Abstract
Background
The incidence of chronic postoperative pain following lumbar spinal surgery has increased with the overall increase in the prevalence of lumbar surgery. This study was conducted to evaluate the analgesic effectiveness of pulsed electromagnetic field (PEMF) therapy in subjects with persistent pain following lumbar surgery.
Patients and methods
A randomized, double-blind, sham-controlled, multicenter study in 36 subjects with persistent low-back and/or radiating leg pain after lumbar surgery was conducted. Eligible subjects were randomized (1:1:1) to receive one of two doses of therapy (42-μs or 38-μs pulse width) or treatment with a sham device. Subjects self-treated twice daily for 60 days. The primary end point was change in pain intensity (∆PI) using the Numerical Pain Rating Scale between average baseline (Days −5 to −1) and end of treatment (Days 56–60) for lumbar and radiating leg pain. Secondary outcome measures included the Oswestry Disability Index, Beck Depression Inventory-II, Patient Global Impression of Change, and consumption of analgesics.
Results
Low-back pain scores for the 42-μs group decreased by 40.2% (p = 0.028), compared to 18.6% for the 38-μs pulse width group (p = 0.037) and 25.6% for the sham group (p = 0.013 per protocol population). Average leg pain scores decreased by 45.0% (42 μs, p = 0.009), 17.0% (38 μs, p = 0.293), and 24.5% (sham, p = 0.065). The proportion of subjects responding to therapy, time to 30% reduction in pain scores, and Patient Global Impression of Change were improved with the PEMF 42-μs device over the sham control, although results were associated with p-values >0.05.
Conclusion
PEMF therapy (42-μs pulse width) was associated with trends for a reduction in pain, compared to sham treatment. Secondary endpoints were consistent with an overall beneficial effect of the PEMF 42-μs pulse width device.
Introduction
In the USA, it has been estimated that more than 80,000 individuals per year experience chronic pain and/or complications after back surgery.Citation1 Persistent or recurrent back and/or leg pain following back surgery – whether associated with laminectomy, discectomy, fusion, or other procedures – is referred to as failed back surgery syndrome (FBSS).Citation2–Citation5 Considering patients with FBSS separately from those with similar symptoms but who have not undergone surgery is important, because identification of the underlying cause of pain of patients in this subgroup has therapeutic implications.Citation4,Citation6 Patients with persistent pain following back surgery may present with axial (low-back) pain and/or radiating leg pain of varying degrees,Citation2,Citation3,Citation6–Citation8 despite having had anatomically satisfactory spinal surgery.Citation4,Citation9,Citation10 The underlying cause of FBSS varies by patient. It can be due to mechanical or neuropathic conditions that develop postoperatively, or, in some cases, it can be due to an initial misdiagnosis of the origin of pain, which, as a result, was not addressed by the surgery.Citation3,Citation5,Citation6,Citation11
Understanding what constitutes effective management strategies for FBSS remains challenging due to the complex neuropathology of FBSS,Citation12 the heterogeneity of underlying causes of FBSS,Citation1,Citation3,Citation4,Citation12 and the need for more clinical data to support an evidence-based approach to treatment.Citation13 Several types of interventions are used to treat FBSS. Typically, conservative (eg, physical therapy, medication) and/or minimally invasive (eg, epidural injection, adhesiolysis) interventions are used prior to undertaking repeat spinal surgery, which is associated with a decrease in success rate for each subsequent surgery compared with the first surgery.Citation1,Citation3,Citation14 Some interventions used to treat FBSS can introduce complications. Pharmaceutical options, for example, are often associated with adverse side effectsCitation15–Citation18 and have the potential for misuse and addiction,Citation17,Citation19 whereas invasive options have been associated with complications such as migration (for implanted devices) and infection.Citation18
Alternative approaches for the treatment of chronic pain associated with FBSS include implanted spinal cord stimulators (SCS),Citation18,Citation20,Citation21 radiofrequency (RF) ablation (denervation or rhizotomy),Citation2,Citation3,Citation5 and, more recently, pulsed electromagnetic field (PEMF) therapy.Citation22 Each of these approaches involve electric currents – either delivered via an electrode (SCS or RF ablation) or induced (PEMF) – with the goal of either modifying pain signaling (SCS and PEMF) or ablating nervous tissue (RF ablation) via different methods. There are no data indicating that PEMF devices can induce electrical currents and, possibly, directly modify vital functions. PEMF can, however, alter gene and protein expression. PEMF therapy involves generating a PEMF with a coil located within an applicator pad that is placed adjacent to the area of the body to be treated. In the case of the PEMF device used in the current trial, a carrier frequency (27.12 MHz) is also employed. Biological effects using this approach most likely occur via induction of electrical current within the tissue.Citation23,Citation24
Whereas clinical data suggest PEMF therapy is effective for the treatment of postoperative pain in soft tissues,Citation23,Citation25 there have been no randomized, double-blind, controlled clinical trials to date on the use of PEMF therapy for FBSS pain. Results of a recent open-label pilot study using PEMF therapy for FBSS pain found clinically meaningful improvements in a subset of study subjects.Citation22 As a follow-up to this study, the current study was designed to examine the effect of PEMF therapy in a multicenter, randomized, sham-controlled, double-blind study in patients with chronic pain following lumbar surgery. The hypothesis was that the 42-μs dose was superior to the sham control. The 38-μs dose was exploratory to examine whether preliminary laboratory observations with this dose would be associated with clinical effects.
Patients and methods
Study design
This was a pilot, multicenter, randomized (1:1:1), double-blind, sham-controlled, parallel-group study designed to evaluate the analgesic effectiveness of PEMF treatment in patients with persistent pain following lumbar surgery (ClinicalTrials.gov identifier: NCT02416973).Citation51 Treatment was administered twice daily over a 60-day period. The study was conducted at 13 sites in the USA and was designed to enroll 45 patients. Ethics committee approval was obtained from the Quorum Independent Review Board for each site () prior to starting the study, and the study was conducted in compliance with the International Standard of Good Clinical Practice (ICH E6-GCP) procedures and the principles of the Declaration of Helsinki (1964).
Study population
The key inclusion criteria were previous anatomically successful lumbar back surgery for low-back pain, persistent pain in the low back and/or radiating to leg(s) for greater than or equal to 3 months and less than or equal to 36 months following the most recent surgery, stable analgesic dosing regimen for greater than or equal to 30 days, and an mean pain intensity (PI) of greater than or equal to three and less than nine on the 11 point Numerical Pain Rating Scale (NPRS; ). Potential subjects underwent a Screening Visit (Day −14 to Day −10). Written informed consent for study participation was obtained from all subjects.
Table 1 Key inclusion and exclusion criteria
Study procedures
Subjects meeting the inclusion and exclusion criteria () entered the 10-day run-in phase of the study. During the run-in phase, subjects were trained in the use of the electronic patient-reported outcome (ePRO) diary, and enrolled into the baseline period of the diary. Subjects were randomized if they continued to meet inclusion criteria and none of the exclusion criteria at the end of the run-in period. Randomization was in a 1:1:1 ratio to therapy with one of two active PEMF devices (42-μs or 38-μs pulse width) or an identical inactive sham device. The randomization numbers were auto-assigned to subjects from the individual sites’ randomization list through a secure interactive web response system as subjects qualified for inclusion into the study. The currently marketed and US Food and Drug Administration (FDA) cleared device (Provant® Therapy System, Regenesis Biomedical, Scottsdale, AZ, USA) utilizes a 42-μs pulse width. Further experimentation was carried out using cells in culture at Regenesis Biomedical and was based on published literatures.Citation23–Citation25 The second active arm was added on the basis of internal laboratory-based research to explore whether a reduction in pulse width would impact efficacy when compared to the 42-μs setting. New therapeutic modalities or additional therapeutic regimens other than the study device were not permitted during the study.
Subjects were instructed to self-treat for 30 minutes twice daily (morning and evening; 8 am ± 2 hours and 8 pm ± 2 hours) for 60 days when at home. Interim Visits were conducted on Days 15, Day 30, and Day 61 to assess safety, concomitant medications, weight, high sensitivity C-reactive protein (hsCRP), the Oswestry Disability Index (ODI), and Beck Depression Inventory II (BDI). Subjects who experienced increased pain during the study were instructed to increase self-administration of their prescribed analgesic(s). Likewise, subjects who experienced decreased pain during the study were instructed to decrease self-administration of their prescribed analgesic(s).
Study devices
The PEMF device used in the study (Provant® Therapy System) uses a solid-state, fixed-power output radiofrequency generator and transmitter designed to operate at the Federal Communication Commission-authorized medical device frequency of 27.12 MHz. Provant is cleared by the FDA for use as an adjunctive treatment for postoperative pain and edema in superficial soft tissues. The therapy system generates a pulsed electromagnetic field using a Class-C RF amplifier. Two pulse durations were evaluated in this study: 42 and 38 μs. Pulses are repeated every 1,000 μs, resulting in an output duty cycle of 4.2% and 3.8% and requiring an average forward power level of <5 W. The amount of forward energy emitted from the treatment applicator is preset at 591 ± 44 V/m at a distance of 5.0 cm from the radiating surface of the treatment applicator. The doses with the current device were based on the FDA-approved and currently marketed device. Further experimentation was undertaken using cells in culture at Regenesis Biomedical and was based on published literatures.Citation23–Citation25
Sham devices were identical to active devices, except that they were deactivated such that no electromagnetic field energy was generated or delivered when the device was turned on. All other functions were identical to that of the active study devices.
ePRO Diary data collection
All subjects in the study were provided with an ePRO Diary login (DSG Inc, Malvern, PA, USA) to access the diary from any Internet browser for use during the study to allow for collection of patient-reported outcomes (average and worst PI, analgesic consumption, and Patient Global Impression of Change [PGIC]). Subjects were instructed by the site, by using a standardized script, to record their PI and analgesic consumption each morning at 8 am (±2 hours) during the 10-day run-in period (Day −10 to Day −1). Furthermore, subjects were instructed to record their ePRO data (PI, analgesic consumption, and PGIC) immediately following each morning treatment for 60 days (Days 1–60), and continue to collect ePRO data for 15 days following completion of treatment each morning at 8 am (±2 hours). Subjects were prompted to report the daily mean and worst PI for their lumbar back pain and/or radiating leg pain separately, analgesic consumption, and PGIC every 7 days. For analgesic consumption, subjects were prompted to report their analgesic consumption (opioid and nonopioid) prescribed for the treatment of the subject’s lumbar back and/or radiating leg pain over the preceding 24 hours.
Outcome measurements
Pain intensity
The PI was self-reported by subjects using the validated 11-point NPRS.Citation26,Citation27 For PI analyses, mean PI scores were calculated for every 5-day interval of the trial period (ie, a total of 16 intervals for per protocol [PP] subjects) for each of the four PI score categories reported (ie, worst back PI, mean back PI, worst leg PI, mean leg PI). The baseline PI was defined as the mean PI for the last 5 days of the 10-day run-in period, and end-of-treatment PI was defined as the mean PI for the last 5 days of the 60-day treatment period.
Responder analyses
For the prespecified responder analysis, subjects reporting a two-point reduction in PI or a 30% decrease in PI from baseline were considered responders.Citation29
Area under the curve
Post hoc area under the curve (AUC) analyses were conducted to assess PI changes over time for all randomized subjects without imputation. AUC analyses were undertaken using SAS software.Citation28
Change from baseline PI AUC
The analysis was conducted using SAS software by integration.
Analgesic consumption
Subjects self-reported their consumption of analgesic tablets by recording the number of pills of each medication consumed in the preceding 24 hours in the ePRO diary. Analgesic medications refer to medications prescribed and administered for the treatment of pain and included opioids, nonsteroidal anti-inflammatory agents, antidepressants, and muscle relaxants. The analysis on analgesic consumption was based on the number and percentage change in the number of pills taken at each 5-day period compared with the 10-day run-in period.
Other patient-reported outcomes
The PGIC is a seven-point validated categorical scale of overall change in status.Citation29,Citation30
The ODI (version 2.1a) consists of a self-reported questionnaire in categorical format that assesses a subject’s level of disability for common activities such as walking, sleeping, and personal care.Citation31
Symptoms of depression were assessed using the BDI, version II.Citation32 A score of 13 or less is considered indicative of minimal depression, whereas a score of 29 or greater indicates severe depression.
High-sensitivity C-reactive protein
The hsCRP levels were assayed using blood samples obtained at the Enrollment and Interim Visits as a biomarker of inflammation.Citation33,Citation34
Safety
Safety was monitored through the collection of adverse events, including serious adverse events. The Medical Dictionary for Regulatory Activities coding dictionary was used to categorize adverse events.
Statistical analyses
Analysis of the primary endpoint (PI) was conducted on the intent-to-treat (ITT) population using the last observation carried forward (LOCF) imputation method, together with a median and quartile imputation. A sensitivity analysis was undertaken on the primary endpoint using a PP population. The PP population was identified prior to the unblinding of the study data and was defined on the basis of subjects that completed 60 days of treatment and did not have significant protocol deviations. The quartile imputation was a worstcase imputation that used the 25th percentile of the treatment group to impute values for the active groups and used the 75th percentile for imputation of values in the sham group. There were no imputations carried out on missing data for the secondary endpoints. There were no adjustments for multiple testing. Adverse events were summarized by number and incidence. The sample size of 15 patients per group and 45 in total was a sample of convenience for this study. No power calculations were conducted.
Statistical tests to evaluate the significance of within-group (WG) and between-group (BG) differences in PI scores were conducted in SAS software. WG and BG differences were tested using one-way analysis of variance. Data were plotted using Sigma Plot 13.0.
Results
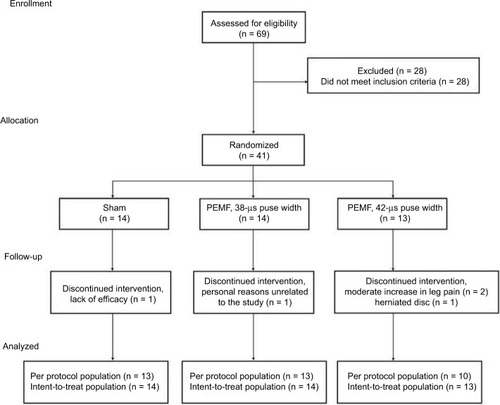
In total, 69 subjects were screened at 13 sites. Of the 69 screened, 52 subjects entered the 10-day run-in period. Eleven subjects were found to be ineligible during the run-in period, leaving 41 eligible subjects who were enrolled in the study and who received at least one treatment (ITT population). Of the 41 subjects in the ITT population, 36 subjects completed the 60-day treatment protocol (PP population). Of the five ITT subjects who withdrew early, three subjects (42-μs group) withdrew on Days 9, 32, and 36 due to an adverse event, one subject (38-μs group) withdrew on Day 7 due to personal reasons, and one subject (sham group) withdrew on Day 15 due to lack of efficacy (). The study was closed to enrollment prior to achieving the planned enrollment (45 subjects) in order to allow for inclusion of study results in a planned regulatory submission.
Figure 1 Study flow chart and patient profile.
Demographics
Demographics and clinical characteristics at baseline were generally similar between study groups (). There was a slightly higher proportion of males in the 42-μs group (62%, 8/13) relative to the sham group (36%, 5/14). The mean duration of time from the most recent surgery was 12.7, 12.6, and 15.1 months for the 42-μs, 38-μs, and sham groups, respectively. Baseline data were generally similar for each of the study groups. The majority of subjects reported both lumbar (40/41) and radiating leg (35/41) pain. Mean BDI scores were low at baseline for all study groups. In terms of concurrently used interventions during the study, 83% of ITT subjects reported participating in regular at-home stretching or exercise, and 7% of ITT subjects received in-office physical therapy.
Table 2 Subject demographics and baseline characteristics
Compliance
The mean total duration of device usage per subject during the study was 57.2 ± 4.4, 49.7 ± 14.5, and 46.7 ± 17 hours, respectively, for the 42-μs, 38-μs, and sham groups for the PP population, based on the device usage meter data.
Pain intensity
The mean end-of-treatment PI was lower for the 42-μs group than for the other study groups, for both lumbar and radiating leg pain ( and B, ). The primary endpoint which was the percentage change from baseline in mean PI scores through Day 60 (end-of-treatment) summaries were conducted on the ITT populations using the LOCF method for imputation of missing data along with a median and quartile imputation. The mean lumbar PI for the 42-μs group decreased by 1.1 units (−17.9%) compared with 1.4 units (−24.9%) in the 38-μs group and 1 unit (−21.1%) in the sham group. For the mean radiating leg PI, the 42-μs group decreased by 1.3 units (−20.2%), compared with 1.1 units (−21.3) in the 38-μs group and 0.9 units (−26.1%) in the sham group. A sensitivity analysis was conducted on the PP population and showed a similar trend, with a greater decrease in both lumbar and radiating leg PI reported for the 42-μs group compared to the 38-μs group or the sham group. Mean lumbar PI for the 42-μs group decreased by 2 units (40.2%, p = 0.028), compared to a decrease of 1.3 units (18.6%, p = 0.037) and 1.3 units (25.6%, p = 0.013) for the 38-μs and sham groups, respectively (, ). shows pain scores normalized to baseline values. For mean radiating leg PI, a decrease of 2.3 units was observed at the end of treatment relative to baseline for the 42-μs group (45.0%, p = 0.009), compared to a decrease of 1.1 units for the 38-μs group (17.0%, p = 0.293), and a decrease of 1 unit (24.5%, p = 0.065) for the sham group (, ).
Figure 2 Mean pain scores at the end of treatment (Days 56–60) compared with baseline.
Abbreviation: NPRS, numerical pain rating scale.
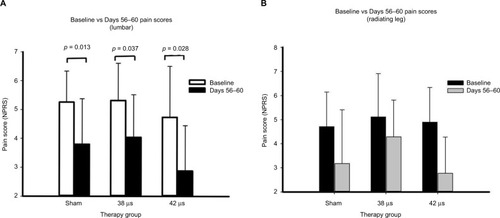
Figure 3 Mean pain scores over time.
Abbreviations: NPRS, numerical pain rating scale; PEMF, pulsed electromagnetic field.
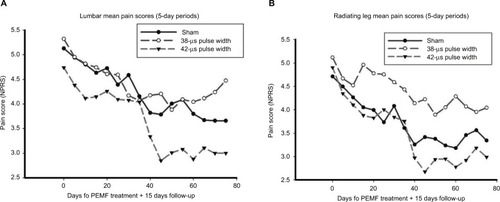
Figure 4 Mean pain scores over time normalized to baseline.
Abbreviation: PEMF, pulsed electromagnetic field.
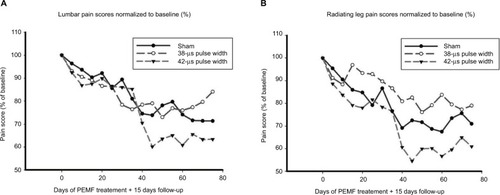
Table 3 Primary outcome measure at 60 days
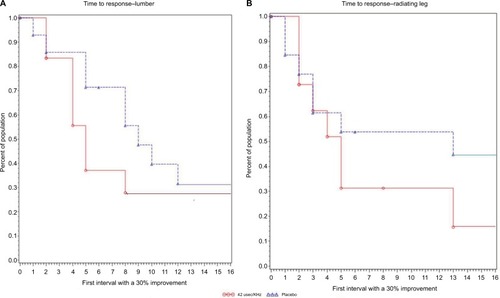
The change in PI was further evaluated by a prespecified responder analysis as well as by a post hoc AUC analysis and time-to-event analysis for PI over the course of the study (). In all cases, results were consistent with those obtained for the primary endpoint. For the responder analysis, subjects who experienced a reduction in PI of 2 points or 30% (mean final PI vs average baseline PI) were considered responders. A two-point or 30% reduction in the pain scores is considered a clinically meaningful change in PICitation27,Citation29 and is associated with not needing rescue medication and ratings of “much” or “some” improvement.Citation29 Based on the latter criterion, 55.6% and 53.9% of PP subjects in the 42-μs and 38-μs groups, respectively, were responders based on change in lumbar PI, compared to 30.8% of PP subjects in the sham group (). None of the subjects reported a two-point decrease in PI without a 30% decrease in PI. In addition, a 50% or greater reduction in lumbar PI was observed in 44.4% of subjects in the 42-μs group, compared with no subjects in the 38-μs group, and 15.4% of subjects in the sham group. A reduction in PI of 50% or greater is considered to represent substantial improvement, corresponding to a rating of “very much improved.”Citation29 Similar trends were observed for the responder analyses of mean radiating leg PI (). The median time to 30% response for both lumbar and radiating leg PI was shorter in the 42-μs group (21–25 days and 21–25 days, respectively) compared with the other study groups: 61–65 and 41–45 days, respectively in the sham group, and 35–40 and 41–45 days for the 38-μs group ().
Table 4 Secondary outcome measures at 60 days
Post hoc pain AUC analyses were conducted in order to utilize all data for all randomized subjects without imputation.Citation28 Analyses were conducted without and with adjustments for baseline differences. The unadjusted AUC for mean lumbar PI was numerically (24.5%) less for ITT subjects in the 42-μs group (186.5 ± 84.2) compared with the sham group (246.9 ± 74.1; p = 0.694, ). Consistent with the primary endpoint, findings were similar for AUC between the sham and the 38-μs groups (251.4 ± 120.9). For mean radiating leg PI, the AUC for ITT subjects in the 42-μs group (173.5 ± 70.8) was 19.3% less than that for the sham group (AUC: 238.1 ± 101.1; p = 0.231). The mean radiating leg AUC for the 38-μs group was similar to that for the sham group ().
The analysis of AUC adjusted for baseline differences for the mean change from baseline PI showed a 130.3% decrease in this measure for radiating leg PI in the 42-μs group (−69.7), which was larger than the same measure for the sham group (−29.4). Furthermore, results for the 38-μs group were better than those observed for the sham group (−48.2) although no results for any of the groups reached statistical significance ().
The median time to 30% reduction in pain scores was numerically shorter for the active 42-μs group: Interval 5 (Days 21–25) compared to Interval 9 (Days 41–45) for the sham group for lumbar pain (p = 0.33, ). For radiating leg pain, in the 42-μs group, the median time to response was Interval 5 (Days 21–25), compared to Interval 13 (Days 61–65) for the sham group (p = 0.32, ). The changes for the 38-μs group are somewhat between that of the 42-μs and the sham groups (data not shown).
Figure 5 Time to 30% reduction in pain score is the time to response. Figures show the time to 30% reduction, which was evaluated using Kaplan–Meier statistics.
Secondary endpoints
To monitor possible effects of the therapy on inflammation, levels of the inflammatory marker hsCRP were assessed at baseline and at Day 61 following the end of treatment. For the 42-μs group, the mean hsCRP level was lower at Day 61 compared to baseline ( and ), whereas, conversely, the mean hsCRP levels for the sham and 38-μs groups were higher at Day 61 compared with baseline ( and ) although BG differences were associated with p > 0.05. No relevant BG differences were observed for ODI and BDI (). On Day 60, 75% of subjects in the 42-μs group reported some level of improvement based on data collected using the PGIC questionnaire, whereas 58.2% and 44.4% of sham and 38-μs group subjects, respectively, reported some level of improvement. With regard to analgesic use, all groups showed minor decreases in analgesic use. For the sham group, the median decrease in pill count at Days 56–60 was −0.67 ± 1.38, n = 12. For the 38-μs and 42-μs pulse groups, the decrease in pill counts was −0.34 ± 0.80, n = 13 and 1.06 ± 1.13, n = 9, respectively. Changes in the secondary endpoints, although directionally in favor of active treatment, may not necessarily be considered clinically significant.
Safety
Adverse events were reported in six subjects (46.2%) in the 42-μs group, three subjects (21.4%) in the 38-μs group, and five subjects (35.7%) in the sham group. None of the events were considered serious. Musculoskeletal disorders were the most common adverse event reported, with 5 in the 42-μs group (back pain [2], disc protrusion [1], and extremity pain [2]), 0 in the 38-μs group, and 1 (back pain) in the sham group. All of the other adverse events were reported by no more than one subject within a treatment group.
Discussion
Diagnosing FBSS (also called Postoperative Persistent Syndrome, ie, POPS)Citation4 and understanding its etiology is complex and has led to challenges in treatment.Citation3 Interventional procedures such as epidural injections, ablation, or finally surgical revision have met with limited success.Citation35,Citation36 Conservative treatments such as physical therapy, acupuncture, and behavioral therapies are noninvasive and, therefore, are commonly used treatments. However, these treatments are typically combined with pharmacological management to reduce pain, which can introduce additional unwanted consequences. Alternative treatments that rely on direct or indirect electrical stimulation of the spinal column have shown promise. SCS uses implantation of electrodes to delivery direct electrical stimulation to the spinal column. Alternatively, PEMF therapy involves application of an electromagnetic field to the affected lumbar region. Unlike SCS, such an approach obviates the need for electrodes, thus is noninvasive, and can be self-administered.
In this article, we describe a pilot, double-blind, randomized clinical study that shows encouraging clinical results about the efficacy of PEMF therapy for the treatment of chronic pain associated with FBSS. This study investigated the use of PEMF therapy as an adjunctive intervention for postoperative pain in a defined group of subjects who had previously undergone back surgery (lower lumbar, nonfusion) and reported chronic back and/or radiating leg pain. The strength of the current study is the double-blind, sham-controlled study design, which is not commonly incorporated in clinical interventional studies of FBSS. Whereas the focus was on the currently available active treatment (42-μs group), a second exploratory active arm was added (38-μs group). The primary outcome analysis evaluated the average percentage reduction in PI between baseline and end of treatment (Days 56–60). By this measure, the 42-μs group reported a mean decrease of 40.2% in back PI at the end of treatment compared with a decrease of 25.6% in PI for the sham group (). The mean decrease in leg PI reported for the 42-µs group was 45.0% compared with a decrease of 24.5% for the sham group. Moreover, results of responder, AUC, and time-to-event analyses were consistent with these findings. We readily acknowledge that the results of the prespecified analyses did not reach nominal statistical significance (ie, p < 0.05); however, the sample was not powered for such differences. Nevertheless, several endpoints and alternative analyses demonstrated a consistent pattern indicative of a true treatment effect.
The decreases in pain scores were associated with modest decreases in analgesic use. It may be considered more relevant that the improvements in pain scores could not be attributed to any increase in self-administration of analgesics. Nevertheless, it is recognized that self-reporting of analgesic use and documentation of the reasons for such use can be challenging in clinical trials.
Even though it is not commonly used in FBSS trials, measurement of hsCRP may have some value as a quantitative tool for accessing pain in clinical trials for therapeutic treatments. Despite the applicability of hsCRP in lumbar pain trials being not well established, the decrease in the hsCRP levels in the 42-μs group suggest that this marker could be of value in assessing the effectiveness of therapeutic products for pain relief.Citation33,Citation34
Surprisingly, a small reduction in the dose of PEMF energy appeared to be associated with a diminution of the therapeutic effect. The decrease in pulse width to 38-μs resulted in a decrease of PEMF dose by 10%. This result underscores the need for further evaluation and optimization of PEMF therapy for the type of tissue and anatomical location being treated.
Another aspect of this study was to establish a placebo effect of PEMF therapy and medical devices in general.Citation37–Citation39 A true sham device is difficult to implement in the field of neuromodulation because of the nature of the therapy. Routinely, medical devices such as transcutaneous electrical nerve stimulation or SCS rely on conventional medical management as a control value in randomized controlled trials. The placebo effect may bring into question the interpretation of pain management therapies when a placebo cannot, or is not, used – especially in the treatment of chronic pain associated with FBSS. In this study, we found that the 42-μs group reported a moderately better outcome for PI improvement over placebo, although with the limitation that the trial included a small number of subjects and the results were not, in general, statistically significant.
As with other types of back pain, both nociceptive and neuropathic mechanisms may contribute to chronic pain associated with FBSS, depending on the underlying cause of an individual’s pain symptoms.Citation4,Citation12 Whether continual stimulation of nociceptive pathways due to mechanical injury or prolonged peripheral sensory stimulation leading to neuropathic pain can cause chronic lumbar pain or FBSS is unclear.Citation3,Citation36 It has been suggested that, in some cases, FBSS could be the result of abnormal excitability of both the afferent or sensory neurons in the peripheral and central nervous systems.Citation12
In terms of mechanism of action, one hypothesis is that PEMF may induce Eddy currents in biological tissue, which could in turn mediate downstream biological effects. Interventions involving electrical stimulation may inhibit pain in part by direct modulation of the nervous system, perhaps by stimulation of inhibitory sensory neurons as proposed in gate control theory,Citation40,Citation41 and/or mediate local electrochemical changes,Citation24 which may, in turn, have downstream effects on gene expression.Citation23,Citation42–Citation46 Recent evidence suggests that SCS and PEMF can mediate changes in gene expression, including genes implicated in pain pathways such as endogenous opioids and eicosanoid enzyme pathways.4243,45,46 Decreases in pain via a neuromodulation mechanism may explain, at least in part, improvements in radiating leg pain in this study and others.Citation47,Citation48 Attempts to use neuromodulation in the treatment of FBSS and neuropathy in general would benefit from a better understanding of the mechanism of action of treatment options that may mediate such an effect. Based on the results of this study, we hypothesize that specific PEMF energetics are effective for the treatment of chronic lumbar and radiating leg pain associated with FBSS.
This study had several primary limitations. Although this study was a double-blinded, randomized sham-controlled trial, the sample size was relatively small and changes did not show substantial differences between the groups. Nevertheless, trends were observed in favor of PEMF at a specific dose of 42 μs. Data from this study can be used as a basis for the design and sample size of future studies. A second limitation of this study was the time of treatment. Most studies conducted with medical devices that may affect neuromodulation (eg, SCS trials) cover a therapy period of 6–12 months with at least a 2-year follow-up.Citation20,Citation49,Citation50 The lack of an extended follow-up limits the interpretation of whether PEMF therapy is actually resolving the cause of the pain or masking it. The last limitation relates to the aforementioned use of as-needed analgesics, which can confound pain score results; however, the as-needed use of pain medications reflects “real-life” practice and clinical care.
Conclusion
The current study on subjects with persistent pain 3–36 months after lumbar surgery demonstrated consistent trends for a reduction in pain at the end of a 60-day treatment protocol with PEMF therapy compared with sham treatment. For subjects responding to the therapy, the time to 30% reduction in pain scores, PGIC, and the reduction in the inflammatory marker hsCRP were consistent with a beneficial effect of PEMF over sham control. The potential influence of therapy dose was also shown, in that a 10% reduction in PEMF energy was associated with a possible diminution of therapeutic outcomes. In comparison with sham, this study supports the effectiveness of PEMF therapy for producing pain relief in patients with persistent pain following lumbar surgery. However, it is recognized that changes did not consistently exceed what is considered to be clinically meaningful. Although the results are encouraging, the findings should not be considered definitive. The data generated can be used to design larger trials with statistical power to confirm the efficacy of PEMF.
Acknowledgments
The authors acknowledge Dr Adrianne Smith, MD and Nicole Kubat, PhD for their help in drafting the article and critical review. The study was funded by Regenesis Biomedical Inc., Scottsdale, AZ, USA.
Supplementary material
Table S1 Titles of participating sites:
Disclosure
The authors report no conflicts of interest in this work.
References
- RagabADeshazoRDManagement of back pain in patients with previous back surgeryAm J Med2008121427227818374682
- BaberZErdekMAFailed back surgery syndrome: current perspectivesJ Pain Res20169979987 eCollection 201627853391
- ChanCWPengPFailed back surgery syndromePain Med201112457760621463472
- RigoardPDesaiMJTaylorRSFailed back surgery syndrome: what’s in a name? A proposal to replace “FBSS” by “POPS”Neurochirurgie201561Suppl 1S16S2125665773
- HussainAErdekMInterventional pain management for failed back surgery syndromePain Pract2014141647823374545
- AssakerRZairiFFailed back surgery syndrome: to re-operate or not to re-operate? A retrospective review of patient selection and failuresNeurochirurgie201561Suppl 1S77S8225662850
- BordoniBMarelliFFailed back surgery syndrome: review and new hypothesesJ Pain Res20169172226834497
- Vleggeert-Lankamp CL, Arts MP, Jacobs WCh, Peul WC. Failed back (surgery) syndrome: time for a paradigm shiftBr J Pain201371485526516497
- KumarKNorthRTaylorRSpinal cord stimulation vs. conventional medical management: a prospective, randomized, controlled, multicenter study of patients with failed back surgery syndrome (PROCESS study)Neuromodulation20058421321822151547
- LevequeJCVillavicencioATBulsaraKRRubinLGoreckiJPSpinal cord stimulation for failed back surgery syndromeNeuromodulation2001411922151565
- NorthRBEwendMGLawtonMTKiddDHPiantadosiSFailed back surgery syndrome: 5-year follow-up after spinal cord stimulator implantationNeurosurgery19912856926991831547
- BlondSMertensPDavidRRoulaudMRigoardPFrom “mechanical” to “neuropathic” back pain concept in FBSS patients. A systematic review based on factors leading to the chronification of pain (part C)Neurochirurgie201561Suppl 1S45S5625596973
- RigoardPAssakerRFailed back surgery syndrome: from pathophysiology to recent therapeutic advances in neurostimulation – introductionNeurochirurgie201561Suppl 1S525744250
- RajaeeSSBaeHWKanimLEDelamarterRBSpinal fusion in the United States: analysis of trends from 1998 to 2008Spine (Phila Pa 1976)2012371677621311399
- HaanpääMLGourlayGKKentJLTreatment considerations for patients with neuropathic pain and other medical comorbiditiesMayo Clin Proc2010853 SupplS15S25
- LeeMSilvermanSMHansenHPatelVBManchikantiLA comprehensive review of opioid-induced hyperalgesiaPain Physician201114214516121412369
- ManchikantiLBenyaminRDattaSVallejoRSmithHOpioids in chronic noncancer painExpert Rev Neurother201010577578920420496
- ChouRHuffmanLHGuideline for the Evaluation and Management of Low Back Pain: Evidence ReviewGlenview, ILAmerican Pain Society2007
- SirohiSTiwariAKPain in the management of opioid use disorderJ Pain Res20169963966 eCollection 201627853389
- GriderJSManchikantiLCarayannopoulosAEffectiveness of spinal cord stimulation in chronic spinal pain: a systematic reviewPain Physician2016191E33E5426752493
- VerrillsPSinclairCBarnardAA review of spinal cord stimulation systems for chronic painJ Pain Res2016948149227445503
- HarperWLSchmidtWKKubatNJIsenbergRAAn open-label pilot study of pulsed electromagnetic field therapy in the treatment of failed back surgery syndrome painInt Med Case Rep J20148132225678825
- GuoLKubatNJIsenbergRAPulsed radio frequency energy (PRFE) use in human medical applicationsElectromagn Biol Med2011301214521554100
- MalmivuoJPlonseyRElectric and magnetic stimulation of neural tissueMalmivuoJPlonseyRBioelectromagnetism: Principles and Applications of Bioelectric and Biomagnetic FieldsNew YorkOxford University Press1995363380
- GuoLKubatNJNelsonTRIsenbergRAMeta-analysis of clinical efficacy of pulsed radio frequency energy treatmentAnn Surg2012255345746722301609
- FarrarJTPolomanoRCBerlinJAStromBLA comparison of change in the 0–10 numeric rating scale to a pain relief scale and global medication performance scale in a short-term clinical trial of breakthrough pain intensityAnesthesiology201011261464147220463579
- FarrarJTYoungJPJrLaMoreauxLWerthJLPooleRMClinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scalePain200194214915811690728
- PruessnerJCKirschbaumCMeinlschmidGHellhammerDHTwo formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent changePsychoneuroendocrinology200328791693112892658
- DworkinRHTurkDCWyrwichKWInterpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendationsJ Pain20089210512118055266
- ScottWMcCrackenLMPatients’ impression of change following treatment for chronic pain: global, specific, a single dimension, or many?J Pain201516651852625746196
- FairbankJCPynsentPBThe Oswestry Disability IndexSpine (Phila Pa 1976)2000252229402952 discussion 295211074683
- BeckATWardCHMendelsonMMockJErbaughJAn inventory for measuring depressionArch Gen Psychiatry1961456157113688369
- ParkCHLeeSHInvestigation of high-sensitivity C-reactive protein and erythrocyte sedimentation rate in low back pain patientsKorean J Pain201023214715020556218
- RathodTNChandanwaleALadkatKMChavanSChavanABhosalePBHigh sensitive C-reactive protein-effective tool in determining postoperative recovery in lumbar disc diseaseIndian J Orthop201448435435925143637
- HayekSMHelmSBenyaminRMSinghVBryceDASmithHSEffectiveness of spinal endoscopic adhesiolysis in post lumbar surgery syndrome: a systematic reviewPain Physician200912241943519305488
- MarkmanJDKressBTFrazerMHansonRKoganVHuangJHScreening for neuropathic characteristics in failed back surgery syndromes: challenges for guiding treatmentPain Med201516352053025530081
- BrodyHPlacebos and the Philosophy of Medicine: Clinical, Conceptual, and Ethical IssuesChicago, ILUniversity of Chicago Press1980
- ConradRThe hardest thing to see is what is in front of your eyes – quo vadis placebo analgesia?J Pain Res20169819823 eCollection 201627789973
- VaseLPetersenGLRileyJL3rdPriceDDFactors contributing to large analgesic effects in placebo mechanism studies conducted between 2002 and 2007Pain200914512364419664881
- MelzackRWallPDPain mechanisms: a new theoryScience196515036999719795320816
- MoayediMDavisKDTheories of pain: from specificity to gate controlJ Neurophysiol2013109151223034364
- KubatNJMoffettJFrayLMEffect of pulsed electromagnetic field treatment on programmed resolution of inflammation pathway markers in human cells in cultureJ Inflamm Res20158596925759595
- MoffettJFrayLMKubatNJActivation of endogenous opioid gene expression in human keratinocytes and fibroblasts by pulsed radiofrequency energy fieldsJ Pain Res2012534735723055776
- ShanthannaHChanPMcChesneyJPaulJThabaneLAssessing the effectiveness of ‘pulse radiofrequency treatment of dorsal root ganglion’ in patients with chronic lumbar radicular pain: study protocol for a randomized control trialTrials2012135222540851
- TilleyDMCedeñoDLKelleyCABenyaminRVallejoRSpinal cord stimulation modulates gene expression in the spinal cord of an animal model of peripheral nerve injuryReg Anesth Pain Med201641675075627512935
- VallejoRTilleyDMCedeñoDLKelleyCADeMaegdMBenyaminRGenomics of the effect of spinal cord stimulation on an animal model of neuropathic painNeuromodulation201619657658627391866
- KumarKTaylorRSJacquesLSpinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndromePain200713212179188
- NorthRBKiddDHFarrokhiFPiantadosiSASpinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trialNeurosurgery200556198106 discussion 106–107
- KapuralLvan BuytenJPVerrillsPResponse: high frequency (10 kHz) or burst spinal cord stimulation in failed back surgery syndrome patients with predominant back pain: preliminary data from a prospective observational studyNeuromodulation201619778727704692
- KumarKHunterGDemeriaDSpinal cord stimulation in treatment of chronic benign pain: challenges in treatment planning and present status, a 22-year experienceNeurosurgery2006583481496 discussion 481–49616528188
- TennantFSajbenNMackJStallRSInterpreting indications for electromagnetic therapyPract Pain Manag201313567 Consensus Statement 7
