Abstract
Background
While chronic neck pain is a common problem in the adult population, with a typical 12-month prevalence of 30%–50%, there is a lack of consensus regarding its causes and treatment. Despite limited evidence, cervical epidural injections are one of the commonly performed nonsurgical interventions in the management of chronic neck pain.
Methods
A randomized, double-blind, active, controlled trial was conducted to evaluate the effectiveness of cervical interlaminar epidural injections of local anesthetic with or without steroids for the management of chronic neck pain with or without upper extremity pain in patients without disc herniation, radiculitis, or facet joint pain.
Results
One hundred and twenty patients without disc herniation or radiculitis and negative for facet joint pain by means of controlled diagnostic medial branch blocks were randomly assigned to one of two treatment groups, ie, injection of local anesthetic only (group 1) or local anesthetic mixed with nonparticulate betamethasone (group 2). The primary outcome of significant pain relief and improvement in functional status (≥50%) was demonstrated in 72% of group 1 and 68% of group 2. The overall average number of procedures per year was 3.6 in both groups with an average total relief per year of 37–39 weeks in the successful group over a period of 52 weeks.
Conclusion
Cervical interlaminar epidural injections of local anesthetic with or without steroids may be effective in patients with chronic function-limiting discogenic or axial pain.
Introduction
Chronic pain in the US has reached crisis levels, with an explosion of diagnostic and therapeutic measures.Citation1 Chronic spinal pain is common in the general adult population, with low back and neck pain constituting the majority of the disorders.Citation2–Citation6 All modalities of treatment, including cervical spine surgery and cervical epidural injections, have risen dramatically over the past two decades.Citation3,Citation7–Citation17 Studies of the prevalence of chronic neck pain and its impact on general health have shown that 14% of patients report grade II–IV neck pain, with a high pain intensity leading to disability, with grade 0 referring to no neck pain; grade I representing pain of low intensity and few activity limitations; grade II with pain of high intensity, but few activity limitations; grade III with pain of high intensity and high levels of disability associated with moderate limitations in activities; and grade IV referring to pain with high levels of disability and several activity limitations.Citation5,Citation6 Further, chronic recurrent neck pain is a common problem in the adult population, with a typical 12-month prevalence of 30%–50%.Citation2,Citation4,Citation16 Apart from cervical disc herniation, cervical facet joint and discogenic pain are the common causes, resulting in chronic mechanical neck pain with or without upper extremity pain.Citation2,Citation3,Citation16–Citation18 Thus, pain emanating from a degenerative disc may result in discogenic pain secondary to chemical irritation or predominantly axial pain secondary to internal disc disruption. Citation19–Citation21 Axial neck pain may be related to either a disc or facet joint, or be musculoligamentous. However, there is a lack of consensus regarding the causes and treatment of chronic neck pain without disc herniation and radiculitis.
Among the various treatments available for managing axial discogenic pain, epidural injections are one of the most common nonsurgical interventions.Citation3,Citation16,Citation22–Citation28 In general, cervical epidural injections are not recommended for axial neck pain, but they are considered to be reasonable in disc herniation with radiculitis and spinal stenosis. The evidence for cervical epidural injections in disc herniation and radiculitis, though debated, is moderate.Citation3 The evidence for epidural injection in axial discogenic pain is based on a single preliminary report of discogenic neck pain after excluding cervical facet joint pain in patients without disc herniation or radiculitis.Citation23 In this trial, 70 patients were included, with 35 patients receiving local anesthetics only and the other 35 receiving local anesthetics with nonparticulate betamethasone. The results showed significant pain relief (≥50%) in 80% of the patients in both groups, along with improvement in functional status (≥50%) in 69% in group 1 (receiving local anesthetic only) and 80% in group 2 (also receiving steroids). In fact, the results of this preliminary evaluation were similar to those for disc herniation in the cervical spine,Citation22 lumbar spine,Citation29,Citation30 thoracic spine,Citation31 and discogenic pain in the lumbar spine,Citation32,Citation33 and superior to the results for spinal stenosis and post surgery syndrome in the lumbar and cervical spine.Citation24,Citation25,Citation34–Citation36
The underlying mechanism of action of epidurally administered local anesthetics and steroids is not clear, and is believed to be due to the anti-inflammatory properties of corticosteroids, but the evidence also indicates that local anesthetics may be as effective as steroids in managing spinal pain of various origins.Citation22–Citation25,Citation29–Citation39 Based on the clinical and experimental evidence, it appears that local anesthetics and steroids may provide long-term relief.Citation40–Citation47
This study was undertaken to evaluate the role of cervical interlaminar epidural injections of local anesthetics with or without steroids in patients with chronic, function-limiting neck pain with or without upper extremity pain secondary to discogenic pain without disc herniation, radiculitis, or facet joint pain. This report consists of the results of 120 patients at one-year follow-up, and is a continuation of a published preliminary report.Citation23
Materials and methods
The study was conducted in an interventional pain management practice, ie, a specialty referral center, in a private practice setting in the United States, based on Consolidated Standards of Reporting Trials guidelines.Citation48 The study protocol was approved by the local institutional review board and was registered with the US Clinical Trial Registry (NCT01071369). This study was conducted with the internal resources of the practice without any external funding either from industry or from elsewhere. All ethical guidelines were followed.
Participants
Patients were recruited from new patients presenting for interventional pain management. All patients were provided with the IRB-approved protocol and informed consent which described in detail all aspects of the study and withdrawal process.
Interventions
The patients were assigned to one of two groups, ie, group 1, in which patients received cervical interlaminar epidural injections of local anesthetic (lidocaine 0.5%, 5 mL), and group 2, in which patients received cervical interlaminar epidural injections comprising 4 mL of lidocaine 0.5% mixed with 1 mL or 6 mg of nonparticulate betamethasone for a total of 5 mL of injectate.
Pre-enrollment evaluation
Initially, all patients with axial pain underwent controlled comparative local anesthetic blocks to exclude facet joint pain.Citation49,Citation50 In addition, patient demographic data, medical and surgical history with coexisting disease(s), radiologic investigations, physical examination, pain rating scores using the Numeric Rating Scale (NRS), work status, opioid intake, and functional status assessment by the Neck Disability Index (NDI) were also collected.
Inclusion criteria
Inclusion criteria were: lack of a diagnosis of cervical facet joint pain by means of controlled, comparative local anesthetic blocks and an absence of cervical disc herniation or radiculitis; at least 18 years of age; a history of chronic function-limiting neck and upper extremity pain of at least 6 months duration; and ability to understand the study protocol and provide voluntary, written, informed consent. In addition, patients should have failed conservative management, including, but not limited to, physical therapy, medical therapy, and a structured exercise program.
Exclusion criteria
Exclusion criteria were: presence of cervical disc herniation; radiculitis secondary to spinal stenosis without disc herniation; uncontrollable or unstable opioid use; uncontrolled psychiatric disorders; uncontrolled medical illness, either acute or chronic; any conditions that could interfere with the interpretation of the outcome assessments; pregnant or lactating women; and a history or potential for adverse reaction(s) to local anesthetics or steroids.
Description of interventions
Diagnostic facet joint nerve blocks were performed on two different occasions utilizing short-acting and long-acting local anesthetics, specifically 0.5 mL of 1% preservative-free lidocaine on the first occasion, and 0.25% preservative-free bupivacaine on the second occasion. The patient’s response was considered positive if pain relief lasted more than two hours following lidocaine injection and lasted at least three hours or more or longer than the duration of relief with lidocaine when bupivacaine was used, plus the ability to perform previously painful movements.
Cervical interlaminar epidural procedures were performed under fluoroscopy in a sterile operating room with patients in the prone position, appropriate monitoring, and intravenous access and sedation as medically necessary by one physician (LM). The epidural space was identified using the loss of resistance technique under fluoroscopic visualization. The epidural space was entered between C7–T1 and C5–C6 with confirmation by injection of nonionic contrast medium. Following confirmation of the epidural space, we performed clear solution injections of 5 mL of preservative-free lidocaine hydrochloride 0.5% or 4 mL of preservative- free lidocaine mixed with 6 mg of nonparticulate betamethasone.
Additional interventions
Repeat cervical epidural injections were provided when increased levels of pain were reported with deteriorating relief below 50%. A patient was unblinded if requested or if an emergency situation arose. Patients who were nonresponsive and continued with conservative management were followed without further epidural injections and medical management, unless they requested unblinding. There was no specific physical therapy, occupational therapy, bracing, or further interventions offered other than the study intervention. All patients continued drug therapy, exercise programs, as well as their work.
Objectives and outcomes
The study was designed to evaluate objectively the effectiveness of cervical epidural injections with or without steroids for managing chronic neck and upper extremity pain secondary to discogenic pain without disc herniation, radiculitis, or facet joint pain. Outcomes measured included NRS, NDI, work status, and opioid intake in terms of morphine equivalents, assessed at baseline and at 3, 6, and 12 months following treatment. The primary outcome was defined as at least 50% pain relief associated with 50% improvement in NDI. The NRS and NDI have been shown to be valid and reliable in patients with mechanical neck pain.Citation51–Citation55 Opioid intake was evaluated with conversion to morphine equivalents.Citation56 Patients unemployed or employed on a part-time basis with limited or no employment due to pain were classified as employable. Patients who chose not to work, were retired, or were homemakers (not working, but not due to pain) were not considered to be in the employment pool.
Randomization and blinding
From a total of 120 patients, 60 were randomly assigned into each group. Randomization was performed by computer-generated random allocations sequence by, simple randomization. The operating room nurse assisting with the procedure randomized the patients and prepared the drugs appropriately to ensure allocation concealment. The patients and the physician were blinded to group assignment. Both solutions were clear and it was impossible to identify if the steroid had been added or not. Further, blinding was also assured by mixing the patients with other patients receiving routine treatment and not informing the physician performing the procedure of the inclusion of the patients in the study. All the patients chosen for one-year follow-up were selected by a statistician who did not provide patient care. The unblinding results were not disclosed to either the treating physician, other health care providers, or patients. Thus, the nature of blinding was not interrupted.
Statistical methods
Sample size was calculated based on significant pain relief. Considering a 0.05 two-sided significance level, a power of 80%, and an allocation ratio of 1:1, 55 patients in each group were estimated to be necessary;Citation57 allowing for a 10% attrition/ noncompliance rate, 60 patients were required. Statistical analysis included the Chi-squared statistic, Fisher exact test, t-test, and paired t-test. Results were considered statistically significant if the P value was less than 0.05. The Chi- squared statistic was used to test the differences in proportions. Fisher exact test was used wherever the expected value was less than 5; a paired t-test was used to compare the pretreatment and post-treatment results of average pain scores and NDI measurements at baseline versus 3, 6, and 12 months. For comparison of mean scores between groups, the t-test was performed. An intent-to-treat-analysis was performed. Either the last follow-up data or initial data were utilized for patients who dropped out of the study and for whom no other data were available. Sensitivity analysis was performed utilizing best case, worst case, and last follow-up score scenarios.
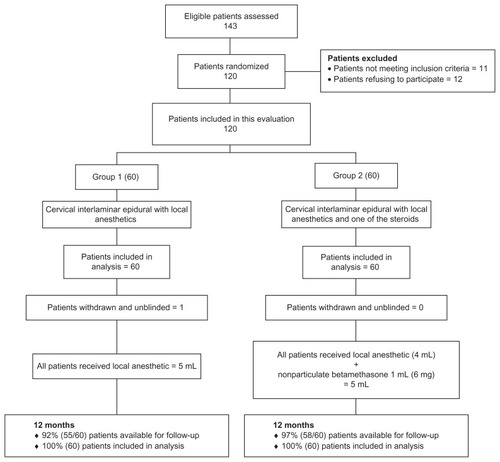
illustrates the patient flow. Recruitment lasted from August 2007 through June 2010. Baseline demographic and clinical characteristics for each group are summarized in . shows the NRS scores and the proportion of patients with ≥50% pain relief in each category. Functional assessment results assessed by the NDI are shown in . shows the pain relief and functional status assessment in all patients, including both failed and successful patients.
Figure 2 Proportion of patients with significant reduction in Numeric Rating Scale and Neck Disability Index (≥50% reduction from baseline).
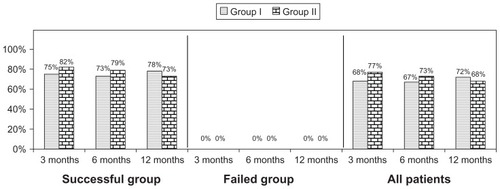
Table 1 Baseline demographic characteristics
Table 2 Characteristics of pain relief on Numeric Rating Scale and proportion of patients with significant relief
Table 3 Illustration of functional assessment scores by Neck Disability Index and proportion of patients with significant (≥50%) improvement
Characteristics of the therapeutic procedure
The characteristics of the therapeutic procedure are summarized in . Epidural entry was in the vertebral interspaces as follows: 33% between C7 and T1, 58% between C6 and C7, and 9% between C5 and C6. No significant differences were noted in average relief per year; in group 1, the average relief was for 36.4 ± 15.9 weeks and in group 2 it was 34.8 ± 16.1 weeks. The total number of injections per year were 3.6 ± 1.1 in group 1 and 3.6 ± 1.0 in group 2. However, when patients were separated into successful and failed groups, the total number of injections per year was 3.7 ± 0.9 for both successful groups, with total relief for 39.2 ± 13.2 weeks in group 1 and for 37.3 ± 13.7 weeks in group 2. In contrast, total relief was for 5.2 ± 8.4 and for 0.8 ± 1.0 weeks in the failed groups. Epidurals were considered to be successful if a patient obtained consistent relief with two initial injections for at least 3 weeks. All others were considered as failures.
Table 4 Therapeutic procedural characteristics with procedural frequency, average relief per procedure, and average total relief in weeks over a period of one year
Employment characteristics
demonstrates employment characteristics in both groups. Among the patients eligible for employment, the total number of employed changed from 10 at baseline to 17 at the end of 12 months in group 1, and changed from 19 to 21 in group 2, representing a significant increase from 48% to 77% in group 1 and a nonsignificant increase from 66% to 75% in group 2.
Table 5 Employment characteristics
Opioid intake
illustrates opioid intake characteristics.
Table 6 Opioid intake (morphine equivalence mg)
Weight changes
There were no differences in change (gain or loss) in body weight from baseline in both groups () even though there was a significant difference at baseline.
Table 7 Patterns of weight change
Adverse events
Of the 434 cervical epidural procedures performed, one subarachnoid puncture was reported. Nerve root irritation was observed in three patients without long-term sequelae. All patients experiencing nerve root irritation, even though transient, were given dexamethasone 8 mg intravenously.
Discussion
This report of the one-year follow-up of a randomized, active controlled trial of 120 patients with axial or discogenic neck pain without evidence of facet joint pain demonstrates significant improvement, with improvement in pain relief and functional status in 72% of patients in group 1 who received local anesthetic only and in 68% of patients in group 2 who received local anesthetics and steroids. In the successful group, significant improvement was seen in 78% who received local anesthetic only, whereas in the group who also received steroids, the improvement was 73%. Overall, the average number of procedures per year was 3 to 4, with an average duration of total relief per year of 36.4 ± 15.9 weeks in group 1 and 34.8 ± 16.1 weeks in group 2, over a period of 52 weeks. Opioid intake was significantly reduced in group 1 from baseline. In addition, employment also increased significantly in group 1, but there was also a nonsignificant increase in group 2. Regarding employment characteristics, it is difficult to differentiate between those seeking work during a recession and those who are unable to work. Further, the number of patients unemployed due to pain decreased from 6 to 2 in group 1 and 6 to 4 in group 2.
There was no significant difference among the patients receiving steroids and those who did not. Both groups showed similar significant improvement. The results were also similar to both the preliminary results of this study and to the results of a similar studyCitation32,Citation33 in the lumbar spine. There were no significant differences noted among the groups, whether they were receiving steroids or not, with respect to weight.
There is a paucity of literature with respect to epidural injections, specifically in managing axial or discogenic neck pain. There have been only two systematic reviews.Citation3,Citation58 However, these reviews included only studies evaluating cervical epidural injections in disc herniation and radiculitis. Further, these were also performed under fluoroscopy. Since the publication of these systematic reviews, multiple studies have been published evaluating the role of cervical epidural injections in various conditions performed with fluoroscopy.Citation22–Citation25 The results of this evaluation are similar to the results in disc herniation, either in the cervical or lumbar spine.Citation29,Citation30,Citation32–Citation36 Overall, this study also provides insight into successful or failed groups based on positive procedures, even though the proportion of patients in the failed group was low, with only five in group 1 and four in group 2 out of 60 patients in each group. Overall, successful patients fared better even though there was no significant difference.
This trial has multiple strengths and limitations. The strengths include it being a practical clinical trial with a fairly large number of patients with an active-control design performed under fluoroscopy and repeat injections provided only upon return of pain and deterioration of functional status. In an era of comparative effectiveness and evidence-based medicine,Citation59–Citation63 the current study, though limited to a single center, provides evidence generalizable to contemporary interventional pain management settings. Patient selection was undertaken with great sensitivity, including only patients with axial neck pain but without facet joint pain. Thus, it may be considered that the study meets the criteria for pragmatic or practical clinical trials with an active-control group instead of a placebo group and for measuring effectiveness, which is more appropriate than explanatory trials that measure efficacy.Citation55,Citation64–Citation67
Limitations include the lack of a placebo group. Having a placebo group has been a controversial issue in interventional pain management and is widely debated.Citation68–Citation74 Placebo interventions have been misinterpreted based on the solution injected and the location of the injection, with some even interpreting local anesthetic injection as placebo, not realizing that inactive substances injected into active structures tend to result in various types of effects.Citation74–Citation78 Further, the only appropriate placebo design, reported by Ghahreman et al,Citation73 showed no significant effect when sodium chloride solution was injected into an inactive structure (injection of an inactive substance into an inactive structure), ie, a true placebo. The other limitation in this study includes the slightly higher weight of the patients in group 1 compared with group 2. However, this is not expected to have caused any variations in outcomes of the study.
The implications of this trial for health care are enormous considering exploding health care costs and the emphasis on comparative effectiveness research and evidence-based medicine. As is well known, studies with appropriate methodology in practical settings are not only crucial, but are also helpful in promoting, improving the quality of, and curtailing the costs of health care. However, by the same token, the inappropriate provision of any type of intervention, specifically one with substantial expenses, will not only be devoid of any benefit, but will harm the patient and reduce access by depleting resources. Likewise, inappropriately performed evaluations that lead to inaccurate and inappropriate conclusions due to a lack of knowledge or bias may reduce health care expenditure, but will also increase patient suffering, reduce function, increase drug use, and finally impede access to medical care.
Conclusion
This randomized, double-blind, active-controlled trial of 120 patients with chronic function-limiting axial or discogenic neck pain treated with fluoroscopically guided cervical epidural injections and local anesthetics with or without steroids showed effectiveness in 75% of patients, with improvement in pain and functional status, requiring an average of 3–4 procedures over a period of one year, with relief for 37–39 weeks over a period of one year in the successful group.
Disclosure
None of the authors report any competing interests in this work.
References
- PizzoPAClarkNMAlleviating suffering 101 – pain relief in the United StatesN Engl J Med2012367319719822256802
- ManchikantiLSinghVDattaSCohenSPHirschJAComprehensive review of epidemiology, scope, and impact of spinal painPain Physician2009124E35E7019668291
- BenyaminRMSinghVParrATConnADiwanSAbdiSSystematic review of the effectiveness of cervical epidurals in the management of chronic neck painPain Physician200912113715719165300
- Hogg-JohnsonSvan der VeldeGCarrollLJThe burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 task force on neck pain and its associated disordersSpine (Phila Pa 1976)200833Suppl 4S39S5118204398
- CôtéPCassidyJDCarrollLThe Saskatchewan health and back pain survey. The prevalence of neck pain and related disability in Saskatchewan adultsSpine (Phila Pa 1976)19982315168916989704377
- CôtéPCassidyJDCarrollLJKristmanVThe annual incidence and course of neck pain in the general population: a population-based cohort studyPain2004112326727315561381
- ManchikantiLPampatiVBoswellMVSmithHSHirschJAAnalysis of the growth of epidural injections and costs in the Medicare population: a comparative evaluation of 1997, 2002, and 2006 dataPain Physician201013319921220495584
- ManchikantiLPampatiVSinghVBoswellMVSmithHSHirschJAExplosive growth of facet joint interventions in the medicare population in the United States: a comparative evaluation of 1997, 2002, and 2006 dataBMC Health Serv Res2010108420353602
- ManchikantiLAilinaniHKoyyalaguntaDA systematic review of randomized trials of long-term opioid management for chronic non-cancer painPain Physician20111429112121412367
- ManchikantiLVallejoRManchikantiKNBenyaminRMDattaSChristoPJEffectiveness of long-term opioid therapy for chronic non-cancer painPain Physician2011142E133E15621412378
- WangMCChanLMaimanDJKreuterWDeyoRAComplications and mortality associated with cervical spine surgery for degenerative disease in the United StatesSpine (Phila Pa 1976)200732334234717268266
- ManchikantiLParrATSinghVFellowsBAmbulatory surgery centers and interventional techniques: a look at long-term survivalPain Physician2011142E177E21521412380
- ManchikantiLFellowsBAilinaniHPampatiVTherapeutic use, abuse, and nonmedical use of opioids: a ten-year perspectivePain Physician201013540143520859312
- HelgesonMDAlbertTJSurgery for failed cervical spine reconstructionSpine (Phila Pa 1976)2012375E323E32722076644
- PatilPGTurnerDAPietrobonRNational trends in surgical procedures for degenerative cervical spine disease: 1990–2000Neurosurgery200557475375816239888
- ManchikantiLBoswellMVSinghVComprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal painPain Physician200912469980219644537
- ManchikantiLDunbarEEWargoBWShahRVDerbyRCohenSPSystematic review of cervical discography as a diagnostic test for chronic spinal painPain Physician200912230532119305482
- YinWBogdukNThe nature of neck pain in a private pain clinic in the United StatesPain Medicine20089219620318298702
- LotzJCUlrichJAInnervation, inflammation, and hypermobility may characterize pathologic disc degeneration: review of animal model dataJ Bone Join Surg Am200688Suppl 27682
- ClowardRBCervical discographyActa Radiol Diagn (Stockh)1963167568814044700
- ClowardRBCervical diskography. A contribution to the etiology and mechanism of neck, shoulder and arm painAnn Surg19591501052106413810738
- ManchikantiLCashKAPampatiVWargoBWMallaYThe effectiveness of fluoroscopic cervical interlaminar epidural injections in managing chronic cervical disc herniation and radiculitis: preliminary results of a randomized, double-blind, controlled trialPain Physician201013322323620495586
- ManchikantiLCashKAPampatiVWargoBWMallaYCervical epidural injections in chronic discogenic neck pain without disc herniation or radiculitis: preliminary results of a randomized, double-blind, controlled trialPain Physician2010134E265E27820648213
- ManchikantiLMallaYCashKAMcManusCDPampatiVFluoroscopic epidural injections in cervical spinal stenosis: preliminary results of a randomized, double-blind, active control trialPain Physician2012151E59E7022270749
- ManchikantiLMallaYCashKAMcManusCDPampatiVFluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical post-surgery syndrome: preliminary results of a randomized, double-blind active control trialPain Physician2012151132622270734
- StavAOvadiaLSternbergAKaadanMWekslerNCervical epidural steroid injection for cervicobrachialgiaActa Anaesthesiol Scand19933765625668213020
- CastagneraLMaurettePPointillartVVitalJMErnyPSenegasJLong term results of cervical epidural steroid injection with and without morphine in chronic cervical radicular painPain19945822392437816491
- PasqualucciAVarrassiGBraschiAEpidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: single injection versus continuous infusionClin J Pain200723755155717710003
- ManchikantiLSinghVCashKAPampatiVDamronKSBoswellMVA randomized, controlled, double-blind trial of fluoroscopic caudal epidural injections in the treatment of lumbar disc herniation and radiculitisSpine (Phila Pa 1976)201136231897190521897343
- ManchikantiLSinghVFalcoFJECashKAPampatiVEvaluation of the effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation or radiculitis: a randomized, double-blind, controlled trialPain Physician201013434335520648203
- ManchikantiLCashKAMcManusCDPampatiVBenyaminRMA preliminary report of a randomized double-blind, active controlled trial of fluoroscopic thoracic interlaminar epidural injections in managing chronic thoracic painPain Physician2010136E357E36921102973
- ManchikantiLCashKAMcManusCDPampatiVSmithHSOne year results of a randomized, double-blind, active controlled trial of fluoroscopic caudal epidural injections with or without steroids in managing chronic discogenic low back pain without disc herniation or radiculitisPain Physician2011141253621267039
- ManchikantiLCashKAMcManusCDPampatiVBenyaminRMPreliminary results of a randomized, double-blind, controlled trial of fluoroscopic lumbar interlaminar epidural injections in managing chronic lumbar discogenic pain without disc herniation or radiculitisPain Physician2010134E279E29220648214
- ManchikantiLCashKAMcManusCDPampatiVAbdiSPreliminary results of randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: part 4. Spinal stenosisPain Physician200811683384819057629
- ManchikantiLCashKAMcManusCDDamronKSPampatiVFalcoFJELumbar interlaminar epidural injections in central spinal stenosis: preliminary results of a randomized, double-blind, active control trialPain Physician2012151516322270738
- ManchikantiLSinghVCashKAPampatiVDattaSPreliminary results of randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: part 3. Post surgery syndromePain Physician200811681783119057628
- ManchikantiLSinghVFalcoFJECashKAFellowsBComparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: a randomized, double-blind controlled trialPain Physician201013543745020859313
- ManchikantiLSinghVFalcoFJECashKAPampatiVEvaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-upIn J Med Sci201073124135
- ManchikantiLSinghVFalcoFJECashKAPampatiVFellowsBComparative effectiveness of a one-year follow-up of thoracic medial branch blocks in management of chronic thoracic pain: a randomized, double-blind active controlled trialPain Physician201013653554821102966
- TachiharaHSekiguchiMKikuchiSKonnoSDo corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation?Spine (Phila Pa 1976)200833774374718379400
- PasqualucciAExperimental and clinical studies about the preemptive analgesia with local anesthetics. Possible reasons of the failureMinerva Anestesiol199864104454579857627
- ArnerSLindblomUMeyersonBAMolanderCProlonged relief of neuralgia after regional anesthetic block. A call for further experimental and systematic clinical studiesPain19904332872971705693
- SatoCSakaiAIkedaYSuzukiHSakamotoAThe prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic painAnesth Analg2008106131332018165597
- ByrodGOtaniKBrisbyHRydevikBOlmarkerKMethylprednisolone reduces the early vascular permeability increase in spinal nerve roots induced by epidural nucleus pulposus applicationJ Orthop Res200018698398711192260
- LeeHMWeinsteinJNMellerSTHayashiNSprattKFGebhartGFThe role of steroids and their effects on phospholipase A2. An animal model of radiculopathySpine (Phila Pa 1976)19982311119111969636970
- MaoJChenLLSystemic lidocaine for neuropathic pain reliefPain200087171710863041
- BisbyMAInhibition of axonal transport in nerves chronically treated with local anestheticsExp Neurol197547348148948475
- AltmanDGSchulzKFMoherDThe revised CONSORT statement for reporting randomized trials: explanation and elaborationAnn Intern Med2001134866369411304107
- ManchukondaRManchikantiKNCashKAPampatiVManchikantiLFacet joint pain in chronic spinal pain: an evaluation of prevalence and false-positive rate of diagnostic blocksJ Spinal Disord Tech200720753954517912133
- FalcoFJEErhartSWargoBWSystematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventionsPain Physician200912232334419305483
- ClelandJAChildsJDWhitmanJMPsychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck painArch Phys Med Rehabil2008891697418164333
- PietrobonRCoeytauxRRCareyTSRichardsonWJDeVellisRFStandard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic reviewSpine (Phila Pa 1976)200227551552211880837
- VernonHMiorSThe Neck Disability Index: a study of reliability and validityJ Manipulative Physiol Ther19911474094151834753
- ManchikantiLHirschJASmithHSEvidence-based medicine, systematic reviews, and guidelines in interventional pain management: part 2: randomized controlled trialsPain Physician200811671777319057624
- ManchikantiLBenyaminRMHelmSHirschJAEvidence-based medicine, systematic reviews, and guidelines in interventional pain management: part 3: systematic reviews and meta-analysis of randomized trialsPain Physician2009121357219165297
- PereiraJLawlorPViganoADorganMBrueraEEquianalgesic dose ratios for opioids. A critical review and proposals for long-term dosingJ Pain Symptom Manage200122267268711495714
- BrownerWSNewmanTBCummingsSRHulleySBEstimating sample size and powerHulleySBCummingsSRBrownerWSGradyDHearstNNewmanTBDesigning Clinical Research: An Epidemiologic Approach2nd edPhiladelphia, PALippincott, Williams and Wilkins2001
- PelosoPMJGrossAHainesTMedicinal and injection therapies for mechanical neck disordersCochrane Database Sys Rev20073CD000319
- ManchikantiLDattaSGuptaSA critical review of the American Pain Society clinical practice guidelines for interventional techniques. Part 2. Therapeutic interventionsPain Physician2010134E215E26420648212
- ManchikantiLFalcoFJEBoswellMVHirschJAFacts, fallacies, and politics of comparative effectiveness research: part 2. Implications for interventional pain managementPain Physician2010131E55E7920119475
- ManchikantiLFalcoFJBenyaminRMHelmS2ndParrATHirschJAThe impact of comparative effectiveness research on interventional pain management: evolution from Medicare Modernization Act to Patient Protection and Affordable Care Act and the Patient-Centered Outcomes Research InstitutePain Physician2011143E249E28221587337
- ManchikantiLFalcoFJEBoswellMVHirschJAFacts, fallacies, and politics of comparative effectiveness research: part I. Basic considerationsPain Physician2010131E23E5420119474
- ManchikantiLDattaSDerbyRWolferLRBenyaminRMHirschJAA critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 1. Diagnostic interventionsPain Physician2010133E141E17420495596
- HotopfMThe pragmatic randomized controlled trialAdv Psychiatr Treat20028326333
- TunisSRStryerDBClancyCMPractical clinical trials. Increasing the value of clinical research for decision making in clinical and health policyJAMA2003290121624163214506122
- RolandMTorgersonDJWhat are pragmatic trials?BMJ199831671272859472515
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human UseICH Harmonised Tripartite GuidelineChoice of Control Group and Related Issues in Clinical Trials E10July 20, 2000 http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E10/Step4/E10_Guideline.pdf
- IversenTSolbergTRomnerBEffect of caudal epidural steroid or saline injection in chronic lumbar radiculopathy: multicentre, blinded, randomised controlled trialBMJ2011343d527821914755
- CaretteSLeclaireRMarcouxSEpidural corticosteroid injections for sciatica due to herniated nucleus pulposusN Engl J Med199733623163416409171065
- KarppinenJMalmivaaraAKurunlahtiMPeriradicular infiltration for sciatica: a randomized controlled trialSpine (Phila Pa 1976)20012691059106711337625
- ManchikantiLGiordanoJFellowsBHirschJAPlacebo and nocebo in interventional pain management: a friend or a foe – or simply foes?Pain Physician2011142E15717521412379
- ManchikantiLSinghVFalcoFJECashKAFellowsBCervical medial branch blocks for chronic cervical facet joint pain: a randomized double-blind, controlled trial with one-year follow-upSpine (Phila Pa 1976)200833171813182018670333
- GhahremanAFerchRBogdukNThe efficacy of transforaminal injection of steroids for the treatment of lumbar radicular painPain Med20101181149116820704666
- ChouRAtlasSJLoeserJDRosenquistRWStanosSPGuideline warfare over interventional therapies for low back pain: can we raise the level of discourse?J Pain201112883383921742563
- IndahlAKaigleAMReikeräsOHolmSHInteraction between the porcine lumbar intervertebral disc, zygapophyseal joints, and paraspinal musclesSpine (Phila Pa 1976)19972224283428409431619
- IndahlAKaigleAReikeräsOHolmSElectromyographic response of the porcine multifidus musculature after nerve stimulationSpine (Phila Pa 1976)19952024265226588747243
- Pham DangCLelongAGuilleyJEffect on neurostimulation of injectates used for perineural space expansion before placement of a stimulating catheter: normal saline versus dextrose 5% in waterReg Anesth Pain Med200934539840319920414
- TsuiBCKropelinBGanapathySFinucaneBDextrose 5% in water: fluid medium maintaining electrical stimulation of peripheral nerve during stimulating catheter placementActa Anaesthesiol Scand200549101562156516223407