Abstract
Background
General practitioners’ (GPs) views about deprescribing prescription opioid analgesics (POAs) may influence the care provided for patients experiencing chronic noncancer pain (CNCP). There are limited data addressing GPs’ beliefs about deprescribing, including their decisions to deprescribe different types of POAs.
Aim
To determine the proportion of GPs who hold attitudes congruent with local pain stewardship, describe their deprescribing decisions, and determine whether type of POA influences deprescribing.
Design and setting
In 2016, a cross-sectional survey of all GPs (n=1,570) in one mixed urban and regional primary health network (PHN) in Australia was undertaken.
Methods
A mailed self-report questionnaire assessed agreement with local guidelines for treating CNCP; influences on deprescribing POAs and likelihood of deprescribing in a hypothetical case involving either oral codeine or oxycodone.
Results
A response rate of 46% was achieved. Approximately half (54%) of GPs agreed POAs should be reserved for people with acute, cancer pain or palliative care and a third (32%) did not agree that a medication focus has limited benefits for peoples’ long-term quality of life and function. Most (77%) GPs were less likely to deprescribe when effective alternate treatments were lacking, while various patient factors (eg, fear of weaning) were reported to decrease the likelihood of deprescribing for 25% of GPs. A significantly higher proportion of GPs reported being very likely to deprescribe codeine compared to the equivalent opioid dose of oxycodone for a hypothetical patient.
Conclusions
Many GPs in the PHN hold attitudes at odds with local guidance that opioids are a nonsuperior treatment for CNCP. Attitudinal barriers to deprescribing include: a lack of consistent approach to deprescribing opioids as a class of drugs, perceived lack of effective treatment alternatives and patient fear of deprescribing. Therefore, the next step in this target population is to appropriately train and support GPs in how to apply the evidence in practice and how to support patients appropriately.
How this fits in
Calls to rethink opioid prescribing for people experiencing chronic noncancer pain (CNCP) have significant implications for general practitioners’ (GPs). This cross-sectional study shows wide variation in GP attitudes with consensus on deprescribing yet to be reached in the pain field. Given that chronic opioid therapy reduces functional recovery, a range of behavior change interventions to modify GP behaviors and support transitioning patients to more effective treatments in order to provide optimal outcomes for patients experiencing CNCP is warranted.
Background
In Australia, between 1990 and 2014 there was an almost fourfold rise in the dispensing of prescription opioid analgesics (POAs). This increase was driven largely by government subsidies for long-acting formulations used to manage pain for people experiencing CNCP, that is, pain lasting longer than 3 months.Citation1–Citation3 Almost 13% of the total Australian population are dispensed at least one government-subsidized POA each year.Citation4
Although there is some evidence worldwide that opioid harms have reached a plateau,Citation5 a substantial rise is evident in Australia in prescription opioid-related harms such as hospitalizations and accidental poisoning deaths.Citation6–Citation8 The available data do not distinguish whether use of illicit opioids or other substances may have contributed, however, the studies do link the rise in harms to an escalation in the use of prescription opioids made available under the government-subsidized system.Citation8 Beyond hospitalization and death, aberrant behavior and dependence are also problematic, particularly when people are younger and on higher prescribed doses.Citation9 Further, there is concern globally when people are coprescribed opioids in combination with benzodiazepines.Citation10,Citation11
Currently, there is evidence that opioids may provide modest short-term (less than 3 months) pain reduction along with minor improvement in physical function when compared with placebo.Citation12,Citation13 Over the longer term the current lack of robust evidence means that, from a clinical ethics perspective, prescribers need to balance a patient-centered approach with population based data that suggest increased harms when opioids are chronically prescribed.Citation14,Citation15
It is now accepted that POAs should not be a first-line treatment for people experiencing CNCP.Citation16 A recent pragmatic randomized controlled trial for chronic back and osteoarthritis-associated pain found that over 12 months treatment the reduction in pain scores was significantly less with opioids than nonopioid treatment. The study found that there were greater adverse events in the opioid arm and opioids brought no improvement in pain interference. Interestingly, the trial also found almost double the use of illicit drugs in the nonopioid arm. Furthermore, it is possible that study outcomes were affected by the limited options for individually titrated dosage in the opioid treatment arm.Citation17
If POAs are initiated in carefully selected patients, that is, those with no substance addiction history, an argument could be made in favor of limiting opioid therapy to a maximum of 3 months as opioid use beyond this time is likely to continue long term.Citation18,Citation19
Across the pain spectrum, widespread clinical variation in opioid prescribing exists.Citation20,Citation21 This variation continues with regard to opioid deprescribing in clinical practice and consensus guidelines. Currently, quality evidence for interventions aiming to reduce prescribed opioids is lacking, though nonrandomized studies indicate that switching to broader treatment approaches, including addressing mental health and physical functioning, may bring about reduction in opioid use.Citation22,Citation23
In practice, consideration of deprescribing after 3 months presents substantial challenges for patients experiencing CNCP and their prescribers.Citation24 Patients may hold concerns regarding opioid withdrawalCitation25 and some prescribers may believe that continuation of POAs poses minimal risk of harm.Citation26 Indeed, targeting early career GPs with teaching of current localized guidelines appears to have had little impact on their actual deprescribing decisions for this patient group.Citation27,Citation28 Currently, although Australian GPs are being urged to consider tapering regimes,Citation29 there is limited evidence about GP perceptions and practices that could be used to guide efforts to improve GPs’ deprescription rates. The available data suggest that GPs regularly face difficulties with patient requests or demands for ongoing opioid treatment.Citation20,Citation30 Further, perceived environmental barriers such as a lack of healthcare providers offering effective treatment alternatives are likely to have an impact on treatment choices.Citation31
In exploring GP perceptions about opioids for CNCP, it is important to consider the various types of opioids available. Low dose codeine (≤30 mg) has consistently been the most widely dispensed formulation in Australia.Citation3,Citation32,Citation33 Codeine is typically classed as a weak opioid or prodrug with its analgesic properties almost entirely attributed to its principal metabolite, morphine.Citation3,Citation34,Citation35 There is risk associated with the drug, however, relating largely to genetic variations which affect the rate at which people convert the prodrug to morphine, plus drug-drug interactions.Citation35,Citation36 This risk was recognized by the Australian Government Therapeutic Goods Administration when legislation passed in Feb 2018 for codeine to be upscheduled from over-the-counter to prescription only.Citation35,Citation37,Citation38 Oxycodone, classed as a strong opioid, is the second most highly dispensed POA in Australia with a substantial portion involving the long-acting formuation.Citation3,Citation4,Citation39 This shift toward a greater reliance on strong and long-acting opioids is relatively recent and has coincided with increased government subsidization.Citation40
It is important to know whether type of POA influences GPs deprescribing decisions, such that peer norms can be shifted via education, training and enablement interventions.Citation41
This study aimed to examine the perceptions and self-reported usual practice regarding POAs among a large urban and regional sample of Australian GPs. Specifically, the study aimed to identify:
The proportion of GPs who agreed with statements congruent with locally available guidelinesCitation27 for CNCP management, ie, POAs should be reserved for people experiencing acute pain, cancer pain, or palliative care; focusing on medication to reduce pain has limited benefits for people’s quality of life and function over the longer term; people who experience CNCP should be screened for depression or anxiety; and addressing sleep problems helps people cope better with their pain.
The proportion of GPs who report that particular factors (patient prefers to remain on opioids; patient expresses fear of weaning; patient has low score on quality of life measure or functional outcome measure; patient has poor psychological health; lack of availability of effective alternate treatment; lack of availability of access to or support from specialist care) influence their likelihood of deprescribing POAs.
Whether type of POA influenced GPs’ decision to deprescribe.
Methods
Study design and population
Between February and April 2016 we conducted a cross-sectional survey of GPs in one Australian primary health network (PHN) in the Hunter Central Coast region of NSW. This PHN is the second largest in NSW and 18.3% of the population is aged 65 years and over compared with 14.4% nationally. There are socioeconomically disadvantaged areas within the PHN with 30% of households experiencing rental stress (compared to 25% nationally); 14.4% experience mental and behavioral problems, which is similar to the national average (13.6%).Citation42
Study participants were GPs listed on the PHN register as at February 2016 with correct addresses.
Procedure
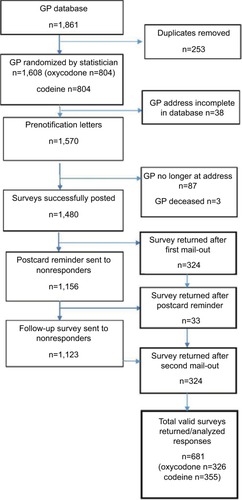
We recruited using a multi-step procedure as shown in .Citation43 After screening the PHN database for duplicates, remaining GPs were randomized. A further 38 duplicates were detected. A personalized prenotification letter introducing the survey and summarizing current best practice in pain management was sent in February 2016 to all GPs. The PHN produced a newsletter simultaneously with the prenotification mail-out. In March 2016, the first survey (n=1,570) pack was mailed and personally addressed to each individual GP. The pack contained a personalized cover letter, a paper copy of the questionnaire and details of the chance to win an AU$500 value sports watch plus a reply paid envelope. The sender was identified as the University of Newcastle and a respondent-friendly questionnaire design was used.Citation34,Citation44 A professionally designed postcard reminder was mailed to nonresponders 2 weeks after the initial mailing.Citation43,Citation45 A final mail-out of the survey pack was sent to all nonresponders 4 weeks after the prenotification letter. We considered return of the completed survey to imply consent to participate. The University of Newcastle Human Research Ethics Committee approved the study.
Study measures
A short study-specific questionnaire was developed by the authors and expert clinicians using current best evidence and key elements from locally available guidelines.Citation27 The guidelines were developed in 2014 and promoted via a portal available to local GPs known as HealthPathwaysCitation46 with links to key messaging videos on YouTube.Citation47 The pool of mutually exclusive attitudinal items described local stewardship in relation to opioid prescribing for CNCP and included four personal attitudes toward CNCP and six attitudinal statements toward deprescribing,Citation27 plus a hypothetical case study. The survey was pilot-tested with three GPs prior to administration to ensure accuracy and face validity with the target group and feasibility of questionnaire completion within 10 minutes. Only the items relevant to the study aims are described here.
GPs medical focus and willingness to prescribe POA was assessed by response to two statements: “opioid therapy should be reserved for people experiencing acute pain, cancer pain, or palliative care” and “focusing on medication to reduce pain has limited benefits for peoples’ quality of life and function over the long-term.”
GPs willingness to screen for underlying mental health comorbidity was assessed by response to two statements: “when caring for people who experience CNCP, screening for depression or anxiety is always important” and “addressing sleep problems help people cope better with their pain experience.”
Five response options for the four personal attitude statements were strongly disagree, disagree, neither agree nor disagree, agree, strongly agree.Citation48 Due to low responses in the “strongly agree” category the responses were collapsed into a three-point Likert scale with, “agree” and “strongly agree” responses aggregated into one category and “strongly disagree” and “disagree” categories were also aggregated. Neither agree nor disagree was maintained for symmetry in the response scale.
Deprescribing attitudes were assessed by response to six attitudinal statements. These statements focused on patient factors (four statements) and health system factors (two statements). Response options for these six statements were in the form of a three-point Likert scale (less likely to initiate wean, no influence on decision, more likely to initiate wean). We then asked respondents to choose which of the following options would encourage them most to deprescribe (lack of therapeutic response, ongoing request for opioids without accepting a broader based approach, other).
Hypothetical patient scenario
Each of the GPs was randomized to receive a case study involving either codeine or immediate release oxycodone of an equivalent oral morphine daily dose of 30 mg. The case study questioned respondents regarding their likelihood to deprescribe opioids to cessation (after 12 months) for a 32-year-old male with the following clinical and psychosocial background: unemployed laborer, chronic shoulder pain, all potentially relevant medical interventions ruled out, attending early for repeat script of opioids, describing his current week as “really tough” eg, medications “taking edge off ” only and not reaching his physical or functional treatment goals. Responses were given on a five-point Likert scale (very unlikely, unlikely, neither likely nor unlikely, likely, and very likely).
Sample size
A priori power analysis was conducted to determine a sufficient sample size for the study. It was calculated that a total sample size of 500 GPs was required to estimate proportions with a margin of error of 4% and maintain a type I error rate of 5% and a type II error rate of 20% (80% power)
Statistical analysis
Data were entered and analyzed using STATA Version 14. A sample of 30 surveys was randomly selected to check data quality. There were four errors detected from 720 questions representing a 0.6% data entry error rate (three skipped entry and one incorrect entry) which is below the benchmark of 1%.
We used descriptive statistics (frequencies and percentages with 95% CI) to report the attitudes of the GPs. Chi-squared test was used to compare the observed and expected number of responses to the case study and the type of opioid used in the case study.
Ethics approval
This study received ethics approval from Hunter New England Health and University of Newcastle Human Research Ethics Committees. HNEHREC reference no: 15/10/21/5.01 NSW HREC Reference No: LNR/15/HNE/371 SSA reference no: LNRSSA/15/HNE/372.
Results
Sample
Of 1,570 questionnaires that were mailed, 1,480 were delivered successfully and 681 were returned completed. There were 90 undeliverable surveys, 87 were due to the GP no longer working at, or having retired from, the practice with three returned due to the GP being deceased. The total valid adjusted response rate was thus 46%. No significant gender differences between responders and nonresponders were found.
Of those that responded, 57% were male and 58% had graduated prior to 1995. The majority of the responders’ practices had practice nurses (92%) and worked in practices with between five and ten full-time equivalent GPs (44 %). Half of the GPs indicated that 5%–10% of their casework involved CNCP and only 3% indicated they had never referred a patient to a tertiary pain service.
Local CNCP pain stewardship
Proportions are reported for each item (). Approximately half (54%) of GPs agreed POAs should be reserved for people with acute pain, cancer pain or needing palliative care as per local guidelines. Approximately one third (32%) did not agree that a medication focus has limited benefits for peoples’ long-term quality of life and function.
Table 1 GPs’ agreement with managing patients experiencing CNCP (n=681)
Deprescribing decisions
describes the reported likelihood of GPs deprescribing opioids for patients with CNCP under various circumstances. More than three quarters (77%) of GPs reported that a lack of effective alternate treatment would make them less likely to initiate a weaning regime. Over one third of GPs would be more likely to deprescribe if the patient had poor psychological health. An ongoing request for opioids was the biggest factor influencing GPs decision to wean the patient off opioids (44%), followed by a lack of therapeutic response 40% (data not shown).
Table 2 Reported likelihood to deprescribe opioid dose to cessation in relation to various patient and resource factors (n=681)
Opioid type
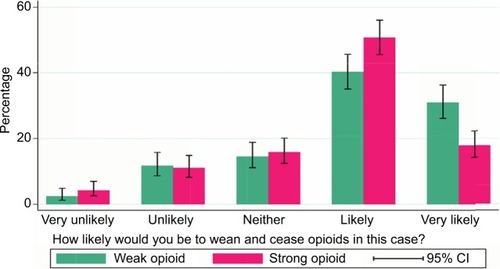
As shown in , there was a significant difference in GPs responses between case studies received (chisquare=17.87, df=4, P=0.001). A higher proportion of GPs who received the codeine case study indicated they were “very likely” to wean the patient off opioids (31%) compared to GPs who received a case study involving oxycodone (18%).
Discussion
Summary of main findings
Australian GPs have been tasked with initiating opioid deprescribing for patients experiencing CNCP after 3 months, avoiding the creation of a future generation of long-term opioid users. We found that only half the GPs surveyed endorsed the idea of reserving opioid use for acute and cancer pain; and a third did not agree that a medication focus had limited benefits.Citation27,Citation28 Our findings are consistent with those from overseas showing that prescribers’ attitudes and prescribing habits vary widely.Citation49 This wide clinical variation in the pain field relates in part at least to provider factors.Citation50 Further education, training and enablement for providers may assist GPs to restructure their practice and modify their prescribing behaviors in line with local guidance, thereby reducing variations in clinical care.Citation41,Citation51,Citation52
There was strong agreement with the idea of promoting quality sleep and screening for depression. The wider literature is clear on the value of addressing sleep problems.Citation53 Although the link between POAs and depression is well supported,Citation54,Citation55 the specific risk associated with codeine prescriptions has only recently been highlighted.Citation56 In contrast, a recent trial in the UK has cast doubt on the usefulness of screening for depression and anxiety, at least in patients presenting to their GP with osteoarthritis.Citation57 It is possible that screening, in the context of more holistic care is effective, this is an area to be explored.
This study showed that patient preference to stay on opioids or patient fear of the process or outcome of weaning impacts heavily on the GPs’ decision to deprescribe. With Australian data suggesting that two out of three people attempting suicide have chronic pain, this risk may contribute further to a reluctance to deprescribe.Citation58 Current evidence suggests guiding suicidal patients toward nonaddictive alternatives and linking patients with mental health supportCitation59 to reduce risk and attain clinical improvement.Citation59,Citation60
Our data showed that GPs’ attitudes vary widely on whether low quality of life measures or poor psychological health influence their decisions to initiate weaning. Practitioners have been urged to examine effects on psychosocial functioning of the select group of patients remaining on long-term opioids.Citation61 While opioid deprescribing may seem logical when patients have poor function and unremitting pain, a rise in aberrant behavior and misuse while tapering is a complex area with little current guidance available.Citation62 We did not explore whether GPs had different attitudes for an older patient requiring “comfort care” compared to a younger person with potential for functional recovery and return to work, though this may have been a factor.Citation63
Arguably, the biggest barrier identified to initiating deprescribing was a perceived lack of effective alternate treatment. While tertiary specialist pain centers are capable of delivering high-quality psychosocial pain care, GPs clearly want access to more accessible evidence based options in primary care.Citation51 Conversely, we showed that a patient actively requesting more opioids was a key factor influencing the GPs’ decision to initiate deprescribing. This may reflect that GPs are aware of guidance to routinely screen for signs of aberrant behavior and are more confident in deprescribing in this patient cohort.Citation27,Citation64
Australian GPs continue to prescribe multiple types of POAs in primary care settings.Citation65 Our data suggest that the majority of GPs favored cessation of opioids in a hypothetical case. While this is good news, management of a hypothetical case does not necessarily correlate with deprescribing in actual practice.Citation66
Study limitations
The response rate to our survey, while low, compares favor-ably to other surveys of primary care practitioners.Citation67,Citation68 The sample size may result in reduced precision in the study data. Study findings may not be generalizable to nonGP prescribers or GPs in more rural and remote areas.Citation69
Respondents may differ from nonrespondents (response bias) such that GPs more interested in pain management may be more likely to return the survey questionnaire than other GPs. Response bias may result in the data providing a more favorable picture of GPs’ perceptions and practices than is actually the case. While such testing is rare for this type of survey, it is possible that survey responses may not provide a precise estimate of participants’ true views. However, given the dearth of evidence available on this topic and the lack of a strong alternative methodology for obtaining this information the data gathered represent a significant advance on what is currently available for the purposes of service planning and delivery. We did not examine the attitudes of GPs regarding substance use disorder, where the attitudes of GPs toward initiation of deprescribing are less ambiguous.Citation70 Finally, we did not examine the influence of patient characteristics or satisfaction levels on prescribing patterns.Citation71,Citation72
Implications for clinical practice and future research
GPs in the surveyed region have been widely encouraged to deprescribe POAs whenever a patient is encountered who has been taking POAs for longer than 3 months.Citation24 The results of this survey suggest that a large proportion of GPs are not following the evidence base about POAs and locally promoted opioid stewardship.Citation73 This finding lends weight to the view that this complex problem would be better managed from a coordinated regulatory and broad societal perspective.Citation74,Citation75
One option to counter decades of often-misleading pharmaceutical company marketing promotion could be a strong education campaign similar to the Victorian (Australia) back pain campaign in the late 1990s.Citation76 Such a population-based campaign would target both patients and providers and promote key messages around the harms and lack of efficacy of long-term opioid use.
Conclusion
In the short term, however, it is our view that there is a clear need to train and support GPs by assisting them to shift toward potentially more effective psychological or behavioral treatments for patients experiencing CNCP. Competent and compassionate GPs who have learnt to view less liberal opioid prescribing as the new norm will benefit from ready access to viable alternatives in order to confidently proceed with the transition to broader treatments. Training GPs in how to support patients who express fear of the deprescribing process is also likely to be an important element of effective training programs.
Acknowledgments
The authors thank the Hunter New England PHN who supported the survey, GPs who returned the survey, and Sandra Dowley for data management. RW is supported by funding from the Ann Taylor Scholarship. CLP is supported by an NHMRC Career Development Fellowship. AB is supported by Early Career Fellowships from the National Health and Medical Research Council (APP1073317) and Cancer Institute New South Wales (13/ECF/1-37). These funding bodies had no role in determining the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
- MerskeyHBogdukNClassification of Chronic Pain Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms2nd edSeattle, WAIASP Press1994
- International Association for the Study of Pain Subcommittee on TaxonomyInternational Association for the Study of Pain. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Merskey H, editorPain1986Suppl 3S1S2253461421
- KarangesEABlanchBBuckleyNAPearsonSATwenty-five years of prescription opioid use in Australia: a whole-of-population analysis using pharmaceutical claimsBr J Clin Pharmacol201682125526726991673
- GisevNPearsonSABlanchBInitiation of strong prescription opioids in Australia: cohort characteristics and factors associated with the type of opioid initiatedBr J Clin Pharmacol20168241123113327260937
- DartRCSurrattHLCiceroTJTrends in opioid analgesic abuse and mortality in the United StatesN Engl J Med2015372324124825587948
- KarangesEABuckleyNAPearsonSAThe rise and rise of prescription opioid use in AustraliaMed Today2017Suppl 227
- MillerGCValentiLBrittHBayramCDrugs causing adverse events in patients aged 45 or older: a randomised survey of Australian general practice patientsBMJ Open2013310e003701
- BlanchBPearsonSAHaberPSAn overview of the patterns of prescription opioid use, costs and related harms in AustraliaBr J Clin Pharmacol20147851159116624962372
- CampbellGNielsenSLaranceBPharmaceutical opioid use and dependence among people living with chronic pain: associations observed within the pain and opioids in treatment (POINT) cohortPain Med20151691745175826011277
- HawkinsEJMalteCAHagedornHJSurvey of primary care and mental health prescribers’ perspectives on reducing opioid and benzodiazepine co-prescribing among veteransPain Med201718345446727558857
- DegenhardtLBlanchBGisevNLaranceBPearsonSThe POPPY Research programme protocol: investigating opioid utilisation, costs and patterns of extramedical use in AustraliaBMJ Open20154e007030
- MeskeDSLawalODElderHLangbergVPaillardFKatzNEfficacy of opioids versus placebo in chronic pain: a systematic review and meta-analysis of enriched enrollment randomized withdrawal trials201811923934
- ChaparroLEFurlanADDeshpandeAMailis-GagnonAAtlasSTurkDCOpioids compared to placebo or other treatments for chronic low back pain: an update of the Cochrane ReviewSpine201439755656324480962
- CohenMJJangroWCA clinical ethics approach to opioid treatment of chronic noncancer painAMA J Ethics201517652152926075979
- MartinBCFanMYEdlundMJDevriesABradenJBSullivanMDLong-term chronic opioid therapy discontinuation rates from the TROUP studyJ Gen Intern Med201126121450145721751058
- ChouRTurnerJADevineEBThe effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention WorkshopAnn Intern Med2015162427628625581257
- KrebsEEGravelyANugentSEffect of Opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE Randomized Clinical TrialJAMA2018319987288229509867
- EdlundMJSteffickDHudsonTHarrisKMSullivanMRisk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer painPain2007129335536217449178
- Von KorffMKorffMVSaundersKDe facto long-term opioid therapy for noncancer painClin J Pain200824652152718574361
- EidAIDepesaCNordestgaardATVariation of opioid prescribing patterns among patients undergoing similar surgery on the same acute care surgery service of the same institution: time for standardization?Surgery2018164592693030049481
- Australian Commission on Safety and Quality in Health Care and National Health Performance AuthorityAustralian Atlas of Healthcare VariationSydneyACSQHC2015
- EcclestonCFisherEThomasKHInterventions for the reduction of prescribed opioid use in chronic non-cancer painCochrane Database Syst Rev201711CD01032329130474
- DemirkolATapering off opioid analgesiaMed Today2017Suppl 21416
- HayesCChronic noncancer pain. The challenge of implementing opioid guidelinesPain Manag Today2017422730
- KiepekNHancockLToppoziniDCromartyHMorganAKellyLFacilitating medical withdrawal from opiates in rural OntarioRural Remote Health2012121922624570
- HutchinsonKMorelandAMde C WilliamsACWeinmanJHorneRExploring beliefs and practice of opioid prescribing for persistent non-cancer pain by general practitionersEur J Pain2007111939816487734
- Hunter Integrated Pain ServiceReconsidering opioid therapy. A Hunter New England Perspective52014 Available from: http://www.hnehealth.nsw.gov.au/Pain/Documents/Reconsidering_opioid_therapy_May%202014.pdfAccessed December 20, 2018
- HollidaySMHayesCDunlopAJDoes brief chronic pain management education change opioid prescribing rates? A pragmatic trial in Australian early-career general practitionersPain2017158227828828092648
- DemirkolATapering off opioid analgesiaMed Today20171Supp 21416
- LeCDMedicineGBanksEDeprescribingAust Prescr201134647
- CaseyDEWhy don’t physicians (and patients) consistently follow clinical practice guidelines?JAMA Intern Med2013173171581158323897435
- RogersKDKempAMcLachlanAJBlythFAdverse selection? A multi-dimensional profile of people dispensed opioid analgesics for persistent non-cancer painPLoS One2013812e8009524312456
- HarrisonCMCharlesJHendersonJBrittHOpioid prescribing in Australian general practiceMed J Aust2012196638038122471532
- RoxburghAHallWDBurnsLTrends and characteristics of accidental and intentional codeine overdose deaths in AustraliaMed J Aust2015203729926424067
- MacDonaldNMacLeodSMHas the time come to phase out codeine?CMAJ201018217182520921244
- IedemaJCautions with codeineAust Prescr2011345133135
- NielsenSTobinCDobbinMOTC codeine: examining the evidence for and againstAust Pharm2012236240
- Australian GovernmentPrescription strong (Schedule 8) opioid use and misuse in Australia – options for a regulatory responseConsultation paper. Version 1.012018 Available from: https://www.tga.gov.au/sites/default/files/consultation-prescription-strong-schedule-8-opiod-use-misuse-in-australia-options-for-regulatory-response.pdfAccessed December 7, 2018
- DegenhardtLGisevNCamaENielsenSLaranceBBrunoRThe extent and correlates of community-based pharmaceutical opioid utilisation in AustraliaPharmacoepidemiol Drug Saf201625552153826781123
- HollingworthSASymonsMKhatunMPrescribing databases can be used to monitor trends in opioid analgesic prescribing in AustraliaAust N Z J Public Health201337213213823551471
- ChauhanBFJeyaramanMMannASBehavior change interventions and policies influencing primary healthcare professionals’ practice-an overview of reviewsImplement Sci2017121328057024
- Hunter NewEnglandCentral CoastPHNHealth Planning CompassHeal Plan Perform Portf2016136 Available from: http://www.hnec-cphn.com.au/media/14230/compass-jun-16-final-002.pdfAccessed August 13, 2017
- EdwardsPJRobertsIClarkeMJMethods to increase response to postal and electronic questionnairesCochrane Database Syst Rev2009183MR000008
- GlidewellLThomasRMaclennanGDo incentives, reminders or reduced burden improve healthcare professional response rates in postal questionnaires? Two randomised controlled trialsBMC Health Serv Res20121225022891875
- Hunter Integrated Pain ServiceUnderstanding pain: what to do about it in less than five minutes?YouTube2011 Available from: https://www.youtube.com/watch?v=5KrUL8tOaQsAccessed December 7, 2018
- NSW GovernmentCommunity HealthPathwaysHunter New England Available from: hne.healthpathways.org.auAccessed October 15, 2017
- WhiteRHayesCWhiteSHodsonFJUsing social media to challenge unwarranted clinical variation in the treatment of chronic noncancer pain: the “Brainman” storyJ Pain Res2016970170927703395
- HIPSHunter Integrated Pain Service (HIPS) Website2013 Available from: http://www.hnehealth.nsw.gov.au/painAccessed December 7, 2018
- WightmanRSNelsonLSOpioid prescribing: how well do we know ourselves?J Med Toxicol201612322122327492362
- DugganAKoffEMarshallVClinical variation: why it mattersMed J Aust2016205103427362671
- SlaterHDaviesSJParsonsRQuintnerJLSchugSAA policy-into-practice intervention to increase the uptake of evidence-based management of low back pain in primary care: a prospective cohort studyPLoS One201275e38037:11322662264
- WindmillJFisherEEcclestonCInterventions for the reduction of prescribed opioid use in chronic non-cancer painCochrane Database Syst Rev20139CD010323
- WiltJADavinSSchemanJA multilevel path model analysis of the relations between sleep, pain, and pain catastrophizing in chronic pain rehabilitation patientsScand J Pain2016201610122129
- KroenkeKA practical and evidence-based approach to common symptoms: a narrative reviewAnn Intern Med2014161857958625329205
- ParchmanMLVon KorffMBaldwinLMPrimary care clinic re-design for prescription opioid managementJ Am Board Fam Med2017301445128062816
- ScherrerJFSalasJBucholzKKNew depression diagnosis following prescription of codeine, hydrocodone or oxycodonePharmacoepidemiol Drug Saf201625556056827004714
- MallenCDNichollBILewisMThe effects of implementing a point-of-care electronic template to prompt routine anxiety and depression screening in patients consulting for osteoarthritis (the Primary Care Osteoarthritis Trial): a cluster randomised trial in primary carePLoS Med2017144e10022732328399129
- CampbellGDarkeSBrunoRDegenhardtLThe prevalence and correlates of chronic pain and suicidality in a nationally representative sampleAust N Z J Psychiatry201549980381125698809
- BernaCKulichRJRathmellJPTapering long-term opioid therapy in chronic noncancer pain: evidence and recommendations for everyday practiceMayo Clin Proc201590682884226046416
- ElmanIBorsookDVolkowNDPain and suicidality: insights from reward and addiction neuroscienceProg Neurobiol201310912723827972
- JankeEACheatleMKeefeFJDhingraLSociety of Behavioral Medicine Health Policy CommitteeSociety of Behavioral Medicine (SBM) position statement: improving access to psychosocial care for individuals with persistent pain: supporting the National Pain Strategy’s call for interdisciplinary pain careTransl Behav Med20188230530829385551
- ManhapraAAriasAJBallantyneJCThe conundrum of opioid tapering in long-term opioid therapy for chronic pain: a commentarySubst Abus2017221110
- BallantyneJCOpioids for the treatment of chronic pain: mistakes made, lessons learned, and future directionsAnesth Analg201712551769177829049121
- HollidaySHayesCDunlopAOpioid use in chronic non-cancer pain-part 2: prescribing issues and alternativesAust Fam Physician201342310411123529518
- RoxburghAHallWDDobbinsTTrends in heroin and pharmaceutical opioid overdose deaths in AustraliaDrug Alcohol Depend201717929129828826104
- HollidaySMHayesCDunlopAJDoes brief chronic pain management education change opioid prescribing rates? A pragmatic trial in Australian early-career general practitionersPain2017158227828828092648
- CohenMMPenmanSPirottaMDa CostaCThe integration of complementary therapies in Australian general practice: results of a national surveyJ Altern Complement Med2005116995100416398590
- ParkinsonAJormLDouglasKARecruiting general practitioners for surveys: reflections on the difficulties and some lessons learnedAust J Prim Health201521225425824581281
- BriggsAMSlaterHBunzliSConsumers’ experiences of back pain in rural Western Australia: access to information and services, and self-management behavioursBMC Health Serv Res201212135723057669
- LovejoyTIMorascoBJDemidenkoMIMeathTHFrankJWDob-schaSKReasons for discontinuation of long-term opioid therapy in patients with and without substance use disordersPain2017158352653428192376
- FoyRLeamanBMcCrorieCPrescribed opioids in primary care: cross-sectional and longitudinal analyses of influence of patient and practice characteristicsBMJ Open201665e010276e010276
- OnishiEKobayashiTDexterEMarinoMMaenoTDeyoRAComparison of opioid prescribing patterns in the United States and Japan:primary care physicians’ attitudes and perceptionsJ Am Board Fam Med201730224825428379832
- MccrackenLMBoichatCEcclestonCTraining for general practitioners in opioid prescribing for chronic pain based on practice guidelines: a randomized pilot and feasibility trialJ Pain2012131324022112421
- DasguptaNBeletskyLCiccaroneDOpioid crisis: no easy fix to its social and economic determinantsAm J Public Health2018108218218629267060
- LaranceBDegenhardtLPeacockAPharmaceutical opioid use and harm in Australia: the need for proactive and preventative responsesDrug Alcohol Rev201837Suppl 1S203S20529024092
- BuchbinderRJolleyDWyattM2001 Volvo Award Winner in Clinical Studies: Effects of a media campaign on back pain beliefs and its potential influence on management of low back pain in general practiceSpine200126232535254211725233