Abstract
Chronic pain following inguinal hernia repair is a common problem and feared complication. Up to 16% of people experience chronic pain following the repair of a groin hernia. The aim of this review was to provide an overview of treatment strategies for patients with chronic pain following inguinal hernia repair based on best practice guidelines and current clinical routines. The optimal management of chronic pain following inguinal hernia surgery should begin with a thorough clinical examination to rule out other causes of chronic pain and to rule out a recurrence. A scaled approach to treatment is recommended. Initially, watchful waiting can be tried if it can be tolerated by the patient and then systemic painkillers, escalating to blocks, and surgery as the final option. Surgery should include mesh removal and triple neurectomy following anterior approaches or mesh and tack removal following a posterior approach. The diagnosis and treatment strategies should be performed by or discussed with experts in the field.
Introduction
Postoperative chronic pain is a special entity within the domain of chronic pain. Chronic postoperative pain occurs following numerous kinds of surgery, from amputations to thoracotomies to inguinal hernia surgery. The chronic pain after inguinal hernia repair has been extensively studied; however, the management is still difficult. Around the globe, millions of groin hernia repairs are conducted annuallyCitation1 and 8%–16% of these patients experience chronic pain to a degree that impairs their daily lives 6 months postoperatively.Citation2,Citation3 A few percent of these patients experience disabling pain, and due to the large number of groin hernia repairs, the number of patients with disabling pain and discomfort is an important clinical problem.Citation4 Depending on the degree of pain and the impact on daily activities, an evidence-based treatment option should be offered. A problem with some of the current evidence, based on research in chronic pain after groin hernia repair, is the use of different assessment methods and different lengths of follow-up. Surgeons, scientists, and pain specialists use different assessment methods, ie, researchers use different questionnaires in order to assess chronic pain in research projects, and this limits comparability.
The aim of this review is to provide an overview of treatment strategies for patients with chronic pain following inguinal hernia repair based on best practice guidelines and clinical routines.
Groin hernia repairs and pain
For the initial repair of groin hernia, recommendations include use of a mesh.Citation5,Citation6 Dedicated centers have shown good results with nonmesh-based techniques,Citation7 but the overall recommendation for routine care includes use of a mesh. Globally, the most used types of mesh-based repairs are the Lichtenstein open repair and one of the variations of the laparoscopic repair.Citation8 The Lichtenstein repair is known to cause discomfort and disabling pain in some patients.Citation3,Citation9 The laparoscopic techniques seem to lower the risk of chronic pain but still cause chronic pain in some people.Citation10
Several potential causes of pain have been investigated for these repair methods. The role of the meshes has been investigated, and the weight of the mesh (g/m2) has been hypothesized to influence the risk of pain. Heavyweight meshes have been compared with lightweight meshes but demonstrated no advantages for laparoscopic repairs.Citation11 However, the lightweight meshes seem to lower the risk of chronic pain following the Lichtenstein repair technique.Citation12 Besides meshes, the choice of fixation method for the mesh can influence the risk of pain. Glue has been demonstrated to reduce the risk of chronic pain in open mesh-based repairs,Citation13,Citation14 but the advantage of glue could not be found in a recent nationwide study of the laparoscopic repair.Citation10
When operating inguinal hernias, there is a risk of causing injuries that will cause pain. If there is injury to tissue, it can cause nociceptive pain, and damage to nerves can cause neuropathic pain. In order to prevent or minimize the risks of pain, surgeons always take care when performing repairs and handle tissue gently. Peroperatively, the role of identification and/or resection of nerves has been investigated in order to minimize the occurrence of chronic pain. The nerves can be in the way when placing the mesh, can be caught or injured during fixation, and can be injured by accident or by dissection in the operative field. It is recommended, in the recently published World Guidelines for inguinal hernia repair, to identify the nerves but not to do a planned resection; however, if the nerves are in the way when placing the mesh, a “pragmatic resection” is recommended.Citation5
Definitions and types of pain
Chronic (postoperative) pain has been defined as pain lasting at least 2–3 months (after surgery), but modifications are proposed to this timeframe.Citation15,Citation16 A group of experts in hernia surgery and chronic pain has suggested modifying the definition for chronic pain after hernia repair as pain lasting at least 6 months after operation.Citation4 The reason for this extended period of time is because the inflammation around the mesh is still ongoing after 3 months, and there is a chance that some patients will improve substantially from 3 to 6 months postoperatively.
Pathogenesis
The cause of chronic pain following inguinal hernia surgery can be multifactorial and often it is not possible to point to a distinct reason for the pain in a specific patient. Pain can be caused by perioperative injury to nerves or nerves that are being stuck and damaged by sutures or perforated by fixation devices such as tacks. Nerves can also be trapped in a “meshoma”, which is when the mesh has shrunk with folding and wrinkling making a ball of mesh material, the so-called meshoma.Citation17 It is reasonable to imagine that some shrinking of the mesh, which is seen in most patients, can also entrap a nerve and thereby cause chronic pain. Pain can also be caused by the inflammation process around the mesh. It is sometimes not possible to diagnose the specific cause of pain in the individual patient. Furthermore, the distinction between neuropathic pain (pain caused by damage to nerves) and nociceptive pain (pain caused by the release of substances due to tissue damage or damage to organs) can be difficult. Some patients might have groin pain from other sources than their hernia repair such as hip pathology or pubalgia. Furthermore, some patients might have received a hernia repair due to these other pathologies, resulting in symptoms similar to a hernia.
When investigating the patient with chronic postoperative pain, it is important to look for a possible recurrence since the recurrence could be the reason for pain or discomfort. If a recurrence is present, it is indicated to repair the recurrence and hopefully that will relieve the complaints and discomfort of the patient. However, care should be taken when repairing recurrent hernias if there is also signs of neuropathic pain, since the patient might at the same time have damaged nerves. If there are damaged nerves, repair of the recurrence might not solve the problem for, and it is therefore recommended to also consider a neurectomy at the same time.
Preoperative and early postoperative pain
A patient’s preoperative level of pain affects the risk of developing chronic pain following surgery. A large questionnaire study found that preoperative pain increased the risk of postoperative pain by a factor 1.5.Citation10 However, preoperative pain is not a contraindication for surgery, but patients should be informed of the increased risk. Not only does the preoperative pain influence the risk of postoperative pain, but also there are strong indications that early high-intensity pain after surgery is a risk factor for developing chronic pain.Citation15 Therefore, a standardized and effective postoperative analgesic regime could be recommended following inguinal hernia repair.
Assessment of pain and severity
When assessing the degree of pain in a research context, it is important to use validated questionnaires and questionnaires that also evaluate the impact on activities of daily living, such as driving, walking, and standing.Citation18–Citation20
For day-to-day clinical work and assessment of patients, it is time-consuming to use these questionnaires and a thorough history as well as clinical examination should be used. It is important to have experience with chronic pain after inguinal hernia surgery when assessing these patients. Some surgeons use a surgical marker to “map” the pain on the patient, with pluses indicating pain, zeros indicating no pain, and minuses meaning numb area.Citation21 The groin, abdomen, thigh, and genitals should be investigated in order to locate the extent of the painful area. Photos of this “map” can be taken and then compared with the same investigation after treatment or shared with colleagues and experts in order to plan the best management strategy for the patient.Citation22 The pain map can provide an indication of which nerves might be involved in the chronic pain pathogenesis. “Pain maps” are sometimes shared in a closed Facebook group called International Hernia Collaboration Group, which now has more than 3,000 members. Here, surgeons discuss clinical cases and the best strategy to treat patients with, eg, chronic postoperative pain.
A more formal testing can be done with the quantitative sensory testing (QST). QST uses a range of methods to investigate pain by pressure, pain, cold, pin prick, etc. QST is time-consuming and not applicable for most routine clinical settings.Citation2
Interventions and management of chronic pain
Authors of a recent review aimed to characterize management and treatment strategies for chronic postoperative pain; however, the authors of the review concluded that there was a lack of evidence, making it impossible to draw firm conclusions regarding effectiveness or harm.Citation23 A problem might be to investigate all interventions to treat all postoperative chronic pain conditions, and it is likely that each of the different procedures resulting in chronic pain needs to have their own specific treatment and diagnostic algorithm.
For chronic pain following inguinal hernia surgery, a range of interventions can be used to treat or manage the chronic pain. Interventions include watchful waiting, pharmacological treatments, local anesthetic blocks, sensory stimulation or ablation of nerves, and surgery (mesh removal, reoperation for recurrence, and neurectomy).Citation24
Watchful waiting
First-line management of chronic pain following inguinal hernia repair is to examine the patient and explain the condition. Since pain is declining with time after surgery, a watchful strategy can be tried in the beginning.Citation25 However, a lifestyle change to sedentary activities is not recommended,Citation26 and chronic pain can severely affect quality of life.Citation27 Basic analgesics can be used in the period of watchful waiting.Citation25 If there are no improvements in the condition after a few months, then systematic pharmacological interventions should be tried, preferably in collaboration with pain specialists. If the pain is bearable, it is import to inform the patient that pain will, for many patients, diminish with time.Citation28
Pharmacological interventions
Systematic pharmacological analgesics are used in the postoperative phase to reduce the acute pain. For chronic pain at the later stages, after 3–6 months, depending on definition, pharmacological interventions can be tried as a first-line treatment, using nonsteroidal anti-inflammatory drugs, gabapentinoids, tricyclic antidepressants, selective serotonin reuptake inhibitor/serotonin–norepinephrine reuptake inhibitor, and/or conventional analgesics.Citation29 Topical administration of analgesics has also been considered. Patches with lidocaine and capsaicin for local application have been tested in randomized studies. Unfortunately, the studies have not been able to demonstrate a benefit, and these patches are therefore not recommended for the treatment of chronic groin pain.Citation30,Citation31
Prevention of chronic pain with the use of preoperatively administered pharmacological interventions has been investigated,Citation32 the hypothesis being that it could be possible to diminish postoperative pain and prevent central sensitization.Citation29 A Cochrane review including 40 randomized clinical trials concluded, cautiously, that preoperatively administered ketamine may reduce the risk of chronic pain but that there is no evidence for recommending gabapentinoids, pregabalin, or other drugs for prevention of chronic postoperative pain.Citation33 At this point, evidence is not strong enough to systematically recommend preoperative analgesics for the prevention of chronic pain, but future studies might prove it beneficial, maybe especially in patients at high risk of developing chronic pain.
Injections
Injections with local anesthetics have been tested and are used for both the relief of pain and the diagnostic purposes in order to identify which nerves are involved in neuropathic pain. Fixed point injections do not have an effect on chronic postoperative pain compared with placebo treatment.Citation34 In a study, it was tested to use injections at tender points, meaning that the point of injection was tailored to each patient depending on where in the groin the pain was.Citation35 The study demonstrated some effect indicating that the peripheral nerves were involved in the chronic pain, but unfortunately, the effect did not last.Citation35 A recent study on injections with a mix of lidocaine, corticosteroids, and hyaluronic acid has investigated the use of up to three repeated injections over 6 weeks in order to treat chronic pain compared with surgical neurectomy. The study demonstrated a 22% success rate, which was lower than the 71% success rate for the neurectomy group.Citation36 In the study, 4% minor complications were found for injections. The injections were safe and minimally invasive, and the authors concluded that it should be considered to use injections before explorative surgery with neurectomy.Citation36 Injections with alcohol can be used for neurolysis.
Radiofrequency treatment
Radiofrequency can be used to block the nerve by moderate heating (40°C) that does not result in thermocoagulation or can be used at a higher intensity, thereby heating the nerve resulting in ablation of the tissue. Radiofrequency can be done either at the peripheral level or at the vertebral level. A study investigated pulsed radiofrequency at the dorsal root ganglia with heating of the nerve to 40–42°C, demonstrating pain relief for up to 20 weeks.Citation37 Another study investigated radiofrequency at a higher intensity, where the nerves were heated to 70–90°C, thereby causing thermocoagulation of the nerve, and demonstrated pain relief lasting up to 12 months.Citation38
Another option is to implant a device that stimulates the nerves (spinal cord stimulation),Citation39 and this has been demonstrated to provide some relief up to 12 months.Citation40 However, the current clinical use of radiofrequency or spinal implants is limited.Citation41
Surgery
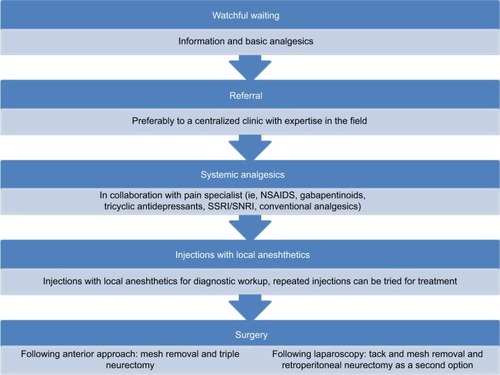
If other treatments (watchful waiting, systemic analgesics, and injections) have been tried and failed, it should be considered to operate the patients for their pain (). Different surgical approaches can be used to remove the mesh, perform a neurectomy, or a combination of both. Neurectomy can be performed via an anterior open approach or via a posterior laparoscopic technique. Surgical strategy will be determined by the initial technique for inguinal hernia repair. Following anterior approaches, a repeated anterior approach with neurectomy and mesh removal is recommended. Following posterior approaches (ie, laparoscopy), a posterior approach is recommended with exploration of the field and removal of tacks and mesh.
Figure 1 Proposed treatment options for chronic pain following inguinal hernia repair.
Abbreviations: NSAID; nonsteroidal anti-inflammatory drug; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin–norepinephrine reuptake inhibitor.
If it is thought that the mesh is causing the problem, and not a recurrence, a surgical removal of the mesh should be considered.Citation25 The pain can be due to damage to the nerves caused by the mesh, but simply removal of the mesh might not reverse the neuropathic pain. Peroperatively, the nerves might seem normal without macroscopically visible damage, but there can still be ultrastructural damages to the nerves that will cause pain and even the removal of the mesh might not reverse the damage and the patient might still have pain. It is therefore recommended to always conduct a triple neurectomy since it is difficult if not impossible to diagnose which nerves are involved in the pain, and a subsequent surgical procedure in the scarred surgical field after mesh removal may be difficult. Thus, when performing mesh removal after a previous Lichtenstein repair, it is recommended to remove as much of the mesh as possible (preferably all mesh material) together with triple neurectomy anterior to the annulus, ie, outside of the abdominal cavity without dissection behind the transversalis fascia.
Surgical treatment of pain following a posterior approach such as laparoscopy can be divided in two methods. The first method is to remove tacks and mesh with a laparoscopic approach. The second method is a neurectomy that should be reserved for skilled hands.
The laparoscopic retroperitoneal triple neurectomy has been developed to avoid the scared field of the groin after open approaches and in order to conduct neurectomy proximal to the nerves following preperitoneal or intraperitoneal approaches.Citation42 In a highly selected group of patients (62 out of 567 with chronic pain after inguinal hernia repair), 95% of patients experienced decrease of their pain to “manageable levels” after laparoscopic retroperitoneal triple neurectomy.Citation42
Centralization
The treatment of patients with chronic pain following inguinal hernia surgery should be considered centralized. In Germany, dedicated hernia centers have been established.Citation43 The specialized management of the patients with this pain should be considered as an expert area. Centralized evaluation and treatment would also allow for proper data collection and high volume research. In Denmark, these patients are all referred to one clinic, which has resulted in good data collection and a uniform treatment of the patients.
Discussion
This review aimed to provide an overview of possible strategies for the treatment of chronic pain after inguinal hernia surgery. At the moment, there is not a single treatment or management strategy that will be appropriate for all patients. Experts and expert-based guidelines recommend to use a scaled intervention, meaning that the patient should start out with watchful waiting, especially in the first 6 months, and then, systemic pain killers and if that cannot relieve the pain, injections should be tried; surgical treatment should be considered as the final option. It is also recommended to always consult a surgeon or, preferably, a regional or a national center with the expertise in chronic pain following inguinal hernia surgery since causes and treatments vary from patient to patient and because one strategy might not fit all.
Several guidelines exist in this area; however, they are mostly based on expert opinions and personal experience and less on solid high-quality evidence.Citation5,Citation25 A regional, national, or maybe even international setup should be in place in order to deal with the most severe and complex cases. This allows for gathering of expertise and ensures that patients are uniformly treated and receive the best standard of care for this condition. An international collaboration could be beneficial in order to share knowledge and collect data for development of treatments. It is likely that the individual surgeon does not see their own patients with chronic pain if the patients go to a different surgeon or institution. Thus, just for reoperation for recurrence, up to 25% of patients go to a different hospital than for the primary repair.Citation44
In general, there is a high need for evidence regarding chronic postsurgical pain management,Citation23 not only for pain following inguinal hernia surgery but also for pain following many different kinds of surgery. The treatment of chronic postoperative pain is difficult, and a simple treatment that works well for all has not been found.Citation23 Therefore, individualized management is becoming more important, and the optimal management is what every surgeon or doctor treating these patients should aim for.
Conclusion
The optimal management of chronic pain following inguinal hernia surgery should begin with a thorough clinical examination to rule out other causes of chronic pain and to rule out a recurrence. If other causes of chronic groin pain have been excluded and the groin pain is caused by the inguinal hernia repair, a scaled approach is recommended. Initially, watchful waiting can be tried if it can be tolerated by the patient and then systemic pain killers, escalating to blocks, and surgery as the final option. Surgery should include mesh removal and triple neurectomy following anterior approaches or mesh and tack removal following a posterior approach. These procedures should be performed by experts in the field. There is a need for new developments and evidence-based guidelines, and this will require centralization of treatment in order to gather the necessary data to support future best practice guidelines.
Disclosure
The authors report no conflicts of interest in this work.
References
- KingsnorthATreating inguinal herniasBMJ20043287431596014715576
- AasvangEKGmaehleEHansenJBPredictive risk factors for persistent postherniotomy painAnesthesiology2010112495796920234307
- AndresenKBurcharthJFonnesSChronic pain after inguinal hernia repair with the ONSTEP versus the Lichtenstein technique, results of a double-blinded multicenter randomized clinical trialLangenbecks Arch Surg2017402221321827837273
- AlfieriSAmidPKCampanelliGInternational guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgeryHernia201115323924921365287
- The HerniaSurge GroupInternational Guidelines for Groin Hernia-ManagementHernia20182211165
- RosenbergJBisgaardTKehletHDanish Hernia DatabaseDanish Hernia Database recommendations for the management of inguinal and femoral hernia in adultsDan Med Bull2011582C424321299930
- ShouldiceEBThe shouldice repair for groin herniasSurg Clin North Am20038351163118714533909
- FitzgibbonsRJJrForseRAClinical practice. Groin hernias in adultsN Engl J Med2015372875676325693015
- BischoffJMAasvangEKKehletHWernerMUDoes nerve identification during open inguinal herniorrhaphy reduce the risk of nerve damage and persistent pain?Hernia201216557357722782363
- AndresenKFengerAQBurcharthJPommergaardHCRosenbergJMesh fixation methods and chronic pain after transabdominal preperitoneal (TAPP) inguinal hernia surgery: a comparison between fibrin sealant and tacksSurg Endosc201731104077408428233095
- BurgmansJPVoorbroodCESimmermacherRKLong-term results of a randomized double-blinded prospective trial of a lightweight (Ultrapro) versus a heavyweight mesh (Prolene) in laparoscopic total extraperitoneal inguinal hernia repair (TULP-trial)Ann Surg2016263586286626779980
- SajidMSLeaverCBaigMKSainsPSystematic review and meta-analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repairBr J Surg20129912937
- ColvinHSRaoACavaliMCampanelliGAminAIGlue versus suture fixation of mesh during open repair of inguinal hernias: a systematic review and meta-analysisWorld J Surg201337102282229223868471
- CampanelliGPascualMHHoeferlinARandomized, controlled, blinded trial of Tisseel/Tissucol for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: results of the TIMELI trialAnn Surg2012255465065722395092
- WernerMUKongsgaardUEI. Defining persistent post-surgical pain: is an update required?Br J Anaesth201411311424554546
- SchugSAPogatzki-ZahnMChronic pain after surgery or injuryPain Clin Updates201114115
- AmidPKRadiologic images of meshoma a new phenomenon causing chronic pain after prosthetic repair of abdominal wall herniasJAMA Surg20041391212971298
- McCarthyMJJonassonOChangCHAssessment of patient functional status after surgeryJ Am Coll Surg2005201217117816038812
- FrannebyUGunnarssonUAnderssonMValidation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repairBr J Surg200895448849318161900
- HenifordBTWaltersALLincourtAENovitskyYWHopeWWKercherKWComparison of generic versus specific quality-of-life scales for mesh hernia repairsJ Am Coll Surg2008206463864418387468
- ChenDCHiattJRAmidPKOperative management of refractory neuropathic inguinodynia by a laparoscopic retroperitoneal approachJAMA Surg20131481096296723903521
- ÁlvarezRDermatome mapping: preoperative and postoperative assessmentJacobBChenDRamshawBTowfighSThe SAGES Manual of Groin PainChamSpringer2016277292
- WyldeVDennisJBeswickADSystematic review of management of chronic pain after surgeryBr J Surg2017104101293130628681962
- WernerMUManagement of persistent postsurgical inguinal painLangenbecks Arch Surg2014399555956924849039
- LangeJFKaufmannRWijsmullerARAn international consensus algorithm for management of chronic postoperative inguinal painHernia2015191334325138620
- HakeemAShanmugamVCurrent trends in the diagnosis and management of post-herniorraphy chronic groin painWorld J Gastrointest Surg201136738121765970
- CourtneyCADuffyKSerpellMGO’DwyerPJOutcome of patients with severe chronic pain following repair of groin herniaBr J Surg200289101310131412296903
- ObergSAndresenKRosenbergJGradual decline in prevalence of chronic pain after laparoscopic groin hernia repair: a nationwide cross-sectional questionnaire studyIn press2018
- BjurstromMFNicolALAmidPKChenDCPain control following inguinal herniorrhaphy: current perspectivesJ Pain Res2014727729024920934
- BischoffJMRingstedTKPetersenMSommerCUceylerNWernerMUA capsaicin (8%) patch in the treatment of severe persistent inguinal postherniorrhaphy pain: a randomized, double-blind, placebo-controlled trialPLoS One2014910e10914425290151
- BischoffJMPetersenMUceylerNSommerCKehletHWernerMULidocaine patch (5%) in treatment of persistent inguinal postherniorrhaphy pain: a randomized, double-blind, placebo-controlled, crossover trialAnesthesiology201311961444145223887198
- ClarkeHBoninRPOrserBAEnglesakisMWijeysunderaDNKatzJThe prevention of chronic postsurgical pain using gabapentin and pregabalin: a combined systematic review and meta-analysisAnesth Analg2012115242844222415535
- ChaparroLESmithSAMooreRAWiffenPJGilronIPharma-cotherapy for the prevention of chronic pain after surgery in adultsCochrane Database Syst Rev20137CD008307
- BischoffJMKoscielniak-NielsenZJKehletHWernerMUUltrasound-guided ilioinguinal/iliohypogastric nerve blocks for persistent inguinal postherniorrhaphy pain: a randomized, double-blind, placebo-controlled, crossover trialAnesth Analg201211461323132922467891
- WijayasingheNRingstedTKBischoffJMKehletHWernerMUThe role of peripheral afferents in persistent inguinal postherniorrhaphy pain: a randomized, double-blind, placebo-controlled, crossover trial of ultrasound-guided tender point blockadeBr J Anaesth2016116682983727199314
- VerhagenTLoosMJAScheltingaMRMRoumenRMHThe Groin-Pain trial: a randomized controlled trial of injection therapy versus neurectomy for postherniorraphy inguinal neuralgiaAnn Surg Epub2017426
- MakharitaMYAmrYMPulsed radiofrequency for chronic inguinal neuralgiaPain Physician2015182E147E15525794213
- KastlerAAubrySPiccandVHadjidekovGTiberghienFKastlerBRadiofrequency neurolysis versus local nerve infiltration in 42 patients with refractory chronic inguinal neuralgiaPain Physician201215323724422622908
- SchuSGulveAElDabeSSpinal cord stimulation of the dorsal root ganglion for groin pain-a retrospective reviewPain Pract201515429329924690212
- LevineABStevenDAParrentAGMacDougallKWSuccessful long-term nerve root stimulation for chronic neuropathic pain: a real world, single center Canadian experiencePain Physician20172029510628158157
- SchwartzJSStrosbergDSRentonDBChronic groin pain following anterior hernia surgeryJacobBPChenDCRamshawBTowfighSThe SAGES Manual of Groin PainChamSpringer2016211219
- MooreAMBjurstromMFHiattJRAmidPKChenDCEfficacy of retroperitoneal triple neurectomy for refractory neuropathic inguinodyniaAm J Surg201621261126113227771034
- KockerlingFBergerDJostJOWhat is a certified hernia center? The example of the German hernia society and German society of general and visceral surgeryFront Surg201412625593950
- NolsøeAAndresenKRosenbergJRepair of recurrent hernia is often performed at a different clinicHernia201620678378727743212
