Abstract
Objectives
To describe our experience and the practical tools we have developed to facilitate early mobilization in the intensive care unit (ICU) as a multidisciplinary team.
Background
Despite the evidence supporting early mobilization for improving outcomes for ICU patients, recent international point-prevalence studies reveal that few patients are mobilized in the ICU. Existing guidelines rarely address the practical issues faced by multidisciplinary ICU teams attempting to translate evidence into practice. We present a comprehensive strategy for safe mobilization utilized in our ICU, incorporating the combined skills of medical, nursing, and physiotherapy staff to achieve safe outcomes and establish a culture which prioritizes this intervention.
Methods
A raft of tools and strategies are described to facilitate mobilization in ICU by the multidisciplinary team. Patients without safe unsupported sitting balance and without ≥3/5 (Oxford scale) strength in the lower limbs commence phase 1 mobilization, including training of sitting balance and use of the tilt table. Phase 2 mobilization involves supported or active weight-bearing, incorporating gait harnesses if necessary. The Plan B mnemonic guides safe multidisciplinary mobilization of invasively ventilated patients and emphasizes the importance of a clearly articulated plan in delivering this valuable treatment as a team.
Discussion
These tools have been used over the past 5 years in a tertiary ICU with a very low incidence of adverse outcomes (<2%). The tools and strategies described are useful not only to guide practical implementation of early mobilization, but also in the creation of a unit culture where ICU staff prioritize early mobilization and collaborate daily to provide the best possible care.
Conclusion
These practical tools allow ICU clinicians to safely and effectively implement early mobilization in critically ill patients. A genuinely multidisciplinary approach to safe mobilization in ICU is key to its success in the long term.
Introduction
Early progressive mobilization of adult intensive care unit (ICU) patients has been shown to be safe and feasible andCitation1,Citation2 result in reduced delirium,Citation3 improved functional outcomes,Citation4,Citation5 reduced hospital length of stay,Citation3,Citation6 and reduced mortality in patients with acute respiratory failure.Citation7 In a recent systematic review of physiotherapy in ICU, StillerCitation6 suggested that, given the evidence supporting the outcomes for early mobilization, “ICU physiotherapists should give priority to interventions aimed at early progressive mobilization”. However, point-prevalence studies from GermanyCitation8 and Australia and New ZealandCitation9 have demonstrated a low incidence of mobilization of patients with an endotracheal tube (8% in Germany and 0% in Australia and New Zealand).
Although there are several guidelines available that discuss the implementation of early mobilization in critically ill patients,Citation10–Citation13 few papers address the practical challenges faced by clinicians attempting to translate this evidence into practice. Our 31-bed mixed tertiary ICU had 1,976 admissions in 2015, with 50% requiring mechanical ventilation. Patients managed include medical, trauma, cardiothoracic, general, and neurosurgical patients. We have been practicing early mobilization and rehabilitation for over a decade, and it is well embedded in our unit culture across the multidisciplinary team (MDT) (physiotherapy, medical, nursing, and support staffCitation14). In this paper, we share the practical tools we have developed to educate and train staff in early mobilization across the spectrum of acuity, including patients with neurological diagnoses. Our approach is applicable to general ICU patients regardless of whether they are intubated and mechanically ventilated, noninvasively ventilated, or not requiring any ventilatory or airway support.
Prior to any mobilization episode, a comprehensive assessment and review of safety criteria should occur to minimize risk. This paper is intended to be used in conjunction with published expert consensus statementsCitation13,Citation15–Citation17 and recommendations and is focused more on the practical implementation of mobilization once a safety assessment has been completed in collaboration with the MDT.
Mobilization methods
We perform a daily assessment of all patients in the ICU regarding their suitability for mobilization with the aim of achieving the highest level of mobilization possible each day. To determine the type of mobilization, a stepwise approach is taken (). The first two steps are to assess the patient’s level of alertness and ability to follow instructions (eg, using the Richmond Agitation–Sedation Scale)Citation18 and identify if there are any other safety concerns or barriers to mobilization. The physiotherapist will discuss any safety concerns with senior medical staff to determine whether these factors should preclude mobilization. In particular, the team must also consider whether the patient has sufficient respiratory and cardiovascular reserve to perform the proposed mobilization task and if acceptable limits of organ support can be established to facilitate mobilization (eg, alteration of ventilator settings or increasing vasoactive infusions). If sedation can be weaned or barriers to mobilization overcome (eg, timing of procedures or tests), this is prioritized by the MDT early in the day to facilitate mobilization. If any member of the MDT has concerns about whether mobilization should proceed, this is discussed openly with the ICU physiotherapist and senior medical staff.
Figure 1 Mobilization flowchart.
Notes: (A) Decision making flowchart for mobilization of ICU patients. *If hemiplegic, ≥ 3/5 on intact side. (B) Nursing guideline for mobilization of ICU patients.
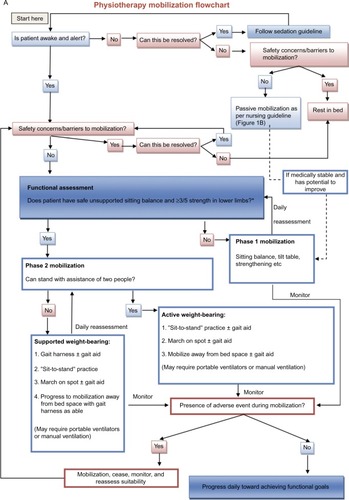
The flowchart in also reinforces the need to continuously monitor the patient during mobilization. For each patient, we clearly articulate and agree on target ranges for physiological parameters during mobilization, rather than arbitrary thresholds. It is important to remember that the normal physiological response to exercise includes an increase in heart rate and to allow for this when setting parameters. Mobilization may need to temporarily cease due to the patient’s physiological response to mobilization (eg, decrease in SpO2 and excessive increase in heart rate). However, after a period of monitoring and rest, mobilization may recommence. In the very rare circumstance of an adverse event,Citation14 mobilization ceases immediately and a referral is made for an urgent medical review.
Ultimately, treatment dosage and intensity should align with the specific goals of treatment for the individual patient, whether this is enhanced respiratory status, maintenance of global function or recovery of strength, endurance or balance deficits, or a combination of these. These goals are collaboratively determined by the physiotherapist, bedside nurse, and patient following assessment. Where patients are able to rate their perceived exertion,Citation19 this can be helpful in guiding treatment intensity and has shown to be reliable in mechanically ventilated patients.Citation20 For example, we may encourage a patient to work at a rated perceived exertion of 3–4 out of 10 while mobilizing around the ICU and reassure them that it will feel challenging at this point in their recovery.
Bed rest
Patients who are awake but must remain on bed rest due to the presence of safety criteria are assessed for their suitability to complete an in-bed exercise program. This program is individually prescribed to maintain strength and/or range of motion. Physiotherapists liaise closely with surgical and medical teams to clarify movement restrictions and duration of bed rest (eg, following pelvic fracture) to determine when active mobilization can commence.
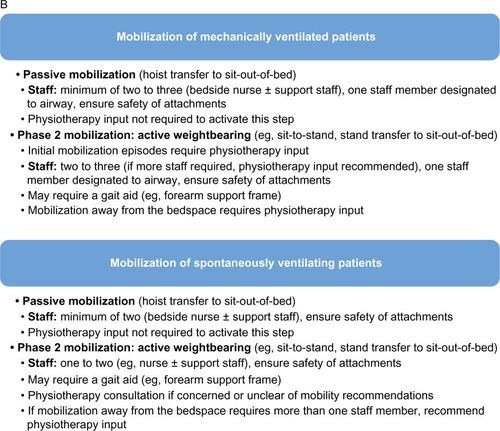
Passive mobilization
If the patient is unable to follow commands and actively participate in mobilization (eg, Richmond Agitation–Sedation Score <−1),Citation18 he or she may be suitable for passive mobilization (ie, hoist transfer to sit-out-of-bed, ). Even patients who are sedated and unresponsive may still benefit from the high sitting position in an appropriate chair to potentially minimize orthostatic intolerance, which is known to occur after just 24 hours of bed rest.Citation21 A portable sling lifter for mobilization is feasible and is a standard practice in our unit.
Active mobilization
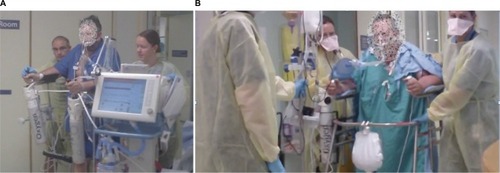
Once the decision to actively mobilize a patient is made, the next step requires the physiotherapist to complete a functional assessment, including a sitting balance and strength assessment. If the patient does not have at least 3/5 (Oxford scale) strength in their lower limbs or safe unsupported sitting balance, the patient commences “phase 1 mobilization” (). Phase 1 can involve sitting balance retraining (eg, reaching and returning to midline from the bed or chair), strength training including the use of weights or slings, and/or treatment on the tilt table (). Some patients in the passive mobilization group (eg, patients with a neurological diagnosis) may be assessed as suitable for “phase 1 mobilization” even if they are unable to participate in therapy or their level of consciousness fluctuates. A patient will remain in this phase until they achieve adequate sitting balance and lower limb strength to progress to “phase 2 mobilization”.
Figure 3 Phase 1 mobilization.
Notes: (A) Tilt table for an awake intubated patient performing squats with assistance. This patient was unable to achieve supported weight-bearing with a gait harness. Note the nurse managing airway and physiotherapists providing support to knees. (B) Sitting balance with a ventilator-dependent patient. Note the nurse providing airway support while physiotherapists assist balance behind and in front of the patient.

If the patient is not able to stand with the assistance of two staff, they progress to the “supported weight-bearing” phase, which involves the use of a gait harness to facilitate mobilization (). A gait harness can be suspended from overhead ceiling tracking or from a sling hoist lifter. For patients with several drains and attachments in the abdomen and thorax, we recommend noncircumferential gait harnesses () as these are less likely to result in compression or dislodgement of these items. The sling is ideally placed under the patient’s pelvis from a seated position. This sometimes requires the patient to be lifted with a standard sling, and then lowered onto the gait harness either on the edge of the bed or in a chair. We also recommend padding the gait harness with a disposable lining to reduce the need for laundering between treatments. Once transferred to a standing position, the patient can be assisted to extend the hips and knees as much as possible and step forward, or practice lateral weight shift.
Figure 4 Phase 2 mobilization: supported weight-bearing for an intubated patient with primary central nervous system pathology.

If the patient is able to stand with the assistance of two staff members, they proceed to the “active weight-bearing phase” (). Patients may require the use of a gait aid (eg, a forearm support frame), and some patients will require a sling hoist to sit out of bed, with more effective mobilization commencing from the chair. Mobilization is progressive both within and between treatments to achieve functional goals (, phase 2 mobilization).
Figure 5 Phase 2 mobilization: active mobilization of awake intubated patients.
Notes: (A) With a ventilator and portable monitoring. Note the spare oxygen cylinders suspended from the forearm support frame. Support staff are following the patient with a chair. (B) With resuscitator bag. Note the bariatric forearm support frame and organization of attachments on the portable pole. Both the physiotherapist and nurse are assisting the patient to steer the frame.
For some chronically critically ill patients, following discussion and planning with the MDT, it has been possible to complete rehabilitation sessions outside of the bed space, including the balcony area adjacent to our ICU and the rehabilitation gym. If rehabilitation is occurring outside the ICU location, we ensure an airway management kit is with the patient at all times, as well as nursing and medical escorts as appropriate. For example, we have had a mechanically ventilated patient complete a 30-minute therapy session in the rehabilitation gym, including treadmill training on a portable ventilator.
Mobilizing an invasively mechanically ventilated patient
Invasive mechanical ventilation, whether through an endotracheal or tracheostomy tube, should not be a barrier for mobilization and has been shown to be safe and feasible.Citation8–Citation10 Considerable planning and preparation is required to ensure safety for both patient and staff. We have developed the “Plan B” mnemonic () which is used routinely by staff in our unit before commencing mobilization of a mechanically ventilated patient.
Figure 6 Plan B mnemonic for mobilization of intubated patients.
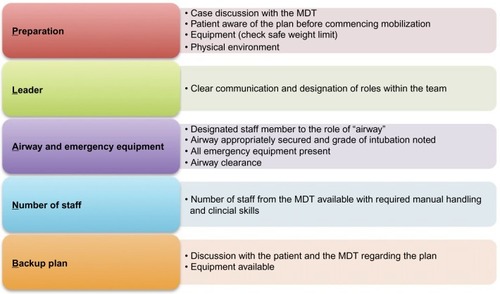
P – preparation
Preparation and planning are essential, as mobilization of an ICU patient requires coordination of the patient, several staff, and equipment. Timing of the mobilization episode needs to be negotiated with the bedside nurse and coordinated with other care needs (eg, procedures and scans). In our experience, 30–60 minutes is a reasonable time frame to allocate for mobilization of a ventilated patient, including preparation time. Mobilization should be timed to coincide with medication peak effectiveness where applicable (eg, analgesia and bronchodilators). Equipment requirements may include portable monitoring, overhead ceiling-mounted tracking or portable sling lifters, gait harnesses, tilt table, gait aid (eg, forearm support frame), a suitable recliner chair, and linen. If mobilizing away from the bed space, other equipment may include portable oxygen, portable suction, and either a portable ventilator or resuscitator bag. When using a portable ventilator, a spare oxygen cylinder should accompany the patient to guarantee adequate oxygen supply. The safe weight limit of all equipment should be checked with the patient’s body weight. When using gait harnesses, patency of all lines and attachments should be checked prior to proceeding with and at multiple time points during mobilization.
Preparation of the awake ventilated patient should include provision of a clear explanation of the plan, process, goals, and rationale for mobilization, answering questions, and providing reassurance as required.
A final review of the physical environment (eg, the bed space) completes the preparation phase. This must include a consideration of lines and attachments to ensure that there is adequate space to perform mobilization safely. If lines are to be removed imminently, consider delaying mobilization until after this has occurred. Often, it is possible to rationalize attachments to reduce the number of staff required for safe mobilization. It is highly recommended to remove any unnecessary equipment and clutter out of the area.
L – leader
Throughout the mobilization episode, it is imperative that there is a clear leader. In our unit, this is usually the physiotherapist, coordinating between the patient, the bedside nurse, support staff, and sometimes, family members as well. Members of the mobilization team must have a clear understanding of their role (eg, airway, attachments, patient, and frame) with clear communication throughout the treatment. However, while the physiotherapist may typically lead the mobilization, the person responsible for the airway reserves the right to revert to a leadership role at any point, as airway safety must be the first priority. In this case, in our unit, the physiotherapist would temporarily transfer leadership to the bedside nurse who is usually responsible for the airway. These leadership transfers are articulated clearly so that the whole team is aware of the change to ensure patient safety.
A – airway and emergency equipment
All mobilization episodes should aim to minimize patient risk. Emergency equipment including emergency airway and ventilation equipment should be checked as part of routine nursing practices. Discussion with the ICU medical team prior to mobilization is recommended for any patient with an identified “difficult airway” (eg, documented grade 3 or 4 Modified Cormack–Lehane score at the time of intubation) or if there is any concern regarding airway stability. Prior to mobilization, all artificial airways should be reviewed and appropriately secured. One staff member (usually the bedside nurse) is dedicated to the role of “airway” and is responsible for supporting the airway to prevent tube migration or displacement. For patients with a high sputum load, airway clearance is recommended prior to any mobilization. If mobilizing a patient with a high sputum load away from the bed space, portable suction must be available.
N – number of staff
The number of staff required to safely mobilize a critically ill patient is risk-assessed on the basis of the patient’s functional assessment. The minimum number of staff required to mobilize a ventilated patient in our ICU is two (one bedside nurse for the airway and one physiotherapist for the patient), but this is only possible where the patient requires minimal physical support. More commonly, we require between three and five staff members to mobilize a ventilated patient and safely manage all the lines and attachments. Our ICU staffing includes dedicated support staff who are available to assist with mobilization. Alternatives could include other nursing or physiotherapy staff or allied health assistants. It is essential that the MDT members are trained in safe manual handling and have a clear understanding of each other’s roles.
B – backup plan
Before mobilization, the leader should clearly articulate the backup plan, which may occur if the patient is unable to complete the planned mobilization episode. The patient should also be aware of the backup plan, so that they are aware of the possible change in direction midtreatment. Examples of this include having the bed nearby, a chair, commode, or wheelchair to follow the patient if mobilizing away from the bed space or a gait harness to prevent a fall in a high-risk patient. Sometimes the backup plan is simply to sit the patient back in the chair if the patient has insufficient standing ability to proceed.
Discussion
We have described strategies to guide the practicalities of safe early mobilization of ICU patients, including those who are unable to actively participate. This approach has been used successfully in our ICU for more than 10 years with a very low incidence of adverse outcomes, ie, 1.1%.Citation14 The two “adverse outcomes” in our audit were both instances of hypotension requiring intervention (ie, return to bed, fluid loading, and transient increase in vasopressor requirements) with no long-term consequences. This is consistent with other available safety data, including a recent review which reported an incidence of ≤4% adverse events with early mobilization in ICUCitation22 and a study of 5,267 ICU physical therapy sessions where a physiological abnormality or a potential safety event occurred in 34 (0.6%) sessions.Citation23
Progressive mobilization protocols have been published from the United StatesCitation3,Citation12,Citation24 and the United Kingdom.Citation11 Bassett et alCitation12 published a goal-directed progressive mobility continuum including safety criteria. All these protocols involve the initial step of passive range of motion exercises. Our clinical practice differs as no member of our MDT routinely performs passive range of motion exercises given the absence of evidence that these reduce or prevent contractures in critically ill patients.Citation25,Citation26 The absence of passive mobilization is consistent with surveyed Australian intensive care physiotherapy practice.Citation27 Another important distinction from other protocols is that we aim to sit our patients out of bed for a minimum of 4 hours per day with pressure care performed in the chair. Although Bassett et alCitation12 targets a frequency of mobilization at two to three times per day, we have opted to individualize the frequency of mobilization. Many of our patients are unlikely to tolerate this frequency due to fatigue. Fatigue was a limiting factor in a recent randomized controlled trial of a protocolized rehabilitation program commencing in ICU, where exercise prescription was targeted to be delivered twice per day but was only feasible in 55% of potential sessions.Citation28
Despite the evidence in favor of early mobilization, substantial barriers exist in many ICUs, including our own. In 2008, we audited our mobilization practice and found that patients were mobilized on 54% of patient days, with avoidable factors identified in 47% of cases where patients were not mobilized.Citation14 Specifically, the most common perceived barriers were femoral vascular access, (particularly femoral dialysis catheters), timing of procedures, and patient agitation or low level of consciousness. More recent evidence indicates that femoral access should not prohibit early mobilization,Citation29 and, in the case of dialysis catheters, mobilization may actually prolong filter life.Citation30 Other potential barriers to mobilization may include staffing, equipment, leadership, referral processes, delirium, sedation, and perceived lack of safety. Strategies to overcome these barriers have been published to assist clinicians in increasing mobility in ICU.Citation10,Citation31
Our ICU sedation practices are goal-directed to achieve a target Richmond Agitation–Sedation Score.Citation18 For patients in whom deep sedation is not indicated, sedation is targeted to achieve a Richmond Agitation–Sedation Score of −1 to 1, as opposed to daily sedation interruption. Oversedation may be a barrier to mobilization, may contribute to delirium, and compromise the patient’s ability to participate in mobilization. Review of sedation practices may be a key step in increasing mobilization in critically ill patients. A strategy to reduce heavy sedation and increase mobilization in medical ICU patients has been shown to be safe, reduce delirium, improve function, and reduce ICU and hospital length of stay.Citation1 The optimization of sedation to facilitate mobilization clearly requires close multidisciplinary collaboration between medical, nursing, and physiotherapy staff. In our ICU, this interaction and negotiation occurs frequently not just in handover meetings and ward rounds, but ad hoc across the day as issues arise. This open multidisciplinary communication requires mutual respect for each other’s roles and expertise, and an understanding of the priorities of competing demands for care of acutely unwell patients.
The description of our experience and approach to early mobilization in ICU adds to the body of evidence by providing specific practical details of how to perform this safe and feasible intervention as a MDT. A limitation of the material presented in this paper is that the ideal timing, type, frequency, intensity, and duration of mobilization required to prevent or minimize functional impairments in ICU survivors are yet to be established. Our approach is a feasible bundle of care that promotes early mobilization in critically ill patients; however, the effect of the individual components cannot be currently demonstrated. Given the heterogeneity of general ICU presentations, individualized goal-directed prescription is warranted. Clinicians need to make informed patient-centered decisions balancing the risks of prolonged bed rest against the benefits of early mobilization. Due to the multidisciplinary nature of the ICU environment, the decision to mobilize an ICU patient should be shared between the physiotherapy, medical, and nursing staff.
Developing and sustaining an ICU MDT culture that promotes, values, and prioritizes early mobilization is essential to translating evidence into clinical practice. Numerous articles are available to assist in units developing an early mobilization culture.Citation1,Citation10,Citation12,Citation16,Citation32,Citation33 In our experience, early mobilization is both feasible and safe and is the result of a concerted commitment from the MDT to make early mobilization the norm, rather than the exception. It is also possible that, despite the contrast of our approach with other published guidelines, we are still too conservative, and the limits of early proactive rehabilitation in ICU are yet to be established.
Conclusion
Early progressive mobilization is safe and feasible in critically ill patients and requires close collaboration of the MDT on a daily basis. It is our hope that the guided clinical reasoning and practical considerations described in this paper will provide tools that allow frontline clinical staff to implement early mobilization in the majority of critically ill patients in a safe and effective manner.
Acknowledgments
The authors gratefully acknowledge the staff of the Physiotherapy Department and Intensive Care Unit of Canberra Hospital for their support in developing this protocol. They also gratefully acknowledge the patients, students, and staff who each kindly consented to publication of the photographs in this report. They thank the Canberra Hospital ICU Research Executive Committee and the ACT Health Chief Allied Health Office for their financial support of this publication.
Disclosure
The authors report no conflicts of interest in this work.
References
- NeedhamDMKorupoluRZanniJMEarly physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement projectArch Phys Med Rehabil201091453654220382284
- BaileyPThomsenGESpuhlerVJEarly activity is feasible and safe in respiratory failure patientsCrit Care Med200735113914517133183
- MorrisPEGoadAThompsonCEarly intensive care unit mobility therapy in the treatment of acute respiratory failureCrit Care Med20083682238224318596631
- SchweickertWDPohlmanMCPohlmanASEarly physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trialLancet200937396781874188219446324
- KayambuGBootsRParatzJPhysical therapy for the critically ill in the ICU: a systematic review and meta-analysisCrit Care Med20134161543155423528802
- StillerKPhysiotherapy in intensive care: an updated systematic reviewChest2013144382584723722822
- MorrisPEGriffinLBerryMReceiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failureAm J Med Sci2011341537337721358312
- NydahlPRuhlAPBartoszekGEarly mobilization of mechanically ventilated patients: a 1-day point-prevalence study in GermanyCrit Care Med20144251178118624351373
- BerneySCHarroldMWebbSAIntensive care unit mobility practices in Australia and New Zealand: a point prevalence studyCrit Care Resusc201315426026524289506
- EngelHJNeedhamDMMorrisPEGropperMAICU early mobilization: from recommendation to implementation at three medical centersCrit Care Med2013419 Suppl 1S69S8023989097
- McWilliamsDWeblinJAtkinsGEnhancing rehabilitation of mechanically ventilated patients in the intensive care unit: a quality improvement projectJ Crit Care2015301131825316527
- BassettRDVollmanKMBrandweneLMurrayTIntegrating a multidisciplinary mobility programme into intensive care practice (IMMPTP): a multicentre collaborativeIntensive Crit Care Nurs2012282889722227355
- HodgsonCLStillerKNeedhamDMExpert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adultsCrit Care201418665825475522
- LeditschkeIAGreenMIrvineJBissettBMitchellIAWhat are the barriers to mobilizing intensive care patients?Cardiopulm Phys Ther J2012231262922807652
- StillerKSafety issues that should be considered when mobilizing critically ill patientsCrit Care Clin2007231355317307115
- GosselinkRBottJJohnsonMPhysiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill PatientsIntensive Care Med20083471188119918283429
- HanekomSBerneySMorrowBThe validation of a clinical algorithm for the prevention and management of pulmonary dysfunction in intubated adults – a synthesis of evidence and expert opinionJ Eval Clin Pract201117480181020630012
- SesslerCNGosnellMSGrapMJThe Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patientsAm J Respir Crit Care Med2002166101338134412421743
- BorgGRatings of perceived exertion and heart rates during short-term cycle exercise and their use in a new cycling strength testInt J Sports Med1982331531587129724
- PowersJBennettSJMeasurement of dyspnea in patients treated with mechanical ventilationAm J Crit Care19998425426110392226
- KhanMHKunselmanARLeuenbergerUAAttenuated sympathetic nerve responses after 24 hours of bed restAm J Physiol Heart Circ Physiol20022826H2210H221512003830
- AdlerJMaloneDEarly mobilization in the intensive care unit: a systematic reviewCardiopulm Phys Ther J201223151322807649
- SricharoenchaiTParkerAMZanniJMNelliotADinglasVDNeedhamDMSafety of physical therapy interventions in critically ill patients: a single-center prospective evaluation of 1110 intensive care unit admissionsJ Crit Care201429339540024508202
- EngelHJTatebeSAlonzoPBMustilleRLRiveraMJPhysical therapist-established intensive care unit early mobilization program: quality improvement project for critical care at the University of California San Francisco Medical CenterPhys Ther201393797598523559525
- StockleyRCMorrisonJRooneyJHughesJMove it or lose it? A survey of the aims of treatment when using passive movements in intensive careIntensive Crit Care Nurs2012282828722196234
- PrabhuRKSwaminathanNHarveyLAPassive movements for the treatment and prevention of contracturesCochrane Database Syst Rev201312CD00933124374605
- WilesLStillerKPassive limb movements for patients in an intensive care unit: a survey of physiotherapy practice in AustraliaJ Crit Care201025350150819819105
- BerneySHainesKSkinnerEHDenehyLSafety and feasibility of an exercise prescription approach to rehabilitation across the continuum of care for survivors of critical illnessPhys Ther201292121524153522879441
- DamlujiAZanniJMMantheiyEColantuoniEKhoMENeedhamDMSafety and feasibility of femoral catheters during physical rehabilitation in the intensive care unitJ Crit Care2013284535.e9e1523499419
- WangYTHainesTPRitchiePEarly mobilization on continuous renal replacement therapy is safe and may improve filter lifeCrit Care2014184R16125069952
- LipshutzAKMEngelHThorntonKGropperMAEarly mobilization in the intensive care unit: evidence and implementationICU Director20123101016
- BaileyPPMillerRR3rdClemmerTPCulture of early mobility in mechanically ventilated patientsCrit Care Med20093710 SupplS429S43520046131
- DafoeSChapmanMJEdwardsSStillerKOvercoming barriers to the mobilisation of patients in an intensive care unitAnaesth Intensive Care201543671972726603796

