Abstract
Aim
This review aims to examine nurses’ perceived barriers to and facilitators of pain assessment and management in adult critical care patients.
Background
Pain is one of the worst memories among critically ill patients. However, pain among those patients is still undertreated due to several barriers that impede effective management. Therefore, addressing the perceived barriers and facilitators to pain assessment management among critical care nurses is crucial.
Methods
A systematic search of pain assessment and management in critical care patient-relevant literature from four databases was done, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results
The barriers and facilitators were categorized into four groups: nurse-related, patient-related, physician-related, and system-related. The most frequently reported barriers in this study included nurses’ lack of knowledge regarding the use of pain assessment tools, patients’ inability to communicate, physicians’ prescription of analgesics being independent of pain scores evaluation, and absence of standardized guidelines and protocols for pain evaluation and control. For the facilitators, the most reported ones include ongoing education and professional training related to pain assessment and management, patients’ ability to self-report pain, effective collaboration between physicians and nurses, and productive discussion of patients’ pain scores during nurse-to-nurse handovers.
Conclusion
Various barriers and facilitators to pain assessment and management were identified and examined in this review. However, future research is still needed to further investigate these barriers and facilitators and examine any other potential associated factors among critical care nurses.
Relevance to Clinical Practice
The findings of our study could help hospital managers in developing continuous education and staff development training programs on assessing and managing pain for critical care patients. Also, our findings could be used to develop an evidence-based standard pain management protocol tailored to effectively assess and promptly treat pain in critical care patients.
Introduction
For intensive care unit (ICU) patients, pain experienced during ICU stay is one of the most upsetting memories.Citation1 According to Puntillo et al, more than half of ICU patients in 28 European countries were found to have experienced pain, whilst in the United States (US), about 60% of ICU patients reported that their pain persisted after discharge from the hospital.Citation1 In addition to various physiological sources of pain, routine nursing care procedures, such as position-changing and endotracheal suctioning, are major sources of intrinsic pain for ICU patients.Citation2 Untreated pain among critical care patients has many adverse effects, leading to serious physiological and psychological complications and increased length of critical care unit stay.Citation2 For example, the influence of unrelieved pain on the physiological condition of patients includes hemodynamic instability, such as blood pressure elevation, tachycardia, tachypnea, and hyperglycemia. Other associated negative physical consequences include the increase in catecholamine release, immunosuppression, urinary retention, and the increase in metabolic rate.Citation2 Furthermore, psychological and emotional distress may develop among patients who suffer from pain as a result of their inability to cope effectively with pain. In turn, this may lower patients’ quality of life.Citation2 As a result of pain symptoms, patients may often find themselves unable to accept certain job tasks and assignments, which may lead to them losing their jobs. This may have several negative consequences on the psychological status of patients.Citation3 Further, unrelieved pain may also negatively affect patients’ social interactions, as the decline in physical and mental functioning caused by persistent pain contributes greatly to impaired social relationships and interactions.Citation3 Thus, pain decreases individuals’ quality of life and markedly decreases their mental and physical health status.Citation3 Therefore, ICU patients require adequate pain assessment and management. However, there are several barriers to effective pain assessment and management among ICU patients.Citation4 For example, although pain is a highly subjective experience, ICU patients’ deteriorated level of consciousness and intubation limits their ability to communicate, which complicates their pain assessment and management.Citation4
In addition to patient-related barriers, other barriers related to healthcare providers and systems complicate pain assessment and management among adult critical care patients.Citation5 For example, studies have found nurses and physicians to have low levels of knowledge, poor attitudes, and inadequate training related to pain assessment and management for adult critical care patients.Citation6 Furthermore, heavy workloads, high patient-provider ratios, tight work schedules, and the unavailability of standard pain protocols in adult critical care units are factors that contribute to the issue of unrelieved pain.Citation5
Moreover, consensus is yet to be reached on the most effective pain assessment tools and pain management measures for adult critical care patients. The American Society for Pain Management Nursing recommends relying on pain-related behaviors to evaluate and treat pain among intubated patients or patients with communication deficits.Citation4 Several nonverbal scales have been approved as valid tools for pain assessment among adult critically ill patients, such as the Behavioral Pain Scale (BPS) and Critical-Care Pain Observation Tool (CPOT).Citation7 However, such tools have been limited by their low specificity and sensitivity for pain indicators, particularly in nonverbal patients, as well as nurses’ misunderstanding, misinterpretation, and underestimation of pain behaviors and nurses’ poor knowledge and attitudes related to the use of such tools.Citation7 Physiological measures, such as blood pressure, heart rate, and respiratory rate, are sometimes used as alternative pain indicators and can provide important clues for proper pain assessment.Citation8 However, the 2012 Society of Critical Care Medicine (SCCM) guidelines do not recommend the use of these measures alone for pain evaluation in critically ill adult patients; rather, these measures should be used in combination with the evaluation of behavioral indicators of pain.Citation2
Pain management for critically ill adult patients in ICUs is classified into pharmacologic and non-pharmacologic treatments.Citation1 Analgesics are the first-line therapy for pain.Citation9 However, the use of analgesics has many adverse effects, including dizziness, physical dependence, vomiting, intolerance, respiratory depression, delayed extubation, induced bowel dysfunction, increased length of hospitalization and healthcare costs, and increased morbidity and mortality.Citation9 According to Gaskin and Richard,Citation10 the extra annual costs of pain management on the healthcare system in the US were between $261-$300 billion in 2010. Several nonpharmacological therapies for pain are cost-effective, easy-to-use, and free of adverse effects. The guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption (PADIS) recommend the use of nonpharmacological interventions, such as music therapy/calming voice and massaging, to target pain among critically ill adults and minimize the harmful side effects of the recurrent and long-term use of analgesics.Citation11
Pain assessment and management in adult ICU patients has been gaining research attention for over 25 years.Citation1 However, pain is still a serious health problem around the world and is still untreated or undertreated among adult ICU patients.Citation1,Citation2 Unfortunately, pain experienced by adult ICU patients remains widely underrecognized and undertreated due to various barriers.Citation2 Furthermore, there remains a wide gap between the findings of previous research and clinical practice. Moreover, there is no evidence in the nursing literature regarding the barriers and facilitators of pain assessment and management in adult critical care adult patients as perceived by nurses. Therefore, summarizing and synthesizing the existing research on pain assessment and management among adult critical care adult patients is needed to guide clinical practice and future research.
Aim
Accordingly, this review aims to identify nurses’ perceived barriers to and facilitators of pain assessment and management in adult critical care patients.
Materials and Methods
Study Design
The current study employed a systematic review design utilizing structured questions retrieved after reviewing the nursing literature relevant to pain among adult critical care patients. The researchers of the current review carefully evaluated and assessed the selected studies and compared their findings to reach consensus and avoid incongruities. This systematic review was guided by the following question: what are the patient-, nurse-, and system-related barriers and facilitators which impact pain assessment and management in adult critical care patients?
Inclusion Criteria
The studies included in the review were (1) peer-reviewed quantitative or qualitative studies, (2) published in English in the last ten years, (3) conducted among critical care nurses, and (4) related to the barriers and facilitators of adequate pain assessment and management in adult critical care patients.
Exclusion Criteria
Studies which were (1) dissertations, (2) book chapters, (3) conducted on target populations other than nurses, (4) conducted in clinical settings other than adult critical care units, or (5) written in languages other than English were excluded from this systematic review.
Search Strategy
An electronic search was performed by two of the researchers to identify all qualitative and quantitative published articles which discussed nurses’ perceived barriers to and facilitators of pain assessment and management in adult critical care patients. The review was conducted in April 2021. No search specifications related to publication date were set, and the researchers thoroughly searched the following databases: EBSCO, MEDLINE, CINAHL, and PubMed. The following keywords were used: “nurse”, “critical care nurses”, “pain”, “critically ill patients”, “adult”, “mechanically ventilated patients”, “critical care unit”, “intensive care unit”, “knowledge”, “attitude”, “pain assessment”, “pain management”, “barriers”, “facilitators”, “enablers”, and “challenges”.
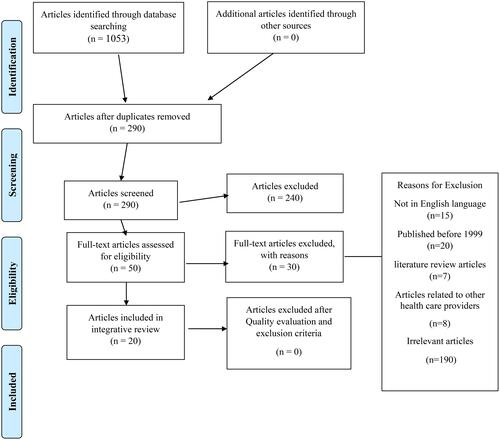
The researchers used the Boolean operators “AND” and “OR” to expand the search options and search the literature in more depth. The search of articles was limited to qualitative and quantitative research studies published in English and with the abstract and reference list available, using “title/” or “abstract” in the search field. After an initial search using different combinations of the previously mentioned keywords, 1053 studies were identified, and after removing exact duplicates or overlapping studies, 290 articles remained. After applying the inclusion and exclusion criteria, the retrieved articles were reduced to 50. The reference lists of all 50 articles were reviewed to identify any other relevant studies not identified through the database searches. Then, after a careful review of the abstracts of the articles in order to determine the main objectives and keywords of the studies and whether pain assessment and management in critical care patients was the main theme, a total of twenty studies were selected for review. below shows the Preferred Reporting Items for Meta-Analysis (PRISMA) checklist and flowchart used as a method of screening and selecting the studies eligible for the current review.
Figure 1 PRISMA flow chart.
Quality of Evidence Appraisal Assessment
The researchers assessed the selected studies using the guidelines of Melnyk and Fineout-Overholt.Citation12 Two of the researchers carried out a detailed review of the guidelines and independently evaluated each study until an agreement on each study’s quality [level of evidence (LOE)]was reached.
Data Synthesis
The researchers developed an evidence-based table to summarize the detailed information of the selected studies (). The following steps were taken to carry out data synthesis: (1) description of the selected studies in terms of the aims of the study, design, population, level of evidence, and major results; (2) identification of the limitations and strengths of the selected articles; and (3) investigation of the main study results to identify heterogeneity and homogeneity.
Table 1 Summary of the Detailed Information of the Selected Studies
Results
Description of the Selected Studies
The selected 20 articles were found to employ different methodologies. Four studies were qualitative,Citation13–Citation16 six were correlational,Citation17–Citation22 three were quasi-experimental,Citation23–Citation25 six were descriptive,Citation26–Citation31 and one was longitudinal.Citation21 The included studies were conducted on critical care patients admitted to various clinical settings, including cardiac units,Citation13,Citation18 oncology units,Citation28 emergency critical care units,Citation29 and neurosurgical units.Citation22 In addition to the abovementioned clinical settings, the majority of the studies also included other settings, such as medical-surgical units, medical units, and burn units.Citation21,Citation27 Only Wang and TsaiCitation20 and Asman et alCitation17 were conducted in medical centers.
The proportion of female participants in the selected studies ranged from 40% to 99.7%, while the proportion of male participants ranged from 14.3% to 63.2%. Six of the studies were conducted in European countries.Citation13,Citation15,Citation16,Citation21,Citation26,Citation32 Of the remaining studies, five were conducted in Asia,Citation14,Citation17,Citation20,Citation27,Citation28 five in North America,Citation18,Citation19,Citation22,Citation23,Citation25 and four in East Africa.Citation24,Citation29–Citation31 Critical care nurses’ pain assessment and management practices used among intensive care unit patients were measured using the Pain Assessment and Management for the Critically Ill survey in three of the studies.Citation18,Citation19,Citation27 In all three of these studies, a panel of experts had reviewed the instrument’s clarity, content validity, and reliability. To measure critical care nurses’ knowledge of and attitudes towards pain evaluation and management, four studies used the Nurses’ Knowledge and Attitudes Survey Regarding Pain (NKASRP).Citation20,Citation28,Citation31 Knowledge of pain management and barriers to pain control were assessed using the Brockopp-Warden Pain Knowledge/Bias Questionnaire [BWPKBQ] in two studies.Citation23,Citation25 Details regarding the measures used in the selected studies are summarized in for quantitative studies and for qualitative studies. Meanwhile, presents a summary of the 20 reviewed studies.
Table 2 The Summary of the Measures Used in the Selected Quantitative Studies
Table 3 The Summary of the Measures Used in the Selected Qualitative Studies
Strengths and Limitations of the Selected Studies
Some of the strengths of the selected studies included the use of a large sample size,Citation19,Citation25,Citation28 multicenter analysis such as Roos-Blom et al,Citation32 and the recruitment of samples from several units.Citation14,Citation27,Citation29,Citation31 Also, most of the studies reported using valid instruments to examine the study variables. However, the studies also had various limitations. For example, some studies had limited generalizability due to the use of convenience, consecutive, and purposive sampling techniques.Citation18,Citation19,Citation25,Citation27–Citation29,Citation31,Citation33 Also, in ten of the studies, most of the participants were female, and therefore, the results may not be representative of the targeted populations.Citation14,Citation17,Citation24,Citation26,Citation29,Citation31,Citation33 Other limitations included low response ratesCitation18,Citation19,Citation32 and small sample sizes.Citation15,Citation23,Citation26,Citation29,Citation31 Additionally, the majority of the selected articles were descriptive correlational studies, which did not allow for causality inference to be established.
Nurse-Related Barriers
Fifteen of the selected studies reported poor knowledge among nurses regarding critically ill patients’ pain as being a barrier to effective pain relief. Eight of the 15 studies reported nurses’ lack of knowledge regarding pain assessment,Citation13,Citation14,Citation18,Citation19,Citation25,Citation27,Citation33 five reported poor knowledge regarding pain management,Citation20,Citation23,Citation24,Citation29,Citation34 and only two reported both.Citation28,Citation31 The remaining studies did not discuss the link between nurses’ knowledge and pain assessment and management in critically ill adult patients. Deficits in knowledge related to pain assessment and management were most frequently related to (1) behavioral pain indicators (eg facial expressions);Citation17,Citation19,Citation28 (2) perception of patient’s pain tolerance (eg patient with severe pain cannot be distracted);Citation28,Citation31 (3) the use of verbal and nonverbal pain assessment tools;Citation13,Citation14,Citation18,Citation27,Citation33 (4) pharmacological pain management,Citation20,Citation23,Citation28,Citation31 especially among post-operative patientsCitation16 and those with terminal illnesses;Citation24 and (5) nonpharmacological management.Citation29
Among the selected studies, 13 discussed nurses’ poor attitudes as being a barrier to effective pain control. Five of these studies reported that the majority of critical care nurses had improper and infrequent use of behavioral pain assessment tools for nonverbal patients.Citation14,Citation18,Citation19,Citation23,Citation27 Also, four studies mentioned that nurses underestimate the importance of pain assessment for sedated patients or patients with a decreased level of consciousness.Citation14,Citation18,Citation19,Citation23,Citation27 Furthermore, most of the participating critical care nurses relied on measuring physiological parameters or observing odd behaviors when assessing critical care patients’ pain rather than using formal pain assessment tools.Citation18,Citation19,Citation26,Citation28,Citation33 Moreover, although self-reporting is the gold standard for pain assessment, three studies reported that nurses perceived self-reporting of pain to be an inaccurate measure of pain intensity among critically ill adult patients.Citation24,Citation27,Citation30 Another three studies found that nurses perceived there to be no need to assess pain or administer primitive analgesia before carrying out pain-inducing procedures.Citation19,Citation21,Citation30
Khalil and MashaqbehCitation28 reported that the majority of the participating nurses tended to encourage their patients to endure pain as much they could before offering analgesia. The study also reported that patients’ spiritual beliefs did not play a significant role in patients’ under-reporting of pain. Only KhalilCitation29 highlighted nurses’ misconceptions related to “fear of addiction” and how these misconceptions relate to the issue of pain under treatment or un-treatment in critically ill patients. According to Wang and TsaiCitation20 and Kizza and Muliira,Citation30 the majority of nurses perceived there to be no need for administering analgesics to sedated patients receiving pain-inducing procedures, as nurses perceived these patients to not feel pain. Moreover, in some cases, nurses were found to be unsure about the patient’s pain rating, which limited their administration of analgesics.Citation13,Citation27 Also, Topolovec-Vranic et alCitation22 discussed analgesics misuse as being a barrier to pain management in critically ill patients.
Nurse-Related Facilitators
A limited number of the reviewed studies discussed improved knowledge among nurses as being a facilitator of optimal pain relief.Citation17,Citation19,Citation27,Citation28,Citation31 The most frequently reported facilitators of pain management in adult critically ill patients were (1) better understanding and interpretation of pain behaviors,Citation18,Citation19,Citation27 (2) sufficient knowledge of pharmacological interventions,Citation17,Citation28,Citation31 and (3) ongoing education and professional training related to pain assessment and management.Citation23,Citation25 Furthermore, taking into account physiological indicators, in addition to verbal and nonverbal indicators, when carrying out pain assessment was found to facilitate pain management in adult critically ill patients.Citation18,Citation19 Moreover, improved perception of patients’ pain among nurses was found to be another facilitator of pain management.Citation18
Patient-Related Barriers and Facilitators
Despite the relatively large number of research studies examining patient-related barriers to pain assessment and management, only eight of the reviewed studies discussed these barriers from the perspective of critical care nurses. The most frequently reported barrier was patients’ inability to communicate,Citation13,Citation18,Citation22 followed by hemodynamic instability.Citation18,Citation29 Also, it was found that patient history of substance abuse, alcoholism, or suicidal attempts impeded proper pain management.Citation20,Citation23 Only five of the 20 studies reported examples of patient-related facilitators of pain assessment and management.Citation13,Citation20,Citation22,Citation24,Citation28 The gold standard of pain assessment is self-reporting of pain by the patient. Thus, three studies reported patients’ self-reporting of pain as being the most accurate measure of pain and a facilitator of effective pain management.Citation20,Citation24,Citation28 In the study of Alasiry et al,Citation13 the participants emphasized the importance of using subjective assessment for critically ill conscious patients. With regard to the objective assessment of pain in critical care patients, the most commonly reported behavioral pain indicators were motor activity (eg, involuntary movements) and facial activity (eg, facial grimacing).Citation13 Even in cases where the patients were unable to verbalize their needs, the nurses used alternative methods in addition to behavioral indicators, such as helping patients write or draw their needs on paper. Moreover, in the study of Pollmann-Mudryj,Citation22 the participating nurses reported that if they continued to rely on behavioral indicators only to interpret patients’ pain, communication between nurses and patients would be lost.
Physician-Related Barriers and Facilitators
Only eight of the reviewed studies discussed physician-related barriers and enablers of pain management. The most frequently reported barrier was “physicians’ prescription of analgesics does not depend on the evaluation of pain scores”.Citation18,Citation19,Citation22 Also, Deldar et al,Citation14 reported that poor interaction between physicians and nurses regarding nonverbal patients’ pain impedes effective treatment. Moreover, Subramanian et alCitation16 reported junior doctors’ lack of experience and senior doctors’ heavy workloads as being significant barriers to effective pain assessment and management. As for the facilitators of pain assessment and management in critically ill adult patients, collaboration between physicians and nurses was the most frequently reported facilitator,Citation13,Citation17 followed by “adequate analgesics doses prescribed by physicians”.Citation18,Citation30
System/Organization-Related Barriers
Of the 20 selected studies, 12 articles discussed barriers to pain management associated with organizational factors. The barriers reported most frequently were (1) lack of standardized pain assessment forms and tools for verbal critically ill patientsCitation16,Citation30 and nonverbal patients,Citation14,Citation19,Citation20 (2) lack of standardized guidelines and protocols for pain evaluation and control,Citation14,Citation16,Citation19,Citation30,Citation32 (3) heavy workloads of nurses,Citation14,Citation18,Citation30 (4) nursing staff shortages,Citation13,Citation29 (5) inadequate nurse-to-patient ratios,Citation14,Citation32 (6) inadequate training and education related to pain assessment and management,Citation14,Citation19,Citation22,Citation30 (7) nontherapeutic, ineffective, or complicated discussions about pain treatment during medical rounds,Citation18 (8) lack of documentation of pain assessment findings,Citation30 (9) lack of autonomous decision-making related to pain management,Citation16,Citation20 and (10) poor hospital environments, such as shared rooms with only curtains between patients.Citation15 Also, only HamdanCitation27 found a significant relationship between hospital type and adequate pain assessment by nurses, whereby nurses in private and governmental hospitals used pain assessment tools less often than did nurses in educational hospitals.
System/Organization-Related Facilitators
Only six studies discussed system-related facilitators of pain assessment and management among adult critically ill patients, and the most frequently reported facilitators were (1) continuous education and professional training for critical care nurses,Citation13,Citation18–Citation20,Citation28,Citation29 and (2) discussing and reporting patients’ pain scores during nurse-to-nurse handovers.Citation18,Citation19,Citation30 Furthermore, higher hospital accreditation was significantly associated with improved pain assessment practices.Citation20 Moreover, WøienCitation21 reported that establishing evidence-based protocols for pain evaluation and documentation led to improved pain control plans. The perceived barriers and facilitators to pain assessment and management in critical care patients are summarized in .
Table 4 The Barriers to and Facilitators of Pain Assessment and Management
Discussion
This review included 20 studies published over the previous 10 years and focused on the barriers and facilitators related to pain assessment and management in critical care units from the perspective of nurses. A limited number of relevant studies were identified. Nurse-related barriers were studied more than other forms of barriers (ie, patient- and system-related barriers), with insufficient education and training related to pain assessment among nurses being the most commonly reported nurse-related barrier. This particular finding is consistent with the findings of a recent systematic review which found nurses’ knowledge deficiencies and poor skills to be significant barriers to pain assessment among nursing home residents.Citation35
Nurse-Related Barriers and Facilitators
Given that they spend most of their time caring for patients, nurses play a major role in pain assessment in critically ill patients.Citation36 However, limited studies have explored nurse-related barriers to pain assessment. According to the literature review of McAuliffe et al,Citation36 nurses have deficient knowledge related to pain assessment in people with dementia (PWD). This is consistent with our review results regarding nurses’ lack of knowledge related to pain assessment, as PWD share some characteristics with critically ill patients, such as difficulty self-reporting pain. Also, in the current review, poor knowledge of nurses regarding pain management among ICU patients was found to be a barrier to effective pain relief. Similarly, several previous studies have reported that nurses’ lack of knowledge regarding postoperative pain management impeded the achievement of optimal pain control.Citation37
A previous systematic review emphasized the importance of using behavioral pain indicators for pain assessment in patients with communication deficits, as opposed to relying only on self-reporting to assess pain. Similar to our findings, the most commonly reported behavioral pain indicators were motor activity (eg involuntary movements) and facial activity (eg facial grimacing).Citation38 In our review, nurses were found to misunderstand these behavioral indicators, thus complicating the effective assessment and prompt management of pain in critical care patients.Citation17,Citation19,Citation28 This misunderstanding may be due to inconsistency in these behaviors between critical care patients and nurses’ lack of knowledge, in addition to poor formal nursing education and clinical training.Citation38
Tolerance of pain differs from one person to another. Several factors influence patients’ pain tolerance, including emotions and lifestyle factors.Citation39 According to Saifan et al,Citation39 nurses had several beliefs and misconceptions related to patients’ pain tolerance which act as barriers to effective pain management. For example, they believe that patients with severe pain cannot be distracted. These findings support the finding of our review that using both verbal and nonverbal pain assessment tools for critical care patients is essential for optimal pain evaluation because it provides a holistic and comprehensive assessment of pain and allows nurses to feel more confident. By using both verbal and nonverbal pain assessment tools for critical care patients, nurses capture affective and physiological components of the pain experience and become certain regarding suspected pain in critical care patients.Citation19,Citation28 Several studies are consistent with our review findings, indicating that nurses’ lack of knowledge regarding how to use verbal and nonverbal pain assessment tools is a major barrier to pain relief.Citation40 For example, a review of the literature related to pain in PWD found nurses to have poor knowledge and practices related to the use of pain assessment tools.Citation40
Adequate administration of pharmacological interventions, specifically opioids, plays an important role in effective pain management.Citation39 However, only three of the selected studies reported sufficient knowledge among nurses regarding pharmacological management as being a facilitator of adequate pain relief. Consistent with this finding, several published studies reported nurses’ lack of knowledge regarding pharmacological management of pain as being a significant barrier to pain management.Citation40 This includes lack of knowledge regarding opioids usage, dosage, and routes of administration.Citation39 Moreover, there is limited evidence regarding nurses’ knowledge of pharmacological pain management and how it relates to effectively assess and promptly treat pain among critical care patients.
Prolonged use of analgesics has many adverse effects on patients’ health status.Citation9 For that reason, nonpharmacological interventions may be an effective alternative for pain control among critically ill patients.Citation11 There is limited evidence related to nurses’ knowledge of and attitudes towards the use of nonpharmacological interventions among adult critically ill patients. In the present review, only one study was found to explore this issue, and this study reported insufficient knowledge among nurses regarding the use of nonpharmacological interventions.Citation29 Despite the limited evidence in the literature, there are conflicting findings regarding nurses’ levels of knowledge and attitudes related to nonpharmacological interventions in general. According to Puntillo et al,Citation1 nurses working in medical and surgical wards had a satisfactory level of knowledge regarding nonpharmacological pain interventions. Conversely, the study of Munkombwe et al,Citation41 which was conducted to investigate nurses’ palliative care practices, showed nurses to have inadequate knowledge and poor attitudes related to nonpharmacological management.
Nurses’ attitudes and beliefs related to pain may influence nurses’ provision of proper pain management.Citation2 More than half of the reviewed studies reported such attitudes and beliefs as being either facilitators of or barriers to pain assessment and management. For example, although behavioral pain assessment tools have limitations, frequent observing or monitoring of pain behaviors using validated and reliable assessment tools is an essential pain assessment practice in the case of patients who have difficulty self-reporting pain.Citation2 However, some of the reviewed studies reported infrequent use of behavioral pain assessment tools by critical care nurses when caring for nonverbal patients. Similarly, SamarkandiCitation42 found ICU nurses to have poor attitudes towards behavioral pain assessment. However, these poor attitudes were found to improve after nurses were taught how to use the Critical-Care Pain Observational Tool (CPOT) for nonverbal patients. Also, a scoping review conducted to explore the issue of pain management in pediatric intensive care units reported poor attitudes among nurses regarding the use of valid nonverbal pain assessment tools.Citation43 Furthermore, several studies conducted in different countries and settings reported negative attitudes among nurses towards pain assessment and management.Citation42 Moreover, Devlin et alCitation11 explored the beliefs of nurses regarding sedation and found the misconception that “sedated patients don’t feel pain at all” to be a major barrier to adequate pain management. This finding supports the findings of about one-third of the reviewed studies.
In the current review, two studies reported that nurses emphasized monitoring physiological and behavioral indicators as being an important aspect of pain assessment, which facilitates pain management in adult critically ill patients. However, overreliance on measuring physiological parameters or observing odd behaviors rather than using formal pain assessment tools to assess critical care patients’ pain was identified as being a major barrier to pain management in the present review. Although physiological parameters such as blood pressure and heart rate can be used to evaluate patients’ pain and provide important clues for effective pain assessment,Citation8 it is not recommended that formal pain assessment tools are replaced with these parameters when evaluating pain in critically ill adult patients.Citation2
A systematic review study conducted to review pain education interventions for nurses working in acute hospital settings reported that different types of education interventions had improved nurses’ attitudes towards and knowledge of pain and increased their confidence in their abilities to assess and manage patients’ pain.Citation44 This finding is consistent with the findings of our review regarding the impact of education programs on improving nurses’ knowledge of and attitudes towards pain in adult critically ill patients. However, future interventional research studies are recommended to bridge the knowledge gap in the literature regarding the role of ongoing education and professional training related to pain for critical care nurses as facilitators of pain management.
Patient-Related Barriers and Facilitators
Pain self-reporting is considered the best way to assess patients’ pain, due to the high subjectivity of the pain experience.Citation20 Only three of the reviewed studies reported the patient’s ability to self-report pain as being a facilitator of pain evaluation. According to Kizza et al,Citation33 a significant proportion of nurses do not trust or believe in patients’ self-reporting of pain. Two of the studies selected in our review reported that nurses did their best to encourage critically ill conscious patients to self-report their pain using different methods. However, this is not always possible, especially for patients with severe cognitive impairments or communication deficits.Citation20 A systematic review conducted to explore cancer patient-related barriers to pain management reported patients’ inability to communicate as being one of the major barriers to effective pain management.Citation45 Also, several studies reported similar findings among different patient groups and in different clinical settings.Citation46 These findings are similar to our finding that the most commonly reported patient-related barrier, as perceived by critical care nurses, was patients’ inability to communicate.
Physiological and behavioral indicators are significant pain clues and should be used in addition to other assessment tools to optimize pain management.Citation8 However, there is a lack of consistency and specificity regarding the use of these indicators, which may complicate the assessment and management of pain in critically ill patients. Consistent with our finding, Reardon et alCitation47 found hemodynamic instability to be a perceived barrier to pain assessment and management.
Though uncommon, drug addiction during the management of pain may occur.Citation9 Therefore, aberrant drug behaviors should be closely monitored to detect addiction and potential drug abuse, especially in patients with a history of substance abuse or alcoholism, when administering opioids to manage pain in such patients.Citation48 According to Passik et al,Citation48 patients with a history of substance abuse and those receiving opioids have more serious aberrant drug behaviors as compared to patients with no history of drug abuse. Consistent with our review findings, PaiceCitation49 revealed having a history of misuse of opioids or alcoholism to be a major barrier to pain management in cancer patients.
Physician-Related Barriers and Facilitators
A recent systematic review, which explored physician-related barriers to effective cancer pain management revealed several barriers as perceived by physicians, including deficiencies in knowledge regarding the use of opioids in cancer pain management, fear of addiction, concerns related to the side effects of opioids, inadequate pain assessment, and inadequate analgesics prescription.Citation50 In our review, physicians’ adequate prescription of analgesics was perceived by nurses to be a facilitator of effective pain management. Also, both our review and the review of Jacobsen et alCitation50 found physicians’ workloads and improper interpretation of pain scores as being barriers to adequate pain management. Our review found that insufficient interaction between physicians and nurses impedes effective pain treatment, while improved collaboration between physicians and nurses was found to be a major facilitator. Several previous studies have also reported that poor collaboration between nurses and physicians impedes optimal pain relief.Citation6,Citation51,Citation52
System-Related Barriers and Facilitators
The presence of standardized protocols and guidelines for pain evaluation and management is essential for optimal pain management.Citation53 Consistently, our review found that the most frequently reported system-related barrier to effective pain management in critical care unit patients was the lack of standardized pain assessment tools and guidelines and pain management protocols. WøienCitation21 also reported that establishing evidence-based protocols for pain evaluation and documentation is essential for facilitating pain control. Similar findings were also reported by a recent integrative review conducted among hospitalized PWD, which found the lack of standardized pain assessment tools and guidelines to be a major barrier to pain management.Citation53
Heavy nurses’ workloads and high nurse-patient ratios are considered major barriers to optimal pain control.Citation5 However, there is limited evidence in the literature related to these barriers and their association with unrelieved pain in critically ill patients. According to previous studies, the quality of care provided to patients suffering from pain differed significantly according to the type of hospital (ie, public or private).Citation54 However, in our review, only a single study was found to have explored the association between hospital type and the tools used to assess pain in critically ill patients.Citation27
In the current review, it was found that most critical care nurses had a lack of education regarding pain management, and about half of the reviewed studies highlighted the importance of continuous and professional pain education for critical care nurses. Consistently, several previous studies have emphasized the importance of updating nurses’ information related to pain assessment and management in verbal and nonverbal patients.Citation54 Ineffective or complicated discussions about pain treatment during medical rounds were also identified as being a system-related barrier to effective pain management in this review. Similarly, three previous studies have reported that reporting and discussing the pain scores of patients during nurse-to-nurse handovers facilitates effective pain management.Citation54–Citation56
Documentation of pain assessment and management is essential for ensuring the provision of good quality pain control, as it enhances communication between healthcare providers and leads to consistency in assessment data.Citation55,Citation56 However, poor nursing documentation of pain assessment findings was identified in this review as being a barrier to pain management. Also, Rafati et alCitation56 revealed that nurses’ lack of documentation of postoperative pain management findings contributed to poor patient outcomes. Moreover, although limited studies in our review discussed the role of nurses’ autonomous decision-making in pain management, reporting it to be insufficient among critical care unit nurses, several published studies have reported that nurses’ lack of autonomous decision-making impedes effective pain management.Citation57
Providing adequate levels of privacy in hospital environments has also been found to facilitate nurses’ pain assessment and management practices.Citation55,Citation58 This finding supports the finding of the current review that issues related to lack of patient privacy, such as shared rooms with no curtains between patients, were significant barriers to pain control among critical care patients. Other system-related barriers pertaining to the hospital environment, such as crowded wards, early discharge of patients, and nursing staff shortages were identified in a recent review.Citation58
Limitations of the Review
This review has several limitations. These limitations include the heterogeneity of the selected studies and the limited availability of relevant studies which examine the primary variables. Also, this review included studies published in English only, while there may be other studies written in other languages investigating the main study variables. Also, in comparison to other studies, some of the reviewed studies were conducted on small samples, which limits the generalizability of the findings of these studies. Further, the reviewed studies were conducted in different countries and regions around the world. Therefore, there may have been confounding variables which were not taken into consideration, but which may have impacted the results, therefore impacting the generalizability of the findings. Finally, another limitation is that most of the reviewed studies were cross-sectional and prospective cohort studies, which limits the determination of causality.
Relevance to Clinical Practice
The findings of our study could help hospital managers in developing continuous education and staff development training programs on assessing and managing pain for critical care patients. Establishing continuous education, workshops, professional developmental lectures focusing on pain evaluation and treatment for both critical care nurses and physicians, as well as training courses on how to use pain assessment tools and other behavioral pain indicators, especially for nonverbal patients are highly recommended. Also, our findings could be used to develop an evidence-based standard pain management protocol tailored to effectively assess and promptly treat the pain of critical care patients and emphasizing the importance of alternative and complementary medicine of pain.
Conclusion
Adequate pain control barriers and facilitators among intensive care unit nurses remain insufficiently researched. Effective pain management in critical care units relies on nurses’ knowledge of and attitudes towards pain assessment and relief. Also, various barriers to and facilitators of effective pain relief, including patient-related, nurse-related, physician-related, and system-related were identified and examined in the reviewed studies. The most frequently reported barriers in this study included nurses’ lack of knowledge regarding the use of pain assessment tools, patients’ inability to communicate, physicians’ prescription of analgesics being independent of pain scores evaluation, and absence of standardized guidelines and protocols for pain evaluation and control. For the facilitators, the most reported ones include ongoing education and professional training related to pain assessment and management, patients’ ability to self-report pain, effective collaboration between physicians and nurses, and productive discussion of patients’ pain scores during nurse-to-nurse handovers.
Acknowledgments
We want to thank the librarians of Jordan University of Science and Technology for their help.
Disclosure
The authors declare no conflicts of interest for this work.
References
- Puntillo KA, Max A, Timsit J-F, et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am J Respir Crit Care Med. 2014;189(1):39–47.
- Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306.
- Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457. doi:10.2147/JPR.S105892
- Gélinas C. Pain assessment in the critically ill adult: recent evidence and new trends. Intensive Crit Care Nurs. 2016;34:1–11. doi:10.1016/j.iccn.2016.03.001
- Alotaibi K, Higgins I, Day J, Chan S. Paediatric pain management: knowledge, attitudes, barriers and facilitators among nurses–integrative review. Int Nurs Rev. 2018;65(4):524–533. doi:10.1111/inr.12465
- Mamhidir A-G, Sjölund B-M, Fläckman B, Wimo A, Sköldunger A, Engström M. Systematic pain assessment in nursing homes: a cluster-randomized trial using mixed-methods approach. BMC Geriatr. 2017;17(1):1–16. doi:10.1186/s12877-017-0454-z
- Stamp R, Tucker L, Tohid H, Gray R. Reliability and validity of the critical-care pain observation tool: a rapid synthesis of evidence. J Nurs Meas. 2018;26(2):378–397. doi:10.1891/1061-3749.26.2.378
- Korving H, Sterkenburg P, Barakova E, Feijs L. Physiological measures of acute and chronic pain within different subject groups: a systematic review. Pain Res Manag. 2020;2020:1–10. doi:10.1155/2020/9249465
- Berde C, Nurko S. Opioid Side Effects—Mechanism-Based Therapy. Mass Medical Soc; 2008.
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. doi:10.1016/j.jpain.2012.03.009
- Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–e873.
- Melnyk BM, Fineout-Overholt E. Evidence-Based Practice in Nursing & Healthcare: A Guide to Best Practice. Lippincott Williams & Wilkins; 2011.
- Alasiry S, Löfvenmark C. Nurses’perceptions of pain assessment and pain management for patients with myocardial infarction in a coronary care unit. Middle East J Nurs. 2013;7(5):9–22.
- Deldar K, Froutan R, Ebadi A. Challenges faced by nurses in using pain assessment scale in patients unable to communicate: a qualitative study. BMC Nurs. 2018;17(1):1–8. doi:10.1186/s12912-018-0281-3
- Lindberg J-O, Engström Å. Critical care nurses’ experiences:“A good relationship with the patient is a prerequisite for successful pain relief management”. Pain Manag Nurs. 2011;12(3):163–172. doi:10.1016/j.pmn.2010.03.009
- Subramanian P, Allcock N, James V, Lathlean J. Challenges faced by nurses in managing pain in a critical care setting. J Clin Nurs. 2012;21(9–10):1254–1262. doi:10.1111/j.1365-2702.2011.03789.x
- Asman O, Slutsker E, Melnikov S. Nurses’ perceptions of pain management adequacy in mechanically ventilated patients. J Clin Nurs. 2019;28(15–16):2946–2952. doi:10.1111/jocn.14896
- Rose L, Haslam L, Dale C, et al. Survey of assessment and management of pain for critically ill adults. Intensive Crit Care Nurs. 2011;27(3):121–128. doi:10.1016/j.iccn.2011.02.001
- Rose L, Smith O, Gélinas C, et al. Critical care nurses’ pain assessment and management practices: a survey in Canada. Am J Crit Care. 2012;21(4):251–259. doi:10.4037/ajcc2012611
- Wang HL, Tsai YF. Nurses’ knowledge and barriers regarding pain management in intensive care units. J Clin Nurs. 2010;19(21‐22):3188–3196. doi:10.1111/j.1365-2702.2010.03226.x
- Wøien H. Movements and trends in intensive care pain treatment and sedation: what matters to the patient? J Clin Nurs. 2020;29(7–8):1129–1140. doi:10.1111/jocn.15179
- Topolovec-Vranic J, Canzian S, Innis J, Pollmann-Mudryj MA, McFarlan AW, Baker AJ. Patient satisfaction and documentation of pain assessments and management after implementing the adult nonverbal pain scale. Am J Crit Care. 2010;19(4):345–354. doi:10.4037/ajcc2010247
- Lewis CP, Corley DJ, Lake N, Brockopp D, Moe K. Overcoming barriers to effective pain management: the use of professionally directed small group discussions. Pain Manag Nurs. 2015;16(2):121–127. doi:10.1016/j.pmn.2014.05.002
- Machira G, Kariuki H, Martindale L. Impact of an educational pain management programme on nurses’ pain knowledge and attitudes in Kenya. Int J Palliat Nurs. 2013;19(7):341–345. doi:10.12968/ijpn.2013.19.7.341
- Schreiber JA, Cantrell D, Moe KA, et al. Improving knowledge, assessment, and attitudes related to pain management: evaluation of an intervention. Pain Manag Nurs. 2014;15(2):474–481. doi:10.1016/j.pmn.2012.12.006
- Gerber A, Thevoz A-L, Ramelet A-S. Expert clinical reasoning and pain assessment in mechanically ventilated patients: a descriptive study. Aust Crit Care. 2015;28(1):2–8. doi:10.1016/j.aucc.2014.06.002
- Hamdan KM. Nurses’ assessment practices of pain among critically ill patients. Pain Manag Nurs. 2019;20(5):489–496. doi:10.1016/j.pmn.2019.04.003
- Khalil H, Mashaqbeh M. Areas of knowledge deficit and misconceptions regarding pain among jordanian nurses. Pain Manag Nurs. 2019;20(6):649–655. doi:10.1016/j.pmn.2019.02.010
- Khalil NS. Critical care nurses’ use of non-pharmacological pain management methods in Egypt. Appl Nurs Res. 2018;44:33–38. doi:10.1016/j.apnr.2018.09.001
- Kizza I, Muliira J. Nurses’ pain assessment practices with critically ill adult patients. Int Nurs Rev. 2015;62(4):573–582. doi:10.1111/inr.12218
- Ufashingabire CM, Nsereko E, Njunwa KJ, Brysiewicz P. Knowledge and attitudes of nurses regarding pain in the intensive care unit patients in Rwanda. Rwanda J. 2016;3(1):21–26. doi:10.4314/rj.v3i1.4F
- Roos-Blom M-J, Dongelmans D, Stilma W, Spijkstra JJ, de Jonge E, de Keizer N. Association between organizational characteristics and adequate pain management at the intensive care unit. J Crit Care. 2020;56:1–5. doi:10.1016/j.jcrc.2019.11.010
- Kizza IB, Muliira JK, Kohi TW, Nabirye RC. Nurses’ knowledge of the principles of acute pain assessment in critically ill adult patients who are able to self-report. Int J Afr Nurs Sci. 2016;4:20–27. doi:10.1016/j.ijans.2016.02.001
- Wang J, Xiao LD, He GP, De Bellis A. Family caregiver challenges in dementia care in a country with undeveloped dementia services. J Adv Nurs. 2014;70(6):1369–1380. doi:10.1111/jan.12299
- Knopp-Sihota JA, Dirk KL, Rachor GS. Factors associated with pain assessment for nursing home residents: a systematic review and meta-synthesis. J Am Med Dir Assoc. 2019;20(7):884–892. e883. doi:10.1016/j.jamda.2019.01.156
- McAuliffe L, Nay R, O’Donnell M, Fetherstonhaugh D. Pain assessment in older people with dementia: literature review. J Adv Nurs. 2009;65(1):2–10. doi:10.1111/j.1365-2648.2008.04861.x
- Dessie M, Asichale A, Belayneh T, Enyew H, Hailekiros A. Knowledge and attitudes of Ethiopian nursing staff regarding post-operative pain management: a cross-sectional multicenter study. Patient Relat Outcome Meas. 2019;10:395. doi:10.2147/PROM.S234521
- de Knegt NC, Pieper MJ, Lobbezoo F, et al. Behavioral pain indicators in people with intellectual disabilities: a systematic review. J Pain. 2013;14(9):885–896. doi:10.1016/j.jpain.2013.04.016
- Saifan AR, Bashayreh IH, Al-Ghabeesh SH, et al. Exploring factors among healthcare professionals that inhibit effective pain management in cancer patients. Cent Eur J Nurs Midwifery. 2019;10(1):967. doi:10.15452/CEJNM.2019.10.0003
- Burns M, McIlfatrick S. Palliative care in dementia: literature review of nurses’ knowledge and attitudes towards pain assessment. Int J Palliat Nurs. 2015;21(8):400–407. doi:10.12968/ijpn.2015.21.8.400
- Munkombwe WM, Petersson K, Elgán C. Nurses’ experiences of providing nonpharmacological pain management in palliative care: a qualitative study. J Clin Nurs. 2020;29(9–10):1643–1652. doi:10.1111/jocn.15232
- Samarkandi OA. Knowledge and attitudes of nurses toward pain management. Saudi J Anaesth. 2018;12(2):220. doi:10.4103/sja.SJA_587_17
- Ismail A, Forgeron P, Polomeno V, Gharaibeh H, Dagg W, Harrison D. Pain management interventions in the paediatric intensive care unit: a scoping review. Intensive Crit Care Nurs. 2019;54:96–105. doi:10.1016/j.iccn.2019.05.002
- Drake G, Williams A. Nursing education interventions for managing acute pain in hospital settings: a systematic review of clinical outcomes and teaching methods. Pain Manag Nurs. 2017;18(1):3–15. doi:10.1016/j.pmn.2016.11.001
- Jacobsen R, Møldrup C, Christrup L, Sjøgren P. Patient‐related barriers to cancer pain management: a systematic exploratory review. Scand J Caring Sci. 2009;23(1):190–208. doi:10.1111/j.1471-6712.2008.00601.x
- Dequeker S, Van Lancker A, Van Hecke A. Hospitalized patients’ vs. nurses’ assessments of pain intensity and barriers to pain management. J Adv Nurs. 2018;74(1):160–171. doi:10.1111/jan.13395
- Reardon DP, Anger KE, Szumita PM. Pathophysiology, assessment, and management of pain in critically ill adults. Am J Health Syst Pharm. 2015;72(18):1531–1543. doi:10.2146/ajhp140541
- Passik SD, Kirsh KL, Donaghy KB, Portenoy RK. Pain and aberrant drug-related behaviors in medically ill patients with and without histories of substance abuse. Clin J Pain. 2006;22(2):173–181. doi:10.1097/01.ajp.0000161525.48245.aa
- Paice JA. Cancer pain management and the opioid crisis in America: how to preserve hard‐earned gains in improving the quality of cancer pain management. Cancer. 2018;124(12):2491–2497. doi:10.1002/cncr.31303
- Jacobsen R, Sjogren P, Moldrup C, Christrup L. Physician-related barriers to cancer pain management with opioid analgesics: a systematic review. J Opioid Manag. 2007;3(4):207–214. doi:10.5055/jom.2007.0006
- Ozawa M, Yokoo K. Pain management of neonatal intensive care units in Japan. Acta Paediatr. 2013;102(4):366–372. doi:10.1111/apa.12160
- Ishikawa H, Kawagoe K, Kashiwagi M, Yano E. Nurse-physician collaboration in pain management for terminally ill cancer patients treated at home in Japan. J Palliat Care. 2007;23(4):255–261. doi:10.1177/082585970702300403
- Tsai I-P, Jeong -SY-S, Hunter S. Pain assessment and management for older patients with dementia in hospitals: an integrative literature review. Pain Manag Nurs. 2018;19(1):54–71. doi:10.1016/j.pmn.2017.10.001
- Tse MMY, Ho SS. Enhancing knowledge and attitudes in pain management: a pain management education program for nursing home staff. Pain Manag Nurs. 2014;15(1):2–11. doi:10.1016/j.pmn.2012.03.009
- Mędrzycka-Dąbrowska WA, Dąbrowski S, Basiński A. Perception of barriers to postoperative pain management in elderly patients in Polish hospitals‐a multicentre study. J Nurs Manag. 2016;24(8):1049–1059. doi:10.1111/jonm.12405
- Rafati F, Soltaninejad M, Aflatoonian MR, Mashayekhi F. Postoperative pain: management and documentation by Iranian nurses. Mater Sociomed. 2016;28(1):36. doi:10.5455/msm.2016.28.36-40
- Rababa M, Al-Rawashdeh S. Critical care nurses’ critical thinking and decision making related to pain management. Intensive Crit Care Nurs. 2021;63:103000. doi:10.1016/j.iccn.2020.103000
- Taylor A, Stanbury L. A review of postoperative pain management and the challenges. Curr Anaesth Crit Care. 2009;20(4):188–194. doi:10.1016/j.cacc.2009.02.003
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi:10.1016/j.nedt.2003.10.001
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R, editors. Analysing Qualitative Data. London: Routledge; 1994:172–194.
- Downe‐Wamboldt B. Content analysis: method, applications, and issues. Health Care Women Int. 1992;13(3):313–321. doi:10.1080/07399339209516006
- Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009;62(10):e1–e34.
