Abstract
Purpose
Fibromyalgia (FM) can cause chronic widespread pain and seriously affect the quality of patient lives. Acupuncture therapy is widely used for pain management. However, the effect of acupuncture on FM is still uncertain. The aim of this review was to determine the effect and safety of acupuncture therapy on the pain intensity and quality of life in patients with FM.
Materials and methods
We searched PubMed, the Cochrane Library, Embase, the China National Knowledge Infrastructure, the Chinese Science and Technology Periodical Database, and the Chinese Biomedical Literature Database to collect randomized controlled trials (RCTs) of acupuncture for FM published before May 2018. A meta-analysis was performed according to the Cochrane systematic review method by using RevMan 5.3 software, and GRADE was used to evaluate the quality of the evidence.
Results
We identified 12 RCTs that compared acupuncture therapy to sham acupuncture or conventional medication. Meta-analysis showed that acupuncture was significantly better than sham acupuncture for relieving pain (MD =−1.04, 95% CI [−1.70, –0.38], P=0.002, I2=78%) and improving the quality of life (MD =−13.39, 95% CI [−21.69, –5.10], P=0.002, I2=82%), with low- to moderate-quality evidence in the short term. At follow-up in the long term, the effect of acupuncture was also superior to that of sham acupuncture. No serious adverse events were found during acupuncture.
Conclusion
Acupuncture therapy is an effective and safe treatment for patients with FM, and this treatment can be recommended for the management of FM.
Introduction
Fibromyalgia (FM) is characterized by widespread musculoskeletal pain,Citation1 is present in as much as 0.4% to 9.3% of the population,Citation2 and is often accompanied by fatigue, sleep difficulties, cognitive dysfunction, depressed mood, or depressive episodes.Citation3,Citation4 FM can occur in all populations at every age, especially involving more middle-aged females than males.Citation5 A recent study reported that the annual medical cost of FM was more than 12,993 million euros (32.5% corresponded to health care costs and 67.5% to indirect costs attributable to productivity losses) in Spain.Citation6 Therefore, it is imperative to find effective therapies relieving pain and reducing social and economic burden.
The management of FM requires a multidimensional approach that includes patient education, behavioral therapy, exercise, and pain management.Citation7 Unfortunately, no effective treatments for FM are presently available. The most common pharmacological therapies for the pain management of FM include amitriptyline, anticonvulsants, and serotonin noradrenaline reuptake inhibitors,Citation8 or their combination.Citation9 However, recent European guideline indicates that the effect size for most treatments is relatively modest and that all pharmacological therapies are only weak recommendations for FM.Citation10 Moreover, the guideline suggests that initial management should focus on nonpharmacological therapies.Citation10
There are different types of nonpharmacological interventions for FM. Acupuncture therapy is a significant component of nonpharmacological therapies. Modern medical researches indicate that the analgesic effects of acupuncture are known to activate peripheral and central pain control systems by releasing various endogenous opioids or nonopioid compounds, such as beta-endorphins, enkephalins, dynorphins, serotonin, norepinephrine, gamma-aminobutyric acid, or ATP.Citation11–Citation13 Excitingly, clinical studies of acupuncture therapy for FM showed promising results that acupuncture is effective in relieving symptoms of FM.Citation14 However, the available systematic reviews published a few years ago indicated that there was no sufficient evidence to confirm the efficacy of acupuncture therapy for FM, mainly due to the small number of studies.Citation15–Citation17 Therefore, more randomized controlled trials (RCTs) were conducted to address this issue after demonstrating controversial results,Citation18–Citation20 which prompted us to conduct a meta-analysis of these primary studies to generate the pooled treatment effect of acupuncture on FM and offer suggestions for future studies and treatments.
Materials and methods
Protocol and registration
The protocol registration number is PROSPERO 2018 CRD42018094636 and is available at http://www.crd.york. ac.uk/PROSPERO/display_record.php?ID=CRD42018094636. This review was reported in compliance with the PRISMA statement.Citation21
Search strategy
We searched for RCTs in the following electronic databases, without language restriction, from their inceptions until May 2018: PubMed, the Cochrane Library, Embase, the China National Knowledge Infrastructure, the Chinese Science and Technology Periodical Database, and the Chinese Biomedical Literature Database. The search words were fibro-myalgia (eg, fibromyalgia, fibrositis, fibromyositis, and FM) and acupuncture (eg, acupuncture, acupressure, acupoint, electroacupuncture, and electro-acupuncture [EA]). In addition, all the available reviews related to FM treatments were manually checked for any additional possibly relevant RCTs.
Inclusion and exclusion criteria
Types of studies: Only RCTs of acupuncture therapy for FM were included. Observational studies, cross-over studies, animal studies, conference abstracts, and letters were excluded, and the sample size of every study must be more than ten patients. The studies of unavailable data were excluded. There were no language restrictions.
Types of participants: Participants with FM must be diagnosed with a standard description of the diagnostic criteria (1990 American College of Rheumatology criteria).Citation22 There are no limits to the age, gender, race, condition, duration, or intensity of the research subjects.
Types of interventions: Acupuncture therapy only included manual acupuncture and EA, regardless of different acupoints or needle materials. However, dry needling not based on traditional Chinese medicine (TCM) theory was excluded. Acupoint injections, laser acupuncture, moxibustion, cupping, herbal medicine, and any combination of the above were excluded. In addition, studies that compared different acupuncture therapies were also excluded.
Types of control groups: Sham acupuncture or conventional pharmacological therapies will be included. There were two types of sham acupuncture: a needling insertion into nonacupoints or ~1–2 cm from acupoints and nonpenetration by a blunt or retractable needle that contacts the skin without inserting the needle. Conventional pharmacological therapies do not contain herbal medicine.
Types of outcome measures: The primary outcome measures include a change in pain intensity and quality of life. The change in pain intensity was measured by using a VAS, a numerical rating scale (NRS), the Multidimensional Pain Inventory (MPI), or the McGill Pain Questionnaire (MPQ). Quality of life was evaluated using the fibromyalgia impact questionnaire (FIQ). The secondary outcome was an adverse event of acupuncture therapy to assess acupuncture safety.
Study selection and data extraction
According to the search strategy, one author (XCZ) performed the searches. Two investigators (XCZ and HC) reviewed the titles and abstracts of the references and screened eligible studies according to inclusion and exclusion criteria. Then, we downloaded the full text of the eligible studies to determine the final selection.
Two authors (XCZ and HC) independently extracted data from each study using a predesigned form. The information extracted included study design, patient characteristics, sample size, diagnostic criteria, interventions, treatment sessions, clinical outcome results, follow-up period, and adverse events. If there were any unclear or missed data, we attempted to contact authors for the details by phone or email. If we could not obtain access to the data by contacting the authors, then we would exclude the studies. Any disagreements were resolved by rechecking the primary papers and further consultation with the third author (WTX).
Assessment of risk of bias
Two independent investigators (XCZ and HC) evaluated the risk of bias (ROB) in each included trial according to the Cochrane risk of bias assessment tool. This tool contains seven items of ROB: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias.Citation23 For each item, ROB was graded as high, low, or unclear. Discrepancies were resolved by further discussion with the third author (WTX).
Quality of evidence
For each comparison in the meta-analysis, we assessed the quality of evidence by using the Grading of Recommendations assessment, Development and Evaluation (GRADE) Guideline Development Tool (GRADEpro GDT, https://gradepro.org/).Citation24 In this online system, the quality of RCTs was initially graded as high and then downgraded as moderate, low, or very low because of any limitations with respect to ROB, inconsistency, indirectness, imprecision, or publication bias. Two authors (XCZ and HC) independently evaluated the quality of evidence according to the GRADE handbook,Citation25 and consensus was adapted to resolve any disagreement.
Statistical analyses
The meta-analysis was performed using RevMan 5.3 software provided by the Cochrane Collaboration. Continuous outcomes were calculated with mean difference (MD) and 95% CI. Dichotomous outcomes were calculated with the risk ratio (RR) and 95% CI. The overall effect was evaluated by the Z test, and a P-value of <0.05 was considered statistically significant. Considering the clinical heterogeneity of different acupuncture therapies, we performed subgroup analysis based on EA and manual acupuncture (MA). Statistical heterogeneity between studies was quantified by the I2 statistic. In accordance with the Cochrane Handbook for Systematic Reviews of Interventions (version 5.10), we defined I2 >50% as representing substantial heterogeneity, and the random effects model was used for meta-analysis.Citation23
Statistical analyses
Sensitivity analyses were performed to explore potential sources of heterogeneity. Publication bias was estimated by funnel plot analysis if sufficient studies were included.
Results
Study selection
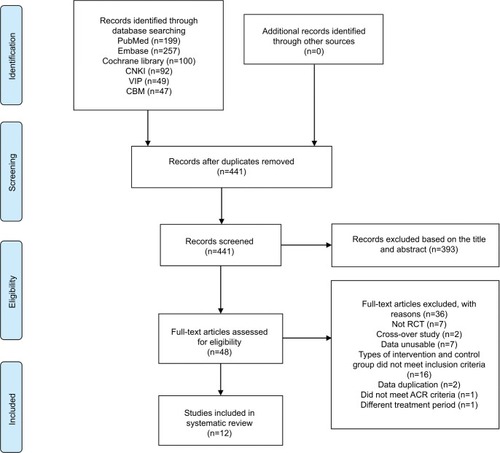
A total of 744 studies were identified from all the initial searches; 441 studies were retained after screening and removing duplications, and 393 studies were excluded according to the title and abstract. Then, 48 full-text studies were further assessed for eligibility. Of these, 36 studies were excluded because of not RCTs, inappropriate intervention, data duplication, or data unusable (). Finally, 12 RCTsCitation14,Citation18–Citation20,Citation26–Citation33 were eligible and included in the systematic review. The flow chart of the study selection process is shown in .
Description of the included studies
In 12 studies, all FM patients were diagnosed by the 1990 American College of Rheumatology criteria. The sample size ranged from 20 to 164 participants. Nine articles were published in English,14,18–20,27,29,30,32,33 two in Chinese,Citation28,Citation31 and one in Portuguese.Citation26 Two studies used EA,Citation14,Citation30 and the other ten studies used MA.Citation18–Citation20,Citation26–Citation29,Citation31–Citation33 The main characteristics of the included studies are presented in .
Table 1 Characteristics of included studies
Risk of bias within studies
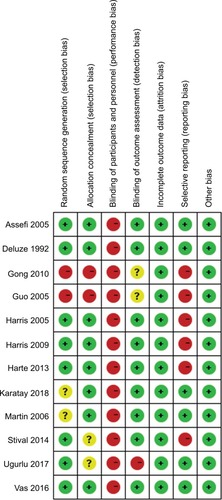
Most of the studies were rated as low ROB, except for four studies.Citation19,Citation26,Citation28,Citation31 Eight studies used computer software or a random number table for random sequence generation.Citation14,Citation18,Citation19,Citation26,Citation27,Citation29,Citation32,Citation33 Two studies reported that participants were divided randomly according to the order of admission, and they did not perform allocation concealment.Citation28,Citation31 Eight studies performed allocation concealment by opaque sealed envelopes or central allocation.Citation14,Citation18,Citation20,Citation27,Citation29,Citation30,Citation32,Citation33 The acupuncturists in all studies were not blinded. Nine studies performed blinding of participants and outcome assessment.Citation14,Citation18,Citation20,Citation26,Citation27,Citation29,Citation30,Citation32,Citation33 There were no missing data in five studies,Citation19,Citation26,Citation28,Citation29,Citation31 and seven other studies reported dropout numbers and reasons.Citation14,Citation18,Citation20,Citation27,Citation30,Citation32,Citation33 Six studies did not report any details about adverse events.Citation26–Citation29,Citation31,Citation32 The ROB summary is presented in .
Effects of interventions
Real acupuncture vs sham acupuncture
Pain changes after treatment
The data regarding pain changes were reported in all studies. Eight studies compared real MA with sham MA,Citation18–Citation20,Citation26,Citation27,Citation29,Citation32,Citation33 and two studies compared real EA with sham EA.Citation14,Citation30 We performed a meta-analysis of pain changes (VAS, 0–10 cm scale). The overall meta-analysis of nine studies showed that real acupuncture was significantly better than sham acupuncture in reducing pain after treatment (MD =−1.04, 95% CI [−1.70, –0.38], P=0.002, I2=78%; ). The quality of evidence was downgraded because of inconsistency and evaluated as moderate (). The subgroup analysis indicated that both real MA (MD =−1.14, 95% CI [−2.18, –0.09], P=0.03, I2=82%; ) and real EA (MD =−0.94, 95% CI [−1.17, –0.72], P<0.00001, I2=0%; ) were statistically significantly better than sham acupuncture in reducing pain after treatment. The quality of evidence was moderate for the comparison of real MA vs sham MA and low for the comparison of real EA vs sham EA ().
Figure 3 Forest plot comparing real acupuncture vs sham acupuncture.
Abbreviations: EA, electro-acupuncture; FIQ, fibromyalgia impact questionnaire; MA, manual acupuncture; SF-MPQ, short form of McGill Pain Questionnaire.
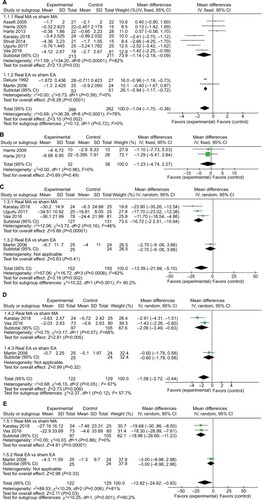
Table 2 Effect size and GRADE quality of evidence
Only two studies measured pain intensity by using a short form of MPQ (SF-MPQ).Citation27,Citation29 The pooled results indicated that there were no statistically significant differences in pain reduction between real MA and sham MA (MD =−1.23, 95% CI [–4.74, 2.27], P=0.49, I2=0%; ). The quality of evidence was evaluated as low (downgraded because of imprecision and publication bias, )
Quality of life: FIQ changes after treatment
Four studies evaluated quality of life by using the FIQ score.Citation18–Citation20,Citation30 The pooled results indicated that real acupuncture was significantly better than sham acupuncture in improving quality of life after treatment (MD =−13.39, 95% CI [−21.69, –5.10], P=0.002, I2=82%; ). The quality of evidence was evaluated as low (downgraded because of inconsistency and imprecision, ). The subgroup analysis showed that the real MA of three studies was sig nificantly better than sham MA for improving quality of life after treatment (MD =−16.72, 95% CI [−22.51, –10.94], P<0.00001, I2=46%; ), and the quality of evidence was evaluated as moderate (). However, there was no statistically significant difference between real EA and sham EA based on one study (MD =−2.7, 95% CI [–9.06, 3.66], P=0.41; ), and the quality of evidence was evaluated as low ().
Long-term effect of acupuncture
There were three studies that followed-up long-term (more than three months after treatment) to assess the effect of acupuncture, and the data can be obtained.Citation18,Citation20,Citation30 Because more than one follow-up result was measured among the studies (), we included the last follow-up result in our pooled analysis.
Two studies compared real MA with sham MA, and one study compared real EA with sham EA. The pooled results indicated that real acupuncture had a superior long-term effect on reducing pain and improving the quality of life compared with sham acupuncture (MD =−1.58, 95% CI [−2.72, –0.44], P=0.006, I2=67%, ; MD =−12.92, 95% CI [−24.92, –0.93], P=0.03, I2=81%; ). Because of inconsistency and imprecision, the quality of evidence was downgraded and evaluated as low (). The subgroup analysis showed that real MA was significantly better than sham MA for reducing pain and improving the quality of life in the long term (MD =−2.06, 95% CI [−3.49, –0.63], P=0.005, I2=68%, ; MD =−18.96, 95% CI [−26.69, –11.23], P<0.00001, I2=0%, ), and the quality of evidence was evaluated as very low and low, respectively (). However, there were no statistically significant differences between real EA and sham EA for reducing pain and improving the quality of life in the long term (MD =−0.6, 95% CI [–1.78, 0.58], P=0.32, ; MD =−3.0, 95% CI [–8.98, 2.98], P=0.33; ), and the quality of evidence was evaluated as low ().
Adverse events
Six studies reported no serious adverse events,Citation14,Citation18–Citation20,Citation30,Citation33 of which four studies observed mild adverse events, such as bruising, soreness, nausea, discomfort of needle insertion, and aggravation of symptoms.Citation14,Citation18,Citation30,Citation33 These mild adverse events were more common in the real acupuncture group than in the sham acupuncture group. The other four studies did not provide any details about adverse events.Citation26,Citation27,Citation29,Citation32
Real acupuncture vs conventional medication
Pain changes after treatment
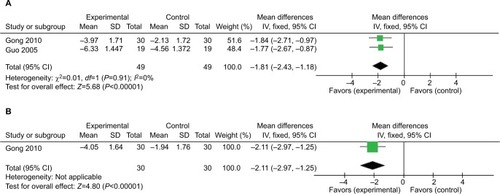
Two studies compared real acupuncture with conventional medication and reported the data on pain changes (VAS, 0–10 cm scale).Citation28,Citation31 The pooled results showed that real acupuncture was statistically significantly better than conventional medication in reducing pain after treatment (MD =−1.81, 95% CI [−2.43, –1.18], P<0.00001, I2=0%; ). However, the quality of evidence was downgraded because of ROB, imprecision and publication bias and was evaluated as very low ().
Long-term effect of acupuncture
Two studiesCitation28,Citation31 included follow-up observations at 6 months after treatment, but only one study provided data on pain changes (VAS, 0–10 cm scale). The result indicated that real acupuncture yielded significantly more pain reduction than conventional medication at follow-up (MD =−2.11, 95% CI [−2.97, –1.25], P<0.00001; ).
Adverse events
There were no details about any adverse events reported.
Heterogeneity and sensitivity analyses
There was considerable heterogeneity (I2=78%) in the comparison of real acupuncture vs sham acupuncture on pain changes after treatment. We conducted sensitivity analyses by omitting potential heterogeneous studies to observe their influence on the pooled effect size. Two studies were omitted because their ROB was high.Citation19,Citation26 The third study was omitted because the mean data were measured from the published article and SD was taken from baseline.Citation33 The fourth study was omitted because the data in the meta-analysis were transformed from NRS.Citation32 All studies omitting either of the four mentioned studies were then recalculated to determine the pooled effect size. Sensitivity analyses indicated that the pooled effect was not changed when omitting either of the four mentioned studies. The result of sensitivity analyses on studies with low ROB was consistent with the result of all studies (). However, the heterogeneity was not resolved and may be caused by various acupoints, different measurement time points, and sham acupuncture methods. The sensitivity analyses of other outcomes were not conducted due to the low number of corresponding included studies.
Publication bias
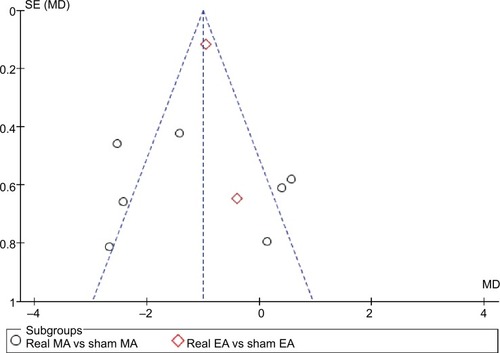
The funnel plot for pain changes after treatment demonstrated that visual inspection of the funnel plot was symmetric and no clear publication bias was detected ().
Discussion
Summary of the main findings
We included 12 RCTs that compared acupuncture therapy to sham acupuncture or conventional medication. With respect to reducing pain (VAS 0–10 cm scale), there was moderate-quality evidence showing that real acupuncture was more effective than sham acupuncture in the short term, and similar results were obtained with low-quality evidence in the long term. With respect to improving the quality of life, there was low-quality evidence showing that real acupuncture was more effective than sham acupuncture in both the short and long term. In the comparison of acupuncture vs conventional medication, we found very low-quality evidence showing that acupuncture was more effective in relieving pain in both the short and long term.
Subgroup analyses demonstrated that real MA was superior to sham MA in reducing pain (VAS, 0–10 cm scale) and improving the quality of life, with moderate-quality evidence in the short term and low- to very low-quality evidence in the long term. There were two studies that compared real EA with sham EA. The results indicated real EA was superior to sham EA in reducing pain in the short term with low-quality evidence, but no significant difference was observed in the long term with low-quality evidence. Only one study compared real EA with sham EA and reported the effect on improving the quality of life. The results demonstrated no significant difference between real EA and sham EA in both the short and long term with low-quality evidence.
According to the TCM theory, FM is categorized as Bi Syndrome; the invasion of pathogenic wind, cold, and dampness can affect imbalance in the flow of Qi and blood, and then cause pain, stiffness, and other symptoms in the body’s muscles, tendons, and joints.Citation34 Therefore, the TCM mechanism of acupuncture for FM is to regulate the circulation of Qi and blood, combined with expelling cold and removing dampness. A modern medical study indicated that acupuncture can significantly increase blood flow in the skin and muscles of patients with FM,Citation35 which is very important for reducing pain symptoms. As a primary mechanism of FM, the central sensitization of nervous system can decrease the pressure pain threshold, elicit hyperalgesia, and as a result, a noxious stimulus can cause more severe pain than in normal individuals.Citation36,Citation37 One recent animal study found that the upregulation of transient receptor potential vanilloid 1 and the phosphoactivation of extracellular signal regulated kinase were associated with mechanical hyperalgesia in FM model mice. EA at the bilateral Zusanli (ST36) acupoints can reverse the upregulation of these receptors and reduce mechanical hyperalgesia significantly.Citation38 Another animal study showed that acid-sensing ion channel 3 and the ERK pathway participated in FM pain attenuated by EA.Citation39 Additionally, acupuncture can regulate the central nervous system to release endogenous opioids and nonopioid compounds, such as endorphin, serotonin, enkephalins, dynorphin, norepinephrine, oxytocin, neuropeptide, and ATP. These substances are essential to decrease the hypersensitivity of pain and reduce pain symptoms.Citation12,Citation13,Citation40,Citation41 However, the specific mechanism of acupuncture therapy for FM is very complex and remains unknown. Therefore, more studies are needed in the future.
Comparison with previous systematic reviews
Previous meta-analyses have drawn various conclusions depending on the inclusion criteria and the number of included studies.Citation15–Citation17,Citation42 One reviewCitation42 published in 2010 included seven RCTs. The pooled analysis found strong evidence for the reduction of pain (standardized mean difference (SMD) =−0.25, 95% CI [−0.49, –0.02]) at posttreatment compared to control acupuncture, which contained sham and simulated acupuncture. However, sensitivity analysis indicated that this small analgesic effect of acupuncture was only present in studies with ROB. Therefore, this review concluded that acupuncture cannot be recommended for the management of FM. In 2013, one systematic reviewCitation16 included 16 RCTs that compared acupuncture alone or combined with other interventions (cupping therapy, point injection, point catgut embedding, or moxibustion) to no treatment, sham, or conventional medication. The conclusion indicated that acupuncture alone or combined with cupping therapy was superior to conventional medications. However, acupuncture had no better effect than sham acupuncture on pain reduction. Another Cochrane review of acupuncture for FM was also published in 2013 and included nine RCTs.Citation17 Pain severity measured with VAS, NRS, MPI, and MPQ was pooled in six studies, and the results indicated that acupuncture was no better than sham acupuncture in reducing pain (SMD =−0.14, 95% CI[–0.53, 0.25]). Therefore, the available systematic reviews demonstrated controversial conclusions about whether acupuncture was more effective than sham acupuncture in relieving pain.
Compared with previous systematic reviews, our review focused mainly on observing the efficacy of acupuncture alone, so we did not involve studies with mixed therapies. We included an additional five new RCTs published after 2013 in our review, three with low ROB and two with high ROB. Since the pain severity of patients was measured with VAS, NRS, MPI, or MPQ, this analysis may produce greater heterogeneity if the results of different measurement tools are directly pooled. Therefore, we extracted the results of the same tool as much as possible. Because most of the included studies used VAS as a measurement tool and FIQ contained VAS, we extracted the results of VAS to pool the analysis. Because one study data of the meta-analysis were transformed from NRS, we conducted sensitivity analyses by excluding this study and found that the pooled effect was not changed. We included nine RCTs, and the results indicated that real acupuncture was superior to sham acupuncture in reducing pain (VAS, 0–10 cm scale) in the short term with moderate-quality evidence (MD =−1.04, 95% CI [−1.70, –0.38]). This new conclusion of our review was completely different from that of previous research and can provide a better reference for clinical decisions because we analyzed direct VAS results.
Limitations and implications
This systematic review has several limitations. First, a low number of studies were included in our review, and most of the studies had a relatively small sample size. This limitation may lead to imprecise evidence. Second, there was considerable heterogeneity in our meta-analysis. We attempted to decrease the heterogeneity by subgroup and sensitivity analyses, but it was not completely resolved. We considered that this heterogeneity possibly derived from methodological bias and differences in acupoint selection, sham acupuncture method, and the frequency and duration of treatment. Third, only a few studies followed-up the patients after treatment and reported adverse events; thus, studies with more details about follow-up and adverse events would better evaluate the long-term effect and safety of acupuncture.
Given the above limitations, more rigorous larger-scale and well-designed RCTs are needed to provide higher-quality evidence and evaluate the efficacy of acupuncture for FM. First, future RCTs should correctly conduct random sequence generation, allocation concealment, and blinding to avoid ROB. Simultaneously, the details about follow-up, dropout, and adverse events must be reported thoroughly. Second, many different kinds of acupuncture are used to treat FM in clinical practice. Therefore, future studies comparing different acupuncture interventions are needed to find the most effective acupuncture treatment. Furthermore, the optimal duration and frequency of treatment are also important for FM. Third, all RCTs must be registered in advance and reported using standards for reporting interventions in clinical trials of acupuncture (STRICTA) guidelineCitation43 to improve the quality of future reports in this field.
Conclusion
In summary, real acupuncture was more effective than sham acupuncture in relieving pain (VAS, 0–10 cm scale) and improving the quality of life in both the short and long term. Both EA and MA were better than sham acupuncture in relieving pain in the short term. Furthermore, acupuncture was more effective in relieving pain in both the short and long term compared with conventional medication. No serious adverse events were found during acupuncture. In brief, acupuncture therapy is an effective and safe treatment for patients with FM, and it can be recommended for the management of FM. However, more large-sample RCTs are needed to investigate the therapeutic effect of EA for FM in the long term.
Author contributions
Study concept and design: GN, XZ. Acquisition of data: XZ, HC, WX. Analysis and interpretation of data: GN, XZ, HC, WX, YS, YG. Article drafting and critical revision of the manuscript for important intellectual content: GN, XZ, HC, WX, YS, YG. Administrative, technical, or administrative support: GN, XZ, HC. Study supervision: GN, XZ. All authors read and approved the final manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81674067). The funding body had no role in the design of the study, in collection, analysis, and interpretation of data, and in writing the manuscript.
Supplementary materials
Table S1 Reasons for excluded studies
Table S2 Sensitivity analyses on pain changes after treatment
References
- MistSDJonesKDRandomized controlled trial of acupuncture for women with fibromyalgia: group acupuncture with traditional Chi-nese medicine diagnosis-based point selectionPain Med20181991862187129447382
- MaSZhaoLCaiCMaXPengSDaiJClinical observation on treating 136 cases of fibromyalgia syndrome by acupuncture at Backshu pointMod Chin Clin Med201825021113
- Castro-SanchezAMGarcia-LopezHMataran-PenarrochaGAEffects of dry needling on spinal mobility and trigger points in patients with fibromyalgia syndromePain Phys201723752
- IannuccelliCGuzzoMPAtzeniFPain modulation in patients with fibromyalgia undergoing acupuncture treatment is associated with fluctuations in serum neuropeptide Y levelsClin Exp Rheumatol201735Suppl 105818528598785
- ZuckerNATsodikovAMistSDCinaSNapadowVHarrisREEvoked pressure pain sensitivity is associated with differential analgesic response to verum and sham acupuncture in fibromyalgiaPain Med20171881582159228340147
- LiDYangLLiJFibromyalgia syndrome treated with acupuncture at the acupoints of the affected meridians and heavy moxibustion at painful points: a randomized controlled trialZhongguo Zhen Jiu2016362147151 Chinese27348913
- DiasPAGuimaraesABAlbuquerqueAOde OliveiraKLCavalcanteMLGuimaraesSBShort-term complementary and alternative medicine on quality of life in women with fibromyalgiaJ Integr Med2016141293526778226
- YuJLiLQinHChenYJinSClinical observation of Zheng Qing Feng Tong Ning combined with acupuncture for fibromyalgia syndromeHubei J TCM20163863738
- WeberAWerneckLPaivaEGansPEffects of music in combination with vibration in acupuncture points on the treatment of fibromyalgiaJ Altern Complement Med2015212778225635925
- de TommasoMDelussiMRicciKD’AngeloGAbdominal acupuncture changes cortical responses to nociceptive stimuli in fibromyalgia patientsCns Neurosci Ther201420656556724836741
- CasanuevaBRivasPRoderoBQuintialCLlorcaJGonzalez-GayMAShort-term improvement following dry needle stimulation of tender points in fibromyalgiaRheumatol Int201434686186623609584
- CollazoEMuñozRMDAragonésMÁGómezFRandomized prospective study to assess the effectiveness of several therapeutic procedures of traditional Chinese medicine in alleviation of pain and improvement in the standard of living in patients with fibromyalgiaRev Int Acupuntura201484121128
- ShaoMJiangMTreatment of fibromyalgia syndrome with acupuncture of soothing liver and relieving depressionHubei J TCM2013351262
- CollazoCEMuñozRMDScalp acupuncture and acupunture for treatment of patients with fibromyalgia. Prospective randomized studyRev Int Acupuntura201371611
- HadianfardMJHosseinzadehPMA randomized clinical trial of fibromyalgia treatment with acupuncture compared with fluoxetineIran Red Crescent Med J2012141063164023285415
- IannuccelliCMannocciFGuzzoMPComplementary treatment in fibromyalgia: combination of somatic and abdominal acupunctureClin Exp Rheumatol2012306 Suppl 7411211623261009
- CollazoCEAcupuncture and traditional Chinese dietary therapy in the treatment of patients with fibromyalgia. A randomized prospective studyRev Int Acupuntura20126394101
- ItohKKitakojiHEffects of acupuncture to treat fibromyalgia: a preliminary randomised controlled trialChin Med201051120331844
- JiangZYLiCDQiuLCombination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome: a multi-central randomized controlled trialZhongguo Zhen Jiu2010304265269 Chinese20568427
- CollazoCEEffectiveness of acupuncture therapy for pain relief in patients with fibromyalgiaRev Int Acupuntura2010415258
- LiBWangYTherapeutic effect of acupuncture at lower Dan-Tian on neuropsychiatric symptoms of fibromyalgia syndromeActa Chin Med Pharmacol20093768990
- ZhaoRHZhuYBObservation on therapeutic effect of herb-partitioned moxibustion on fibromyalgia syndromeZhongguo Zhen Jiu2009293200202 Chinese19358502
- TarginoRAImamuraMKaziyamaHHA randomized controlled trial of acupuncture added to usual treatment for fibromyalgiaJ Rehabil Med200840758258818758677
- HarrisRESundgrenPCPangYDynamic levels of glutamate within the insula are associated with improvements in multiple pain domains in fibromyalgiaArthritis Rheum200858390390718311814
- SunY28 cases of fibromyalgia syndrome treated by acupuncture and moxibustionWorld Chin Med200833170171
- LiYSixty-six cases of fibromyalgia syndrome treated with affected meridian pointsWorld J Acupunct Moxibustion20071745455
- FuLiCDXYJiangZYClinical study on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndromeZhongguo Zhen Jiu2006261810 Chinese16491748
- YaoQZhangXWangXTreatment of fibromyalgia syndrome with Tiao Du Tong Mai acupunctureJ Clin Acupunct Moxibustion20062222425
- HarrisREGracelyRHMcLeanSAComparison of clinical and evoked pain measures in fibromyalgiaJ Pain20067752152716814691
- GuoXJJiaJComparison of therapeutic effects on fibromyalgia syndrome between dermal-neurological electric stimulation and electric acupunctureAdv Clin Rehabil2005946171173
- WangWLiuZWuYClinical observation on 42 cases of fibromyalgia syndrome treated by acupuncture and moxibustionJ Tradit Chin Med20041912627
- WangSWangXZhangDXiaPYangHClinical observation on therapeutic effect of acupuncture treatment based on syndrome differentiation of meridians on fibromyalgiaZhongguo Zhen jiu20022212807809
- LiuQLiFClinical analysis of 30 cases of fibromyalgia treated by acupunctureAnthol Med2002212183184
- ZhangYClinical observation on acupuncture treatment of primary fibromyalgia syndromeZhongguo Zhen jiu20012111920
- SandbergMLundebergTGerdleBManual acupuncture in fibromyalgia: a long-term pilot studyJ Musculoskelet Pain1999733958
- SprottHEfficiency of acupuncture in patients with fibromyalgiaClin Bull Myofascial Ther1998313743
- HarrisRETianXWilliamsDATreatment of fibromyalgia with formula acupuncture: investigation of needle placement, needle stimulation, and treatment frequencyJ Altern Complement Med200511466367116131290
- UgurluFGSezerNAktekinLFidanFTokFAkkusSThe effects of acupuncture versus sham acupuncture in the treatment of fibromyalgia: a randomized controlled clinical trialActa Reumatol Port2017421323728371571
- StivalRSCavalheiroPRStasiakCEGaldinoDTHoekstraBESchafranskiMDAcupuncture in fibromyalgia: a randomized, controlled study addressing the immediate pain responseRev Bras Reumatol201454643143625458024
- AssefiNPShermanKJJacobsenCGoldbergJSmithWRBuchwaldDA randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgiaAnn Intern Med20051431101915998750
Disclosure
The authors report no conflicts of interest in this work.
References
- WolfeFClauwDJFitzcharlesMA2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteriaSemin Arthritis Rheum201646331932927916278
- QueirozLPWorldwide epidemiology of fibromyalgiaCurr Pain Headache Rep201317835623801009
- FitzcharlesMASte-MariePAGoldenbergDL2012 Canadian Guidelines for the diagnosis and management of fibromyalgia syndrome: executive summaryPain Res Manag201318311912623748251
- ClauwDJFibromyalgia: a clinical reviewJAMA2014311151547155524737367
- HäuserWAblinJFitzcharlesM-AFibromyalgiaNat Rev Dis Primers20157815022
- Cabo-MeseguerACerda-OlmedoGTrillo-MataJLFibromyalgia: prevalence, epidemiologic profiles and economic costsMed Clin201714910441448
- TheoharidesTCTsilioniIArbetmanLFibromyalgia syndrome in need of effective treatmentsJ Pharmacol Exp Ther2015355225526326306765
- AblinJFitzcharlesMABuskilaDShirYSommerCHäuserWTreatment of fibromyalgia syndrome: recommendations of recent evidence-based interdisciplinary guidelines with special emphasis on complementary and alternative therapiesEvid Based Complement Alternat Med20132013317
- ThorpeJShumBMooreRAWiffenPJGilronICombination pharmacotherapy for the treatment of fibromyalgia in adultsCochrane Database Syst Rev20182CD01058529457627
- MacfarlaneGJKronischCDeanLEEULAR revised recommendations for the management of fibromyalgiaAnn Rheum Dis201776231832827377815
- CoutauxANon-pharmacological treatments for pain relief: TENS and acupunctureJoint Bone Spine201784665766128219657
- OndrejkovicovaAPetrovicsGSvitkovaKBajtekovaBBanghaOWhy acupuncture in pain treatment?Neuro Endocrinol Lett201637316316827618609
- TangYYinHYRubiniPIllesPAcupuncture-induced analgesia: a neurobiological basis in purinergic signalingNeuroscientist201622656357827343858
- DeluzeCBosiaLZirbsAChantraineAVischerTLElectroacupuncture in fibromyalgia: results of a controlled trialBMJ19923056864124912521477566
- YangBYiGHongWEfficacy of acupuncture on fibromyalgia syndrome: a meta-analysisJ Tradit Chin Med201434438139125185355
- CaoHLiXHanMLiuJAcupoint stimulation for fibromyalgia: a systematic review of randomized controlled trialsEvid Based Complement Alternat Med2013201336283124454493
- DeareJCZhengZXueCCAcupuncture for treating fibromyalgiaCochrane Database Syst Rev2013315CD007070
- VasJSantos-ReyKNavarro-PabloRAcupuncture for fibromyalgia in primary care: a randomised controlled trialAcupunct Med201634425726626879181
- UgˇurluFGSezerNAktekinLFidanFTokFAkkus¸SThe effects of acupuncture versus sham acupuncture in the treatment of fibromyalgia: a randomized controlled clinical trialActa Reumatol Port2017421323728371571
- KarataySOkurSCUzkeserHYildirimKAkcayFEffects of acupuncture treatment on fibromyalgia symptoms, serotonin, and substance P levels: a randomized sham and placebo-controlled clinical trialPain Med201819361562829220534
- MoherDLiberatiATetzlaffJAltmanDGGroup P, PRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementInt J Surg20108533634120171303
- WolfeFSmytheHAYunusMBThe American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria CommitteeArthritis Rheum19903321601722306288
- HigginsJPTGreenSCochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration; 2011. Available from http://handbook-5-1.cochrane.org/Accessed June 15, 2018
- GuyattGHOxmanADVistGEGRADE: an emerging consensus on rating quality of evidence and strength of recommendationsBMJ2008336765092492618436948
- SchünemannHBrożekJGuyattGOxmanAGRADE Handbook for Grading Quality of Evidence and Strength of Recommendations [Updated October 2013] The GRADE Working Group, 2013. Available from https://gdt.gradepro.org/app/handbook/handbook.htmlAccessed June 15, 2018
- StivalRSCavalheiroPRStasiakCEGaldinoDTHoekstraBESchafranskiMDAcupuncture in fibromyalgia: a randomized, controlled study addressing the immediate pain responseRev Bras Reumatol201454643143625458024
- HarteSEClauwDJNapadowVHarrisREPressure pain sensitivity and insular combined glutamate and glutamine (Glx) are associated with subsequent clinical response to Sham but not traditional acupuncture in patients who have chronic painMed Acupunct201325215416024761170
- Wei-ZhiGYu-QiWObservations on the therapeutic effect of acupuncture on fibromyalgia syndromeShanghai J Acupunct Moxibust20102911725727
- HarrisREZubietaJKScottDJNapadowVGracelyRHClauwDJTraditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on mu-opioid receptors (MORs)Neuroimage20094731077108519501658
- MartinDPSlettenCDWilliamsBABergerIHImprovement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trialMayo Clin Proc200681674975716770975
- GuoYSunYZClinical study on treatment of fibromyalgia syndrome with penetration needling at the backZhongguo Zhen Jiu20052529810016312890
- HarrisRETianXWilliamsDATreatment of fibromyalgia with formula acupuncture: investigation of needle placement, needle stimulation, and treatment frequencyJ Altern Complement Med200511466367116131290
- AssefiNPShermanKJJacobsenCGoldbergJSmithWRBuchwaldDA randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgiaAnn Intern Med20051431101915998750
- YangGLiangSWeiHTreatment of fibromyalgia syndrome with traditional Chinese medicineInt J Clin Acupunct201524297104
- KimSYMinSLeeHChanges of local blood flow in response to acupuncture stimulation: a systematic reviewEvid Based Complement Alternat Med201620166111
- WuMYHuangMCChiangJHSunMFLeeYCYenHRAcupuncture decreased the risk of coronary heart disease in patients with fibromyal-gia in Taiwan: a nationwide matched cohort studyArthritis Res Ther20171913728245860
- JiRRNackleyAHuhYTerrandoNMaixnerWNeuroinflammation and central sensitization in chronic and widespread painAnesthesiology2018129234336629462012
- LinJGHsiehCLLinYWAnalgesic effect of electroacupuncture in a mouse fibromyalgia model: roles of TRPV1, TRPV4, and pERKPLoS One2015106e012803726043006
- YenLTHsiehCLHsuHCLinYWTargeting ASIC3 for relieving mice fibromyalgia pain: roles of electroacupuncture, opioid, and adenosineSci Rep2017714666328440280
- Cidral-FilhoFJda SilvaMDMoréAOCórdovaMMWernerMFSantosARManual acupuncture inhibits mechanical hypersensitivity induced by spinal nerve ligation in ratsNeuroscience201119337037621835228
- ZhangRLaoLRenKBermanBMMechanisms of acupuncture-electroacupuncture on persistent painAnesthesiology2014120248250324322588
- LanghorstJKlosePMusialFIrnichDHäuserWEfficacy of acupuncture in fibromyalgia syndrome: a systematic review with a meta-analysis of controlled clinical trialsRheumatology201049477878820100789
- MacPhersonHAltmanDGHammerschlagRRevised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statementPLoS Med201076e100026120543992