Abstract
Purpose
Low back pain (LBP) is one of the most frequent chronic conditions worldwide. Data from a recent meta-analysis indicated that whole-body electromyostimulation (WB-EMS), a time-effective, joint–friendly, and highly individualized training technology, demonstrated promising effects on LBP; however, methodologic limitations prevent definitive evidence for this result. Thus, the aim of this study was to conduct a randomized controlled WB-EMS trial to determine the corresponding effect on chronic, nonspecific LBP in people with chronic LBP.
Patients and methods
Thirty LBP patients, 40–70 years old, were randomly assigned into two groups (WB-EMS: 15; control [CG]: 15). While the nonactive CG maintained their lifestyle, the WB-EMS group completed a 12-week WB-EMS protocol (1×20 min/week) with slight movements, specifically dedicated to LBP. Pain intensity and frequency were determined by a 4-week pain diary before and during the last 4 weeks of intervention. Primary study endpoint was average pain intensity at the lumbar spine.
Results
At baseline, no group differences apart from nonregular exercise were observed. Mean intensity of LBP decreased significantly in the WB-EMS group (P=0.002) and remained unchanged in the CG (P=0.730), with a significant difference between both groups (P=0.027). Maximum isometric trunk extensors improved significantly in the WB-EMS group (P=0.005), while no significant difference was seen in the CG (P=0.683). In contrast to the significant difference between WB-EMS group and CG for the latter parameter (P=0.038), no intergroup difference was determined for maximum isometric trunk flexors (P=0.091). The WB-EMS group showed a significant increase of this parameter (P=0.003), while no significant change was determined in the CG (P=0.563).
Conclusion
WB-EMS is a time-effective training method for reducing chronic nonspecific LBP and increasing maximum trunk strength in people with such complaints. After this promising comparison with a nonactive CG, research needs to be extended to include comparisons with active groups (WB-Vibration, conventional back strengthening).
Introduction
Low back pain (LBP) is one of the leading orthopedic diseases worldwide and affects almost everyone at least once in their lives.Citation1,Citation2 In about 80% of cases, the cause of LBP is not known and is declared nonspecific.Citation3 Physical exercise seems to be an effective conservative method to improve LBP.Citation4 However, nowadays a lack of time might be the main obstacle to exerciseCitation5; so many people may abstain from time-consuming exercise programs. Furthermore, “kinesiophobia”, that is, the fear of movement because of pain, is common in LBP patients and impedes their taking up physical activity.Citation6
A considerable number of studies have already confirmed the effect of training technologies like whole-body vibration on LBP and show positive results.Citation7–Citation10 Other novel methods, such as whole-body electromyostimulation (WB-EMS), have not been addressed by clinical trials, but two master’s theses have addressed LBP in this context.Citation11,Citation12 Nevertheless, the time-effective character of WB-EMS with low subjective intensity seems to be an optimal option for people unmotivated or unable to exercise conventionally. In addition to the benefits mentioned above, the easy and joint-gentle low-intensity, low-amplitude exercises may also optimally respond to the “kinesiophobia” of LBP patients. Therefore, the aim of this study was to compare the effect of WB-EMS with a nonactive control group (CG) on chronic nonspecific LBP patients between 40 and 70 years. Our primary hypothesis was that, compared with the CG, WB-EMS significantly decreases mean pain intensity at the lumbar spine (LS) in people with chronic nonspecific LBP. The secondary hypothesis was that, compared with the CG, WB-EMS increases maximum isometric strength in back and abdominal muscle in people with chronic nonspecific LBP.
Patients and methods
Trial design
The study was a randomized, controlled, 12-week parallel-group trial with nonspecific chronic LBP patients 40–70 years old. In the present study, which constituted the initial phase of a multicenter project that compared the effects of WB-EMS with recognized methods (WB-Vibration, conventional exercises interventions) of nonpharmacologic LBP therapy, we focus on the comparison between WB-EMS application and a non-training control. The study was planned, implemented, and conducted from February to July 2017 at the Institute of Medical Physics (IMP), Friedrich-Alexander University Erlangen-Nürnberg (FAU), Germany. The IMP was supported by the Pain Research Center Erlangen, both part of the University of Erlangen-Nürnberg (FAU) Germany. The study complied with the Helsinki Declaration “Ethical Principles for Medical Research Involving Human Subjects” and was approved by the Ethical Committee of the FAU (ethics application no. 224_15b). After detailed information, all study participants gave their written informed consent. The project was registered under DRKS00009528.
Participants
For the initial project phase, around 5,000 people, 40–70 years old living in the area of Erlangen, Germany, were contacted by personal letters using citizen registers provided by the municipality. Of importance, the letters already included the most important eligibility criteria (eg, LBP complaints). Three hundred fifty-one persons responded and were further assessed for eligibility. Subjects were included if they met the following criteria. 1) 40–70 years old; 2) characteristics of chronic LBP (50% in the last 3 months); 3) nonspecific LBP (eg, no orthopedic diagnosis; average numerical rating scale [NRS] ≥1); 4) no continuous or very frequent use of analgesics (>4 days/week); 5) no pharmacologic therapy or diseases affecting muscle metabolism (eg, glucocorticoids); 6) no conditions that prevent WB-EMS application (eg, epilepsy, cardiac pacemaker, thrombosis); and 7) absence of less than 2 weeks during the study period. Applying these criteria, 60 subjects (20 men, 40 women) were eligible and willing to participate in the study. Participants were randomly assigned to four intervention groups: WB-EMS (n=15), WB-Vibration (n=15), conventional training (n=15), and nonactive CG (n=15) stratified by age (40–55, 56–70). However, in this contribution we focus on the comparison of WB-EMS group vs nonactive CG (n=30; nine men, 21 women). gives the participant flow through the study. shows the baseline characteristics of the subjects of all groups.
Figure 1 Flow diagram of the study intervention.
Abbreviations: CG, control group; CT, conventional back exercises; ITT, intent-to-treat; n, numbers; TEP, total endoprosthesis; WB-EMS, whole-body electromyostimulation; WB-Vibra, whole-body vibration.
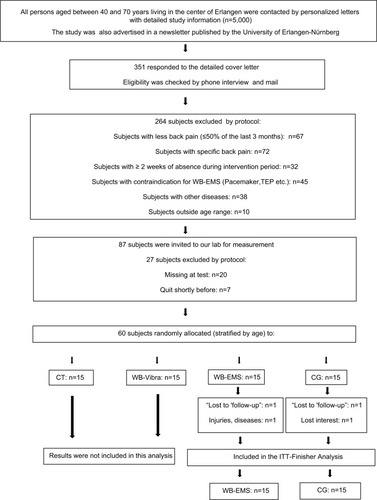
Table 1 Baseline characteristics of the WB-EMS group and control group
Intervention
We contrasted a 12-week WB-EMS application to a nonactive CG, without any further intervention. The intervention was conducted at the IMP, Erlangen, Germany, which is centrally located and can be easily reached by public transport. Certified trainers, who also recorded the participant’s attendance and compliance, supervised and guided all the sessions. Apart from the study intervention, all the participants were requested to maintain their usual lifestyle.
WB-EMS
WB-EMS enables the simultaneous activation of up to eight to ten muscle groups (upper legs, upper arm, bottom, abdomen, chest, lower back, upper back, latissimus dorsi, and two free options; total stimulation area 2,800 cm2) with regionally dedicated intensity.Citation13 We applied bipolar electric current with a frequency of 85 Hz, an impulse width of 350 µs, a rectangular mode and an interval of 6 seconds stimulation and 4 seconds of rest once a week for 20 minutes. During the stimulation phase, participants performed low-amplitude movements specifically dedicated to LBP (Box 1). The participants completed one to three sets with six repetitions of six easy movements in a minor range of motion (eg, dynamic squatting with knee ankle ≥120°) to keep the effect of the voluntary exercise itself as low as possible. Once a week four subjects underwent video-guided exercise under the supervision of two certified instructors using WB-EMS devices from miha bodytec (Gersthofen, Germany).Citation14
The intensity of the stimulation was regulated using the BORG CR 10 scale.Citation15 Subjects were requested to exercise at a rate of perceived exertion (RPE) between “hard (5)” and “very hard (7)”. In the first session current intensity was individually adapted in close interaction with the participants and saved to generate a fast and valid setting during the following sessions. The first four sessions’ time was increased from 12 to 20 minutes with a time rise of 2 minutes per session. During each session, instructors slightly increased the intensity every 2–3 minutes in close cooperation with the individuals. Research assistants regularly monitored compliance with the prescribed exercise intensity.
Control group
The CG was asked to maintain its usual lifestyle. Participants of this group were regularly contacted by phone and asked about their current status and lifestyle changes. To maintain compliance with the CG protocol, participants of the CG were offered random allocation to one of the intervention groups (WB-EMS, WB-Vibration, conventional back exercises) of the second study period.
Outcomes
Primary endpoint
Changes of average LBP intensity (4-week pain diary) from baseline to 12-week follow-up.
Secondary endpoint
Changes of maximum isometric trunk extension from baseline to 12-week follow-up.
Changes of maximum isometric trunk flexion from baseline to 12-week follow-up.
Testing procedures
The intervention took place between April 2017 and July 2017. Participants were assessed by the same research assistant at baseline and follow-up test at the same time of the day (±60 minutes).
Anthropometry
Height was determined barefoot to the nearest 0.1 cm with a stadiometer. Body mass and composition were determined through direct-segmental, multifrequency Bio-Impedance Analysis (DSM-BIA, InBody 770, Seoul, Korea). This device measures impedance of the trunk, arms, and legs separately using a tetrapolar eight-point tactile electrode system, which applies six frequencies between 1 and 1000 kHz. Participants were asked to avoid intense physical activity (eg, intensive endurance or resistance training) and to fast 3 hours prior to the assessments. Body mass index was calculated as body mass/body height (kg/m2).
Back pain diary and questionnaire
LBP intensity was monitored using a NRS from 0 (no pain) to 10 (worst possible pain) conducted 4 weeks before and during the last 4 weeks of the intervention.Citation16 For this, participants were provided with standardized questionnaires and were requested to rate their highest daily LBP intensity. The average 4-week LBP intensity before and during the last 4 weeks of the intervention was included in the analysis as the primary endpoint. In parallel, the maximum daily pain intensity during the 4-week periods was determined by the identical procedure. Apart from the NRS, other tools for back pain research (German pain questionnaire, chronic pain grade [GCPS], Roland and Morrison Disability Questionnaire [RMDQ]) were applied; however, during the present first project phase we refrained from the analysis of these assessments.Citation17–Citation19 To detect factors that may confound our results, baseline and follow-up questionnaires monitored diseases, medication, lifestyle (changes), and adverse events related or unrelated to the intervention. The same baseline questionnaire asked for demographic parameters, education, family and social status, physical activity, psychosocial factors, and exercise. Research assistants carefully checked the completeness and accuracy of the baseline and follow-up questionnaires together with the participants.
Functional testing
In view of the focus on LBP, the functional testing concentrated on maximum isometric strength of trunk flexion and extension (Back-Check 607, Dr Wolff, Arnsberg, Germany). For the exact positioning and procedure, the assistants followed the manufacturer’s recommendations. The adjustment of the devices was standardized for all patients. Patients were in a standing position (0°) with flexed knees (20°). Movement of the hip was fixed at the level of iliac crest back and front. For flexion, a pad was placed at the level of the sternum, while extension was measured at the scapula level. All patients completed each test three times; the highest result was included in the analysis. Applying this approach, reliability for maximum trunk extension (test–retest reliability; intra class correlation [ICC]) in this cohort was 0.88 (95% CI: 0.82–0.93). A slightly lower ICC (0.86 [95% CI: 0.81–0.90]) was determined for maximum trunk flexion.
Sample size
The sample size calculation of the study was based on the primary study endpoint “changes of LBP intensity”. Based on previous research, we expected a standardized mean difference (SMD) between the WB-EMS group and CG of 0.45±0.45 when applying the NRS 0–10 scale.Citation4,Citation20 Thus, at least 16 participants per group were required to generate α=0.05 and β–1=80%.
Randomization
Using age strata of 15 years (40–55, 46–70), eligible participants (n=30) were randomly assigned (1–1) to the study arms, WB-EMS and non-training CG (). By drawing lots, participants allocated themselves in the study groups. Lots were placed in opaque plastic shells and drawn from a bowl. Neither participants nor the researchers knew the allocation beforehand. After balanced (n=15/study arm) group allocation, the principal investigator (AW), responsible for the randomization process, instructed participants in detail about their status and corresponding dos and don’ts.
Blinding
Due to the inability to reliably blind participants, instructors, and primary researchers, we focused on blinding of the research assistants/outcome assessors concerning the group status of the participants. In other words, the outcome assessors were unaware whether subjects were allocated to the WB-EMS or CG and were not allowed to ask participants.
Statistical analyses
All the participants, who were randomly allocated, were included in the primary (intention to treat) analysis independent of compliance or loss to follow-up. R statistics software was used in combination with multiple imputation by Amelia II.Citation21 The full data set was used for multiple imputation, with imputation being repeated 100 times. Overimputation diagnostic plots confirmed that the multiple imputations worked well in all cases. Based on a statistically (Shapiro–Wilk test) and graphically (QQ- and box-plots) checked normal distribution of the primary and secondary outcomes presented here, dependent t-tests were used to analyze within-group changes. Welch two-sample t-test was applied to determine differences between the groups.Citation22 Chi-square tests were applied to detect difference in nominal scaled (baseline) data. Data were reported as mean value, SD, and 95% CI. All tests were two-tailed, and statistical significance was accepted at P <0.05. Effect sizes (ESs) were calculated using Cohen’s d.Citation23 ES ≥0.5 were considered as moderate; ES ≥0.8 were considered as high. SPSS 25.0 (SPSS Inc, Chicago, IL, USA) was used for statistical procedures for baseline data.
Results
With the exception of no regular exercises, no significant differences were observed for baseline characteristics between WB-EMS group and CG ().
Based on 30 subjects randomized, two subjects, one in each group, were lost to follow-up. One woman of the WB-EMS group quit the trial during the first two weeks of intervention because of health problems unrelated to the study. The reason for one person dropping out from the CG is not known. Attendance rate of WB-EMS group was high and averaged 93%±4%; only one participant missed more than one WB-EMS session. Participants appropriately complied with the exercise protocol. With respect to exercise intensity, participants reported exercising within the given stipulation of RPE 5–7 at Borg CR10 RPE with a significant increase (P=0.001) from 5.4±0.3 in week 4 to RPE 5.9±0.5 in week 12.Citation15 No adverse or unintended effects were observed during the WB-EMS session, and no participants reported any WB-EMS-related discomfort during or after WB-EMS application.
After 12 weeks of intervention, average daily LBP intensity monitored over 4 weeks (P=0.028) changed significantly more favorably in the WB-EMS, compared with the CG (ES: d=0.754). In detail, while pain intensity decreased significantly in the WB-EMS group (P=0.002), this parameter remained unchanged in the CG (P=0.730) ().
Table 2 Changes of primary and secondary study endpoints for the WB-EMS group and CG
The maximum isometric trunk extensor (ie, lower back extensor) strength increased significantly by 14.6%±18.6% in the WB-EMS group (P=0.005) and was maintained in the CG (–2.6%±18.9%, P=0.683). The corresponding intergroup difference was significant (P=0.038) with an ES that can be considered as “high”. On the other hand, the effect for maximum isometric trunk flexor strength did not reach significance (P=0.091). Within the WB-EMS group a significant increase of the maximum trunk flexion strength was determined (15.3%±17.8%, P=0.003), whereas no significant changes were observed in the CG (4.0%±17.3%, P=0.563).
No participant of the WB-EMS group or CG reported relevant changes of lifestyle including physical activity, exercise, diet, or general medication. However, the number of subjects with acute intake of analgesics was maintained in the CG (n=5) and decreased from three to one person in the WB-EMS group.
Discussion
The primary aim of this study was to demonstrate the effect in the WB-EMS group vs a nonactive CG on chronic nonspecific LBP. In summary, our findings clearly indicate a significant positive effect on LBP in this mixed cohort 40–70 years old. Less consistently, significant effects in the WB-EMS group were determined for maximum isometric trunk extension but not for maximum isometric trunk flexion.
To our best knowledge to date, no other evidence-based trials have addressed the issue of WB-EMS effects on chronic LBP. There are only two nonpublished master’s theses that evaluate the influence of WB-EMS on people with back-pain problems.Citation11,Citation12 Grützmacher (2003) reported a reduction of back pain in about 89% of the 49 participants after 6 weeks of 2×45 min/week WB-EMS (85 Hz; 350 µs; 4 seconds load – 2 seconds pause; bipolar). However, due to lack of a CG, weak statistical procedures, and vague study endpoints, the scientific evidence of this study is quite restricted. After 6 weeks of WB-EMS application with the identical stimulation protocol as described above, Vatter (2010) reported a 92.3% reduction of back pain in his WB-EMS group (n=119). Comparing the WB-EMS group with the CG (n=5), the author reported a significant positive effect of WB-EMS on back pain (P<0.001). Nevertheless, in both studies intervention groups are not clearly limited to participants with nonspecific LBP.Citation11,Citation12
Confirming the data of a recent meta-analysis (WB-EMS vs CG) of individual patient data, the SMD of −0.84 is slightly higher than in the present study (SMD: −0.75).Citation20 We attribute this difference predominantly to the different methodology of the studies. While the participants of the meta-analysis had to state their back pain retrospectively for the last week, the present study used a much more reliable 4-week pain diary. Further, the cohort of the present study was much more homogeneous (chronic, nonspecific, LS) with respect to LBP.
Comparing the study results with conventional exercise programs in the area of LBP, the average SMD reported by a recent meta-analysis (0.32) is below the effect of the present study.Citation4 Closer to WB-EMS training, strength and resistance training trials demonstrated an average SMD of 0.51; however, the results for the individual exercise trials vary considerably. Reviewing the most effective exercise studies, two of which applied strength and resistance exercise, and one a core stabilization protocol, they reported very impressive effects on chronic LBP.Citation24–Citation26 Both resistance exercise training protocols, a periodized whole-body strength training with free weights (16 weeks, 3 units/week, 12–15 exercises, three sets with 8–12 repetitions at 53%–72% 1 repetition maximum), and closely supervised, isolated back-extension exercise training on a specific back device (MEDX Lumbar Extension Machine, MedX, Ocala, Florida; one unit/week, one set with 80% 1 repetition maximum, full range of motion vs limited range of motion [50%]) resulted in nearly twice as high effects as the present study. However, the most striking effect (SMD: 2.27) came from a core stabilization program (4 weeks; 3 × 30 min/week).Citation26 Despite the high effects generated by these exercise studies, their exercise programs either required moderate–high training volume, or prescribed high exercise intensities. However, as discussed above, both aspects conflict with the lack of time and “kinesiophobia” of many participants with LBP.
Although we did not observe a difference between WB-EMS group and CG for maximum isometric trunk flexion, the significant changes of maximum isometric strength in the back (+14.6%±18.6%; P=0.005) and abdomen (+15.3%±17.8%, P=0.003) were impressive. Only a few studies with emphasis on LBP include a measurement of maximum trunk extensors and flexors and none of them applied a similar device (Dr Wolff Back-Check, Arnsberg, Germany), which renders a comparative discussion difficult. Including a comparable cohort, after 6 weeks of isolated lumbar extension resistance training, Steele et al generated an increase of isometric trunk extension up to 54%.Citation24 However, the training and test exercise were identical, and thus the results might be partially biased by a habituation effect. A similar isolated back-extension program conducted with active US soldiers without LBP (n=298) demonstrated an increase of 13.3% for isometric back-extension strength.Citation27 A study with conventional back exercises (stabilization vs dynamic; two sessions per week; 60 minutes; 8 weeks) reported back extension strength changes of between 16.3% and 48.5% (0°–72° lumbar flexion), whereby the stabilization group performed significantly better than the dynamic one.Citation28 However, with an average age of 28.5±4.9 years, the cohort is also much younger than in the present study, which may explain the difference in strength gain. A similar cohort (52.3±12.3 years) with LBP was measured after classical outpatient rehabilitation (ie, exercises, manual therapy, massage, and electrotherapy).Citation29 After 6 months of intervention, LS extension strength increased by 18.2%, while lumbar flexion rose by 16.7%. While these results were comparable to the present study, the time efficiency of this trial (42.6±2.3 sessions in 6 months) is much less favorable. Thus, although there might be exercise protocols similar or slightly more effective than our protocol, the comparative advantage of WB-EMS vs conventional exercise strategies is its time-effective, joint–friendly, and highly customized application. Further, by applying a minimum degree of common sense and the proper application of recently published WB-EMS guidelines, WB-EMS is a very safe exercise technology even eligible for multimorbid older people.Citation14,Citation30,Citation31
However, some limitations might decrease the scientific evidence and generalizability (ie, external validity) of our study results. 1) The sample size of 15 per group is slightly lower than that suggested by power analysis (n=16) based on a recent meta-analysis of individual patient data.Citation20 2) Although this LBP project focuses on a comprehensive evaluation of different types of exercise (WB-EMS vs WB-Vibration vs back-strengthening exercise), the sample size generated in the first study phase did not allow a meaningful statistical comparison of the treatment groups. 3) As mentioned above, average intensity (5.9 RPE) was reported at an average of between 5 “hard” and 7 “very hard”. Compared with other WB-EMS studies, a slightly lower intensity was specified in order to prevent possible “kinesiophobia” and a certain caution in electrical applications, especially in this critical group. To what extent this relatively low-intensity protocol optimally addresses chronical nonspecific back pain is still open to question and requires further studies. 4) In this study we determined a positive effect of WB-EMS on chronic nonspecific LBP in 40–70-year-old people with corresponding complaints. Thus, with respect to generalization, we conclude that our results are transferable to the majority of people with chronic nonspecific LBP. However, our results did not cover acute nonspecific LBP, which is still listed as a relative contraindication by the manufacturer (miha bodytec). In addition, the effects of WB-EMS on specific back pain are very difficult to grasp, as there are too many different causes with different responses to the electrical impulses. 5) Despite the specification to refrain from changes of lifestyle or physical activity habits during the intervention period, three participants of the CG started new treatments (acupuncture, osteopathy, and physical activity/exercise). However, no CG participant finished a complementary therapy. In contrast, no changes were reported by the WB-EMS group.
Conclusion
In summary, WB-EMS is a time-effective, safe, and joint-friendly option for people unable or unmotivated to exercise conventionally. Due to a supervised WB-EMS training, especially participants with “kinesiophobia” get an optimal support without being afraid of movement load. Due to the rather small sample size generated during the first study phase, emphasis of this contribution was placed on the comparison with a nonactive CG. By increasing the number of participants, our further research will focus on the comparison of WB-EMS with established training options for LBP (WB-Vibration, conventional back exercises).
Acknowledgments
This publication is part of the doctoral work for the title “Dr rer. biol. hum.”
Disclosure
The authors report no conflicts of interest in this work.
References
- GBD 2013 DALYs and HALE CollaboratorsMurrayCJBarberRMDalysGBDGlobal, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transitionLancet2015386100092145219126321261
- SchmidtCORaspeHPfingstenMBack pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional surveySpine200732182005201117700449
- AbrahamIKillackey-JonesBLack of evidence-based research for idiopathic low back pain: the importance of a specific diagnosisArch Intern Med2002162131442144412090876
- SearleASpinkMHoAChuterVExercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trialsClin Rehabil201529121155116725681408
- KorschSHerboldDWiezoreckMPromoting factors, barriers and barrier management to the implementation of health-promoting behavior among rehabilitative patients with chronic low back pain - a qualitative analysisRehabilitation201655421021627529297
- LüningBCLundbergMLindbergPElfvingBChange in kinesiophobia and its relation to activity limitation after multidisciplinary rehabilitation in patients with chronic back painDisabil Rehabil2012341085285822214399
- BoucherJAAbboudJDuboisJDLegaultEDescarreauxMHenchozYTrunk neuromuscular responses to a single whole-body vibration session in patients with chronic low back pain: a cross-sectional studyJ Manipulative Physiol Ther201336956457124156915
- IwamotoJTakedaTSatoYUzawaMEffect of whole-body vibration exercise on lumbar bone mineral density, bone turnover, and chronic back pain in post-menopausal osteoporotic women treated with alendronateAging Clin Exp Res200517215716315977465
- KaedingTSKarchASchwarzRWhole-body vibration training as a workplace-based sports activity for employees with chronic low-back painScand J Med Sci Sports201727122027203928185300
- del Pozo-CruzBHernández MocholíMAAdsuarJCParracaJAMuroIGusiNEffects of whole body vibration therapy on main outcome measures for chronic non-specific low back pain: a single-blind randomized controlled trialJ Rehabil Med201143868969421687923
- VatterJElektrische Muskelstimulation als Ganzkörpertraining - Multicenterstudie zum Einsatz von Ganzkörper-EMS im Fitness-StudioMünchenAVM-Verlag2010
- Boeckh-BehrensWGrützmacherNSebelefskyJElektromyostimulationstraining mit dem BodyTransformer - eine erfolgreiche Maßnahme zur Reduzierung von RückenbeschwerdenBayreuthInstitute of Sport Science2002
- KemmlerWvon StengelSWhole-body electromyostimulation as a means to impact muscle mass and abdominal body fat in lean, sedentary, older female adults: subanalysis of the TEST-III trialClin Interv Aging201381353136424130433
- KemmlerWFroehlichMvon StengelSKleinöderHWhole-body electromyostimulation – the need for common sense! Rationale and guideline for a safe and effective trainingDeutsche Zeitschrift für Sportmedizin2016201609218221
- BorgEKaijserLA comparison between three rating scales for perceived exertion and two different work testsScand J Med Sci Sports2006161576916430682
- von KorffMJensenMPKarolyPAssessing global pain severity by self-report in clinical and health services researchSpine200025243140315111124730
- KlasenBWHallnerDSchaubCWillburgerRHasenbringMValidation and reliability of the German version of the Chronic Pain Grade Questionnaire in primary care back pain patientsPsychosoc Med20041 Doc07
- CasserHRHüppeMKohlmannTGerman pain questionnaire and standardised documentation with the KEDOQ-Schmerz. A way for quality management in pain therapySchmerz201226216817522527646
- RolandMMorrisRA study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back painSpine1983821411446222486
- KemmlerWWeissenfelsABebenekMEffects of whole-body electromyostimulation on low back pain in people with chronic unspecific dorsal pain: a meta-analysis of individual patient data from randomized controlled WB-EMS trialsEvid Based Complement Alternat Med20172017848042929234437
- HonakerJKingGBlackwellMAmelia II: a program for missing dataJSS2011457147
- BarnardJRubinDBMiscellanea. Small-sample degrees of freedom with multiple imputationBiometrika1999864948955
- CohenJStatistical Power Analysis for the Behavioral Sciences2nd edHillsdale, NJLawrence Erlbaum Associates1988
- SteeleJBruce-LowSSmithDJessopDOsborneNA randomized controlled trial of limited range of motion lumbar extension exercise in chronic low back painSpine201338151245125223514876
- KellRTAsmundsonGJA comparison of two forms of periodized exercise rehabilitation programs in the management of chronic nonspecific low-back painJ Strength Cond Res200923251352319209082
- ChoHYKimEHKimJEffects of the CORE exercise program on pain and active range of motion in patients with chronic low back painJ Phys Ther Sci20142681237124025202188
- MayerJMChildsJDNeilsonBDChenHKoppenhaverSLQuillenWSEffect of lumbar progressive resistance exercise on lumbar muscular strength and core muscular endurance in soldiersMil Med201618111e1615e162227849497
- MoonHJChoiKHKimDHEffect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back painAnn Rehabil Med201337111011723525973
- AlfuthMWelsinkDWPain and functional outcomes after outpatient physiotherapy in patients with low back painOrthopade201746652252928204835
- KemmlerWTeschlerMWeissenfelsAWhole-body electro-myostimulation to fight sarcopenic obesity in community-dwelling older women at risk. Results of the randomized controlled FORMOsA-sarcopenic obesity studyOsteoporos Int201627113261327027289534
- KemmlerWWeissenfelsATeschlerMWhole-body electromyo-stimulation and protein supplementation favorably affect sarcopenic obesity in community-dwelling older men at risk: the randomized controlled FranSO studyClin Interv Aging2017121503151328989278
