Abstract
Objective
We aimed to assess whether patients suffering from COPD have a higher prevalence of chronic back pain (neck and low back pain) than age-, sex-, and residence-matched non-COPD controls. We also aimed to identify which variables are associated with chronic neck pain (CNP) and chronic low back pain (CLBP) among COPD patients.
Methods
We carried out a retrospective case–control study using data obtained from the Spanish National Health Survey conducted in 2017.
Results
We analyzed data from 1034 COPD and 1034 matched non-COPD controls. The prevalence of CNP and CLBP was 38.20% and 45.16%, respectively, among COPD patients and 22.82% and 28.34% for non-COPD controls, respectively (p<0.001 for both). Multivariable analysis showed that COPD patients had a 1.62-fold (95% CI 1.50–1.74) higher risk of CNP and a 1.83-fold (95% CI 1.73–1.91) higher risk of CLBP than non-COPD controls. Experiencing one type of pain greatly increased the risk of having the other. Factors associated with the presence of both types of pain among COPD patients included female sex, “fair/poor/very poor” self-rated health, migraine or frequent headache and use of pain medication. Being aged from 70 to 79 years was a risk factor for CLBP, and suffering from a mental disorder was a risk factor for CNP.
Conclusion
The prevalence of CNP and CLBP was significantly higher among COPD patients than among non-COPD controls after adjusting for age, sex and other relevant clinical variables. Our findings add new data to the knowledge of chronic pain in COPD patients.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable and treatable condition that is characterized by persistent and often progressive airflow limitation, mainly associated with tobacco smoking. It is a leading cause of morbidity and mortality worldwide and induces a substantial economic and social burden. In addition, the prevalence and burden of COPD are projected to increase over the coming decades due to continued exposure to COPD risk factors and aging of the world population.Citation1
Symptoms, including dyspnea, cough, and sputum production, are relatively common in COPD patients and constitute risk factors for poor health-related quality of life and a decrease in their physical activity.Citation2 Most recently, chronic pain has been reported as a frequent symptom in these patients, in addition to the previous ones, and in turn, it can have a negative impact on the degree of dyspnea, physical activity, and quality of life of these patients.Citation3
Pain in patients with COPD can have different causes. Low back pain is one of the most common localizations.Citation4 Other body localizations of pain in these patients are the neck, trunk, and limbs.Citation5–Citation7 The potential mechanisms that can cause, contribute to, or maintain this symptom in individuals with COPD include the mechanical limitations of the movement of the chest wall as a result of hyperinflation, musculoskeletal disorders, postural deviations, osteoporosis, compression fractures, vertebral deformations, costovertebral arthropathy, side effects of prolonged use of steroids, the presence of comorbidities, and certain individual characteristics, such as gender and socioeconomic factors.Citation8
The incidence, severity, and risk factors for pain in patients with COPD are rather heterogeneous.Citation9 The prevalence rates for pain range between 21% and 82% among COPD patients, depending on factors such as the clinical context of the study population, sampling source, measurement instrument and study period.Citation8 Regarding severity, it has been reported that the pain experienced by COPD patients is stronger than that perceived by those without a respiratory disease or by patients with other chronic diseasesCitation10 and is comparable to the pain observed in oncologic patients at the terminal stage.Citation4,Citation11 However, in the few studies that have been conducted so far, various methods have been used to assess pain in COPD patients, which could lead to misinterpretation of the phenotype of this symptom and justify the wide range in the estimated prevalence of pain that has been reported.Citation12 Regarding risk factors, a recent study has highlighted the influence of age, sex, blood pressure, and obesity in some types of pain suffered by these patients.Citation13 Nevertheless, the role of other comorbidities in the presence of pain in COPD remains controversial.Citation14
These limitations highlight the need for additional research on the prevalence and characteristics associated with the occurrence of pain in COPD patients. Improving knowledge of these aspects is important and necessary to improve pain recognition and treatment in individuals with this disease.
Using the Spanish National Health Survey conducted in 2017 (SNHS2017), we aimed to assess whether patients suffering from COPD have a higher prevalence of chronic back pain (neck and low back pain) than age-, sex-, and residence-matched non-COPD controls. We also aimed to identify which variables are associated with chronic neck pain (CNP) and chronic low back pain (CLBP) among COPD patients.
Materials and Methods
Study Design
We designed a case–control study. The data used were obtained from the SNHS2017 conducted in Spain from October 2016 to October 2017. Details in the methodology can be found elsewhere.Citation15 Briefly, the SNHS2017 includes a representative sample of the Spanish population aged 15 years or older residing in main family dwellings. The sampling method is a stratified three-stage sampling: first stage units are the census tracts; the second stage units are the main family dwellings; in the third stage, an adult (aged ≥15 years) was randomly selected (Kish method) from each household to fill in the questionnaire.Citation15
The information collection method is computer-assisted personal interviews (CAPIs). For our investigation, we selected only persons aged 35 years or older. The reason for this cutoff point is the extremely low prevalence of COPD below this age.Citation16
Study Variables
In the SNHS2017, the self-reported presence of chronic conditions is collected using three consecutive questions: 1) Do you have or have you ever had any of the following diseases or heath conditions? 2) Have you suffered this disease/health condition in the past 12 months? And 3) Was this disease/health condition been diagnosed by a doctor? A card with a list of 32 conditions is shown to the person interviewed after the first question, and for those conditions reported by the participant, the second and third questions are completed consecutively for each specific condition.
Participants were asked if they suffered COPD, and only persons who answered affirmatively to the three questions used to identify the presence of this disease were considered “COPD sufferers”. The same method was used to identify participants who suffered CNP and CLBP.
All participants were informed by the interviewer, prior to answering these questions, that a “chronic disease or health condition” is one that has lasted for at least 6 months.Citation15
The independent variables analyzed and their categories are detailed in and and included age, sex, educational level, monthly income, living with a partner and self-rated health. The pain characteristics analyzed were pain intensity and the use of pain medication prescribed by a physician.
Table 1 Distribution According to Study Variable Among Patients with COPD and Age–Sex–Province of Residence-Matched Non-COPD Subjects
Table 2 Prevalence of Chronic Neck Pain and Chronic Low Back Pain Among COPD Subjects and Non-COPD Controls According to Pain Characteristics, Health Status and Lifestyles Variables
The same methods used to identify those with COPD, CNP and CLBP were used to determine the presence of self-reported asthma, heart disease, diabetes, high blood pressure, cancer, mental disorders (anxiety and/or depression) and migraine or frequent headache. Lifestyle variables included body mass index, physical exercise, tobacco use and alcohol consumption.
All the questions included in the SNHS2017 and explanations on how the questionnaires are conducted are described elsewhere.Citation15,Citation17
Case–Control Design
The prevalence of COPD among those aged 35 years or over in the SNHS2017 was 5.99%, with a mean age of 68.29 years (SD 13.58, SEM 0.623, CR 0.189). The mean age for those without COPD was significantly lower (p<0.001), 46.58 years (SD 18.58 SEM 0.399, CR 0.189). Given this large difference, it is necessary to match COPD patients with non-COPD subjects to obtain comparable populations. To do this, for every person with COPD (patient), we used the SNHS2017 database to identify a participant without COPD (control) with exactly the same age, sex and residence as the control. If more than one control was available for a patient, the selection was done randomly. We were able to find a matched control for each of the 1034 COPD participants identified in the SNHS2017.
Statistical Analysis
All results are shown and compared according to the presence of COPD. We estimated the prevalence of CNP and CLBP according to the study variables. As descriptive statistics for quantitate variables, we used means, standard deviations, standard error of the mean (SEM) and coefficient of variation (CV) and for qualitative variable proportions. To compare proportions between matched patients and controls, we used the McNemar test. A paired Student’s t-test was used to compare means. To assess the association between the study variables and the presence of CNP and CLBP within the two study populations (patients and controls), we used the Chi square test.
Multivariable conditional logistic regression models were constructed to estimate the risk of suffering CNP and CLBP among COPD patients versus non-COPD controls after adjusting for possible confounders.
Unconditional logistic regression models were used to identify which variables were independently associated with self-reported CNP and CLBP among COPD sufferers.
Variables included in multivariable models were those significant in the bivariate analysis and those previously reported as relevant by the scientific literature. These models were conducted following the recommendation of Hosmer et al.Citation18
The adjusted odds ratio (OR) with 95% confidence intervals (95% CI) is the measure of association provided by the multivariable models.
STATA 14.0 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. USA) was used for statistical analysis using the command “svy” for complex sample analyses. Significance was set at two-tailed α < 0.05.
Ethical Aspects
In accordance with the Spanish legislation, as we used a public access dataset with all data anonymous, it was not necessary to obtain the approval of an ethics committee. The database can be downloaded freely by anyone.Citation19
Results
We analyzed data from 1034 COPD- and 1034 matched non-COPD controls. The distribution of the study populations is shown in . No differences in the sociodemographic characteristics analyzed were found between patients and controls after matching. COPD patients reported worse self-rated health and a higher prevalence of asthma, heart disease, diabetes, high blood pressure, mental disorders and migraine or frequent headache than non-COPD controls. Obesity and current smoking were more frequent (28.63% vs 19.05% and 20.02% vs 15.19%, respectively) among COPD patients (p<0.001). Severe/extreme pain intensity and use of pain medication were also more prevalent in COPD subjects (p<0.001).
The prevalence of CNP and CLBP was 38.20% and 45.16% among COPD patients, respectively, and 22.82% and 28.34% among non-COPD controls, respectively (p<0.001 for both). After multivariable analysis, the ORs showed a significantly higher adjusted risk of self-reporting CNP (OR 1.62; 95% CI 1.50–1.74) and CLBP (OR 1.83, 95% CI 1.73–1.91) among COPD patients than non-COPD controls.
show the prevalence of CNP and CLBP among COPD subjects and non-COPD controls according to sociodemographic variables.
Figure 1 Prevalence of chronic neck pain (CNP) and chronic low back pain (CLBP) among COPD subjects and non-COPD controls according to age groups. *Significant difference (p<0.05) between COPD suffers and non-COPD sufferers.
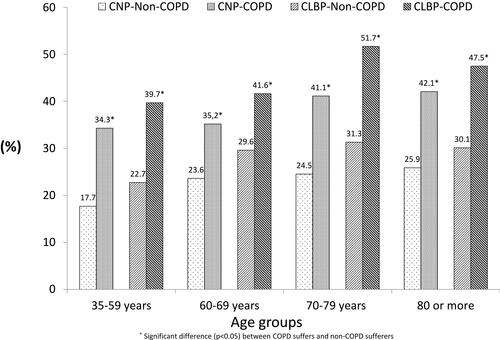
Figure 2 Prevalence of chronic neck pain (CNP) and chronic low back pain (CLBP) among COPD subjects and non-COPD controls according to gender and educational level. *Significant difference (p<0.05) between COPD suffers and non-COPD sufferers.
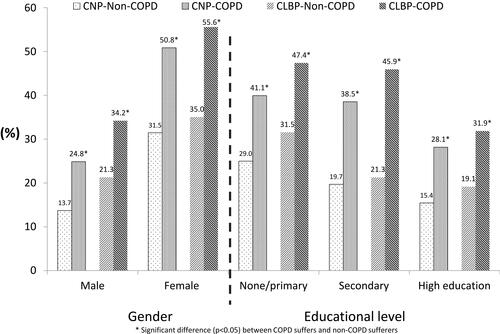
Figure 3 Prevalence of chronic neck pain (CNP) and chronic low back pain (CLBP) among COPD subjects and non-COPD controls according monthly income and living with a partner. *Significant difference (p<0.05) between COPD suffers and non-COPD sufferers.
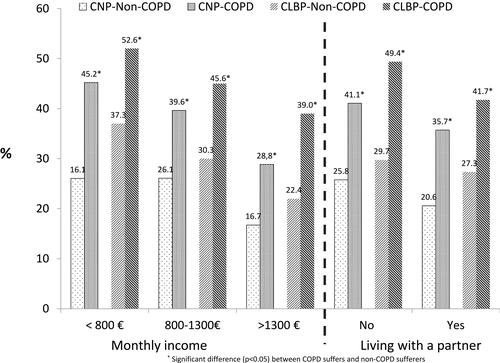
The prevalence of CNP and CLBP was significantly higher among COPD patients than among non-COPD controls for all the categories of the sociodemographic variables included in –.
Among COPD patients, the prevalence of CNP increased with age, from 34.30% in the lower age group to 42.08% in the highest. Women had two times higher values than men (50.85% vs 24.85%; p<0.001).
For CLBP, the highest prevalence among COPD patients was found in the age group of 70–79 years (51.70%), and the lowest was found in the age group of 35–59 years (39.71%). A total of 55.56% of women with COPD reported CLBP compared with 34.19% of non-COPD women (p<0.001).
As seen in , regarding pain characteristics, COPD sufferers with CNP or CLBP showed higher pain intensity, more use of pain medication and higher prevalence of migraine or frequent headache than controls. Compared with the controls, subjects with COPD had a higher prevalence of both CNP and CLBP for all the health status and lifestyle variables analyzed.
Among COPD controls, the prevalence of CNP was higher for those with worse self-rated health and suffering any of the diseases analyzed than among those with better self-rated health and not suffering these conditions. The highest prevalence of CNP for COPD patients was found among those suffering mental disorders (55.88%) and heart disease (51.36%).
Regarding lifestyles, a BMI of 30 kg/m2 or over and practicing less physical exercise were variables associated with a higher prevalence of CNP among COPD sufferers.
COPD patients experienced more severe CLBP if they had worse self-rated health or any of the clinical conditions analyzed than COPD patients with better self-rated health and not experiencing these conditions.
CLBP was reported by 61.40% of COPD patients with mental disease and over half of those with concomitant asthma (53.68%), heart disease (52.73%), high blood pressure (50.22%) or BMI ≥30 (50.68%).
The predictors for CNP and CLBP among COPD patients after multivariable adjustment are shown in . For CNP and CLBP, the probability of reporting these pains was significantly higher among women, those with “Fair/poor/very poor” self-rated health, pain medication users and those who reported migraine or frequent headache.
Table 3 Factors Associated with Suffering Chronic Neck Pain and Chronic Low Back Pain Among COPD Sufferers
For CNP, the risk increased significantly among COPD patients with mental disorders and among those who reported suffering concomitant CLBP.
Among COPD subjects, those aged 70–79 years old had a 1.67 times higher risk of CLBP than those aged 35–59 years old. Finally, concomitant CNP was a risk factor for CLBP.
Discussion
Our study demonstrated that COPD patients had a significantly higher risk of CNP and CLBP than non-COPD controls. In addition, we observed that experiencing one type of pain greatly increased the risk of having the other among individuals with COPD. Moreover, COPD patients with CNP and CLBP showed higher pain intensity, more use of pain medication and higher prevalence of migraine or frequent headache than controls without COPD.
The prevalence of CNP and CLBP in our study is consistent with previous studies.Citation14,Citation20 Greater pain in the COPD population could be due to more prolonged induction of painful stimuli or possibly to lower thresholds for this symptom compared to non-COPD controls. Possible etiologies include systemic inflammation, central adaptations related to pain and dyspnea, and musculoskeletal conditions.Citation6
Among COPD patients, being aged between 70 and 79 years was associated with a higher risk of CNP than being aged between 35 and 59 years old. Regarding gender, female sex was a risk factor for CNP and CLBP. This finding is consistent with other authors who have also reported a higher prevalence of pain in women than in men.Citation21 Christiansen et alCitation11 also reported a higher frequency of pain in women with COPD than in men with this disease. Possible explanations to justify the differences in pain between women and men include neuroimmunological, hormonal, genetic, and psychological factors.Citation22 Furthermore, questions have also been raised as to whether men and women construct different meanings around pain, which may influence the way they report their experience of this symptom.Citation23
Previous studies have shown that mental disorders are positively associated with subsequent back/neck pain onset.Citation24 We found higher probabilities of CNP in COPD patients with mental disorders, but we did not detect an association between mental disorders and CLBP. The relationship between chronic pain and mental disorders is complex and could be related to the neuroanatomical and functional overlap between pain and emotion/reward/motivation brain circuits.Citation25 Behavior-related mechanisms could also be relevant, since mental disorders are related to being sedentary and worse diets, leading to dyslipidemia and obesity, causing inflammation, which is in turn associated with both pain and psychiatric morbidity. Other lifestyle-related behaviors, such as occupational stress and tobacco smoking, may also contribute to psychoimmune dysfunctions and inflammation.Citation24
Our results are in line with earlier studies reporting that pain is negatively associated with health-related quality of life and health status in patients with stable COPD.Citation6,Citation7,Citation9,Citation26,Citation27 Thus, COPD patients with poorer self-rated health had a significantly higher risk of CNP and CLBP than those with a better perception of their health. Van Dam van Issel et alCitation28 also showed that COPD patients with pain had a significantly and clinically relevant worse health status, attributed to the functional domain.
A relationship between migraine or severe headache and chronic health conditions, including COPD, has been reported in previous studies.Citation29 Our study further confirms that suffering from migraine or frequent headache is a risk factor for CNP and CLBP among COPD patients. These results corroborate previous reports indicating that headache or migraine is often associated with other musculoskeletal pains, including neck and back pains.Citation30,Citation31 Furthermore, an increased number of comorbid pains has been significantly associated with a lower level of perceived general health.Citation29
The probability of reporting CNP and CLBP in COPD patients in our study was significantly higher among pain medication users. Roberts et alCitation32 reported that COPD patients have substantially more utilization of pain medications than those with most other chronic diseases. In addition, they found that compared with patients with chronic disease other than COPD, individuals with COPD had a 47% higher prevalence of chronic use of pain or pain-related outpatient prescription medications and a 27% higher prevalence of chronic use of short-acting or long-acting opioid medications.Citation33
We did not find a relationship between obesity and physical activity with the appearance of CNP and CLBP in patients with COPD in our study. In contrast, HajGhanbart et alCitation6 demonstrated that pain in the COPD population is associated with decreased physical activity and higher BMI. Pain-inducing activity limiting factors in these patients include comorbidities (ie, osteoporosis and osteoarthritis), specific medications (such as beta-2 agonists that can cause cramps in the calf muscles) and symptoms of deconditioning.Citation34–Citation36 However, we did not collect information on musculoskeletal comorbidities, medication for COPD or symptoms of deconditioning, so we cannot assess this relationship. On the other hand, it has been suggested that obesity increases the prevalence of pain by increasing pro-inflammatory cytokines and increasing the risk of osteoarthritis.Citation37 In a vicious cycle, this symptom may also increase the risk of obesity by causing reductions in physical activity or hormonal changes.Citation6
The strengths of this population-based study include a matched case–control design, the use of standardized surveys, and training of the data collectors. A matched case––control design is effective to avoid the confounding effect of age, sex and province of residence. Furthermore, the novelty of our work is that we analyzed sociodemographic variables that are not collected in clinical records and self-reported lifestyles and pain characteristics, variables that are not usually collected with standardized methods in the clinical settings. Furthermore, we used a large (over 1000 subjects) representative sample of the entire Spanish population suffering from COPD rather than a selected sample from one or several hospitals or primary care centers; in our opinion, this provides great external validity to our results.
While the analysis was rigorous, our findings have several limitations. First, comorbid COPD and CLBP/CNP may have various causal links (ie, depression, discopathy, inflammation, overweight/obesity) and consequences (ie, reduction in physical activity, therapy compliance, quality of life), which could not be fully investigated given the limited information collected by the SNHS2017. Furthermore, cross-sectional designs suffer from the possibility of reverse causality bias; therefore, we can identify significant associations but not establish risk factors or causality. Further prospective studies with more clinical variables are needed to confirm our results. Second, the only source to assess information on the types of pain analyzed is self-reporting; therefore, under- or overreporting may appear because of recall, information or social desirability biases. Third, we were able to adjust for a large number of potential confounding factors in the multivariate analyses, but the possibility of residual confounding by unrecognized factors cannot be definitively ruled out. Fourth, the specific characteristics of COPD are not collected in the SNHS2017, including severity of airway obstruction, disease duration or treatments. However, none of the included studies on pain or symptom burden in a recent meta-analysis reported a significant relationship between lung function and pain prevalence or severity.Citation14 Fifth, the validity of the self-reported conditions included in the SNHS2017 has not been evaluated, which could have resulted in misclassification of patients in the analysis.
Conclusions
In conclusion, the prevalence of CNP and CLBP was significantly higher among COPD patients than among non-COPD controls. In addition, suffering one of the pains greatly increased the risk of having the other and vice versa. Associated factors with suffering these types of pain among COPD subjects included age 70 to 79 years (only for CLBP), being female, having mental disorder (only for CNP), having worse self-rated health, suffering migraine or frequent headache, and using pain medication. Our findings add new data to the knowledge of chronic pain in COPD patients and justify its inclusion in clinical practice guidelines for this disease.
Disclosure
The authors declare no conflicts of interest.
Additional information
Funding
References
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2020. Available from: https://www.goldcopd.org. Accessed April 27, 2020.
- Brown R. Control of COPD symptoms: addressing an unmet need. J Fam Pract. 2016;65(12 Suppl).
- De Miguel Díez J, Jiménez García R, López de Andrés A. Living with COPD: pain is important too. Arch Bronconeumol. 2019;56(6):351–352.
- Chen YW, Camp PG, Coxson HO, et al. Comorbidities that cause pain and the contributors to pain in individuals with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2017;98:1535–1543. doi:10.1016/j.apmr.2016.10.016
- Bentsen SB, Rustøen T, Miaskowski C. Prevalence and characteristics of pain in patients with chronic obstructive pulmonary disease compared to the Norwegian general population. J Pain. 2011;12:539–545. doi:10.1016/j.jpain.2010.10.014
- HajGhanbari B, Holsti L, Road JD, et al. Pain in people with chronic obstructive pulmonary disease (COPD). Respir Med. 2012;106:998–1005. doi:10.1016/j.rmed.2012.03.004
- Borge CR, Wahl AK, Moum T. Pain and quality of life with chronic obstructive pulmonary disease. Heart Lung. 2011;40:e90–101. doi:10.1016/j.hrtlng.2010.10.009
- Lewthwaite H, Williams G, Baldock KL, et al. Systematic review of pain in clinical practice guidelines for management of COPD: a case for including chronic pain? Healthcare (Basel). 2019;7:15. doi:10.3390/healthcare7010015
- Bentsen SB, Miaskowski C, Cooper BA, et al. Distinct pain profiles in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2018;13:801–811. doi:10.2147/COPD.S150114
- Bordoni B, Marelli F, Morabito B, et al. Chest pain in patients with COPD: the fascia’s subtle silence. Int J Chron Obstruct Pulmon Dis. 2018;13:1157–1165. doi:10.2147/COPD.S156729
- Christensen VL, Holm AM, Kongerud J, et al. Occurrence, characteristics, and predictors of pain in patients with chronic obstructive pulmonary disease. Pain Manag Nurs. 2016;17:107–118. doi:10.1016/j.pmn.2016.01.002
- Johnson AM, Smith SM. A review of general pain measurement tools and instruments for consideration of use in COPD clinical practice. Int J Chron Obstruct Pulmon Dis. 2017;12:923–929. doi:10.2147/COPD.S119889
- De Miguel-díez J, López-de-Andrés A, Hernandez-Barrera V, et al. Prevalence of pain in COPD patients and associated factors: report from a population-based study. Clin J Pain. 2018;34:787–794. doi:10.1097/AJP.0000000000000598
- Van Dam van Isselt EF, Groenewegen-Sipkema KH, Spruit-van Eijk M, et al. Pain in patients with COPD: a systematic review and meta-analysis. BMJ Open. 2014;4:e005898. doi:10.1136/bmjopen-2014-005898
- Instituto Nacional de Estadística. Encuesta Nacional de Salud 2017. [National health survey 2017]. Available from: https://www.ine.es/en/metodologia/t15/t153041917_en.pdf. Accessed March 11, 2020.
- Force GT. Clinical practice guideline for the diagnosis and treatment of patients with chronic obstructive pulmonary disease (COPD) – the Spanish COPD guideline (GesEPOC). Arch Bronconeumol. 2017;53:S2–S64.
- Instituto Nacional de Estadistica. Encuesta Nacional de Salud 2017. Cuestinario de adultos [National health survey 2017. Adults questionnaire]. Available from: https://www.ine.es/metodologia/t15/ense_adu17.pdf. Accessed March 11, 2020.
- Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed. New Jersey, USA: John Wiley & Sons, Inc; 2013.
- Ministerio de Sanidad Consumo y Bienestar Social. Encuesta Nacional de Salud 2017. Microdatos. [National health survey 2017. Microdata]. Available from: https://www.mscbs.gob.es/estadisticas/microdatos.do. Accessed March 11, 2020.
- Sánchez Castillo S, Smith L, Díaz Suárez A, et al. Associations between physical activity and comorbidities in people with COPD residing in Spain: a cross-sectional analysis. Int J Environ Res Public Health. 2020;17(2):594. doi:10.3390/ijerph17020594
- Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111:52–58. doi:10.1093/bja/aet127
- Andenæs R, Momyr A, Brekke I. Reporting of pain by people with chronic obstructive pulmonary disease (COPD): comparative results from the HUNT3 population-based survey. BMC Public Health. 2018;18:181. doi:10.1186/s12889-018-5094-5
- Unruh AM. Gender variations in clinical pain experience. Pain. 1996;65:123–167. doi:10.1016/0304-3959(95)00214-6
- Viana MC, Lim CCW, Garcia Pereira F, et al. Previous mental disorders and subsequent onset of chronic back or neck pain: findings from 19 countries. J Pain. 2018;19:99–110. doi:10.1016/j.jpain.2017.08.011
- Elman I, Zubieta JK, Borsook D. The missing p in psychiatric training: why it is important to teach pain to psychiatrists. Arch Gen Psychiatry. 2011;68:12–20. doi:10.1001/archgenpsychiatry.2010.174
- Janssen DJ, Wouters EF, Parra YL, et al. Prevalence of thoracic pain in patients with chronic obstructive pulmonary disease and relationship with patient characteristics: a cross-sectional observational study. BMC Pulm Med. 2016;16:47. doi:10.1186/s12890-016-0210-8
- Lee AL, Goldstein RS, Brooks D. Chronic pain in people with chronic obstructive pulmonary disease: prevalence, clinical and psychological implications. Chronic Obstr Pulm Dis. 2017;4:194–203.
- Van Dam van Isselt EF, Groenewegen-Sipkema KH, van Eijk M, et al. Pain in patients with chronic obstructive pulmonary disease indicated for post-acute pulmonary rehabilitation. Chron Respir Dis. 2019;16:1479972318809456. doi:10.1177/1479972318809456
- Minen MT, Weissman J, Tietjen GE. The relationship between migraine or severe headache and chronic health conditions: a cross-sectional study from the national health interview survey 2013–2015. Pain Med. 2019;20:2263–2271. doi:10.1093/pm/pnz113
- Scher AI, Bigal ME, Lipton RB. Comorbidity of migraine. Curr Opin Neurol. 2005;18:305–310. doi:10.1097/01.wco.0000169750.52406.a2
- Scher AI, Stewart WF, Lipton RB. The comorbidity of headache with other pain syndromes. Headache. 2006;46:1416–1423. doi:10.1111/j.1526-4610.2006.00584.x
- Roberts MH, Mapel DW, Thomson HN. The impact of chronic pain on direct medical utilization and costs in chronic obstructive pulmonary disease. Clinicoecon Outcomes Res. 2015;7:173–184. doi:10.2147/CEOR.S80424
- Roberts MH, Mapel DW, Hartry A, et al. Chronic pain and pain medication use in chronic obstructive pulmonary disease. A cross-sectional study. Ann Am Thorac Soc. 2013;10:290–298. doi:10.1513/AnnalsATS.201303-040OC
- Ferguson GT, Calverley PMA, Anderson JA, et al. Prevalence and progression of osteoporosis in patients with COPD: results from the towards a revolution in COPD health study. Chest. 2009;136:1456–1465. doi:10.1378/chest.08-3016
- O’Donnell DE, Hernandez P, Kaplan A, et al. Canadian thoracic society recommendations for management of chronic obstructive pulmonary disease - 2008 update - highlights for primary care. Can Respir J. 2008;15:1A–8A.
- Wagner PD. Skeletal muscles in chronic obstructive pulmonary disease: deconditioning, or myopathy? Respirology. 2006;11:681–686. doi:10.1111/j.1440-1843.2006.00939.x
- Steultjens MP, Dekker J, van Baar ME, et al. Muscle strength, pain and disability in patients with osteoarthritis. Clin Rehabil. 2001;15:331–341. doi:10.1191/026921501673178408
