Abstract
Objective
The aim of this study was to investigate factors related to insomnia in a cohort of people with asthma.
Design
This secondary analysis utilized cross-sectional data from the Norwegian Nord-Trøndelag Health Study, a population-based health survey (n=50,807).
Participants
We used self-reported data from 1,342 men and women with a physician-confirmed asthma diagnosis ranging in age from 19.5 to 91 years.
Measurements
Data on sleep, lifestyle variables (smoking and exercise), anxiety, and depression were included. An insomnia scale and asthma impact scale were constructed using factor analysis. Hierarchical series of multiple regression models were used to investigate direct and mediational relationships between the study variables and insomnia.
Results
The hierarchical models revealed significant independent contributions of female sex, higher age, not exercising, asthma impact, anxiety, and depression on insomnia (R2=25.2%). Further, these models suggested that the impact of smoking on insomnia was mediated by anxiety, and that the beneficial impact of exercise was mitigated by depression symptoms.
Conclusion
Smokers with asthma have more insomnia, and this relationship may be mediated by anxiety. Further, people with asthma who experience depression symptoms are less likely to benefit from physical exercise as a method to enhance sleep quality. Our findings would suggest that helping smokers to manage their anxiety and depression through behavioral methods may reduce their insomnia symptoms, and enable them to engage in other health-enhancing pursuits, such as physical exercise.
Introduction
Sleep problems are widespread both in general population and in clinical practice. Insomnia is the most common sleep disorder, and is characterized by subjective complaints about dissatisfaction with sleep quality or duration, as well as difficulty with initiating sleep, maintaining sleep at bedtime, waking up in the middle of the night or too early in the morning, or nonrestorative, poor quality of sleep.Citation1 Population studies show that up to 48% of adults report “some insomnia problems over the past year”, and 6%–15% report chronic insomnia.Citation2
Sleep patterns change throughout life. Sleep problems are common in adolescents,Citation3 possibly because of the puberty-related circadian shift toward being a “night owl”.Citation4 Menopausal transition status is also related to severe self-reported sleep difficulty,Citation5,Citation6 which may be due to hormonal changes.Citation7 Later in life, people note that they have more difficulty staying asleep at night and, perhaps consequently, more difficulty staying awake during the day.Citation8 The cause of sleep problems in older people is more complex than hormones, and can be related to circadian rhythm changes, medication, medical and psychiatric illness, and other primary sleep disorders.Citation9 Thus, the biological reasons underlying sleep difficulties may change over the life trajectory.
Although primarily defined as a sleep disorder, consequences of insomnia extend beyond the sleep period. Daytime symptoms, such as tiredness, irritability, and decreased cognitive and psychomotor alertness, are typical complaints that motivate people to seek treatment.Citation10 These consequences of insomnia carry a heavy burden for both individuals and the society, as evidenced by their association with fatal accidents, human errors,Citation11 increased sick leave, reduced work capacity, increased health care utilization, and heightened risk of anxiety or depression.Citation11,Citation12
In addition to the social costs of insomnia, there are long-term effects of sleep problems on health. For example, sleep has profound effects on airway function. Indeed, asthma is reported to be the fifth most frequent physical condition related to insomnia, after headache, hypertension, obesity, and arthrosis.Citation13 Many people with asthma experience worsening of symptoms at night, and a greater proportion of people with asthma die at night as compared with general population.Citation14,Citation15 Factors contributing to the pathophysiology of nocturnal asthma are increased airway resistance and bronchial hyperreactivity, and diminished flow rates.Citation16 As one of the most common chronic medical conditions, currently affecting an estimated 235 million people worldwide,Citation17 asthma has reached historically high levels in the US,Citation18 and is associated with high health care utilization. Caused by allergies and respiratory sensitization,Citation19 asthma is exacerbated by active and passive smoking,Citation20,Citation21 viral infections, and poor indoor and outdoor air quality.Citation22
In addition to the above environmental factors, lifestyle factors also contribute to asthma symptom burden. For example, chronic heavy smoking in adulthood is a significant risk factor for insomnia.Citation20,Citation21,Citation23 In contrast, habitual physical activity is protective, reducing the prevalence of insomniaCitation24 and improving sleep quality.Citation25 Other relevant correlates of insomnia are affective disorders, such as depression and anxiety.Citation26–Citation31 Compared with people with no sleep difficulties, people with insomnia have an almost tenfold risk of clinical depression and more than a 17-fold risk of clinical anxiety.Citation27,Citation32
In order to improve interventions, it is important to understand social and mental health determinants of insomnia. Determinants of insomnia in asthma are not well understood. Therefore, the aim of this study was to investigate factors related to insomnia in a cohort of people with asthma.
Materials and methods
Data source
We analyzed data from the third wave of the Nord-Trøndelag Health Study (HUNT study), which is a large population database for medical and health-related research. The present study uses data from the most recent survey, HUNT3, which was carried out between October 2006 and June 2008. Nord-Trøndelag is located in central Norway. The area is fairly representative of Norway in terms of geography, economy, industry, and sources of income, as well as in terms of the age distribution, morbidity, and mortality rates of its inhabitants.Citation33,Citation34 The present study was approved by the Regional Committee for Ethics in Medical Research (2015/660) and by the HUNT Publication Review Board.
Study sample
All inhabitants in the county were invited to participate. From among 93,860 who were eligible for participation, 50,807 (54.1%) responded to the first questionnaire (Q1) that was enclosed with the invitation letter. The data were collected in each of the 24 municipalities in the county by using temporarily located health examination sites staffed by certified fieldwork teams. A second questionnaire (Q2) focusing more on symptoms and diseases was handed out to everyone to be completed at home, and returned by mail in a prepaid envelope. Respondents with lung diseases also participated in a substudy (n=12,128). Our data came from this substudy. Eligibility criteria for inclusion in our study sample were: 1) having a physician-confirmed diagnosis of asthma and 2) endorsing having had asthma symptoms in the year prior to the interview. Those who reported having a diagnosis of chronic obstructive pulmonary disease, chronic bronchitis, or emphysema were excluded from the study sample.
Measures
Insomnia
Participants were asked four questions on insomnia symptoms, which included how often during the last 3 months they had 1) experienced difficulties with falling asleep at night; 2) woke up repeatedly during the night; 3) woke up too early without being able to get back to sleep; and 4) felt sleepy during the day. Response options were: 1 (never/seldom), 2 (occasionally), or 3 (several times a week). A factor analysis yielded one component with an eigenvalue greater than 1.0 (). We computed a total sum score representing insomnia from these four items. This score ranged from 4 to 12, with higher scores reflecting more severe insomnia. The summary score had acceptable internal consistency reliability (Cronbach’s α=0.68). Thus, the HUNT3 questions assessing insomnia symptoms generated a unidimensional score with high internal consistency, and were a sound psychometric composite for analysis.
Table 1 Items and factor structure for insomnia and asthma impact measures
Asthma impact
Questions on the impact of asthma included how much they had experienced asthma symptoms in the last 7 days, and use of asthma medication. Specific questions were: 1) How many of the last 7 days have you noticed symptoms from your respiratory disease? 2) How many of the last 7 days have breathlessness restricted your normal activities (school, sport, work, housekeeping, etc)? and 3) How many of the last seven nights did you wake up/were affected by breathlessness (including cough)? A factor analysis generated one component (eigenvalue =1.78; Cronbach’s α=0.61; ). We thus created a subscale by adding the three asthma items into an asthma impact score, ranging from 0 to 21. Higher scores reflect more asthma symptoms. Thus, the HUNT3 questions assessing asthma impact generated a unidimensional score with high internal consistency, and were a sound psychometric composite for analysis.
Anxiety and depression
The Hospital Anxiety and Depression ScaleCitation35 was used to assess self-reported symptoms of anxiety and depression. The questionnaire consisted of 14 questions: seven for anxiety and seven for depression. Response options were on a 4-point scale ranging from 0 (not at all) to 3 (very often). Recall time was the last week. Responses were summed to provide separate scores for anxiety and depression symptoms, with possible scores ranging from 0 to 21 for each scale. Higher scores indicate greater likelihood of depression or anxiety.Citation35,Citation36 The psychometric properties of the scale have been validated previously.Citation36,Citation37 Cronbach’s α was 0.82 for the anxiety score and 0.76 for the depression score. A cutoff score of 8 on both subscales has been shown to give an optimal balance between sensitivity and specificity at ~0.80 for depression, according to the Diagnostic and Statistical Manual of Mental Disorders (III and IV) and the International Classification of Disorders (ICD-8 and 9).Citation38 The anxiety and depression scores were dichotomized according to this cutoff score for the present analyses.Citation36,Citation37
Demographic and lifestyle variables
The following variables were included to characterize the sample. Age was categorized in 6 decades, from 19 to 79 years, and one additional group with those 80 years and older. Partnership was dichotomized into those living with a partner and those living alone. Data on education were obtained from the National Population Registry of Norway, and highest completed education was classified as: 0, primary and lower secondary school – up to 10 years; 1, high school – 11–13 years; 2, university and high school, short; and 3, university and high school, long. Physical activity was assessed by the single item “How often do you perform exercise?” with response options as: 0, never; 1, less than once a week; 2, once a week; 3, two to three times a week; and 4, almost every day. Smoking was characterized as either “never smoking”, “quit smoking”, “now and then”, or “daily”, with yes/no response options. For daily smokers, number of cigarettes per day was also recorded. Questions on medications included use of prophylactic- and symptom-reducing medication.
Statistical analysis
Hierarchical series of multiple regression analyses were performed with insomnia as dependent variable. Mediation was tested by a multistage regression approach outlined by Baron and Kenny,Citation39 in which the three regression equations were estimated: first, regressing the mediator (M) on the independent variable (X); second, regressing the dependent variable (Y) on the independent variable (X); and third, regressing the dependent variable (Y) on both the independent variable (X) and on the mediator (M).Citation39 The mediator has been called an intervening or process variable. Complete mediation is the case in which variable X no longer affects Y after M has been controlled and so path c′ is zero. Partial mediation is the case in which the path from X to Y is reduced in absolute size but is still different from zero when the mediator is introduced.Citation40 The type I error rate was set to P<0.05, and all tests were two-tailed. The statistical analyses were carried out using SPSS 22.0 for Windows (IBM Corporation, Armonk, NY, USA).Citation41
Results
From the 3,348 participants who reported that they had, or ever had asthma, only those with a current asthma diagnosis, and with no missing data on sleep questions were included. The final asthma sample included 1,342 persons. The age range was 19–91 years (mean 53.0, standard deviation 1.8). The majority was female (60.3%), and there was a high prevalence of current tobacco smokers (33% smoking daily, and now and then). Approximately 11% reported a high level of depression and 18% had a high level of anxiety (). The asthma sample did not differ from the HUNT3 in age, partnership, or smoking. However, the asthma sample had more women (P≤0.001), a higher prevalence of insomnia (P≤0.001), and fewer people with more than 20 years of education compared with the HUNT3 (P≤0.035). Further, those with asthma had more anxiety (P≤0.001) and depression (P≤0.001), which is consistent with the research literature.Citation12
Table 2 Description of study population
Univariate regressions suggested that reporting insomnia was associated with being female, older, less educated, and/ or a smoker. It was also associated with never exercising, having worse reported asthma symptom impact, and reporting anxiety or depression (). Of study participants, more than 40% used asthma prophylactic medication, and nearly 28% reported that they had used a medication to reduce asthma symptoms in the past 3 days. We evaluated the medication variables in the univariate models, but they showed no significant association with insomnia, and were not kept for later models.
Table 3 Hierarchical multiple regression analyses (standardized beta coefficient) with insomnia as dependent variable (N=1,254)
shows the results of the hierarchical multiple regression analyses modeling the prediction of insomnia. Because all of the bivariate correlations between variables used in the analysis were r<0.7, we assumed no multicollinearity of variables (). Inspection of residuals indicated no violation of regression assumptions.
In step 1, controlling for demographic and lifestyle variables, female sex, higher age, current smoking, and never doing physical activity, were all independently associated with insomnia (P<0.001 for all variables). In step 2, asthma impact was entered into the model and was found to have an independent effect on insomnia (β=0.14, P<0.001). In step 3, depression was entered into the model and was found to have an independent effect on insomnia (β=0.36, P<0.001). Further, exercise was no longer a significant predictor of insomnia, suggesting that the beneficial impact of exercise was mitigated by depression symptoms. In step 4, anxiety was entered into the model along with the step 1 and step 2 covariates, and was found to have an independent effect on insomnia (β=0.39, P<0.001). In step 5, depression and anxiety were entered together into the model and were found to have independent effects on insomnia (β=0.20 and 0.28, respectively; P<0.001 in both cases). In step 6, two interaction terms were entered into the model (anxiety x asthma impact, and depression x asthma impact); both were not statistically significant.
Sociodemographic and lifestyle variables (step 1) explained 6.8% of the variance in explaining insomnia, whereas asthma impact (step 2) added only 1.9%. Anxiety and depression accounted for 16.6% variance (step 5), adding most to the explained 25.0% variance in the total model.
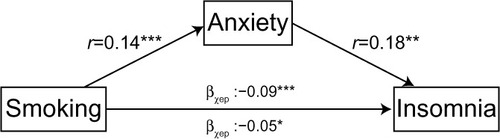
This hierarchical approach to modeling insomnia revealed that when anxiety was entered into the model (step 3), the previously significant direct relationship between smoking and insomnia (β=0.06, P<0.01) was no longer significant (β=0.05 in both steps 4 and 5; P=0.06 in step 4 and 0.08 in step 5). This pattern suggests that anxiety mediated the relationship between smoking and insomnia. displays the mediation model.
Discussion
Our findings from this large population-based survey suggest that insomnia in people with asthma is associated with demographic characteristics, lifestyle factors, and asthma impact. By far, the most important explanatory variables were anxiety and depression, accounting for two-thirds of the explained variance in the model. Further, we found that when we adjusted for anxiety, the predictive value of smoking diminished, suggesting that this affective problem mediates the relationship between smoking and insomnia.
Despite the cross-sectional structure of the data used in this secondary analysis, the mediation analysis allows the examination of potentially causal models to generate hypotheses for future longitudinal research.Citation40 As Kenny notes, the mediator is presumed to cause the outcome and not vice versa. One reason for testing mediation is to suggest a mechanism by which the variable affects the outcome. While it is known smoking in people with asthma is associated with anxiety,Citation31 research on the relationship between smoking and insomnia is inconclusive.Citation42,Citation43 In the present sample, more than 31% of the participants reported that they were current smokers. This is a surprising number given that these people have asthma and are likely aware of the harmful effect of cigarette smoking on their lungs. It also puts them at higher risk for the development of chronic obstructive pulmonary disease.Citation44–Citation46 Why would these people with asthma not quit smoking? Perhaps these people continue to smoke despite its harmful effects because nicotine has mood-altering effects that make quitting difficult.Citation47 While it is known that nicotine reduces depressionCitation47 and anxietyCitation48 in the short-term (ie, acute effects),Citation49 the relationship is a complex one.Citation48 For example, it is conceivable that over extended periods of time, smoking may actually induce negative affect, through the emergence of a withdrawal syndrome or some other mechanism.Citation50 Our findings suggest that the relationship between smoking and insomnia is related to heightened anxiety, but we are not able to determine whether this anxiety is alleviated or caused by the smoking due to the cross-sectional nature of the data.
It is also possible that other variables in our model interrelate with smoking, anxiety, and insomnia. For example, it is well known that anxiety and panic attacks are associated with asthma,Citation51 and most likely the relationship is bidirectional.Citation52 Persons with asthma having emotional problems may develop a vicious cycle between anxiety and symptoms; they may cope or self-medicate by smoking cigarettes to regulate their affect. This approach to managing their anxiety in the short-term may exacerbate their insomnia in the longer-term, and may lead to more negative affect due to the sleep deprivation (insomnia). This escalation in negative affect may in turn lead to more smoking. Future research might utilize longitudinal data from the HUNT study or another data source to investigate causal models of the relationship between smoking, anxiety, asthma symptoms, and insomnia in people with asthma.
Increase in asthma symptoms significantly associated with insomnia
In addition to the intriguing mediation effect discussed earlier, we also found robust independent effects of asthma impact on insomnia. Based on these findings, one might speculate that nocturnal asthma – exacerbations of asthma that occur during the night – may further disrupt sleep, causing difficulty initiating and maintaining sleep as well as poor overall sleep quality.Citation53,Citation54 Future research might examine the effectiveness of proactive or preventative use of asthma medication (eg, inhalers) just before going to bed at night to reduce insomnia.
Prescribing physical activity
Along with identifying health behaviors associated with worse insomnia, our model also identified a robust and independent impact of engaging in physical exercise in reducing insomnia. It is notable that this effect was mediated by depression, suggesting that the salutogenic effect of exercise is explained by (reduced) depression. Thus, engaging in exercise may reduce individuals’ depression symptoms and thus enable a good night’s sleep. When anxiety was entered into the model, this mediation effect was no longer present, suggesting that exercise did not buffer the impact of anxiety on insomnia. Since asthma guidelinesCitation55 aim to help people with asthma to remain active and sleep well, future research might investigate whether exercise-based interventions can be tailored to mitigate both depression and anxiety and thereby improve sleep in people with asthma.Citation55
Strengths and limitations of the study
This study has a number of notable strengths, including the sample size, the population-based sampling strategy, and the quality of the data collected. Our analyses built on these strengths to ask a research question with clear clinical significance and implications. The limitations of the present study must, however, be acknowledged. First, the main limitation is that the data were not collected for the purpose of the specific research question for our study. Consequently, the measures might not be the best operationalization of a construct of interest; the sample might not be the most fitting to ask the question (eg, including asthmatics who are using medications that could interfere with sleep). Second, although the HUNT3 has a reasonable compliance rate (54%)Citation56 for such a large study, nonparticipant analyses suggest that the study sample tends to include relatively healthy people (ie, those with a lower mortality rate), and underrepresents lower socioeconomic status.Citation56 Third, the flip side of the power advantages of large samples is that analyses of such sample can yield statistically significant findings that have questionable clinical significance. In our analysis, the difference in beta coefficients between model step 1 and 4 was 0.04, yet the significance changed from P<0.001 to P<0.06. Future research might replicate these analyses in an independent sample to evaluate their robustness. Finally, our mediation analysis is not able to make causal inferences about the relationships among the study variables. It is intended to suggest causal hypotheses that can be tested in future longitudinal investigations.
Conclusion
It is well known that an untreated sleep problem can have a negative effect on an individual’s physical and psychosocial functioning.Citation52,Citation57 We found that while the impact of asthma on insomnia is modest, smokers with asthma have more insomnia, and anxiety seems to mediate this relationship. Further, people with asthma who have symptoms of depression do not get the benefit of exercise on insomnia. Our findings would suggest that helping smokers to manage their anxiety and depression through behavioral methods may reduce their insomnia symptoms, and enable them to engage in other health-enhancing pursuits, such as physical exercise. Future research should investigate the impact on sleep and other health behaviors of behavioral interventions aimed at negative-affect reduction in people with asthma.
Author contributions
Both authors contributed to the conception and design, analysis, and interpretation of data. Further, RA drafted the article with substantial contributions from CES, and both authors revised it critically for important intellectual content, and approved the final version. The authors agree that they are accountable for all aspects of the work, confirming that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
The Nord-Trøndelag Health Study (the HUNT study) is a collaboration between the HUNT Research Centre (Faculty of Medicine, Norwegian University of Science and Technology), the Nord-Trøndelag County Council, the Central Norway Health Authority, and the Norwegian Institute of Public Health. The authors thank Carolina Campos, RN, MNSc for helpful discussions earlier in the course of this project. This study was performed at the Department of Nursing and Health Promotion, Oslo and Akershus University College, Oslo, Norway.
Disclosure
The authors report no other conflicts of interest in this work.
References
- MorinCMBencaRChronic insomniaLancet20123791129114122265700
- LichsteinKLTDanielJMcCraeChristina SInsomnia: epidemiology and risk factorsKrygerMHRothTDementWCPrinciples and Practice of Sleep Medicine5th edSt. Louis, MOElsevier Saunders2011827838
- ReiterJRosenDThe diagnosis and management of common sleep disorders in adolescentsCurr Opin Pediatr20142640741224932653
- KronholmEPuusniekkaRJokelaJTrends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011J Sleep Res20152431025367818
- TomSEKuhDGuralnikJMMishraGDSelf-reported sleep difficulty during the menopausal transition: results from a prospective cohort studyMenopause2010171128113520551846
- PartinenMHublinCEpidemiology of sleep disordersKrygerMHRothTDementWilliam CPrinciples and Practice of Sleep Medicine5th edSt. Louis, MOElsevier Saunders2011695715
- LeeKAMoeKMenopauseKrygerMHRothTDementWilliam CPrinciples and Practice of Sleep MedicineSt. Louis, MOElsevier Saunders201115921601
- FeinsilverSHSleep in the elderly. What is normal?Clin Geriatr Med20031917718812735121
- Ancoli-IsraelSShochatTInsomnia in older adultsKrygerMHRothTDementWCPrinciples and Practice of Sleep MedicineSt. Louis, MOElsevier Saunders201115441550
- LegerDPoursainBAn international survey of insomnia: under-recognition and under-treatment of a polysymptomatic conditionCurr Med Res Opin2005211785179216307699
- LaugsandLEStrandLBPlatouCVattenLJJanszkyIInsomnia and the risk of incident heart failure: a population studyEur Heart J2014351382139323462728
- MorinCMBencaRMInsomnia: nature, diagnosis, and treatmentMontagnaPChokrovertySHandbook of Clinical Neurology, Sleep DisordersPart II99AmsterdamElsevier B.V2011
- UhligBLSandTØdegårdSSHagenKPrevalence and associated factors of DSM-V insomnia in Norway: the Nord-Trøndelag Health Study (HUNT 3)Sleep Med20141570871324767721
- DouglasNJAsthma at nightClin Chest Med198566636742867849
- DouglasNJNocturnal asthmaQ J Med1989712792892594959
- KhanWHMohseninVD’AmbrosioCMSleep in asthmaClin Chest Med20143548349325156764
- WHOAsthma. Fact sheet 307.2013GenevaWorld Health Organization Available from: http://www.who.int/mediacentre/factsheets/fs307/en/Accessed October 19, 2015
- ZhangXMorrison-CarpenterTHoltJBCallahanDBTrends in adult current asthma prevalence and contributing risk factors in the United States by state: 2000–2009BMC Public Health201313115624325173
- PallasahoPJuuselaMLindqvistASovijarviALundbackBRonmarkEAllergic rhinoconjunctivitis doubles the risk for incident asthma – results from a population study in Helsinki, FinlandRespir Med20111051449145621600752
- CooganPFCastro-WebbNYuJO’ConnorGTPalmerJRRosenbergLActive and passive smoking and the incidence of asthma in the Black Women’s Health StudyAm J Respir Crit Care Med201519116817625387276
- MagnusMCHåbergSEKarlstadØNafstadPLondonSJNystadWGrandmother’s smoking when pregnant with the mother and asthma in the grandchild: the Norwegian Mother and Child Cohort StudyThorax20157023724325572596
- SubbaraoPMandhanePJSearsMRAsthma: epidemiology, etiology and risk factorsCMAJ2009181E181E19019752106
- BrookDWRubenstoneEZhangCBrookJSTrajectories of cigarette smoking in adulthood predict insomnia among women in late mid-lifeSleep Med2012131130113722901402
- InoueSYorifujiTSugiyamaMOhtaTIshikawa-TakataKDoiHDoes habitual physical activity prevent insomnia? A cross-sectional and longitudinal study of elderly JapaneseJ Aging Phys Act20132111913922832375
- YangPYHoKHChenHCChienMYExercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic reviewJ Physiother20125815716322884182
- OhayonMMRothTPlace of chronic insomnia in the course of depressive and anxiety disordersJ Psychiatr Res20033791512482465
- TaylorDJLichsteinKLDurrenceHHReidelBWBushAJEpidemiology of insomnia, depression, and anxietySleep2005281457146416335332
- KatonWJRichardsonLLozanoPMcCauleyEThe relationship of asthma and anxiety disordersPsychosom Med20046634935515184694
- de Miguel DíezJHernández BarreraVPuente MaestuLCarrasco GarridoPGómez GarcíaTJiménez GarcíaRPsychiatric comorbidity in asthma patients. Associated factorsJ Asthma20114825325821341970
- UrrutiaIAguirreUPascualSImpact of anxiety and depression on disease control and quality of life in asthma patientsJ Asthma20124920120822308974
- GadaEKhanDADeFinaLFBrownESThe relationship between asthma and self-reported anxiety in a predominantly healthy adult populationAnn Allergy Asthma Immunol201411232933224428963
- BaglioniCSpiegelhalderKNissenCRiemannDClinical implications of the causal relationship between insomnia and depression: how individually tailored treatment of sleeping difficulties could prevent the onset of depressionEPMA J2011228729323199164
- HolmenJMidthjellKØysteinKrügerThe Nord-Trøndelag Health Study 1995-97 (HUNT 2): objectives, contents, methods and participationNorsk Epidemiol2003131932
- LanghammerAKrokstadSRomundstadPHegglandJHolmenJThe HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptomsBMC Med Res Methodol20121214322978749
- ZigmondASSnaithRPThe Hospital Anxiety and Depression ScaleActa Psychiatr Scand1983673613706880820
- BjellandIDahlAAHaugTTNeckelmannDThe validity of the Hospital Anxiety and Depression Scale. An updated literature reviewJ Psychosom Res200252697711832252
- MykletunAStordalEDahlAAHospital Anxiety and Depression (HAD) scale: factor structure, item analyses and internal consistency in a large populationBr J Psychiatry200117954054411731359
- SivertsenBLallukkaTSaloPInsomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in NorwayJ Sleep Res20142312413224635564
- BaronRMKennyDAThe moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerationsJ Pers Soc Psychol198651117311823806354
- KennyDAMediation. 2014 Available from: http://davidakenny.net/cm/mediate.htmAccessed October 19, 2015
- IBM CorporationSPSS. Version 22Armonk, NYIBM Corporation
- MakK-KHoS-YThomasGNSmoking and sleep disorders in Chinese adolescentsSleep Med20101126827320176504
- SuttonDAMoldofskyHBadleyEMInsomnia and health problems in CanadiansSleep20012466567011560179
- HarmsenLGottliebVMakowska RasmussenLBackerVAsthma patients who smoke have signs of chronic airflow limitation before age 45J Asthma20104736236620528587
- VignoudLPinIBoudierASmoking and asthma: disentangling their mutual influences using a longitudinal approachRespir Med20111051805181421873041
- PerretJLWaltersEHAbramsonMJMcDonaldCFDharmageSCThe independent and combined effects of lifetime smoke exposures and asthma as they relate to COPDExpert Rev Respir Med2014850351424834459
- HughesJRSteadLFHartmann-BoyceJCahillKLancasterTAntidepressants for smoking cessationCochrane Database Syst Rev20141CD00003124402784
- KasselJDStroudLRParonisCASmoking, stress, and negative affect: correlation, causation, and context across stages of smokingPsychol Bull200312927030412696841
- KasselJDUnrodMSmoking, anxiety, and attention: support for the role of nicotine in attentionally mediated anxiolysisJ Abnorm Psychol200010916116610740949
- ParrottACDoes cigarette smoking cause stress?Am Psychol19995481782010540594
- GoodwinRDEatonWWAsthma and the risk of panic attacks among adults in the communityPsychol Med20033387988512877402
- HaslerGBuysseDJGammaAExcessive daytime sleepiness in young adults: a 20-year prospective community studyJ Clin Psychiatry20056652152915816796
- KlinkMEDodgeRQuanSFThe relation of sleep complaints to respiratory symptoms in a general populationChest19941051511548275723
- MastronardeJGWiseRAShadeDMOlopadeCOScharfSMSleep quality in asthma: results of a large prospective clinical trialJ Asthma20084518318918415823
- Institute NHLaBEPR 3 Guidelines on Asthma 2012 Available from: http://www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines/full-reportAccessed October 19, 2015
- KrokstadSLanghammerAHveemKCohort profile: the HUNT study, NorwayInt J Epidemiol20134296897722879362
- LuysterFSStrolloPJJrZeePCWalshJKSleep: a health imperativeSleep20123572773422654183