 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
A consequence of HIV infection is sensory neuropathy, a debilitating condition that degrades the quality of life of HIV patients. Furthermore, life-extending antiretroviral treatment may exacerbate HIV sensory neuropathy. Analgesics that relieve other neuropathic pains show little or no efficacy in ameliorating HIV sensory neuropathy. Thus, there is a need for analgesics for people with this particular pain. While lidocaine is used in the management of painful peripheral neuropathies, another local anesthetic mepivacaine, with a potentially improved bioavailability, could be utilized for the management of HIV neuropathic pain.
Methods
The efficacy of topical anesthetics was evaluated in a preclinical rodent model of painful peripheral neuropathy induced by epineural administration of the HIV envelope protein gp120 delivered using saturated oxidized cellulose implanted around the sciatic nerve. Beginning at 2 weeks following gp120 administration, the effects of local anesthetics topically applied via gauze pads were tested on heat and mechanical hyperalgesia in the hind paw. Rats were tested using several concentrations of mepivacaine or lidocaine during the following 2 weeks.
Results
By 2 weeks following epineural gp120 implantation, the ipsilateral hind paw developed significant hypersensitivity to noxious pressure and heat hyperalgesia. A short-lasting, concentration-dependent amelioration of pressure and heat hyperalgesia was observed following topical application of mepivacaine to the ipsilateral plantar hind paw. By contrast, topical lidocaine ameliorated heat hyperalgesia in a concentration-dependent manner but not pressure hyperalgesia. Equipotent concentrations of mepivacaine and lidocaine applied topically to the tail of mice significantly increased tail withdrawal latencies in the tail flick test, demonstrating that both local anesthetics attenuate responding to a brief noxious stimulus.
Conclusion
These findings showed that mepivacaine, rather than lidocaine, consistently attenuated two distinct symptoms of neuropathic pain and suggest that topical formulations of this local anesthetic could have utility in the alleviation of clinical HIV neuropathic pain.
Introduction
Distal sensory polyneuropathies are the most common and disabling neurological consequence of HIV infection. Symptoms of HIV sensory neuropathies include numbness and sensory loss but are frequently accompanied by persistent neuropathic pain which can significantly diminish the quality of life and daily functioning of these patients.Citation1–Citation6 HIV neuropathic pain is reminiscent of other neuropathic pains such as painful diabetic neuropathy, which is characterized by burning sensations, sharp stabbing, and paresthesias, predominantly affecting the distal innervation of the feet and hands. While there are a number of treatments that have been used in managing other peripheral neuropathic pains, including anticonvulsants such as pregabalin and antidepressants such as amitriptyline, none of these have demonstrated significant efficacy in HIV neuropathic pain.Citation5,Citation7–Citation10
Topical local anesthetics, such as lidocaine, are recommended as a first-line therapy in postherpetic neuralgia and other localized neuropathic pains.Citation11,Citation12 There are significant benefits in using topical anesthetics in pain management, such as use on an as-needed basis rather than adherence to a fixed dosing schedule for parenteral medications and safety. With regard to painful HIV-associated neuropathy, there are no available data from placebo-controlled randomized clinical trials demonstrating the efficacy of topically applied local anesthetics. Indeed, in the only available placebo-controlled randomized clinical trial of topical lidocaine, there were no significant differences in efficacy from placebo.Citation13
Mepivacaine, a structural analog of bupivacaine with distinct pharmacokinetics,Citation14 could be more suitable for distal neuropathies, such as painful diabetic neuropathy and HIV neuropathy, which primarily involves the feet, in contrast to postherpetic neuralgia which involves more proximal areas such as the thorax. Mepivacaine has improved bioavailability due to its intrinsic vasoconstrictor effect, reducing the rate at which the drug is cleared away from the site of application. In addition, mepivacaine may have improved neurological safety, as it showed the least neurotoxic effects on developing or regenerating primary cultured neurons among a series of local anesthetics tested, with lidocaine having the highest neurotoxic potential.Citation15 Mepivacaine has been used clinically for intraganglionic nerve blocksCitation16 but has not been tested for topical application in neuropathic pain.
A preclinical model of HIV-induced neuropathy has been previously described which demonstrates robust signs of neuropathic pain.Citation17,Citation18 Although the pathogenic mechanisms underlying HIV-associated neuropathies are poorly understood, direct involvement of viral proteins such as gp120 in producing neurotoxicity and axonal degeneration has been suggested by in vitro and in vivo studies.Citation19–Citation24 Epineural placement of gp120 around the sciatic nerve results in an inflammatory response in the peripheral nerve and subsequent development of increased responsiveness of the hind paw to noxious stimuli (“hyperalgesia”). A number of clinical analgesics have been tested in this model, but the efficacy of a topical local anesthetic has not been evaluated.Citation18 Thus, the current study evaluated the antinociceptive effects of topically applied mepivacaine in a rat model of HIV-associated peripheral neuropathic pain. Portions of this work were presented previously as a poster at scientific conferences.Citation25,Citation26
Methods
Animals
To evaluate the effects of topical anesthetics in a model of HIV-associated neuropathic pain, male Sprague Dawley rats (Harlan Sprague Dawley Inc., Indianapolis, IN, USA) weighing 150–200 g at delivery were used. For assessment of anesthetic effects following topical application to normal skin using the radiant tail flick assay, male mice (C57BL/6; Charles River Laboratories, Wilmington, MA, USA) weighing 15–20 g at delivery were used. Animals were housed in a temperature-controlled environment (22°C±1°C, 30%–55% humidity) under a 12-hour light/dark cycle two animals per cage (rats) or five animals per cage (mice). Food and water were available ad libitum. Animals were acclimatized to the housing facility for at least 1 week prior to the start of the studies. All animal procedures followed National Institutes of Health guidelines concerning the care and use of laboratory animals and were reviewed and approved by the University of Miami Animal Care and Use Committee.
Rat gp120 HIV-associated neuropathic pain model
The rat gp120 model was induced by application of HIV envelope protein gp120 to the sciatic nerve; the virus itself was not utilized.Citation17 Under isoflurane anesthesia, the left sciatic nerve was isolated under aseptic surgical conditions by blunt dissection of the biceps femoris, without damaging the perineurium. Oxidized cellulose (Oxycel®; BD, Franklin Lakes, NJ, USA) was used as a carrier matrix to deliver gp120 directly to the sciatic nerve. Oxycel was prepared in strips of ~8 mm length and 4 mm width, and saturated with a 50 µL solution containing 300 ng gp120 in water (HIV-1 MN recombinant [Baculovirus], Product 1021-2; Immunodiagnostics, Inc., Bedford, MA, USA). The Oxycel was wrapped loosely around the sciatic nerve 2–3 mm proximal to the trifurcation using care not to cause any nerve constriction. Following Oxycel implantation, the muscular layer was closed using 3-0 silk, and the skin sealed with veterinarian-grade cyanoacrylate. Animals were held in recovery for observation for ~24 hours post-surgery and then returned to their home cages and checked daily. These procedures resulted in the development of neuropathic pain symptoms (mechanical and thermal hyperalgesia and allodynia) by ~2 weeks following gp120 application.Citation17
Behavioral testing
Rat gp120 hyperalgesia
In rats, behavioral testing was conducted before and 2 weeks after gp120 administration to determine baseline responses prior to local anesthetic administration. For assessment of pressure hyperalgesia, responsiveness to an increasing force (measured in grams) applied to the plantar hind paw was measured with a Randall-Selitto apparatus (Ugo-Basile SRL, Monvalle, Italy). The rat was loosely wrapped in a towel, and the hind paw placed on the apparatus’ pedestal. A plinth was gently lowered onto the hind paw, and the apparatus activated. A gradually increasing force (32 g/s) was applied until the rat withdrew its paw from the apparatus. The presurgical withdrawal threshold of naïve rats was ~175 g, and a cut-off of 500 g was assigned in the absence of a response. For assessment of thermal hyperalgesia, responsiveness to a brief, noxious heat stimulus was measured using an apparatus previously described.Citation27 Rats were placed on an elevated glass surface and allowed to acclimate for ~15 minutes prior to baseline testing. An infrared emitter was positioned beneath one of the paws. The length of time between initiation of the stimulus and withdrawal of the rat’s hind paw from the stimulus was recorded by the apparatus (measured in seconds). The stimulus intensity was adjusted to result in mean presurgical baseline latencies of 10–12 seconds, with a cut-off of 20 seconds in the absence of a response used to avoid skin damage. Because of the short duration of the anesthetic, the response to the infrared stimulus was tested once.
Mouse tail flick test
The gp120 model was used to study the potential beneficial effects of topical anesthetic treatment of neuropathic pain resulting from HIV sensory neuropathy. However, it is important to compare topical anesthetic effects in a model of sensitivity to acute pain in non-injured animals commonly used for antinociceptive testing. Toward this end, the mouse tail flick assay was selected as a simple screen for antinociceptive effects to noxious thermal stimulation.
In the mice, responsiveness of the tail to brief, noxious heat stimulation was determined using a Tail Flick Analgesia Meter (Model 33; IITC, Inc., Woodland Hills, CA, USA; set at sensitivity 7.5 and beam 5.0). Tail flick latencies (in seconds) were measured on the distal 3 cm region of the tail at baseline by applying a focused beam of light (thermal stimulus) to the ventral aspect of the tail. The tail flick latency is the time interval between onset of the heat stimulus and withdrawal of the tail from the beam. A maximum cut-off latency of 8 seconds was used to prevent tissue damage.
For assessment of local anesthetic effects on normal skin, treatments were administered topically to the mouse tail by immersion of the distal portion of the tail (3 cm) in drug or vehicle solutions for 5 minutes. Tail flick latencies were determined immediately after removal of the tail from the solution and again at 5 and 10 minutes. Testing of the drugs was done in a pseudo-Latin square design by an observer blinded to treatment assignment.
Local topical anesthetics
Pharmaceutical-grade mepivacaine base was procured from Cambrex Karlskoga AB (Karlskoga, Sweden). The local anesthetic lidocaine was selected as a “gold standard” comparator, since this agent is clinically utilized as a topical analgesic.Citation11,Citation12,Citation28,Citation29 Lidocaine base (American International Chemical, Inc., Framingham, MA, USA), manufactured by Gufic Biosciences (Mumbai, India) (Lot No. 1049), was provided by Relmada Therapeutics, Inc. (New York, NY, USA). Dimethyl sulfoxide was procured from Sigma-Aldrich Co. (St Louis, MO, USA). Fresh drug solutions were prepared on each test day. On the day of testing, dimethyl sulfoxide was diluted with distilled water to prepare a 90%:10% (v/v) solution to serve as the vehicle. Since the purpose of the study was to compare potency of topical mepivacaine with more commonly used clinical local anesthetic lidocaine, a wide range of concentrations of both agents was used. Drugs were serially diluted in vehicle and mixed by vortexing, to achieve concentrations ranging from 2 to 32 mM.
Application of topical anesthetics to the hind paw of the rat gp120 model
For local anesthetic delivery to the rat hind paw in the region where noxious stimuli were to be delivered, a 2×2 in gauze pad was saturated with either drug or vehicle and secured to the left plantar hind paw with Parafilm for 5 minutes. Following removal of the pad, rats were immediately tested. Rats were tested again at 5 and 10 minutes after removal of the pad.
Due to the rapid onset and short duration of topical application of local anesthetic agents, animals were evaluated for thermal or mechanical responses in separate groups. In order to minimize the number of animals, rats were tested for responses to several drugs/concentrations over the 2-week period following induction of neuropathic pain, with at least 48-hour intervals between testing days. Drug dosing was done using pseudo-Latin square design by an observer blinded to treatment assignment, and continued until n=6–9 animals were accrued for each drug concentration and pain test (each animal was used four to five times). Although each animal did not receive all possible treatments, all concentrations were given to at least one animal on each test day in order to minimize effects of day-to-day environmental variables. The continued presence of hyperalgesia in the rats was confirmed by predrug application baseline testing on each test day.
Application of topical anesthetic to the mouse tail
For this part of the study, 4 and 10 mM lidocaine concentrations (based on the effective concentration range of this agent determined using the mouse tail flick testCitation30) were compared with higher concentrations of mepivacaine (8, 16, and 32 mM).
Statistical analysis
Statistical comparisons for changes in thermal and mechanical hyperalgesia in the gp120 model and mouse tail flick latencies were performed using two-way analysis of variance (repeated measures) and the Newman–Keuls test for multiple post hoc analysis (SigmaPlot 12.0). The data were also analyzed as a percent change in baseline response:
(1) wherein “drug effect” = withdrawal threshold (in grams) or withdrawal latency (in seconds) following drug or vehicle treatment, and “predrug effect” = withdrawal threshold (in grams) or withdrawal latency (in seconds) prior to drug or vehicle treatment. Thus, a 100% change is antinociceptive, whereas a 0% change indicates no efficacy. The percent change, withdrawal threshold, and latency data were presented as mean ± standard error of the mean.
Since a reduction in symptom severity by 30%–50% is considered a clinically relevant therapeutic outcome in the management of neuropathic pain, “analgesia” was defined quantally as a response ≥33% increase over baseline calculated for an individual animal.Citation2,Citation5 The percentage of all rats that demonstrated such a response is presented. Data are graphically represented using GraphPad Prism software. Statistical significance was declared if the two-sided P-value was <0.05.
Results
Effects of topical mepivacaine on gp120-induced neuropathic hyperalgesia
Baseline responses to noxious pressure () and noxious heat () are shown prior to gp120 surgery (“pre-gp120”) and at 2 weeks following gp120 sciatic nerve exposure (“predrug”). Neither pre-gp120 nor predrug scores differed between any of the treatment groups (P>0.05 at these test points, for both mechanical and heat tests). Epineural placement of gp120 around the rat sciatic nerve via Oxycel carrier resulted in significantly decreased thresholds of withdrawal from pressure () and decreased latencies to withdrawal from noxious heat (), suggesting the emergence of pressure and heat hyperalgesia, respectively, 2 weeks following epineural gp120 administration.
Figure 1 Effect of topically applied mepivacaine on mechanical hyperalgesia in rats with gp120-induced neuropathic pain.
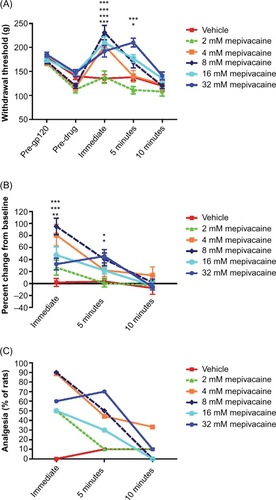
Figure 2 Effect of topically applied mepivacaine on thermal hyperalgesia in rats with gp120-induced neuropathic pain.
Topical administration of mepivacaine produced significant antinociception (overall F [df 5,4] =59.5, P<0.001) as indicated by an increase in withdrawal threshold (). By contrast, vehicle treatment alone did not significantly alter withdrawal thresholds. The antinociceptive effects of mepivacaine on gp120-induced mechanical hyperalgesia were most robust immediately following removal of the topical bandage, and tended to dissipate over the next 5–10 minutes. Significant antinociceptive effects were achieved by mepivacaine concentrations 4, 8, 16, and 32 mM (P<0.001 compared with vehicle treatment). No significant reversal of pressure hyperalgesia was observed with the lowest tested mepivacaine concentration (2 mM). Antinociceptive effects were sustained for at least 5 minutes following removal of the adhesive containing the two highest concentrations of mepivacaine (P<0.05 and P<0.001 for 16 and 32 mM, respectively).
Results are shown as percent change from predrug baselines in . Using this evaluation, all concentrations of mepivacaine appeared to increase mechanical thresholds from baseline, although statistically significant increases from individual baseline responses were reached only immediately following gauze pad removal (P<0.001 at 4 and 8 mM concentrations and P<0.01 at 16 mM concentration compared with vehicle) or at 5 minutes (P<0.05 at 8 and 32 mM concentrations compared with vehicle).
Data were also evaluated using a 33% “analgesia” criterion across all subjects in a dosing group, since this is frequently considered as indicative of clinically relevant efficacy.Citation2,Citation5 According to this analysis, 50%–90% of the topical mepivacaine-treated animals tested displayed clinically significant antinociception at any given time point. In contrast, 0%–10% of vehicle-treated animals showed antinociception at any given time point (). In this case, the antinociceptive effects of topical mepivacaine were strongest immediately at removal of the application gauze but continued for at least 5 minutes for all mepivacaine concentrations except for the lowest (2 mM).
Topical mepivacaine treatment significantly increased withdrawal latencies as assessed by the heat hyperalgesia test (; overall F [df 5,4] =7.4, P<0.001). Similar to responses of decreased withdrawal thresholds to noxious pressure, withdrawal response latencies to noxious heat were decreased 2 weeks following sciatic nerve exposure to gp120, indicative of thermal hyperalgesia (pre-gp120 vs predrug responses). In animals that received topical mepivacaine, the most robust antinociceptive response was observed 5 minutes following gauze removal (P<0.001 for the 8, 16, and 32 mM concentrations and P<0.05 for the 4 mM concentration, compared with vehicle). The highest concentration (32 mM) showed antinociceptive effects beginning immediately following pad removal (P<0.01 compared with vehicle). As observed for mechanical hyperalgesia, antinociceptive effects of topical mepivacaine dissipated By ~10 minutes following removal of the gauze. In contrast, vehicle application to the hind paw did not affect thermal hyperalgesia at any given time point.
The percent change from predrug baseline following treatment is shown in . While all concentrations of mepivacaine produced positive increases in withdrawal latencies, statistically significant differences between treatment groups were not found (P>0.05 compared with vehicle). None of the mepivacaine concentrations showed a >50% change from baseline. (By contrast, in the paw pressure test, neuropathic rats treated with either 16 or 32 mM of mepivacaine showed >50% changes from baseline [].)
When the percent of animals reaching 33% or better “analgesia” was analyzed, 20%–60% of animals that received mepivacaine concentration in the 4–32 mM concentration range were found to satisfy this 33% “analgesia” criterion immediately following removal of the gauze pad (). However, 5 minutes after removal of the gauze pad, 50%–70% of the rats treated with 4–32 mM mepivacaine demonstrated analgesia.
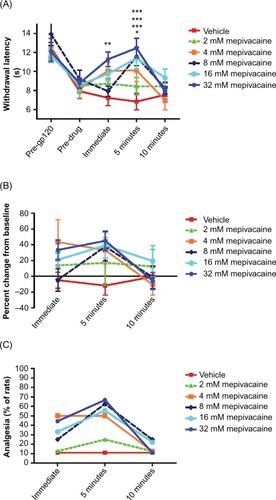
Effects of topical lidocaine on gp120-induced neuropathic hyperalgesia
In neuropathic rats only modest and transient antinociceptive effects of lidocaine on pressure hyperalgesia were observed (P<0.05 for 16 and 32 mM lidocaine compared with vehicle, immediately following gauze pad removal) (). When calculated as a percent change from baseline, no significant differences between lidocaine treatment and vehicle were observed (). In addition, only 15%–40% animals reached the 33% analgesia criterion following topical lidocaine treatment in the 4–32 mM range ().
Figure 3 Effect of topically applied lidocaine on mechanical hyperalgesia in rats with gp120-induced neuropathic pain.
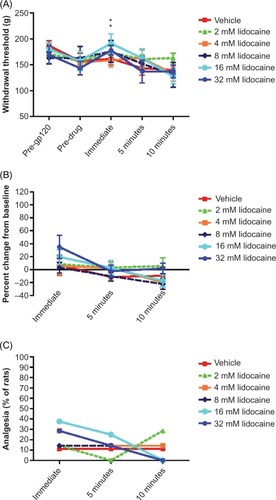
Topical lidocaine appeared more effective against thermal hyperalgesia, with 8 and 32 mM concentrations producing significantly increased thermal withdrawal latencies immediately following gauze removal (P<0.01 and 0.05, respectively, for 32 and 8 mM, compared with vehicle, ). This is also suggested by analyzing percent change from baseline (), with some treatments resulting in 70%–80% increases in thermal response latencies from baseline, although these were not statistically significant from vehicle. In addition, 30%–70% of animals reached the 33% analgesia criterion (). Topical lidocaine in this concentration range appeared to sustain antinociceptive effects on thermal hyperalgesia for up to 10 minutes following gauze pad removal ().
Figure 4 Effect of topically applied lidocaine on thermal hyperalgesia in rats with gp120-induced neuropathic pain.
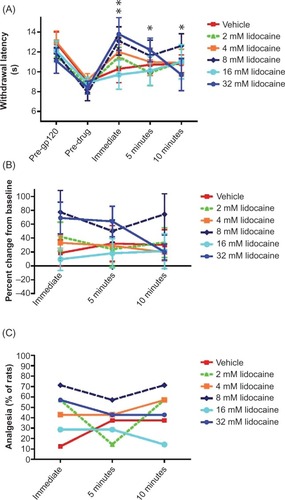
Effects of topical anesthetics on acute nociception in mice
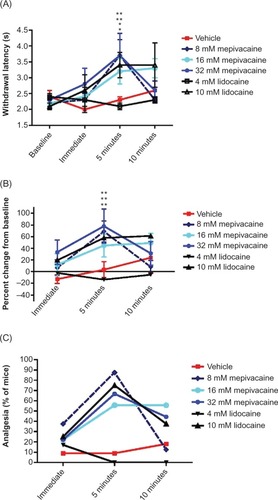
Peak antinociceptive effects of all local anesthetic concentrations except 4 mM lidocaine (P<0.01 for 32 and 8 mM mepivacaine and P<0.05 for 16 mM mepivacaine and 10 mM lidocaine compared with vehicle) were observed 5 minutes following removal of the tail from the anesthetic solution (). Similarly, significant efficacy of these treatments was apparent when the increases in tail withdrawal latencies were converted to a percent change from baseline (; P<0.01 at 5 minutes posttreatment for 32 mM mepivacaine, 8 mM mepivacaine, and 10 mM lidocaine, compared with vehicle). All concentrations of local anesthetics, except 4 mM lidocaine, produced 50%–90% antinociception as assessed by the 33% analgesia criterion 5 minutes after removal from local anesthetic solution ().
Figure 5 Effects of topically applied mepivacaine and lidocaine on acute nociception in the mouse tail flick assay.
Discussion
The current study was designed to assess potential development of the local anesthetic, mepivacaine, as a topical treatment approach for reducing HIV-related painful peripheral neuropathy. While a clinical formulation for extended or intermittent treatment using, for example, a patch or gel can be envisioned for future development, as a necessary first step, this study evaluated the transient acute antinociceptive effects of short-term topical application in an animal model of HIV-induced painful sensory neuropathy. Topical application of mepivacaine to the hind paw significantly alleviated both mechanical and thermal hyperalgesia in the current rat model. By contrast, the topical application of the more traditionally used local anesthetic lidocaine was effective in reducing heat hyperalgesia but only marginally effective in reducing pressure hyperalgesia in this neuropathic pain model. Topical mepivacaine and lidocaine produced comparable effects in response to noxious heat in non-injured animals (the mouse tail flick test). The current data suggest that the topical application of the local anesthetic mepivacaine could have improved effectiveness in reducing painful symptoms of HIV-induced neuropathic pain.
HIV distal sensory polyneuropathies are attributable to both the disease itself and antiretroviral treatments which exacerbate neurotoxicity.Citation31 As combination antiretroviral therapy has markedly improved survival in HIV patients and reduced some neurotoxic complications of the treatments, the prevalence of HIV sensory neuropathy has increased with increasing survival rates, and remains high globally, estimated from 20% to over 50%, with nearly half of patients experiencing pain rated as “severe”.Citation2,Citation5,Citation32 Symptomatic control of HIV-associated neuropathic pain is difficult to achieve using conventional analgesic therapies and further complicated by concerns with potential substance abuse disorders in this patient population.Citation2,Citation3 Although several therapies have been tried for its treatment, to date, no drugs have been specifically approved for painful HIV-associated neuropathy. Small clinical trials have suggested beneficial effects compared to placebo for smoked cannabis, recombinant nerve growth factor, and topical capsaicin.Citation32–Citation39 These treatments however are not without side effects such as the psychomimetic effects of cannabis, myalgia that occurs following nerve growth factor treatment, and the intense, acute pain following capsaicin application. Pharmacotherapies that are used in the management of other painful peripheral neuropathies, including the anticonvulsants lamotrigine, gabapentin, and pregabalin, and the antidepressants amitriptyline, mexiletine, and memantine, have not demonstrated substantial analgesic effects on HIV-induced neuropathic pain.Citation5,Citation7–Citation10
Spontaneous peripheral nerve activity following injury or disease has been suggested to have a key role in maintaining the neuropathic pain state.Citation40 The gp120 model for HIV-associated neuropathic pain also appears to have an inflammatory pain component.Citation41 An inflammatory-like response was observed following application of gp120 to the sciatic nerve, with axonal swelling and endoneural vasodilation.Citation17 The inflammatory cytokine tumor necrosis factor was found within and surrounding the nerve, suggesting the presence of infiltrating immune cells. Application of tumor necrosis factor to the sciatic nerve leads to ectopic activity in rat sciatic nerve and mechanical and thermal hyperalgesia.Citation42 Thus, peripheral nerve spontaneous activity evoked by gp120 is one mechanism by which HIV infection could lead to neuropathic pain.
Local anesthetics are thought to attenuate spontaneous activity and ectopic discharges due to upregulated sodium channels in injured peripheral nerves, thereby leading to pain relief.Citation28,Citation43 The application of lidocaine to an injured nerve can suppress ectopic activity and neuropathic pain.Citation44 Topical local anesthetics, particularly lidocaine, have been clinically evaluated in the treatment of peripheral neuropathic pain states.Citation45–Citation48 Several formulations of topical lidocaine are available or in development including a lidocaine 5% patch (Lidoderm® 5%), 5% plaster, cream mixtures (eg, EMLA), ointments, gels, and sprays. The Lidoderm® 5% patch is one of three US Food and Drug Administration-approved treatments for the management of postherpetic neuralgia (along with gabapentin and pregabalin). Nevertheless, the lidocaine patch provides only modest pain relief in patients with postherpetic neuralgia,Citation46 and a recent review of randomized controlled studies concludes that there is no evidence to support the use of topical lidocaine for the treatment of neuropathic pain.Citation29 In the only available placebo-controlled randomized clinical trial of topical lidocaine for HIV-associated neuropathic pain, the effect of treatment did not differ significantly from placebo.Citation13 Although the lidocaine patch has not demonstrated efficacy in well-controlled clinical trials in painful HIV-associated neuropathy, in the absence of other approved therapies, it continues to be used for this purpose.
A potential value of mepivacaine for neuropathic pain treatment is its improved bioavailability compared with lidocaine. This is supported by the current findings showing a broader range of behavioral effects on pain symptoms. Mepivacaine has an intrinsic vasoconstrictor effect which could reduce the rate at which the drug is cleared away from peripheral (skin) sites of pain generation. In addition, mepivacaine may have improved neurological safety, allowing higher doses to be applied to achieve improved analgesia. Among a series of local anesthetics, mepivacaine had the lowest neurotoxic effects on primary cultured neurons (lidocaine had the highest).Citation15 In the current study, the topical application of mepivacaine attenuated both hind paw mechanical and thermal hyperalgesia in rats with gp120-induced peripheral neuropathy. The topically applied local anesthetics in this model likely suppressed pain by a transient suppression of spontaneous activity of peripheral nerves. In contrast to mepivacaine, topical lidocaine suppressed heat but not mechanical hyperalgesia. It is possible that local anesthetics do not suppress mechanical hyperalgesia as well as thermal hyperalgesia, and that a higher concentration of lidocaine could also have had an antinociceptive effect on mechanical hyperalgesia. However, neurotoxicity is likely at high concentrations of lidocaine. Lidocaine and mepivacaine were equipotent in modestly reducing responsiveness to heat in normal skin, as assessed by the mouse tail flick test, similar to the effects reported by others.Citation30 Thus, the improved analgesic effects of topical mepivacaine, to expand coverage to include suppression of mechanical as well as heat hyperalgesia, may be indicative of distinct mechanisms such as inhibition of a wide range of nociceptor subpopulations.
There is a need for an alternative, topically applied local anesthetic for the treatment of HIV-induced painful peripheral neuropathy. Although the gp120 model produces a mononeuropathy in contrast to the distal symmetrical polyneuropathy more characteristic of HIV-associated neuropathic pain, topical treatment approaches using other agents (eg, capsaicinCitation34–Citation37) have been explored for this condition, and a potential value of topical application is the ability to apply it locally (or bilaterally) on an as-needed basis. Thus, topical anesthetics can improve patient compliance, and dosing is not a significant safety or off-target issue compared with orally or parenterally administered medications. Mepivacaine in the current study demonstrated good antinociception in a rat model of gp120-induced peripheral neuropathic pain, whereas an equivalent concentration of lidocaine that demonstrated comparable antinociception in the tail flick test was not effective on neuropathic mechanical hypersensitivity. Thus, mepivacaine could be a useful treatment in managing HIV-induced painful peripheral neuropathy.
It should be noted that, like most experimental animal models relying on assessment of evoked responses to cutaneous stimuli, the more common complaints of patients with HIV-related neuropathic pain, such as spontaneous burning and stabbing sensations, can only be inferred using these outcome measures. HIV neuropathic pain patients report a number of sensory disturbances including sensitivity to temperature and touch.Citation1 Future preclinical efforts focused on the development of clinical therapies should include newly emerging models to capture non-evoked spontaneous pain outcomes. In addition, with the development of transgenic and HIV humanized mouse models, future studies using these models may further strengthen the search for effective therapeutics in the treatment of HIV-induced neuropathic pain.
Although significant analgesic efficacy was achieved by topical mepivacaine in this initial exploration of HIV-associated painful sensory neuropathy, a limitation in its potential therapeutic usefulness is the transient and rapidly dissipating antinociceptive effect. The development of improved transdermal delivery systems should overcome this limitation and prolong analgesic effects of topical local anesthetics. Gel formulations showing enhanced local anesthetic action in tail flick test using various agents (mepivacaine, prilocaine, bupivacaine) have been reported.Citation49,Citation50 Thus, future directions will include development of mepivacaine gel formulations for evaluation as a treatment approach in managing HIV-associated neuropathic pain. Based on the promising outcomes in the current study, clinical formulations of mepivacaine gels with increased permeation over time compared with 5% lidocaine patch are being developed by the study sponsor. These advances should markedly improve the efficacy and safety in the management of neuropathic pain syndromes, particularly HIV-induced painful peripheral neuropathy.
Acknowledgments
This study was supported by Relmada Therapeutics, Inc. The authors are highly grateful to Ms Ludmilla Rusakova for her expert technical assistance.
Disclosure
Jacqueline Sagen served as a consultant to Relmada Therapeutics. The authors report no other conflicts of interest in this work.
References
- FreemanRBaronRBouhassiaraDCabreraJEmirBSensory profiles of patients with neuropathic pain based on neuropathic pain symptoms and signsPain201415536737624472518
- PhillipsTJCCherryCLCoxSMarshallSJRiceASCPharmacological treatment of painful HIV-associated sensory neuropathy: a systematic review and meta-analysis of randomised controlled trialsPLoS ONE20105e1443321203440
- Robinson-PappJMorgelloSVaidaFAssociation of self-reported painful symptoms with clinical and neurophysiological signs in HIV-associated sensory neuropathyPain201015173273620851521
- RobertsonKKumwendaJSupparatpinyoKA multinational study of neurological performance in antiretroviral therapy-naive HIV-1-infected persons in diverse resource-constrained settingsJ Neurovirol20111743844721786076
- SchützSGRobinson-PappJHIV-related neuropathy: current perspectivesHIV/AIDS (Auckl)20135243251
- VermaSEstanislaoLSimpsonDHIV-associated neuropathic pain: epidemiology, pathophysiology and managementCNS Drugs20051932533415813646
- KemperCAKentGBurtonSDeresinskiSCMexiletine for HIV-infected patients with painful peripheral neuropathy: a double-blind, placebo-controlled, crossover treatment trialJ Acquir Immune Defic Syndr Hum Retrovirol1998193673729833745
- KieburtzKSimpsonDYiannoutsosCA randomized trial of amitriptyline and mexiletine for painful neuropathy in HIV infection. AIDS Clinical Trial Group 242 Protocol TeamNeurology199851168216889855523
- ShlayJCChalonerKMaxMBAcupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: a randomized control trialJAMA1998280159015959820261
- SimpsonDMDorfmanDOlneyRKPeptide T in the treatment of painful distal neuropathy associated with AIDS: results of a placebo-controlled trialNeurology199647125412598909439
- AttalNCruccuGBaronREuropean Federation of Neurological SocietiesEFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revisionEur J Neurol2010171113e8820402746
- DworkinRHO’ConnorABBackonjaMPharmacologic management of neuropathic pain: evidence-based recommendationsPain200713223725117920770
- EstanislaoLCarterKMcArthurJOlneyRSimpson D; GroupL-HNA randomized controlled trial of 5% lidocaine gel for HIV-associated distal symmetric polyneuropathyJ Acquir Immune Defic Syndr2004371584158615577414
- BrockmannWGMepivacaine: a closer look at its properties and current utilityGen Dent201462707525369391
- RadwanIASaitoSGotoFThe neurotoxicity of local anesthetics on growing neurons: a comparative study of lidocaine, bupivacaine, mepivacaine, and ropivacaineAnesth Analg20029431932411812691
- LeeHIParkYSChoTGParkSWKwonJTKimYBTransient adverse neurologic effects of spinal pain blocksJ Korean Neurosurg Soc20125222823323115666
- HerzbergUSagenJPeripheral nerve exposure to HIV viral envelope protein gp120 induces neuropathic pain and spinal gliosisJ Neuroimmunol2001116293911311327
- WallaceVCBlackbeardJPhebyTPharmacological, behavioural and mechanistic analysis of HIV-1 gp120 induced painful neuropathyPain2007133476317433546
- ApostolskiSMcAlarneyTHaysAPLatovNComplement dependent cytotoxicity of sensory ganglion neurons mediated by the gp120 glycoprotein of HIV-1Immunol Invest19942347528144198
- MilliganEDMehmertKKHindeJLThermal hyperalgesia and mechanical allodynia produced by intrathecal administration of the human immunodeficiency virus-1 (HIV-1) envelope glycoprotein, gp120Brain Res200086110511610751570
- OhSBTranPBGillardSEHurleyRWHammondDLMillerRJChemokines and glycoprotein120 produce pain hypersensitivity by directly exciting primary nociceptive neuronsJ Neurosci2001215027503511438578
- KeswaniSCPolleyMPardoCAGriffinJWMcArthurJCHokeASchwann cell chemokine receptors mediate HIV-1 gp120 toxicity to sensory neuronsAnn Neurol20035428729612953261
- JonesGZhuYSilvaCPeripheral nerve-derived HIV-1 is predominately CCR5-dependent and causes neuronal degeneration and neuroinflammationVirology200533417819315780868
- MelliGKeswaniSCFischerAChenWHokeASpatially distinct and functionally independent mechanisms of axonal degeneration in a model of HIV-associated sensory neuropathyBrain20061291330133816537566
- BabulNHamaABaslerABaumJSagenJResponse to the local anesthetic TQ-1019 in the GP120 model of painful HIV neuropathy12th World Congress on PainAug, 17–24, 2012Glasgow, Scotland Abstract PW350
- RusakovaLBabulNCastellanosDWeinrichJBaumDSagenJAntinociceptive response of the local anesthetic TQ-1019 in the radiant heat tail flick assay12th World Congress on PainAug, 17–24, 2012Glasgow, Scotland Abstract PW353
- HargreavesKDubnerRBrownFFloresCJorisJA new and sensitive method for measuring thermal nociception in cutaneous hyperalgesiaPain19883277883340425
- AnitescuMBenzonHTArgoffCEAdvances in topical analgesicsCurr Opin Anesthesiol201326555561
- WiffenDSMooreRAQuinlanJTopical lidocaine for neuropathic pain in adultsCochrane Database Syst Rev20147CD01095825058164
- KolesnikovYAChereshnevIPasternakGWAnalgesic synergy between topical lidocaine and topical opioidsJ Pharmacol Exp Ther200029554655111046087
- GhoshRKGhoshSMChawlaSRecent advances in antiretroviral drugsExpert Opin Pharmacother201112314620698725
- EllisRJToperoffWVaidaFSmoked medicinal cannabis for neuropathic pain in HIV: a randomized, crossover clinical trialNeuropsychopharmacology20093467268018688212
- AbramsDIJayCAShadeSBCannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trialNeurology20076851552117296917
- PaiceJAFerransCELashleyFRVizgirdaVPitrakDTopical capsaicin in the management of HIV-associated peripheral neuropathyJ Pain Symptom Manage200019455210687326
- SimpsonDMBrownSTobiasJNGX-4010 C107 Study GroupControlled trial of high-concentration capsaicin patch for treatment of painful HIV neuropathyNeurology2008702305231318541884
- SimpsonDMEstanislaoLBrownSHSampsonJAn open-label pilot study of high-concentration capsaicin patch in painful HIV neuropathyJ Pain Symptom Manage20083529930617959343
- SimpsonDMBrownSTobiasJKVanhoveGFNGX-4010, a capsaicin 8% dermal patch, for the treatment of painful HIV-associated distal sensory polyneuropathyClin J Pain20143013414223446088
- SimpsonDMMcArthurJCOlneyRLamotrigine HIV Neuropathy Study TeamLamotrigine for HIV-associated painful sensory neuropathies: a placebo-controlled trialNeurology2003601508151412743240
- SimpsonDMOlneyRMcArthurJCKhanAGodboldJEbel-FrommerKA placebo-controlled trial of lamotrigine for painful HIV-associated neuropathyNeurology2000542115211910851374
- BaronRPeripheral neuropathic pain: from mechanisms to symptomsClin J Pain200016S12S2010870735
- NasirinezhadFJergovaSPearsonJPSagenJAttenuation of persistent pain-related behavior by fatty acid amide hydrolase (FAAH) inhibitors in a rat mode of HIV sensory neuropathyNeuropharmacology20159510010925486617
- SorkinLSXiaoWHWagnerRMyersRRTumour necrosis factor-alpha indices ectopic activity in nociceptive primary afferent fibersNeuroscience1997812552629300418
- FloresMPCastroAPNascimentoJSTopical analgesicsRev Bras Anestesiol20126224425422440379
- KirillovaITeilbanAGorodetskayaNEffect of local and intravenous lidocaine on ongoing activity in injured afferent nerve fibersPain20111521562157121474243
- DeversAGalerBSTopical lidocaine patch relieves a variety of neuropathic pain conditions: an open-label studyClin J Pain20001620520811014393
- MeierTWasnerGFaustMEfficacy of lidocaine patch 5% in the treatment of focal peripheral neuropathic pain syndromes: a randomized, double-blind, placebo-controlled studyPain20031615115814581122
- MadsenCSJohnsenBJFulglsang-FrederiksenAJensenTSFinnerupNBDifferential effects of a 5% lidocaine medicated patch in peripheral nerve injuryMuscle Nerve20134826527123653369
- PeppinJFAlbrechtPJArgoffCSkin matters: a review of topical treatments for chronic pain. Part two: treatments and applicationsPain Ther20154335025630651
- ChoCWChoiJSShinSCEnhanced local anesthetic action of mepivacaine from the bioadhesive gelsPak J Pharm Sci201124879321190925
- KangCShinSCDevelopment of prilocaine gels for enhanced local anesthetic actionArch Pharm Res2012351197120422864742
