Abstract
Purpose
Idiopathic intracranial hypertension (IICH) is a condition characterized by raised intracranial pressure (ICP), and its diagnosis is established when the opening pressure measured during a lumbar puncture is elevated >20 cm H2O in nonobese patients or >25 cm H2O in obese patients. Papilledema is caused by forced filling of the optic nerve sheath with cerebrospinal fluid (CSF). Other common but underappreciated symptoms of IICH are neck pain, back pain, and radicular pain in the arms and legs resulting from associated increased spinal pressure and forced filling of the spinal nerves with CSF. Widespread pain and also several other characteristics of IICH share notable similarities with characteristics of fibromyalgia (FM) and chronic fatigue syndrome (CFS), two overlapping chronic pain conditions. The aim of this review was to compare literature data regarding the characteristics of IICH, FM, and CFS and to link the shared data to an apparent underlying physiopathology, that is, increased ICP.
Methods
Data in the literature regarding these three conditions were compared and linked to the hypothesis of the shared underlying physiopathology of increased cerebrospinal pressure.
Results
The shared characteristics of IICH, FM, and CFS that can be caused by increased ICP include headaches, fatigue, cognitive impairment, loss of gray matter, involvement of cranial nerves, and overload of the lymphatic olfactory pathway. Increased pressure in the spinal canal and in peripheral nerve root sheaths causes widespread pain, weakness in the arms and legs, walking difficulties (ataxia), and bladder, bowel, and sphincter symptoms. Additionally, IICH, FM, and CFS are frequently associated with sympathetic overactivity symptoms and obesity. These conditions share a strong female predominance and are frequently associated with Ehlers-Danlos syndrome.
Conclusion
IICH, FM, and CFS share a large variety of symptoms that might all be explained by the same pathophysiology of increased cerebrospinal pressure.
Plain language summary
The pathological mechanisms that cause both fibromyalgia (FM) and chronic fatigue syndrome (CFS) are incompletely understood. FM and CFS share very similar symptoms with idiopathic intracranial hypertension (IICH), a condition characterized by an increase in intracranial pressure (ICP) due to an unknown cause. The authors reviewed the literature to explore these common symptoms and to link them to the hypothesis that increased intracranial and spinal fluid pressure is the possible mechanism that initiates the multitude of symptoms in these conditions. The symptoms include neck pain, back pain, pain in arms and legs, numbness/tingling, headaches, fatigue, cognitive impairment, gradual loss of gray matter, in addition to symptoms involving cranial nerves, overload of the lymphatic system in the nasal mucosa and disturbance of the autonomic nervous system. Other shared characteristics include higher frequency in females and family members, and an association with obesity and Ehlers Danlos syndrome (a connective tissue disorder).
These findings are relevant as they provide an alternative hypothesis concerning the pathological mechanisms in FM and CFS.
Introduction
IICH is a condition characterized by elevated ICP of unknown etiology. Patients may present with headache, papilledema, and visual disturbances. The diagnosis is established when the opening pressure (OP) measured during a lumbar puncture is elevated >20 cm H2O in nonobese patients and >25 cm H2O in obese patients.Citation100
Recently, these cutoff values used to define IICH have been debated. ICP might rather be a continuum with no clear cutoff value. Additionally, headache and/or papilledema may be absent even if the ICP is above these cutoff values. As IICH and CFS share similar symptoms such as fatigue and headache, Higgins et al hypothesized that the milder forms of IICH may present as CFS.Citation41
Common but underappreciated symptoms of IICH are neck pain, back pain, and radicular pain radiating to the arms and legs. These associated symptoms are due to the forced filling of the nerve roots with cerebrospinal fluid (CSF), irritating or compressing the nerve root fibers inside.Citation10,Citation38,Citation43,Citation53,Citation67,Citation72,Citation88,Citation101 Therefore, it is likely that milder forms of elevated ICP may also present as FM or unexplained pain. Indeed, FM has sensory symptoms and signs comparable to those of peripheral neuropathy.Citation16,Citation61,Citation71,Citation80,Citation93,Citation102 Moreover, electrophysiologic abnormalities have been detected in the limbs of patients with FM.Citation15,Citation97
This hypothesis may also provide an explanation for several overlapping chronic pain conditions.
While IICH is characterized by a significant increase in cerebrospinal pressure (CSP), FM and CFS may be the result of intermittent and/or mild chronic increased CSP.
The data in the literature regarding the signs and symptoms of these three conditions were compared and linked to the hypothesis of the shared underlying physiopathology of increased CSP.
shows an overview of reported signs and symptoms for each condition associated with increased ICP; presents signs and symptoms associated with increased spinal pressure. depicts an overview of the interactions of ICP with all the nerves presented in this paper, the olfactory lymphatic pathway, and the inner ear.
Figure 1 Overview of the interactions of ICP with all the nerves presented in this paper, the olfactory lymphatic pathway, and the inner ear.
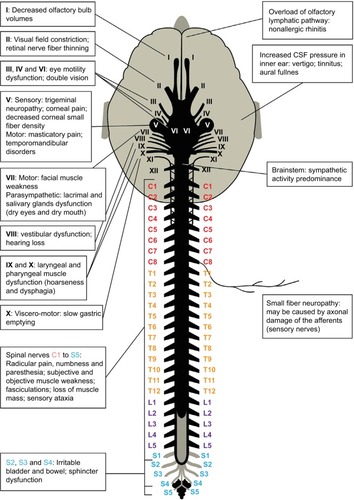
Table 1 Overview of the reported signs and symptoms for each condition that may be caused by increased ICP
Table 2 Overview of the reported signs and symptoms for each condition that may be caused by increased spinal pressure
Symptoms associated with increased ICP
Headache
Most patients with IICH present with headaches. Approximately one in three patients with IICH may already suffer from chronic headaches before diagnosis.Citation101 Additionally, there is significant overlap between the headache types observed in patients with IICH and the headache types of primary headache disorders.Citation59 When performing a lumbar puncture in patients with unresponsive migraine without papilledema, 86% display an OP >20 cm H2O. Evacuation of CSF induces headache remission in 77%.Citation25 However, when the ICP is reduced in patients with IICH using a shunt, the different types of headaches may persist. Therefore, headache is a poor marker of disease activity.Citation104
In patients with FM or CFS, different types of primary headaches such as migraine and tension headache are highly prevalent.Citation51,Citation79
In patients with CFS suffering from headaches, a lumbar puncture revealed an OP ≥20 cm H2O in 40% of patients, and evacuation of CSF improved headaches, alertness, and/or fatigue in 85%.Citation41
Fatigue
Fatigue is the most pronounced symptom of IICH and one of the core symptoms of CFS and FM. Patients with CFS respond to spinal fluid evacuation the same way that patients with IICH do, that is, improvement of the headaches and fatigue.Citation41
Cognitive impairment
Patients with IICH may suffer multidomain cognitive impairment and impaired processing speed, which does not improve after normalization of the ICP.Citation103,Citation105
It is well established that FM and CFS patients may experience mental fogginess. In patients with FM, the term “fibrofog” is used. Cognitive impairment is also measurable in these patients.Citation17,Citation56 Moreover, in both patients with FM and those with CFS, the most pronounced finding in cognitive testing is impaired processing speed. This finding may be a sign of premature aging, as it is also the most prominent abnormality in cognitive aging.Citation22,Citation56
These cognitive impairments may be associated with premature gray matter loss, as seen in patients with FM and CFS. Patients with FM may have a greater overallCitation57 or regionalCitation83 premature age-associated gray matter volume loss. Similar regional gray matter changes were found in MRI studies of patients with CFS. Several other chronic pain disorders have been associated with gray matter reductions such as vulvodynia, irritable bowel syndrome, tension headache, and chronic back pain.Citation76,Citation84 It is not clear whether these gray matter changes are the cause or the consequence of FM or CFS. However, this hypothesis proposes that these changes might be related to damage to neurons due to mechanical compression from elevated ICP.
Cranial nerve involvement
It has been shown that the perineural spaces of several cranial nerves including the olfactory, optic, trigeminal, and auditory nerves show multiple lymphatic pathways of CSF drainage toward the retropharyngeal and cervical lymph nodes.Citation19
When CSP increases, CSF is forced into the cranial nerve root sheaths. This might compromise the blood supply or cause mechanical pressure on the neurons or axons during their intracranial course.
The olfactory nerve (I)
Patients with IICH often show decreased olfactory bulb volumesCitation91 and impaired olfactory function.Citation9 These findings have also been reported for patients with FM.Citation3 It is most likely that these symptoms are due to increased pressure compromising the blood supply and damaging the olfactory nerve cell bodies.
The optic nerve (II)
In IICH, the optic nerve diameter may be increased as the pressure of the CSF dilates the nerve sheath.Citation96 Additionally, due to the increased pressure, the optic nerve fibers inside may be damaged. Consequently, even in the absence of papilledema, peripheral visual field defects may occur.Citation27
Visual field defects have been detected in patients with FM,Citation75,Citation102 which might indicate that the nerve root fibers of the optic nerve are damaged by the increased pressure.
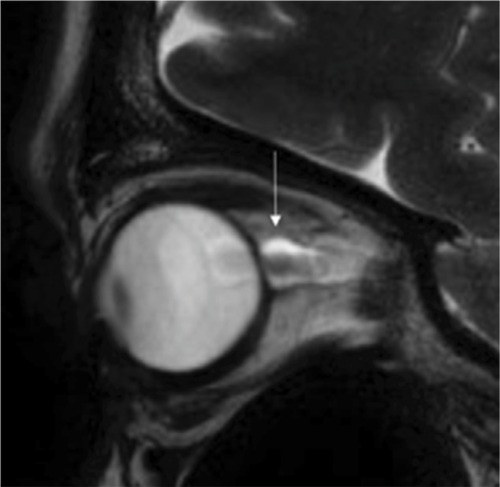
shows T2-weighted sagittal MRI images of a dilated optic nerve in a 46-year-old female patient with unexplained widespread pain. She was later diagnosed with IICH because a lumbar puncture revealed an OP of 23 cm H2O, and visual field defects were detected. Evacuation of 20 mL of CSF dramatically improved her symptoms during a period of 2 or 3 days.
The oculomotor nerve (III), trochlear nerve (IV), and abducens nerve (VI)
The third, fourth, and sixth cranial nerves control the motor function of the eye muscles. In IICH, compression of these nerves may cause oculomotor weakness, and patients present with double vision and, in severe cases, even oculomotor palsy.Citation59,Citation101 In patients with FM and CFS, double vision has been reported, and in patients with CFS, eye motility dysfunction has been observed.Citation6,Citation37,Citation87,Citation102
The trigeminal nerve (V)
The motor fibers of the fifth cranial nerve supply the masticatory muscles. Irritation of these fibers may produce hypertonia of the masticatory muscles, bruxism, temporo-mandibular disorders, and masticatory pain. The sensory fibers supply the facial dermatomes. Irritation of these fibers may produce facial pain. In patients with IICH, there have been reports of trigeminal hypersensitivity or neuralgia of the trigeminal dermatome. Electrophysiologic studies have indicated trigeminal nerve involvement, and the symptoms were reversed following lumbar puncture.Citation4
Hypertonia of the masticatory muscles and facial pain are commonly reported in patients with FM and CFS.Citation68,Citation83
Additionally, small fiber scarcity has been detected in women suffering from FM by measuring corneal nerve fiber thickness with a confocal microscope. In these patients, nerve scarcity was associated with neuropathic pain descriptors.Citation77 Small fiber neuropathy in the cornea may be the consequence of damage to the sensory afferents in the trigeminal nerves.
The facial nerve (VII)
The motor fibers of the facial nerve innervate the muscles of the face. In IICH, several cases of facial weakness or facial palsy due to nerve fiber compression have been reported.Citation101 The facial nerve supplies the autonomic function of the salivary and the lacrimal glands. A few cases of Sicca syndromeCitation94 were reported in patients with IICH. According to this hypothesis, this may be due to the compression of the autonomic fibers running toward the salivary and lacrimal glands.
To the best of our knowledge, facial nerve weakness has not been reported in patients with FM or in CFS. However, in patients with FM and those with CSF, the symptoms of dry eyes and dry mouth are highly prevalent.Citation18,Citation89
Additionally, in cases of severe dry eyes, the sensory trigeminal nerve fibers supplying the conjunctiva and the cornea may also be involved. Severe dry eye is a condition that is shared by patients with FM and those with CFS. It has been suggested that severe dry eyes are the consequence of a corneal somatosensory dysfunction, and evidence suggests that in some patients, the symptom of severe dry eyes may actually be neuropathic ocular pain.Citation58
The vestibulocochlear nerve (VIII)
The eighth cranial nerve provides the sensory innervation of the inner ear, that is, the cochlea for hearing and the vestibula for balance. Irritation or damage to the nerve fibers may cause hearing loss or vertigo in patients with IICH.
Hearing loss and vertigo may also result from the transmission of increased CSF pressure to the inner ear via the cochlear aqueduct. Menière’s disease and IICH share similar symptoms, such as a higher prevalence of vertigo, tinnitus, aural fullness, sensorineural hearing loss, and headache. When lumbar puncture was performed in patients with IICH, vertigo, dizziness, fluctuating hearing loss, tinnitus, and aural fullness improved.Citation78 Additionally, the medical management strategies are similar for both IICH and Menière’s disease, for example, diuretics and corticosteroids.Citation21,Citation95
Patients with FM often complain of subjective hearing loss. Recently, objective audiologic abnormalities were detected in patients with FM.Citation49,Citation102
Additionally, vestibular test abnormalities were detected in patients with CFS.Citation5,Citation73
The glossopharyngeal nerve (IX) and the vagus nerve (X)
The ninth and tenth cranial nerves supply the sensory and motor functions of the larynx and the pharynx. The hoarseness and dysphagia reported in patients with FM and those with CFS are probably caused by the compression of the ninth and tenth cranial nerve motor fibers.Citation81,Citation102
The tenth cranial nerve supplies the parasympathetic innervation of the cardiovascular, respiratory, and gastrointestinal systems. This might explain why increased ICP is associated with slower gastric emptying, as seen in brain-injured patients.Citation66 In patients with FM and those with CFS, slower gastric emptying is a common complaint,Citation74 and in patients with CFS, slower gastric emptying has been observed.Citation12
The olfactory lymphatic pathway
As previously mentioned, CSF drainage routes involve the flow of CSF along the perineural space of the cranial nerves. The most common pathway involves the olfactory nerve, the fibers of which leave the olfactory bulb and penetrate through the foramina of the cribriform plate to leave the brain. The endothelial layer of the olfactory nerve sheath becomes thinner in the nasal mucosa covering the conchae, nasal septum, ethmoid sinus, and lateral walls of the nasal cavity. Subsequently, CSF penetrates through the endothelium into the lymphatic pathways of the nasal submucosa toward the regional lymph nodes.Citation19,Citation48
In patients with IICH, several cases of sinusitis have been reported. Masri reported that 5 (26%) of 19 children with IICH had sinusitis.Citation36,Citation52,Citation63,Citation64
In patients with severely increased CSP, a spontaneous dural leak through the thin layer of the olfactory nerve root sheath may cause rhinorrhea.Citation60
In patients with FM and those with CFS, idiopathic nonallergic rhinitis is a common symptom and presents as nasal obstruction and rhinorrhea.Citation8 According to this hypothesis, obstruction of the nose and rhinorrhea may occur when the olfactory lymphatic drainage system becomes saturated by excess CSF. Excess CSF might cause swelling of the nasal submucosa and leaking of CSF into the paranasal and nasal cavities may cause rhinorrhea or sinusitis. In addition, when CSF pressure is severely increased, a spontaneous transnasal dural leak may occur.
Symptoms associated with increased spinal pressure
The spinal nerves
As the ICP increases, when the patient is in the upright position, due to hydrostatic pressure, the CSF will be forced downwards into the spinal subarachnoid space and, subsequently into the subarachnoid space of the nerve root sheaths.
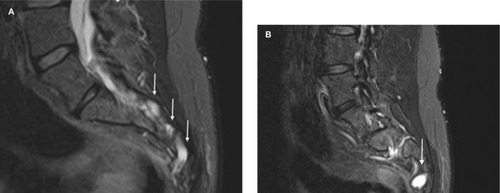
Sacral nerve root sheath dilations can be observed, which appear very similar to the optic nerve root sheath dilations. shows T2-weighted sagittal MRI images of such nerve root dilations in the sacrum of the patient that was initially diagnosed with FM and CFS shown in . shows a more lateral view of the sacrum, demonstrating a significant dilation or Tarlov cyst on nerve root S3.
Figure 3 (A) Sacral nerve root sheath dilations can be observed, and these appear to be very similar to the optic nerve root sheath dilations. (B) A more lateral view of the sacrum showing significant dilation (Tarlov cyst) of nerve root S3.
As the pressure inside the nerve root sheath increases, the nerve root fibers inside may be irritated or compressed, and radicular pain may occur. As mentioned above, radicular pain in IICH is a common but underestimated symptom.Citation101 Irritation or compression of the nerve fibers in the spinal nerves may also produce numbness, paresthesia, or weakness in the arms and legs.Citation33 Similar symptoms have been detected in FM and CFS patients.Citation17,Citation55 More than half of the patients with FM complain of weakness in the arms and legs, and in 13% of patients with FM, the weakness is associated with the loss of muscle mass.Citation102 Electromyography and nerve conduction studies have objectified demyelinating and/or axonal sensorimotor polyneuropathy in 90% of FM patients.Citation15
Additionally, different authors have reported small fiber neuropathy detected in skin biopsies of patients with FM.Citation29 It has been speculated that small fiber neuropathy may be the consequence of immunologic processes. However, small fiber neuropathy may also be the consequence of axonal damage of the central afferents of the small fibers, that is, sensory nerves.
When performing a lumbar puncture in patients with chronic unexplained pain or FM, 50% of patients showed an OP at or above 20 cm H2O. Following the evacuation of 15–25 mL of CSF, 70% of patients responded with significant improvement of their pain symptoms.Citation44
Patients with IICH may present with walking difficulties, mostly ataxia.Citation33 It is likely that radiculopathy may cause sensory ataxia due to damage to the afferent fibers carrying the proprioceptive information from the legs. Ataxia and poor balance in patients with FM and reduced gait automaticity in patients with CFS have been reported.Citation28,Citation102
In humans in the upright position, the hydrostatic pressure is higher inside the sacral nerve roots than in the lumbar, dorsal, and cervical nerve roots. Therefore, if the CSP increases, the sacral nerve roots are at the greatest risk. The sacral nerve roots provide the autonomic innervation of the distal colon and the detrusor of the bladder as well as the motor innervation of the anal and urinary sphincters. This may explain why urinary incontinence and nocturia may occur in patients with IICH.Citation101
In patients with FM and those with CFS, bladder, bowel, and sphincter dysfunctions are commonly reported. Urodynamic testing in patients with FM showed that detrusor overactivity was the most common observation.Citation23
Sympathetic activity predominance
The sympathetic nervous system prepares the body to fight or flight. Sympathetic activity predominance symptoms include the following: digestive problems (slower gastric emptying), constipation (slower bowel peristalsis), superficial breathing, tachycardia, postural hypotension, anxiety, night sweats, poor sleep quality, obstructive sleep apnea, and fatigue.
Use of muscle microneurography to assess sympathetic activity showed that a 9 cm H2O ICP increase (from 11 to 20 cm H2O) significantly increased sympathetic activity by 17%. This was probably due to pressure sensitive receptors in the brainstem that have the potential to trigger a sympathetically mediated systemic response.Citation92
A systematic review revealed that 60% of studies on FM and CFS describe sympathetic activity predominance in those conditions. The most frequently used methods to assess sympathetic functionality were heart rate variability analysis, tilt table testing, sympathetic skin response, and genetic studies.Citation62
Miscellaneous
Genetic origin
Patients suffering from IICH, FM, and CFS are significantly predominantly femaleCitation11,Citation20,Citation30,Citation101 and there is a strong indication of family inheritance.Citation1,Citation13,Citation50 Additionally, patients with connective tissue disorders, such as Ehlers-Danlos syndrome, have increased risk of developing one of these three conditions.Citation39,Citation40,Citation85 This may indicate that genetic defects may play a role in ICP dysregulation.
Obesity
IICH is mostly diagnosed in obese female patients. Obesity increases intra-abdominal pressure and therefore also increases ICP.Citation101 This hypothesis might explain why obese women have an increased risk of developing FM or CFS.Citation26,Citation70
Depression/anxiety/poor quality of life
It is well known that FM and CFS patients suffer from depression, anxiety, and poor quality of life.Citation20,Citation47
IICH is also characterized by poor quality of life and headaches or obesity alone cannot account for this result.Citation54
Sleep disturbances
Among FM patients, 70% were found to suffer from sleep disorders.Citation55 Sleep disturbances are associated with the symptoms of sympathetic overactivity, such as a higher heart rate during sleep in patients with FM compared to healthy controls. In patients with FM, sleep is less efficient than in healthy controls, with a higher proportion of non-rapid eye movement sleep, more arousals, more periodic limb movements, and a higher proportion of periodic breathing (cyclic abnormalities in the breathing pattern including episodes of apnea and hypopnea).Citation82
Among adolescent patients with CFS, 69% were found to suffer from one or more sleep disorders such as obstructive sleep apnea (40%), periodic limb movement disorder (9%), and restless legs syndrome (41%).Citation47
Similarly, 82% of patients with IICH may suffer from sleep disturbances.Citation54
Disability
Additionally, as in patients with FM and those with CFS, patients with IICH have a high rate of disability, as reflected by objective measures such as unemployment.Citation32,Citation65 Patients with IICH also have a high hospital admission rate (38% in 2007), which is only partly due to the higher rate of concomitant obesity.Citation34
The role of cerebral blood flow in the pathophysiology of IICH, FM, and CFS
Although the pathophysiology of IICH is unknown, growing evidence suggests that cerebral venous outflow obstruction due to transverse sinus stenosis may be the underlying cause. Bilateral transverse sinus stenosis can be identified on magnetic resonance venography in more than 90% of patients with IICH and only in 3% of healthy controls.Citation69
Venous sinus stenting was applied as a management strategy in patients with IICH with and without papilledema, resolving the condition in all papilledema patients and improving overall symptoms by 89%.Citation14 Venous sinus stenting has been used for the treatment of a CFS patient with borderline IICH, after which pressure headache, fatigue, concentration, and pain significantly improved and she was able to return to work.Citation42
Arterial cerebral blood flow may also play a role. In FM patients, cerebral blood flow velocity characteristics assessed by transcranial Doppler showed significant differences compared with healthy controls.Citation86 CFS patients often present with orthostatic intolerance symptoms, such as blurred vision, dizziness, lightheadedness, sweating, and/or headaches that occur when a patient changes from a supine to an upright position. In these patients, cerebral blood flow autoregulation efficiency is likely reduced. Using quantitative flow MRI techniques, it was demonstrated that CFS patients with more severe orthostatic intolerance symptoms exhibited higher levels of cerebral perfusion and lower levels of intracranial compliance. Cerebral compliance represents the ability to buffer increased intracranial volume while preventing rise of the ICP.Citation31
Conclusion
IICH, FM, and CFS share very similar characteristics and are probably caused by the same underlying disorder of increased CSP. IICH, FM, and CFS can be considered progressive neurologic disorders affecting the central and peripheral nervous systems.
This hypothesis may also provide an explanation for several overlapping chronic pain conditions. These include FM, CFS, temporomandibular disorders, irritable bowel syndrome, chronic tension headache, chronic migraine, severe dry eyes, and chronic nonspecific low back pain.
Unraveling the physiopathology of FM and CFS is important for the recognition of the suffering of patients with these disorders, as there is a stigma associated with the diagnosis of FM or CFS. Moreover, future research should probably focus on therapeutic strategies to lower CSF pressure.
Disclosure
The authors report no conflicts of interest in this work.
References
- AlbrightFLightKLightABatemanLCannon-AlbrightLAEvidence for a heritable predisposition to Chronic Fatigue SyndromeBMC Neurol20111116221619629
- AlmansaCReyESánchezRGSánchezAADíaz-RubioMPrevalence of functional gastrointestinal disorders in patients with fibromyalgia and the role of psychologic distressClin Gastroenterol Hepatol20097443844519138763
- AmitalHAgmon-LevinNShoenfeldNOlfactory impairment in patients with the fibromyalgia syndrome and systemic sclerosisImmunol Res2014602–320120725424576
- ArsavaEMUlucKNurluGKansuTElectrophysiological evidence of trigeminal neuropathy in pseudotumor cerebriJ Neurol2002249111601160212532926
- Ash-BernalRWallCKomaroffALVestibular function test anomalies in patients with chronic fatigue syndromeActa Otolaryngol199511519177762393
- BadhamSPHutchinsonCVCharacterising eye movement dysfunction in myalgic encephalomyelitis/chronic fatigue syndromeGraefes Arch Clin Exp Ophthalmol2013251122769277623918092
- BaraniukJNClauwDYutaANasal secretion analysis in allergic rhinitis, cystic fibrosis, and nonallergic fibromyalgia/chronic fatigue syndrome subjectsAm J Rhinol19981264354409883301
- BaraniukJNZhengYRelationships among rhinitis, fibromyalgia, and chronic fatigueAllergy Asthma Proc201031316917820615318
- BershadEMUrfyMZCalvilloEMarked olfactory impairment in idiopathic intracranial hypertensionJ Neurol Neurosurg Psychiatry201485995996424474821
- BortoluzziMDi LauroLMariniGBenign intracranial hypertension with spinal and radicular pain. Case reportJ Neurosurg19825768338367143069
- BruceBBKedarSVan StavernGPIdiopathic intracranial hypertension in menNeurology200972430430918923135
- BurnetRBChattertonBEGastric emptying is slow in chronic fatigue syndromeBMC Gastroenterol2004413215619332
- BuskilaDSarzi-PuttiniPAblinJNThe genetics of fibromyalgia syndromePharmacogenomics200781677417187510
- CappuzzoJMHessRMMorrisonJFTransverse venous stenting for the treatment of idiopathic intracranial hypertension, or pseudotumor cerebriNeurosurg Focus2018451E11
- CaroXJGalbraithRGWinterEFEvidence of peripheral large nerve involvement in fibromyalgia: a retrospective review of EMG and nerve conduction findings in 55 FM subjectsEur J Rheumatol20185210411030185358
- CaroXJWinterEFDumasAJA subset of fibromyalgia patients have findings suggestive of chronic inflammatory demyelinating polyneuropathy and appear to respond to IVIgRheumatology200847220821118208823
- CarruthersBMvan de SandeMIde MeirleirKLMyalgic encephalomyelitis: International Consensus CriteriaJ Intern Med2011270432733821777306
- ChenCHYangTYLinCLDry eye syndrome risks in patients with fibromyalgia: a national retrospective cohort studyMedicine2016954e260726825913
- ChenLEliasGYostosMPStimecBFaselJMurphyKPathways of cerebrospinal fluid outflow: a deeper understanding of resorptionNeuroradiology201557213914725398655
- ClauwDJFibromyalgia: a clinical reviewJAMA2014311151547155524737367
- ÇobanKAydınEÖzlüoğluLNAudio-vestibular findings in increased intracranial hypertension syndromeJ Int Adv Otol201713110010428084997
- CvejicEBirchRCVollmer-ConnaUCognitive dysfunction in chronic fatigue syndrome: a review of recent evidenceCurr Rheumatol Rep20161852427032787
- de AraújoMPFariaACTakanoCCUrodynamic study and quality of life in patients with fibromyalgia and lower urinary tract symptomsInt Urogynecol J Pelvic Floor Dysfunct20081981103110718317663
- De BeckerPMcGregorNDe MeirleirKA definition-based analysis of symptoms in a large cohort of patients with chronic fatigue syndromeJ Intern Med2001250323424011555128
- De SimoneRRanieriAMontellaSIntracranial pressure in unresponsive chronic migraineJ Neurol201426171365137324781838
- DiasDNGMarquesMAABettiniSCPaivaEDSPrevalence of fibromyalgia in patients treated at the bariatric surgery outpatient clinic of Hospital de Clínicas do Paraná - CuritibaRev Bras Reumatol Engl Ed201757542543029037315
- DigreKBNakamotoBKWarnerJELangebergWJBaggaleySKKatzBJA comparison of idiopathic intracranial hypertension with and without papilledemaHeadache200949218519319222592
- EyskensJBNijsJWoutersKMoorkensGReduced gait automaticity in female patients with chronic fatigue syndrome: Case-control studyJ Rehabil Res Dev201552780581426745400
- FarhadKOaklanderALFibromyalgia and small-fiber polyneuropathy: what’s in a name?Muscle Nerve20181314611613
- FaroMSàez-FrancásNCastro-MarreroJAlisteLFernández de SevillaTAlegreJGender differences in chronic fatigue syndromeReumatol Clin2016122727726190206
- FinkelmeyerAHeJMaclachlanLBlamireAMNewtonJLIntracranial compliance is associated with symptoms of orthostatic intolerance in chronic fatigue syndromePLoS One2018137e020006829969498
- FitzcharlesMASte-MariePARampakakisESampalisJSShirYDisability in fibromyalgia associates with symptom severity and occupation characteristicsJ Rheumatol201643593193626980580
- FričREidePKComparative observational study on the clinical presentation, intracranial volume measurements, and intracranial pressure scores in patients with either Chiari malformation Type I or idiopathic intracranial hypertensionJ Neurosurg201712641312132227341045
- FriesnerDRosenmanRLobbBMTanneEIdiopathic intracranial hypertension in the USA: the role of obesity in establishing prevalence and healthcare costsObes Rev2011125e372e38020804521
- Garcia-MartinEGarcia-CampayoJPuebla-GuedeaMFibro-myalgia is correlated with retinal nerve fiber layer thinningPLoS One2016119e016157427584145
- García-PérezAEspinoMBarrioAPseudotumor cerebri associated with maxillary sinusitis: clinicopathological studyRev Neurol2000311454810948583
- GodtsDMoorkensGMathysenDGBinocular vision in chronic fatigue syndromeAm Orthopt J2016661929727799582
- GrovesMDMccutcheonIEGinsbergLEKyritsisAPRadicular pain can be a symptom of elevated intracranial pressureNeurology19995251093109510102441
- HakimADe WandeleIO’CallaghanCPocinkiARowePChronic fatigue in Ehlers-Danlos syndrome-hypermobile typeAm J Med Genet C Semin Med Genet2017175117518028186393
- HendersonFCAustinCBenzelENeurological and spinal manifestations of the Ehlers-Danlos syndromesAm J Med Genet C Semin Med Genet2017175119521128220607
- HigginsJNPPickardJDLeverAMLChronic fatigue syndrome and idiopathic intracranial hypertension: different manifestations of the same disorder of intracranial pressure?Med Hypotheses20171056928735654
- HigginsNPickardJLeverABorderline intracranial hypertension manifesting as chronic fatigue syndrome treated by venous sinus stentingJ Neurol Surg Rep2015762e244e24726623235
- HulensMDankaertsWStalmansIFibromyalgia and unexplained widespread pain: the idiopathic cerebrospinal pressure dysregulation hypothesisMed Hypotheses201811015015429317060
- HulensMRasschaertRDankaertsWStalmansIVansantGBruyninckxFSpinal fluid evacuation may provide temporary relief for patients with unexplained widespread pain and fibromyalgiaMed Hypotheses2018118555830037615
- JohnstonSCStainesDRMarshall-GradisnikSMEpidemiological characteristics of chronic fatigue syndrome/myalgic encephalomyelitis in Australian patientsClin Epidemiol201689710727279748
- JonesKDMaxwellCMistSDKingVDenmanMAGregoryWTPelvic floor and urinary distress in women with fibromyalgiaPain Manag Nurs201516683484026259883
- JosevEKJacksonMLBeiBSleep quality in adolescents with chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME)J Clin Sleep Med20171391057106628760189
- KapoorKGKatzSEGrzybowskiDMLubowMCerebrospinal fluid outflow: an evolving perspectiveBrain Res Bull200877632733418793703
- Kapusuz GencerZBalbaloğluÖÖzkırışMSaydamLDoes fibro-myalgia have an effect on hearing loss in women?Turk J Med Sci20174761699170229306226
- KaramanKGverović-AntunicaAZuljanIFamilial idiopathic intracranial hypertensionCroat Med J200344448048412950154
- KarapetyanAManvelyanHEHMTI-0116. Tension type primary headaches and fibromyalgia: strong correlationsJ Headache Pain201415S1C42
- KerenTLahatEPseudotumor cerebri as a presenting symptom of acute sinusitis in a childPediatr Neurol19981921531549744640
- KincaidORowinJIntracranial hypertension causing polyradiculopathy and late or absent F-wavesJ Neurol Neurosurg Psychiatry200677121384138617110754
- KleinschmidtJJDigreKBHanoverRIdiopathic intracranial hypertension: relationship to depression, anxiety, and quality of lifeNeurology200054231932410668690
- KoroschetzJRehmSEGockelUFibromyalgia and neuropathic pain-differences and similarities. A comparison of 3057 patients with diabetic painful neuropathy and fibromyalgiaBMC Neurol20111115521612589
- KravitzHMKatzRSFibrofog and fibromyalgia: a narrative review and implications for clinical practiceRheumatol Int20153571115112525583051
- KuchinadASchweinhardtPSeminowiczDAWoodPBChizhBABushnellMCAccelerated brain gray matter loss in fibromyalgia patients: premature aging of the brain?J Neurosci200727154004400717428976
- LevittAEGalorAChowdhuryAREvidence that dry eye represents a chronic overlapping pain conditionMol Pain201713174480691772930628814146
- MalleryRMFriedmanDILiuGTHeadache and the pseudotumor cerebri syndromeCurr Pain Headache Rep201418944625086688
- Martínez-CapoccioniGSerramito-GarcíaRMartín-BailónMGarcía-AllutAMartín-MartínCSpontaneous cerebrospinal fluid leaks in the anterior skull base secondary to idiopathic intracranial hypertensionEur Arch Otorhinolaryngol201727452175218128175991
- Martínez-LavinMLópezSMedinaMNavaAUse of the leeds assessment of neuropathic symptoms and signs questionnaire in patients with fibromyalgiaSemin Arthritis Rheum200332640741112833249
- Martínez-MartínezLAMoraTVargasAFuentes-IniestraMMartínez-LavínMSympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis: a review of case-control studiesJ Clin Rheumatol201420314615024662556
- MasriAJaafarANomanRGharaibehAAbabnehOHIntracranial hypertension in children: etiologies, clinical features, and outcomeJ Child Neurol201530121562156825762586
- MatachGCartryGAl HusseinHDesratsLGhalayiniAdi NolfoMIdiopathic intracranial hypertension and sphenoid sinusitis: is there any relationship?J Fr Ophtalmol2007302S:318
- MaxmenAThe invisible disabilityNature2018553141729300036
- McarthurCJGinTMclarenIMCritchleyJAOhTETeOGastric emptying following brain injury: effects of choice of sedation and intracranial pressureIntensive Care Med19952175735767593899
- MoosaAJoyMAKumarAExtensive radiculopathy: another false localising sign in intracranial hypertensionJ Neurol Neurosurg Psychiatry200475710801081
- Moreno-FernándezAMJiménez-CastellanosEIglesias-LinaresABueso-MadridDFernández-RodríguezAde MiguelMFibromyalgia syndrome and temporomandibular disorders with muscular pain. A reviewMod Rheumatol201727221021627539739
- MorrisPPBlackDFPortJCampeauNTransverse sinus stenosis is the most sensitive MR imaging correlate of idiopathic intracranial hypertensionAJNR Am J Neuroradiol201738347147728104635
- NorrisTHawtonKHamilton-ShieldJCrawleyEObesity in adolescents with chronic fatigue syndrome: an observational studyArch Dis Child20171021353927655658
- OaklanderALHerzogZDDownsHMKleinMMObjective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgiaPain2013154112310231623748113
- ObeidTAwadaAMousaliYNusairMMuhayawiSMemishSExtensive radiculopathy: a manifestation of intracranial hypertensionEur J Neurol20007554955311054141
- PalaniappanRSirimannaTPeripheral vestibular dysfunction in chronic fatigue syndromeInt J Pediatr Otorhinolaryngol2002641697212020917
- PamukONUmitHHarmandarOIncreased frequency of gastrointestinal symptoms in patients with fibromyalgia and associated factors: a comparative studyJ Rheumatol20093681720172419567625
- Pilar BamboMGarcia-MartinEGutierrez-RuizFStudy of perfusion changes in the optic disc of patients with fibromyalgia syndrome using new colorimetric analysis softwareJ Fr Ophtalmol201538758058725976129
- PuriBKJakemanPMAgourMRegional grey and white matter volumetric changes in myalgic encephalomyelitis (chronic fatigue syndrome): a voxel-based morphometry 3 T MRI studyBr J Radiol2012851015e270e27322128128
- RamírezMMartínez-MartínezLAHernández-QuintelaEVelazco-CasapíaJVargasAMartínez-LavínMSmall fiber neuropathy in women with fibromyalgia. An in vivo assessment using corneal confocal bio-microscopySemin Arthritis Rheum201545221421926094164
- RanieriACavaliereMSicignanoSFalcoPCautieroFde SimoneREndolymphatic hydrops in idiopathic intracranial hypertension: prevalence and clinical outcome after lumbar puncture. Preliminary dataNeurol Sci201738Suppl 1193196
- RavindranMKZhengYTimbolCMerckSJBaraniukJNMigraine headaches in chronic fatigue syndrome (CFS): comparison of two prospective cross-sectional studiesBMC Neurol20111113021375763
- RehmSEKoroschetzJGockelUA cross-sectional survey of 3035 patients with fibromyalgia: subgroups of patients with typical comorbidities and sensory symptom profilesRheumatology20104961146115220236955
- RhodusNLFrictonJCarlsonPMessnerROral symptoms associated with fibromyalgia syndromeJ Rheumatol20033081841184512913944
- RizziMRadovanovicDSantusPInfluence of autonomic nervous system dysfunction in the genesis of sleep disorders in fibro-myalgia patientsClin Exp Rheumatol201735Suppl 105(3)7480
- RobinsonLJDurhamJNewtonJLA systematic review of the comorbidity between temporomandibular disorders and chronic fatigue syndromeJ Oral Rehabil201643430631626549386
- RobinsonMECraggsJGPriceDDPerlsteinWMStaudRGray matter volumes of pain-related brain areas are decreased in fibromyalgia syndromeJ Pain201112443644321146463
- RodgersKRGuiJDinulosMBChouRCEhlers-Danlos syndrome hypermobility type is associated with rheumatic diseasesSci Rep2017713963628051109
- RodríguezATemblJMesa-GresaPMuñozMÁMontoyaPReyBAltered cerebral blood flow velocity features in fibromyalgia patients in resting-state conditionsPLoS One2017127e018025328700720
- RosenhallUJohanssonGOrndahlGEye motility dysfunction in chronic primary fibromyalgia with dysesthesiaScand J Rehabil Med19871941391453481474
- RoundRKeaneJRThe minor symptoms of increased intracranial pressure: 101 patients with benign intracranial hypertensionNeurology1988389146114642970600
- RuizEAlegreJGarcía QuintanaAMAlisteLBlázquezAFernández de SevillaTChronic fatigue syndrome: study of a consecutive series of 824 cases assessed in two specialized unitsRev Clin Esp2011211838539021794854
- SayılırSÇulluNDecreased olfactory bulb volumes in patients with fibromyalgia syndromeClin Rheumatol201736122821282428744789
- SchmidtCWienerEHoffmannJStructural olfactory nerve changes in patients suffering from idiopathic intracranial hypertensionPLoS One201274e3522122493741
- SchmidtEADespasFPavy-Le TraonAIntracranial pressure is a determinant of sympathetic activityFront Physiol201891129472865
- SimmsRWGoldenbergDLSymptoms mimicking neurologic disorders in fibromyalgia syndromeJ Rheumatol1988158127112733184073
- StanescuDBodaghiBHuongDLPseudotumor cerebri associated with Sjögren’s syndromeGraefes Arch Clin Exp Ophthalmol2003241433934212719998
- TawfikKOStevensSMMihalDRadiographic evidence of occult intracranial hypertension in patients with Ménière’s diseaseOtolaryngol Head Neck Surg2017157226026828349763
- TuncelSAYılmazEÇağlıBTekataşAÇelikYÜnlüMELumbar opening pressure and radiologic scoring in idiopathic intracranial hypertension: is there any correlation?Pol J Radiol20178270170529657636
- ÜçeylerNSommerCObjective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgiaPain20131541125692569
- ÜçeylerNSommerCFibromyalgia syndrome: a disease of the small nerve fibers?Z Rheumatol201574649049526169747
- VijBWhippleMOTepperSJMohabbatABStillmanMVincentAFrequency of migraine headaches in patients with fibromyalgiaHeadache201555686086525994041
- WallMCorbettJJFriedmanDILiuGDigreKRevised diagnostic criteria for the pseudotumor cerebri syndrome in adults and childrenNeurology2014832198200
- WallMKupersmithMJKieburtzKDNordic Idiopathic Intracranial Hypertension Study Group: The idiopathic intracranial hypertension treatment trial: clinical profile at baselineJAMA Neurol20147169370124756302
- WatsonNFBuchwaldDGoldbergJNoonanCEllenbogenRGNeurologic signs and symptoms in fibromyalgiaArthritis Rheum20096092839284419714636
- YriHMFagerlundBForchhammerHBJensenRHCognitive function in idiopathic intracranial hypertension: a prospective case-control studyBMJ Open201444e004376
- YriHMRönnbäckCWegenerMHamannSJensenRHThe course of headache in idiopathic intracranial hypertension: a 12-month prospective follow-up studyEur J Neurol201421121458146425070715
- ZurDNaftalievEKeslerAEvidence of multidomain mild cognitive impairment in idiopathic intracranial hypertensionJ Neuroophthalmol2015351263025383589