic skin pH. The skin moisture was 11.90, indicating the skin began to retain moisture more than before attending the program.
Case 10
The older female patient was 88 years old with good conscience, 40 kg, 160 cm, 15.62 kg/m2 of BMI, SPENT Nutrition Screening Tool was three, indicating high risk of malnutrition, and Nutrition Alert Form (NAF) was 11 points. This patient was admitted to the hospital due to a high fever and tired for a day; diagnosed with pneumonia, no underlying disease, and was treated by expelling the antibiotic Tazocin. The patient received oxygen nasal cannula 3 LPM. The severity of the disease was assessed using an APACHE II score of 11 points. She had urinary incontinence and was managed using diapers. Before joining the program, PAT was nine, indicating a high risk of IAD with no pressure injury. The skin around the buttocks was clean, with a skin surface pH of 6.85, indicating a weakly acidic skin pH. The skin moisture was 10.00, indicating dry skin. During the program, she had liquid/watery feces 4–6 times a day. After completing the program, the skin around the buttocks was clean. The skin surface pH was 6.40, indicating a weakly acidic skin pH. The skin moisture was 12.10, indicating the skin began to retain moisture more than before attending the program.
Discussion
This study served as a pilot investigation to examine the possibility and effectiveness of a nursing program to prevent IAD in older patients in semi-ICU. The findings suggested that the nursing program for preventing IAD and using zinc oxide and petroleum jelly was feasible for research purposes and practice. This possibility was due to its step-by-step procedure following a daily schedule, aligning with the nursing process. The included activities are also familiar to nurses, making them easily implementable. This program’s approach aligns with the work of JinapornCitation16 in preventing IAD in medical wards. The activities involve skin cleaning with mildly acidic products, moisturizing, and skin protection. Checking excretion every two hours was consistent with the participatory action research conducted by Uppanisakorn et alCitation17 for preventing dermatitis in the medical intensive care unit. This study found that nurses could effectively perform the following activities: 1) Assessing the risk of IAD every eight hours or every shift, 2) Cleaning the skin using mildly acidic soap, employing tapping techniques instead of vigorously scrubbing the skin, 3) Utilizing products to enhance the moisture of the skin, and 4) Using skin care products to protect the skin. Following the program, there was a significant decrease in the incidence of IAD, consistent with the research conducted by Qiao & BanharakCitation9 in China. Their study reviewed the literature and reported case studies, emphasizing nursing activities to prevent IAD in the ICU. These activities include risk assessment, risk management, skin cleaning using appropriate products, and promoting knowledge and skills to medical personnel for preventing IAD.
Such measures contributed significantly to preventing the development of IAD in older adults. However, researchers have also developed a program preventing IAD specifically designed for older patients and ward contexts. This program differs from the research as mentioned above in the following aspects: 1) Risk Assessment: Assessing the risk of IAD; 2) Interdisciplinary Collaboration: Identifying causes and risk factors associated with the development of IAD by collaborating with interdisciplinary professionals such as doctors, nurses, and nutritionists; 3) Patient Positioning Techniques: Implementing patient positioning techniques to decrease contacted area, including lay down in left or right sides and checking excretion every two hours; 4) Nutritional Status Promotion: Undertaking activities to promote nutritional status; 5) Comprehensive Evaluation: Evaluating the effectiveness of implemented activities through various assessments, including statistical evaluations of outcomes such as the incidence and severity of IAD. Moreover, the evaluations included using biomarkers, such as skin moisture and pH evaluation tools. The researcher had carefully designed the nursing program to be detailed, easy to understand, concise, and aligned with daily nursing activities appropriate to the context of the ward. How we designed the program ensured clarity for operators and eased nurses’ job performance. Consequently, this program was feasible, could be easily implemented, and there was potential for studying its effectiveness in the future.
Providing knowledge and skill training to prevent IAD was crucial. Nurses and medical personnel needed the necessary knowledge to assess the risk of IAD in patients with incontinence. This activity included knowledge and skills training to prevent IAD. It was found that most personnel still need to prioritize the prevention and care of IAD. They confused between IAD and pressure ulcers, which have distinct causes. They also need to gain more knowledge regarding proper cleaning techniques tailored to the skin condition of older patients. The study by Qiao & BanharakCitation9 in China highlighted the significance of activities that provide knowledge to nurses, particularly in ICU/semi-ICU, where older patients may be unable to express their needs or care for themselves. Nurses in these wards play a crucial role in preventing the development of IAD and ensuring the correct implementation of skin care practices for older patients. Consistent with the research of Banharak et al,Citation2 as revealed in a systematic literature review, educating nurses and medical personnel on preventing IAD was a fundamental part of high-quality care for IAD. This education enhanced understanding of the deteriorating changes in the skin condition of older patients, raised awareness of the severity and effects impacting older patients and their relatives, and contributed to the overall quality of patient care. Using correct techniques, selecting appropriate cleaning products, and employing products with properties to protect and moisturize the skin could effectively reduce the incidence of IAD.
Risk assessment was a crucial nursing activity to assess the risk of IAD in older patients initially. Nurses and staff prioritize this activity, recognizing its significance in identifying the risk of IAD. The information gathered through this assessment was then utilized to plan appropriate nursing care for older patients experiencing incontinence. This result aligned with the study of Qiao & BanharakCitation9 in China, where a literature review emphasized that assessment was the initial step in providing nursing care and facilitating the planning of care tailored to each patient’s needs. The study by Uppanisakorn et alCitation17 about nurses’ perspectives on IAD care agreed that assessing the risk of IAD was crucial and should be started first. Nurses recommended that risk assessment should be conducted every eight hours or every shift. Assessing the risk of IAD served as a critical initial step to gather essential information for planning nursing activities geared towards preventing IAD. However, the tool for IAD assessment should be sensitive and practical. SimimCitation8 have adopted and translated standard tools into Thai. These tools included the Perineal Assessment Tool Thai Version (PAT-T) and the Incontinence-Associated Dermatitis Intervention Tool Thai Version (IADIT-T).
Managing the cause and related factors of IAD was a first recommendation priority. This management was to prevent the development of IAD. This activity was prioritized on initial prevention and non-invasive care for older patients. Nurses collaborate with consulting doctors to identify the causes of loose stools and related factors, marking the first recommended step in preventing IAD. Nurses and doctors work together to investigate potential causes, such as infections, the absence of fiber in tube feeding, rapid tube feeding, and exposure to certain drugs known to induce loose bowel movements, such as Elixir KCl and Phosphate mixture.Citation18 Additionally, there are still challenges in finding causes and factors that contribute to IAD in older patients. This approach aligns with the research of Qiao & BanharakCitation9 in China, which emphasizes the importance of medical personnel paying attention to finding the cause of diarrhea in older patients, which is a crucial cause of IAD. Finding causes also included other factors related to skin damage, such as protein deficiency and skin infections.
The literature review suggests that selecting suitable skin cleansing products for older patients significantly reduced the risk of IAD. Researchers recommended that using mild acidity minimized bacterial infections on the skin.Citation19 This recommendation aligned with the systematic review of Banharak et al.Citation2 The cleaning products should be mildly acidic and appropriate for the skin’s pH between 4.0 and 6.8. It was crucial to avoid cleaning products containing alcohol, chemical dyes, lotions, or perfumes. Furthermore, a cleaning technique involving tapping instead of scrubbing the skin was recommended. Finally, room-temperature water during the skin cleaning process was strongly recommended.
The application of medical products was reported for IAD prevention. Skin protection products should be able to block chemical contamination or create a barrier to shield the skin from contact with waste while also strengthening and revitalizing the skin and keeping it moisturized.Citation2 Our study was particularly interested in the effectiveness of zinc skin protection products, precisely a mixture of zinc oxide and petroleum gel. This approach compared the use of mixed and separated products. The recommended application of the product was in the morning and evening after showering; however, in cases where the patient urinated or feces, it was advised to reapply the skin protection products after cleaning. Case studies indicated that professional nurses could effectively follow these guidelines. This approach aligned with the principles identified in the research of Qiao & BanharakCitation9 in China, emphasizing the use of products to protect the skin from contact with waste, such as feces and urine, while simultaneously adding moisture and aiding in skin rehabilitation, such as petroleum jelly and zinc oxide. A study by PuengsiriCitation11 further supported the effectiveness of skin protection with a mixture of petroleum jelly and powder containing zinc oxide. This mixture protected the skin and was easy to wash and clean, allowing for a clear assessment of the skin’s condition.
Body positioning was an essential activity that promoted skin breathing in older patients. This positioning reduced skin humidity and minimized contact between the skin and urine or feces. Additionally, it monitored the excretion of older patients, mainly when patients could not express their needs, thus reducing the risk of skin inflammation due to incontinence.Citation2 The researcher specifies that patients should be repositioned every two hours, taking into account the context of the ward. This frequency aligned with the program’s implementation and was consistent with activities aimed at preventing pressure ulcers.Citation7 Importantly, this approach was crafted to be efficient, not increasing the nurse’s workload and allowing for the seamless integration of both activities simultaneously. This dual focus ensures effective skin care and supports overall patient well-being.
Nutrition promotion was a crucial nursing activity to enhance protein, carbohydrates, fiber, and nutrient intake for older patients. This activity was designed to ensure the skin receives adequate nutrients, promoting overall health. Nurses collaborated with the doctor to provide tailored nursing activities, including selecting the appropriate type of food for each specific older patient. A systematic review conducted by Banharak et alCitation2 supported the importance of promoting nutritional status. The research highlights that emphasizing protein and nutrients from all five food groups was beneficial in building firm skin and preventing IAD.Citation2
The evaluation was the final step of the program. This process involved the evaluation of the results of the nursing program in preventing IAD in older patients. Statistical methods were employed, and the IADIT-T assessment tool was utilized to present the incidence and severity of IAD. In addition to the IADIT-T assessment, other accurate medical tools were used to assess skin conditions, including SkinUp, measuring skin moisture assessment tool. This tool provides information about the skin’s moisture and strength, aiding in identifying conditions such as excessive dryness or edema in the epidermis (stratum corneum). Excessive dryness may indicate a lack of a protective barrier, leading to water evaporation, while edema may suggest a lack of skin protection, allowing external waste to penetrate the skin.Citation6 The HI981037 skin pH meter was also an easy-to-use tool, offering convenience and mobility. This tool assessed the skin’s pH level, which, in a healthy state, is typically acidic in the pH range of 4.1–5.8 in the stratum corneum. Changes in pH level may indicate that the skin lacks a protective barrier, allowing external waste to penetrate and resulting in an elevated pH level.Citation19
On the third day of implementing the nursing program along with products to protect the skin (zinc oxide mixed with petroleum jelly), one case had IAD with a mild severity level. This finding aligned with the results of the skin pH assessment, revealing an increased alkalinity value indicative of imbalanced skin caused by elevated alkalinity from enzymes and bile salts released along with feces from loose stools.Citation20 Furthermore, the study indicated decreased skin moisture, leading to moisture evaporation outside the skin.Citation20 This study also found that zinc oxide promoted wound healing when absorbed into the skin protected the skin from heat and wetness, and resisted germs to some extent. Conversely, petroleum jelly acted as a barrier, preserving skin function, retaining moisture, preventing evaporation, and contributing to tissue restoration. However, it hindered the absorption of other products into the skin,Citation13 potentially reducing the effectiveness of the nursing program and skin care products. Interestingly, these findings contrast with the study of Puengsiri,Citation11 which compared zinc oxide, petroleum jelly, and a mixture of petroleum jelly and zinc oxide. The study suggested that the product with petroleum jelly and powder containing zinc oxide could significantly prevent IAD. This difference might be due to this pilot study consisting of smaller samples and a need for more control over confounding variables, such as basic information and illness. Thus, future studies are needed to confirm these results.
Conclusion and Recommendations
A study on implementing a nursing program with eight activities, including zinc oxide and petroleum jelly application, found the program feasible. The group receiving zinc oxide followed by petroleum jelly significantly reduced IAD incidence and severity, adjusted skin pH to a mildly acidic level, and enhanced skin moisture more effectively than other groups.
Future studies should use rigorous and concise research methods, such as experimental studies applying randomized techniques, increasing the sample size to increase the power of testing, generalization, and more reliable research results, and longer study duration to confirm the actual and long-term measurement outcomes. Other products, such as natural or herbal products, should be used to prevent and care for IAD in older adults.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest for this work.
Acknowledgments
We want to thank those who contributed to this study. A special thanks is extended to the critical older patients and their caregivers who participated in the study. We also want to acknowledge the hospital staff at semi-intensive care units for their cooperation and participation during the research process. Lastly, special appreciation is extended to a native speaker and nursing professor for grammar proving and reviewing early drafts.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to prohibited laws (and/or rules, regulations, and contracts). However, they are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Beeckman D, Verhaeghe S, Defloor T, Schoonhoven L, Vanderwee K. A 3-in-1 perineal care washcloth impregnated with dimethicone 3% versus water and pH neutral soap to prevent and treat incontinence-associated dermatitis: a randomized, controlled clinical trial. J Wound Ostomy Con Tinence Nurs. 2011;38(6):627–634. doi:10.1097/WON.0b013e31822efe52
- Banharak S, Panpanit L, Subindee S, et al. Prevention and care for incontinence-associated dermatitis among older adults: a systematic review. J Multidiscipl Healthc. 2021;14:2983–3004. doi:10.2147/JMDH.S329672
- Limpawattana P. Geriatric Syndromes and Interesting Health Issues. 1st ed. Geriatric Medicine Unit Department of Internal Medicine Faculty of Medicine Khon Kaen University; 2018.
- Alderden J, Rondinelli J, Pepper G, Cummins M, Whitney J. Risk factors for pressure injuries among critical care patients: a systematic review. Int J Nurs Stud. 2017;71:97–114. doi:10.1016/j.ijnurstu.2017.03.012
- Muangpaisan W. Challenges and Solutions for Healthy Aging. Chulalongkorn University Publishing House; 2018.
- Khalid KA, Nawi AFM, Zulkifli N, Barkat MA, Hadi H. Aging and wound healing of the skin: a review of clinical and pathophysiological hallmarks. Life. 2022;12(12):2142. doi:10.3390/life12122142
- Doughty D, Junkin J, Kurz P. Incontinence-associated dermatitis: consensus statements, evidence-based guidelines for prevention and treatment, and current challenges. J Wound Ostomy Cont Nurs. 2012;39(3):303–315. doi:10.1097/WON.0b013e3182549118
- Supin Simim. Translation, Psychometric Test and Implementation of Perineal Assessment Tool (PAT) and Incontinence - Associated Dermatitis Intervention Tool (IADIT) Among Patients in Semi Intensive Medical Care Units. [ Master of Nursing Science Thesis in Gerontological Nursing]. Graduate School, Khon Kaen University; 2023.
- Qiao G, Banharak S. Incontinence-Associated dermatitis in older intensive care patients: a review and case report. J Multidiscipl Healthc. 2023;16:3299–3308. doi:10.2147/JMDH.S434275
- Van Damme N, Clays E, Verhaeghe S, Van Hecke A, Beeckman D. Independent risk factors for the development of incontinence-associated dermatitis (category 2) in critically ill patients with fecal incontinence: a cross- sectional observational study in 48 ICU units. Int J Nurs Stud. 2018;81(November 2017):30–39. doi:10.1016/j.ijnurstu.2018.01.014
- Phungsiri P. The effect of utilizing work instruction for incontinence associated dermatitis in high-risk patient. J Pub Med. 2016;30:59–67.
- Czarnowicki T, Malajian D, Khattri S, et al. Petrolatum: barrier repair and antimicrobial responses underlying this ”inert” moisturizer. J Allergy Clin Immunol. 2016;137(4):1091–1102.e7. doi:10.1016/j.jaci.2015.08.013
- Alonso C, Larburu I, Bon E, et al. Efficacy of petrolatum jelly for the prevention of diaper rash: a randomized clinical trial. J Spec Pediatr Nurs. 2013;18(2):123–132. doi:10.1111/jspn.12022
- Kon Y, Ichikawa-Shigeta Y, Iuchi T, et al. Effects of a skin barrier cream on management of incontinence-associated dermatitis in older women: a cluster randomized controlled trial. J Wound Ostomy Cont Nurs. 2017;44(5):481–486. doi:10.1097/WON.0000000000000353
- Westermann TVA, Viana VR, Berto Junior C, Detoni da Silva CB, Carvalho ELS, Pupe CG. Measurement of skin hydration with a portable device (SkinUp® Beauty Device) and comparison with the Corneometer®. Skin Res Technol. 2020;26(4):571–576. PMID: 31957168. doi:10.1111/srt.12833
- Jinaporn J, Temtap S, Nilmanat K. Comparison of petroleum-based skin-protection product and zinc oxide-based skin-protection product on incidence and the level of severity of early incontinence associated dermatitis in hepatic encephalopathy patients with incontinence. J Pub Health Nurs. 2018;32(2):59–78.
- Upanisorn S, Sommai T, Watthanasarn P, Boonrat J. Prevention and care of wounds caused by incontinence associated dermatitis in critically ill patients receiving treatment in ICU-Internal Medicine Ward. Thai J Nurs Counc. 2015;30(2):86.
- Phelps SJ, Hagemann TM, Lee KR, Thompson AJ. Pediatric Injectable Drugs: The Teddy Bear Book. 11th ed. American Society of Health-System Pharmacists; 2018.
- Proksch E. pH in Nature, Humans and Skin. J Dermatol. 2018;45:1044–1052. doi:10.1111/1346-8138.14489
- Avishai E, Yeghiazaryan K, Golubnitschaja O. Impaired wound healing: facts and hypotheses for multi-professional considerations in predictive, preventive and personalised medicine. EPMA J. 2017;8(1):23–33. doi:10.1007/s13167-017-0081-y