Abstract
Purpose
Previous studies have demonstrated that minimally invasive (MI) transforaminal lumbar interbody fusion (TLIF) is comparable to the open approach in terms of efficacy and safety. However, few comparative studies of surgical procedures in patients with obesity show that they may react differently to open-TLIF (O-TLIF) and MI-LTIF approaches.
Patients and Methods
The main indicators were complications, visual analog scale (VAS) score, and Oswestry Disability Index (ODI) score, and secondary indicators were operative time, blood loss, and hospital stay.
Results
No significant differences in the VAS and ODI scores for back pain at the last follow-up and wound infection rates were observed between the two groups. Dural tear incidence and complication rate were significantly lower in the MI-TLIF group than that in the O-TLIF group (P = 0.002 and 0.001, respectively). No significant difference in operative time was found between the two groups. There was less blood loss and shorter hospital stay (P = 0.001 and 0.002, respectively) in the MI-TLIF group than that in the O-TLIF group.
Conclusion
Compared with O-TLIF, MI-TLIF is an effective and safe surgical option for patients with obesity, which resulted in similar improvements in pain and functional disability, as well as a lower complication rate.
Introduction
According to the World Health Organization (WHO) regulations, a body mass index (BMI) >30 is defined as obese.Citation1 According to related reports,Citation2 the obesity rate has been increasing. In 2008, the obesity rate was almost double that of 1980. By 2025, approximately two-thirds of the population will be overweight or obese, which has become the focus of global attention. Obesity is associated with a variety of chronic complications such as hypertension and diabetes,Citation3,Citation4 which not only increases the difficulty of spinal surgery but also increases the risk of surgical complications.Citation5–Citation8 Several studies have shown that patients with obesity have a significantly higher risk of perioperative complications, such as wound infection, deep venous thrombosis, and pulmonary embolism. They also have an increased risk of readmission due to revision surgery and postoperative complications.Citation7,Citation9,Citation10
Several studies have pointed out that obesity is a risk factor for a variety of diseases,Citation11–Citation14 including cervical spondylosis, lumbar disc herniation, lumbar spondylolisthesis, and spinal canal stenosis, which need to be treated surgically, if necessary. Patients with obesity are susceptible to difficulty in intubation and have a higher risk of postoperative infection rate, and thromboembolic events, and thus demand more awareness from anesthesiologists and surgeons.Citation15–Citation20 Spinal surgery requires high precision, but for spinal fusion in patients with obesity, surgeons must perform precise operations in a limited surgical space, with indistinct anatomical landmarks. Therefore, it is important to strictly follow protocols and choose a suitable surgical treatment option for patients with obesity.
Transforaminal lumbar interbody fusion (TLIF) has become a routine surgical treatment for lumbar degenerative diseases, with a widely recognized clinical effect, making it a preference by many surgeons. Traditional TLIF is performed using an open approach (O-TLIF). The invention and improvement of the minimally invasive approach (MI-TLIF) have brought more beneficial choices for patients in the last 20 years. In general, MI-TLIF and O-TLIF yield good results for patients without obesity, but MI-TLIF provides less tissue trauma, less postoperative pain, and shorter hospital stay, as confirmed by several researchers.Citation21–Citation24 However, the advantages of MI-TLIF over O-TLIF in patients with obesity have not been fully and effectively confirmed. It is meaningful to verify which surgical methods will bring higher benefits to patients.
Our meta-analysis aimed to further evaluate the efficacy of MI-TLIF and O-TLIF in the treatment of obese lumbar disease. This may provide useful information for spinal surgeons in making surgical plans for patients with obesity.
Materials and Methods
A meta-analysis of this article was conducted based on the standard principles set by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,Citation25,Citation26 and referred to the checklist and flow diagram.
Literature Search
Systematic literature retrieval was carried out on electronic databases such as PubMed, Embase, Web of Science, and Cochrane Library, and the period was set from the establishment of the database to September 2020. Literature retrieval was based on the Cochrane Handbook and PRISMA guidelines.Citation27
The following terms with appropriate operator combinations “AND,” “OR,” and “NOT” were used in the search strategy: “obesity,” “obese and overweight,” “BMI,” “fusion,” “transforaminal lumbar interbody fusion,” “TLIF,” “minimally invasive transforaminal lumbar interbody fusion,” “MIS-TLIF,” and “MI-TLIF.” The titles and abstracts of all reports were independently reviewed by two researchers (CX and GXL), and full texts of suitable studies were retrieved. Moreover, a manual search was carried out for the reference list of the selected literature, as well as similar literature and previous similar meta-analyses. A list of references of all included target articles was reviewed to identify potentially relevant studies. The language used in the literature was limited to English. The retrieval strategy (eg, PubMed), is provided in supplementary file (Table S1).
Inclusion and Exclusion Criteria
The inclusion criteria for this meta-analysis were as follows: (1) original clinical studies that compared outcomes of MI-TLIF and O-TLIF in patients with obesity and (2) the report data including at least one outcome indicator (perioperative parameters, functional outcomes, and complications).
The following studies were excluded: (1) animal studies, reviews, comments, technique papers, case reports, and cadaver studies; (2) unrelated to TLIF, such as other methods of interbody fusion comparison studies; and (3) studies examining patients who received any surgical intervention in the cervical or thoracic vertebrae.
Data Collection
Patient demographic data, functional outcomes, complications, and other analyzable data were extracted and summarized from the included studies, such as estimated intraoperative blood loss, operative time, length of hospitalization stay, peri- and postoperative complications, and clinical outcomes (visual analog scale [VAS] pain and Oswestry Disability Index [ODI] scores) pre- and postoperatively.
Data Extraction and Quality Assessment
The study design, country, year of publication, duration of the study, clinical outcome, and follow-up time for each surgical group were independently recorded using data extraction forms. The corresponding authors were contacted by e-mail to seek out study details not mentioned in the published versions of their papers. In addition, a quality assessment of the included observational clinical controlled studies was performed using the Newcastle–Ottawa Quality Assessment Scale (NOS). The scale evaluates studies on the three items of selection, comparability, and exposure. For RCTs, the risk of bias was evaluated using the domain-based Cochrane Collaboration tool. Observational studies were of high quality if they obtained scores of 7–9, whereas RCTs were considered of high quality if they satisfied three or more criteria. In addition, the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) standard recommended by the Cochrane Library was used to evaluate the quality of evidence of the main outcome indicators.
Statistical Analysis
All meta-analyses were conducted using the Review Manager software (RevMan version 5.3, Cochrane Collaboration). The continuous variables were statistically analyzed using weighted mean difference (WMD) or standard mean difference, and dichotomous variables were calculated and analyzed by odds ratio (OR). Noteworthily, for studies that do not provide the mean and standard deviation directly, they were estimated according to the method described by Hozo et al.Citation28
The chi-square test was used to test the heterogeneity of the study, and the I2 statistics was calculated as a reference index. When P < 0.05, and I2 > 50%, the heterogeneity was considered statistically significant. A random-effects or fixed-effects model was used for the meta-analysis. When I2 ≥ 50% and P < 0.05, the combined study showed high heterogeneity. A random-effects model was used for analysis. When I2 < 50% and P > 0.05, the fixed-effects model was used.Citation29 Moreover, if a study had significant heterogeneity, a sensitivity analysis was performed, and one study at a time was excluded to check the heterogeneity of the study. Subgroup analyses, performed by reporting the clinical outcomes of the differential diagnosis of segments (single or multiple), were applied to find the source of heterogeneity among the studies. The bias risk in this study was evaluated according to the Cochrane Back Review Group,Citation30 and because of the insufficient number of studies (n < 10), the assessment of publication bias was not applicable. P values < 0.05 were considered statistically significant.
Results
Study Selection
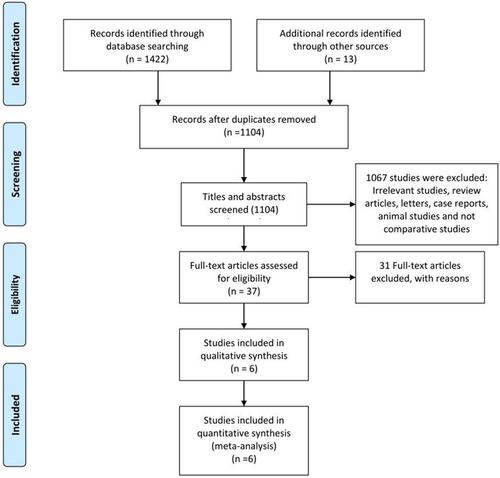
A total of 1422 studies were selected in the preliminary research, including 465 from PubMed, 565 from Web of Science, 331 from Embase, 61 from the Cochrane Library, and 13 from other sources. After reviewing the duplications, 331 duplicate studies were excluded. After cross-browsing the title and abstracts, 37 potential articles were included, and after reading the full text, only six articles were selected. The manually retrieved articles did not include any other studies. This meta-analysis consisted of the remaining six studiesCitation24,Citation31–Citation35 ().
Studies based on the inclusion and exclusion criteria were critically evaluated. Among the six included studies, one studyCitation24 was an RCT with CONSORT 22 with a maximum score of 25. Studies with surgical intervention as a random condition may be ethically challenging, making it difficult for subjects to be randomized. Based on the NOS (supplementary file; Table S2), the non-randomized controlled trials involved in this study were considered to be of high quality (5–9 points).Citation36 Two studiesCitation32,Citation35 received 8/9, two studiesCitation31,Citation34 received 7/9, and the last studyCitation33 received 6/9 (supplementary file; #2). In addition, the GRADE standard quality classification principle showed that low back pain VAS score, ODI index score, and complication rate were medium-quality evidence.
Demographic Results
A total of 654 patients were identified, of whom 273 (41.7%) underwent O-TLIF and 381 (58.3%) underwent MI-TLIF. Of these, 267 (40.8%) were men and 387 (59.2%) were women. There was no difference in demographic characteristics between the two groups. The collected age was 57.29 ± 12.47 years for the O-TLIF group and 54.01 ± 10.78 years for the MI-TLIF group. The pooled BMI was 32.42 ± 5.59 kg/m2 for the O-TLIF group and 33.33 ± 5.41 kg/m2 for the MI-TLIF group. The percentage of males in the O-TLIF group was 55.8%, and the percentage of males in the MI-TLIF group was 44.2%. The most common surgical indications were lumbar spondylolisthesis and spinal canal stenosis, which are difficult to treat surgically. Up to 1036 spinal levels were fused. Except for the article by Abbasi et al, the most commonly operated level was at L4/5 (39.3%) and L5/S1 (31.8%), followed by L3/4 (13.8%), L2/3 (9.0%), and L1/2 (6.1%) (–).
Table 1 Characteristics of Studies Included in the Meta-Analyses
Table 2 Diagnosis of Included Studies
Table 3 Fused Level of Included Studies
Comparison of Perioperative Outcomes
Operative Time
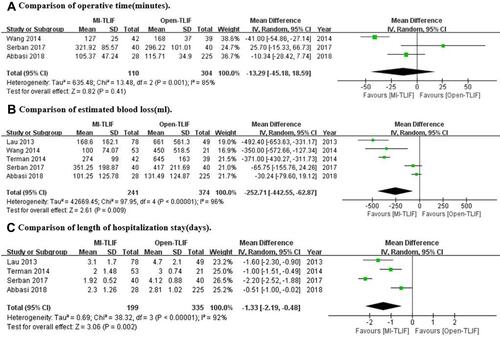
The pooled operative time of the O-TLIF group came from three eligible inclusion studies, involving 304 patients, which was 146.17 ± 99.65 min, whereas the pooled operative time in the MI-TLIF group, involving 110 patients, was 192.37 ± 114.70 min. Significant heterogeneity could be observed among the studies (I2 = 85% P = 0.001), the random-effects model was used for analysis, and the results indicated no significant difference in operative time between the two groups (WMD = −13.29 min; 95% CI: −45.18 to 18.59; P = 0.41) (A).
Estimate of Intraoperative Blood Loss
Five studies involved estimated intraoperative blood loss, including 374 patients in the O-TLIF group at 302.88 ± 348.06 mL and 241 patients in the MI-TLIF group at 194.36 ± 167.05 mL. Significant heterogeneity was detected among the studies (I2 = 96%, P < 0.00001), the random-effects model was used for analysis, and the blood loss was significantly lower in the MI-TLIF group than that in the O-TLIF group (WMD = −252.71 mL; 95% CI: −422.55 to −62.87; P = 0.009) (B).
Length of Hospital Stay
Four studies reported that the length of hospital stay, including 335 patients in the O-TLIF group, was 3.25 ± 1.41 days, whereas the combined hospitalization of 199 patients with obesity included in the MI-TLIF group was 2.45 ± 1.50 days. At the same time, significant heterogeneity was observed (I2 = 82%, P = 0.02), and the random-effects model was used for analysis. The length of hospitalization was significantly shorter in the MI-TLIF group (WMD = −1.33 days; 95% CI: −2.19 to −0.48; P = 0.002) (C).
Visual Analog Scale (VAS)
Three studies included the visual analog scale (VAS) score, and two studies provided sufficient data on the VAS score of early low back pain (early BP-VAS), with the O-TLIF group including 60 patients with obesity with a score of 3.98 ± 2.99 and the MI-TLIF group including 95 patients with a score of 3.25 ± 2.93. A significant heterogeneity was noted (I2 = 82%, P = 0.02). Using the random-effects model for combined analysis, no significant difference was observed in the VAS score for early postoperative low back pain between the two groups (WMD = −1.17; 95% CI: −3.78 to 1.43; P = 0.38) (A).
Figure 3 Forest plots comparing final pain outcomes between MI-TLIF and Open-TLIF with (A) comparison of early back pain and leg pain Visual Analog Scale (VAS), (B) comparison of late back pain and leg pain of VAS, (C) comparison of latest Oswestry Disability Index (ODI).
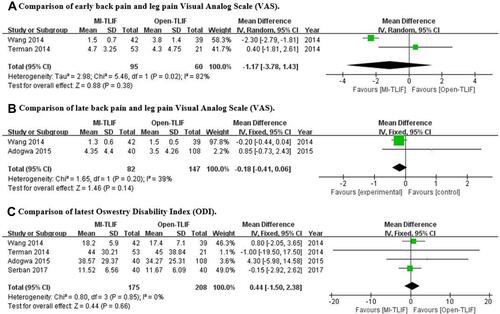
Two studies mentioned sufficient data from the back pain VAS score on the last follow-up (last BP-VAS), with 147 patients in the O-TLIF group (2.97 ± 3.76 scores) and 82 patients in the MI-TLIF group (2.78 ± 3.44 scores). For the heterogeneity analysis (I2 = 39%, P = 0.20), fixed-effects model was selected, and a significant difference in the late BP-VAS scores was found between the two groups (WMD = −0.81; 95% CI: −0.41 to 0.06; P = 0.14) (B).
Oswestry Disability Index (ODI)
Four articles reported the ODI score of the last follow-up, including 384 patients: 208 patients in the O-TLIF group (27.85 ± 24.81 scores) and 175 patients in the MI-TLIF group (29.53 ± 26.00 scores). A nonsignificant heterogeneity was observed between the two groups (I2 = 0%, P = 0.85). Therefore, the fixed-effects model was selected for statistical analysis, showing no significant difference in the ODI score between the two groups at the last follow-up (WMD = 0.44; 95% CI: −1.5 to –2.38; P = 0.66) (C).
Complications
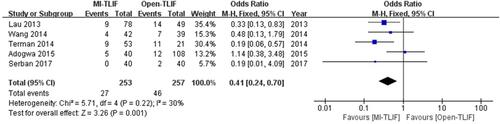
Five studies reported information regarding perioperative complications, including 510 patients. A total of 257 patients in the O-TLIF group had a complication rate of 19.1%, and 253 patients in the MI-TLIF group had complication rate of 10.7%. A nonsignificant heterogeneity was noted (I2 = 0%, P = 0.81). The incidence of complications in the MI-TLIF group was significantly lower than that in the O-TLIF group (OR = 0.41; 95% CI: 0.24 to 0.70; P = 0.001) ().
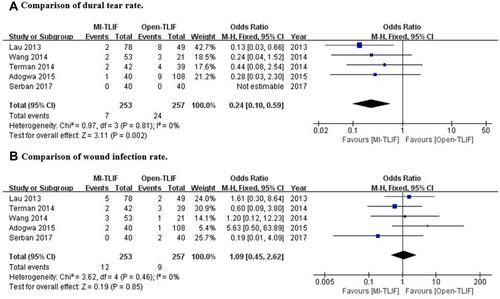
Dural Tear
Dural tears and wound infections are the most common complications. The incidence of dural tear in the O-TLIF group was 9.3% and in the MI-TLIF group was 2.8%. A nonsignificant heterogeneity was found (I2 = 0%, P = 0.81), the fixed-effects model was used for combined analysis, and the dural tear incidence was significantly lower in the MI-TLIF group (OR = 0.24; 95% CI: 0.10 to 0.59; P = 0.002) (A).
Wound Infection
According to the combined statistics, the wound infection rate in the O-TLIF and MI-TLIF groups was 3.5% and 4.7%, respectively, the heterogeneity of the two groups was nonsignificant (I2 = 0%, P = 0.46), and the fixed-effects model was used for combined analysis. No significant difference was observed in the wound infection rate between the two groups (OR = 1.09; 95% CI: 0.45 to 2.62; P = 0.85) (B).
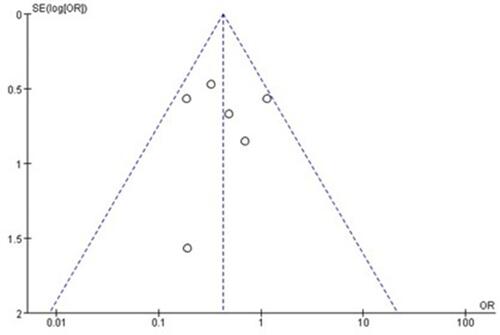
Sensitivity Analysis and Publication Bias
In the sensitivity analysis, one experiment was excluded one by one, and the forest plot was not reversed. Switching between the fixed-effects and random-effects models in the merger analysis and sensitivity analysis reduced the bias. In addition, a funnel plot was used to evaluate publication bias. The incidence of complications was used as an indicator of publication bias. Distinct asymmetry is not observed in , indicating no risk of bias. However, considering the insufficient number of studies (<10), the results should be treated with caution.
Discussion
Foley et alCitation37 first described MI-TLIF in 2003, which uses muscle space to split the approach and insert a tubular retractor to reduce soft tissue injury, which is an alternative to the traditional open approach. After continuous verification and development of the concept of MI surgeries, MI-TLIF technology has made great progress.Citation38 In recent years, some surgeons have summarized the comparison between MI-TLIF and O-TLIF,Citation39 as well as the comparison of the two procedures in patients with obesity. Therefore, a meta-analysis was carried out to provide more objective and relatively fair results to guide clinical practice.
In this meta-analysis, an extensive literature search was conducted, finally including only six articles that met the inclusion criteria. Nevertheless, the sample size collected was relatively large, data were extracted for statistical analysis, and meaningful results were obtained. The current meta-analysis a nonsignificant difference in operative time between the O-TLIF and MI-TLIF groups and a nonsignificant difference between the VAS and ODI scores after the operation; however, there was less intraoperative bleeding and shorter hospital stay in the MI-TLIF group than that in the O-TLIF. Moreover, the incidence of intraoperative dural tear and total complications in the MI-TLIF group was lower than that in the O-TLIF group, and no significant difference in the incidence of postoperative infection was noted between the two groups. However, there is not enough follow-up information to compare the incidence of long-term complications of O-TLIF and MI-TLIF in patients with obesity. Larger samples and longer follow-up periods are required for further comparison.
Our meta-analysis showed that the estimated intraoperative blood loss and hospitalization stay were shorter in the MI-TLIF group than that in the O-TLIF group, which were roughly the same as those of other studies.Citation40,Citation41 Regarding the operative time, different results were obtained from most studies, and the difference in operative time between the two groups may not be significant, which is probably due to the fewer studies included and the different learning curves of the doctors included in the study. In this article, Serban et alCitation24 pointed out that the operative time of MI-TLIF is not superior to that of O-TLIF, or even longer. No significant difference in postoperative VAS and ODI scores were found between the two groups. These two indicators relatively intuitively show the benefits of patients; thus, it can be considered that the two surgical methods improved symptoms significantly. At present, the surgical instruments and consumables of MI-TLIF are more expensive; nevertheless, it has notable economic benefits to patients by reducing the length of hospital stay and reducing the incidence of complications. We can draw from the experience that technological innovation and development need social tolerance, and doctors need to comprehensively consider the pros and cons, combined with the actual situation to solve patients’ problems.
Some studiesCitation42–Citation44 have confirmed that patients with obesity have a higher risk of complications from O-TLIF than that in patients without obesity. The occurrence of infection may be owing to a thicker subcutaneous fat layer and less blood circulation in patients with obesity, resulting in slower healing. Concurrently, larger incisions in open surgery are more likely to form a dead space, thus increasing the risk of infection and poor vascularization of adipose tissue. It has been confirmed that fat layer thickness is related to the healing time.Citation45 Several studiesCitation46–Citation50 subdivide patients with obesity into classes I, II, III, and IV. The study and analysis of MI-TLIF surgery showed that more severe obesity may be associated with a higher occurrence of complications, showing that the risk of complications in this population is much higher than that in normal-weight patients. However, the results of our analysis showed that no significant difference in the risk of wound infection was observed in patients with obesity undergoing O-TLIF or MITLIF. Infection, a surgeon’s ordeal, remains an important problem to be solved.
Owing to the difference between surgical procedures and instruments, the surgical incision in O-TLIF is larger, the scope of exposure is wider, and the risk of dural tear is higher.Citation51 Studies have indicated that patients with obesity still have a higher risk of dural tear than on those with normal weight, regardless of MI or open surgery.Citation52–Citation54 According to the analysis of the incidence of dural tear after an operation, a significant difference was found between the two surgical methods. The occurrence of a dural tear in the MI-TLIF group was significantly lower than that in the O-TLIF group. However, regarding complications, except for dural tear and wound infection, the MI-TLIF group had a lower incidence of complications, and the difference was statistically significant. According to our meta-analysis, the total number of complications in the MI-TLIF group was significantly lower than that in the O-TLIF group. However, according to the situation of each study, the follow-up period summarized in our current analysis is not long enough, some long-term complications are inevitably ignored, and studies with longer (5- or 10-year) follow-up are expected to be reported.
Moreover, Xie et alCitation55 published a similar meta-analysis, which included PLIF (Posterior Lumbar Interbody Fusion). The reasons mentioned above limit the quality and credibility of the study. Both Othman et alCitation40 and Tan et alCitation41 included four studies to analyze perioperative outcomes, whereas we conducted a combined analysis of six studies. It is noteworthy that our inclusion of Abbasi et al and Lau et al’s study only conducted a statistical analysis of the perioperative efficacy and the part that can be combined for analysis was extracted and relatively high-quality credibility was obtained. Using the “one-by-one elimination method” for sensitivity analysis, the results were not reversed, which proved that the results were reliable, but the number of cases in Abbasi et al’s study was quite different from that in the TLIF control group (28/225). It is difficult to unify the diagnoses and surgical segments of the patients, and its heterogeneity and statistical rigor are worthy of discussion. Our research was conducted in strict accordance with the Cochrane Handbook, exploring the heterogeneity among the studies as much as possible, fully considering the possible confounding factors, and presenting the research results as objectively as possible.
Only Serban et alCitation24 reported the fusion rate between the two groups, which were very high and similar. The fusion rate is often a key index to measure spinal fusion surgery; it is also an important factor in determining recurrence and repair rates. Only Lau et alCitation31 mentioned the cost of patient treatment, and patients hope to obtain a good treatment effect, while considering the cost of treatment, which is an important determinant of patient satisfaction. Recent technologies often need expensive support to develop, and after verifying the efficacy of surgery, they will be further promoted and developed to reduce the cost of surgery and bring well-being to critically ill patients.Citation56,Citation57 Comparative studies on the fusion rates of MI-TLIF and O-TLIF in patients with obesity are required to further evaluate their efficacy.
Study Limitations
Too few RCTs comparing MI-TLIF and O-TLIF in people with obesity are available. Second, significant heterogeneity was observed in the analysis of some indicators. Wang et al and Serban et al included patients with a BMI <30 kg/m2. According to the WHO definition of obesity, they are not obese patients, but overweight patients. The comorbidities of patients with obesity often include hypertension, coronary heart disease, diabetes, and kidney disease. Third-degree patients with obesity have a higher risk of venous thrombosis. Of the six studies included in the meta-analysis, the follow-up period in two studies was not long enough (6 months). In addition, unpublished studies were not included because of difficulty in obtaining their data, but no evidence of publication bias was found. Another limitation is the lack of reported data that have been followed up for more than 5 years, which may provide more convincing evidence.
Conclusion
When comparing the results of MI-TLIF and O-TLIF in patients with obesity, the clinical effects were similar in both techniques with regard to the postoperative VAS score and the final ODI score. It was found that MI-TLIF was superior to O-TLIF in terms of complications, incidence of dural tears, estimated blood loss, and shorter hospital stays. However, randomized controlled trials with large samples and long-term follow-up are still lacking, which is necessary to reflect the real value of such a technique.
Abbreviations
BMI, body mass index; BP, back pain; GRADE, Grades of Recommendation, Assessment, Development and Evaluation; NOS, Newcastle-Ottawa Quality Assessment Scale (NOS); MI, minimally invasive; ODI, Oswestry disability index; O-TLIF, open TLIF; OR, odds ratio; PRISMA, preferred reporting item for systematic reviews and meta-analyses; SMD, standard mean difference; TLIF, transforaminal lumbar interbody fusion; VAS, visual analog scale; WHO, World Health Organization; WMD, weighted mean difference.
Acknowledgments
Guang-Xun Lin and Gang Rui are co-corresponding authors.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Surveillance report 2018 – obesity: identification, assessment and management (2014) NICE guideline CG189 and BMI: preventing ill health and premature death in black, Asian and other minority ethnic groups (2013) NICE guideline PH46. London: National Institute for Health and Care Excellence (UK) Copyright © NICE 2018; 2018.
- PwC. Action required: the urgency of addressing social determinants of health. A PwC Health Research Institute report 2019.
- Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53:1925–1932. doi:10.1016/j.jacc.2008.12.068
- Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121:21–33. doi:10.3810/pgm.2009.11.2074
- De la Garza-ramos R, Bydon M, Abt NB, et al. The impact of obesity on short- and long-term outcomes after lumbar fusion. Spine. 2015;40:56–61. doi:10.1097/BRS.0000000000000655
- Flippin M, Harris J, Paxton EW, et al. Effect of body mass index on patient outcomes of surgical intervention for the lumbar spine. J Spine Surg. 2017;3:349–357. doi:10.21037/jss.2017.06.15
- Villavicencio A, Nelson EL, Rajpal S, Vivek N, Burneikiene S. The impact of BMI on operating room time, blood loss, and hospital stay in patients undergoing spinal fusion. Clin Neurol Neurosurg. 2019;179:19–22. doi:10.1016/j.clineuro.2019.02.012
- Narain AS, Parrish JM, Jenkins NW, et al. Risk factors for medical and surgical complications after single-level minimally invasive transforaminal lumbar interbody fusion. Int J Spine Surg. 2020;14:125–132. doi:10.14444/7018
- Urquhart DM, Kurniadi I, Triangto K, et al. Obesity is associated with reduced disc height in the lumbar spine but not at the lumbosacral junction. Spine. 2014;39:E962–6. doi:10.1097/BRS.0000000000000411
- Divi SN, Goyal DKC, Galetta MS, et al. How does body mass index influence outcomes in patients after lumbar fusion? Spine. 2020;45:555–561. doi:10.1097/BRS.0000000000003313
- Bagley C, MacAllister M, Dosselman L, Moreno J, Aoun SG, El Ahmadieh TY. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Research. 2019;8:137. doi:10.12688/f1000research.16082.1
- Delgado-López PD, Castilla-Díez JM. Impact of obesity in the pathophysiology of degenerative disk disease and in the morbidity and outcome of lumbar spine surgery. Neurocirugia. 2018;29:93–102. doi:10.1016/j.neucir.2017.06.002
- Lee SY, Kim W, Lee SU, Choi KH. Relationship between obesity and lumbar spine degeneration: a cross-sectional study from the fifth Korean national health and nutrition examination survey, 2010–2012. Metab Syndr Relat Disord. 2019;17:60–66. doi:10.1089/met.2018.0051
- Jain D, Berven S. Effect of obesity on the development, management, and outcomes of spinal disorders. J Am Acad Orthop Surg. 2019;27:e499–e506. doi:10.5435/JAAOS-D-17-00837
- Valette S, Cohendy R. [Anesthesia and obesity]. Rev Pneumol Clin. 2002;58:117–20. French
- Huschak G, Busch T, Kaisers UX. Obesity in anesthesia and intensive care. Best Pract Res Clin Endocrinol Metab. 2013;27:247–260. doi:10.1016/j.beem.2013.02.001
- Pouwels S, Buise MP, Twardowski P, Stepaniak PS, Proczko M. Obesity Surgery and Anesthesiology Risks: a Review of Key Concepts and Related Physiology. Obes Surg. 2019;29:2670–2677. doi:10.1007/s11695-019-03952-y
- Itani KMF, Dellinger EP, Mazuski J, et al. Surgical Site Infection Research Opportunities. Surg Infect (Larchmt). 2017;18:401–408. doi:10.1089/sur.2017.060
- Cheadle WG. Risk factors for surgical site infection. Surg Infect (Larchmt). 2006;7(Suppl 1):S7–11. doi:10.1089/sur.2006.7.s1-7
- Yuan K, Chen HL. Obesity and surgical site infections risk in orthopedics: a meta-analysis. Int J Surg. 2013;11:383–388. doi:10.1016/j.ijsu.2013.02.018
- Bin Abd Razak HR, Dhoke P, Tay K-S, Yeo W, Yue W-M. Single-Level Minimally Invasive Transforaminal Lumbar Interbody Fusion Provides Sustained Improvements in Clinical and Radiological Outcomes up to 5 Years Postoperatively in Patients with Neurogenic Symptoms Secondary to Spondylolisthesis. Asian Spine J. 2017;11:204–212. doi:10.4184/asj.2017.11.2.204
- Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. 2019;14:229. doi:10.1186/s13018-019-1266-y
- Seng C, Siddiqui MA, Wong KPL, et al. Five-Year Outcomes of Minimally Invasive Versus Open Transforaminal Lumbar Interbody Fusion A Matched-Pair Comparison Study. Spine. 2013;38:2049–2055. doi:10.1097/BRS.0b013e3182a8212d
- Serban D, Calina N, Tender G. Standard versus Minimally Invasive Transforaminal Lumbar Interbody Fusion: a Prospective Randomized Study. Biomed Res Int. 2017;2017:7236970. doi:10.1155/2017/7236970
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(264):w64. doi:10.7326/0003-4819-151-4-200908180-00135
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–94. doi:10.7326/0003-4819-151-4-200908180-00136
- Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019. doi:10.1002/14651858.ED000142
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi:10.1186/1471-2288-5-13
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi:10.1002/sim.1186
- Furlan AD, Malmivaara A, Chou R, et al. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine. 2015;40:1660–1673. doi:10.1097/BRS.0000000000001061
- Lau D, Khan A, Terman SW, Yee T, La Marca F, Park P. Comparison of perioperative outcomes following open versus minimally invasive transforaminal lumbar interbody fusion in obese patients. Neurosurg Focus. 2013;35:E10. doi:10.3171/2013.5.FOCUS13154
- Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of the Clinical Outcome in Overweight or Obese Patients After Minimally Invasive Versus Open Transforaminal Lumbar Interbody Fusion. J Spinal Disord Tech. 2014;27:202–206. doi:10.1097/BSD.0b013e31825d68ac
- Abbasi H, Grant A. Effect of Body Mass Index on Perioperative Outcomes in Minimally Invasive Oblique Lateral Lumbar Interbody Fusion versus Open Fusions: a Multivariant Analysis. Cureus. 2018;10:e2288. doi:10.7759/cureus.2288
- Terman SW, Yee TJ, Lau D, Khan AA, La Marca F, Park P. Minimally invasive versus open transforaminal lumbar interbody fusion: comparison of clinical outcomes among obese patients. Clinical article. J Neurosurg Spine. 2014;20:644–652.
- Adogwa O, Carr K, Thompson P, et al. A prospective, multi-institutional comparative effectiveness study of lumbar spine surgery in morbidly obese patients: does minimally invasive transforaminal lumbar interbody fusion result in superior outcomes? World Neurosurg. 2015;83:860–866. doi:10.1016/j.wneu.2014.12.034
- Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63:530–538. doi:10.1001/archpsyc.63.5.530
- Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003;28:S26–35. doi:10.1097/01.BRS.0000076895.52418.5E
- Sayari AJ, Patel DV, Yoo JS, Singh K. Device solutions for a challenging spine surgery: minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). Expert Rev Med Devices. 2019;16:299–305. doi:10.1080/17434440.2019.1601013
- Wong AP, Smith ZA, Stadler JA 3rd, et al. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am. 2014;25:279–304. doi:10.1016/j.nec.2013.12.007
- Othman YA, Alhammoud A, Aldahamsheh O, Vaishnav AS, Gang CH, Qureshi SA. Minimally Invasive Spine Lumbar Surgery in Obese Patients: a Systematic Review and Meta-Analysis. HSS J. 2020;16:168–176. doi:10.1007/s11420-019-09735-6
- Tan JH, Liu G, Ng R, Kumar N, Wong HK, Liu G. Is MIS-TLIF superior to open TLIF in obese patients?: a systematic review and meta-analysis. Eur Spine J. 2018;27:1877–1886. doi:10.1007/s00586-018-5630-0
- Chotai S, Parker SL, Sivaganesan A, et al. Effect of complications within 90 days on patient-reported outcomes 3 months and 12 months following elective surgery for lumbar degenerative disease. Neurosurg Focus. 2015;39:E8. doi:10.3171/2015.8.FOCUS15302
- Senker W, Meznik C, Avian A, Berghold A. Perioperative morbidity and complications in minimal access surgery techniques in obese patients with degenerative lumbar disease. Eur Spine J. 2011;20:1182–1187. doi:10.1007/s00586-011-1689-6
- Lingutla KK, Pollock R, Benomran E, et al. Outcome of lumbar spinal fusion surgery in obese patients: a systematic review and meta-analysis. Bone Joint J. 2015;97-b:1395–1404. doi:10.1302/0301-620X.97B10.35724
- Mehta AI, Babu R, Karikari IO, et al. 2012 Young Investigator Award winner: the distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine. 2012;37:1652–1656. doi:10.1097/BRS.0b013e318241b186
- Shafa E, Schwender JD. Complications with minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) in the morbidly obese population with degenerative spondylolisthesis. Spine J. 2016;16:S274. doi:10.1016/j.spinee.2016.07.379
- Bohl DD, Ahn J, Mayo BC, et al. Does Greater Body Mass Index Increase the Risk for Revision Procedures Following a Single-Level Minimally Invasive Lumbar Discectomy? Spine. 2016;41:816–821. doi:10.1097/BRS.0000000000001340
- Narain AS, Hijji FY, Bohl DD, Yom KH, Kudaravalli KT, Singh K. Is Body Mass Index a Risk Factor for Revision Procedures After Minimally Invasive Transforaminal Lumbar Interbody Fusion? Clin Spine Surg. 2018;31:E85–e91. doi:10.1097/BSD.0000000000000547
- Buerba RA, Fu MC, Gruskay JA, Long WD 3rd, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14:2008–2018. doi:10.1016/j.spinee.2013.11.047
- Yoo JS, Hrynewycz NM, Brundage TS, Singh K. The Use of Patient-Reported Outcome Measurement Information System Physical Function to Predict Outcomes Based on Body Mass Index Following Minimally Invasive Transforaminal Lumbar Interbody Fusion. Spine. 2019;44:E1388–E95. doi:10.1097/BRS.0000000000003137
- JSt C, Jackson TR. Minimally invasive lumbar discectomy in obese patients. Neurosurgery. 2007;61:539–44; discussion 44. doi:10.1227/01.NEU.0000290900.23190.C9
- Qin R, Liu B, Zhou P, et al. Minimally Invasive Versus Traditional Open Transforaminal Lumbar Interbody Fusion for the Treatment of Single-Level Spondylolisthesis Grades 1 and 2: a Systematic Review and Meta-Analysis. World Neurosurg. 2019;122:180–189. doi:10.1016/j.wneu.2018.10.202
- Chen YC, Zhang L, Li EN, et al. An updated meta-analysis of clinical outcomes comparing minimally invasive with open transforaminal lumbar interbody fusion in patients with degenerative lumbar diseases. Medicine. 2019;98:e17420. doi:10.1097/MD.0000000000017420
- Khan NR, Clark AJ, Lee SL, Venable GT, Rossi NB, Foley KT. Surgical Outcomes for Minimally Invasive vs Open Transforaminal Lumbar Interbody Fusion: an Updated Systematic Review and Meta-analysis. Neurosurgery. 2015;77:847–74; discussion 74. doi:10.1227/NEU.0000000000000913
- Xie Q, Zhang J, Lu F, Wu H, Chen Z, Jian F. Minimally invasive versus open Transforaminal lumbar Interbody fusion in obese patients: a meta-analysis. BMC Musculoskelet Disord. 2018;19:15. doi:10.1186/s12891-018-1937-6
- Djurasovic M, Gum JL, Crawford CH, et al. Cost-effectiveness of minimally invasive midline lumbar interbody fusion versus traditional open transforaminal lumbar interbody fusion. J Neurosurg Spine. 2019;32:31–35.
- Passias PG, Brown AE, Alas H, et al. A cost benefit analysis of increasing surgical technology in lumbar spine fusion. Spine J. 2021;21:193–201. doi:10.1016/j.spinee.2020.10.012