Abstract
Background
The sacroiliac (SI) joint is frequently the primary source of low back pain. Over the past decades, a number of different SI injection techniques have been used in its diagnosis and therapy. Despite the concerns regarding exposure to radiation, image-guided injection techniques are the preferred method to achieve safe and precise intra-articular needle placement. The following study presents a comparison of radiation doses, calculated for fluoroscopy and CT-guided SI joint injections in standard and low-dose protocol and presents the technical possibility of CT-guidance with maximum radiation dose reduction to levels of fluoroscopic-guidance for a precise intra-articular injection technique.
Objective
To evaluate the possibility of dose reduction in CT-guided sacroiliac joint injections to pulsed-fluoroscopy-guidance levels and to compare the doses of pulsed-fluoroscopy-, CT-guidance, and low-dose CT-guidance for intra-articular SI joint injections.
Study design
Comparative study with technical considerations.
Methods
A total of 30 CT-guided intra-articular SI joint injections were performed in January 2012 in a developed low-dose mode and the radiation doses were calculated. They were compared to 30 pulsed-fluoroscopy-guided SI joint injections, which were performed in the month before, and to five injections, performed in standard CT-guided biopsy mode for spinal interventions. The statistical significance was calculated with the SPSS software using the Mann–Whitney U-Test. Technical details and anatomical considerations were provided.
Results
A significant dose reduction of average 94.01% was achieved using the low-dose protocol for CT-guided SI joint injections. The radiation dose could be approximated to pulsed-fluoroscopy- guidance levels.
Conclusion
Radiation dose of CT-guided SI joint injections can be decreased to levels of pulsed fluoroscopy with a precise intra-articular needle placement using the low-dose protocol. The technique is simple to perform, fast, and reproducible.
Introduction
The sacroiliac (SI) joint has been implicated as the primary source of pain in 10%–26.6% of patients with chronic low back pain.Citation1,Citation2 Whereas historical and physical examination findings have been previously advocated as useful tools in identifying patients with SI joint pain, more recent studies have demonstrated that they have limited diagnostic value.Citation3,Citation4 Blind, fluoroscopy-, and CT-guided SI joint injection techniques are well described in literature for the diagnosis and treatment of pain originating from SI joints.Citation5–Citation7 The purpose of image-guidance in spinal injections is to achieve safe and precise needle placement and accurate delivery of the injected solution, but the intra-articular needle placement can become problematic even in fluoroscopic-guidance due to the complex orientation and asymmetric anatomy of the SI joint.
Computed tomographic (CT) guidance for injections into the SI joint is the preferred method for some authors for precise intra-articular needle placement because of the complex configuration of the joint.Citation6 Long-lasting effects of intra-articular corticoids and TNF-alpha-inhibitors have been described for CT-guided SI injections in patients with sacroiliitis.Citation8,Citation9 Despite the precise intra-articular injection of medications in CT-guidance, radiation exposure remains a serious concern. The aim of the following study was to determine the possibility of rapid radiation dose reduction in intra-articular CT-guided SI joint injections to levels of fluoroscopy without a loss of accuracy in needle placement.
Materials and methods
A total of 30 CT-guided intra-articular sacroiliac joint injections were performed in January 2012 using a new technique in low-dose mode; the radiation doses were calculated. Inclusion criteria were: inpatient adults, suffering from low-back pain with irradiation to the buttocks, and positive SI joint provocation testing. Patients were excluded if they did not sign the informed consent, had an absolute indication for surgery, were non-adults, or were suffering from coagulopathy, gravidity, or infection. The results were compared to 30 pulsed-fluoroscopy-guided SI joint injections, which were performed during the month prior, and to five injections, performed in standard CT-guided biopsy mode for spinal interventions in the past year.
CT-guided injections were performed by one experienced interventionalist, using the SOMATOM Emotion CT-scanner (syngoCT 2009E, 16-slice solution; Siemens Medical Solutions AG, Erlangen, Germany). The standard intervention mode, used in past SI joint injections consisted of topogram acquisition (120 mA, 130 kV), spiral scan (80 mA, 130 kV), and biopsy mode (50 mA, 130 kV). The low-dose protocol consisted of topographic marking of the SI joint height based on anatomic landmarks (see anatomical and technical considerations) and the biopsy mode with reduced energy and tube current (50 mA, 80 kV). Fluoroscopy-guided injections were performed using the AXIOM Luminos dRF (Siemens Medical Solutions AG) in pulsed fluoroscopy mode (f/second = 7.5) for spinal interventions (60 mA, 75–80 kV).
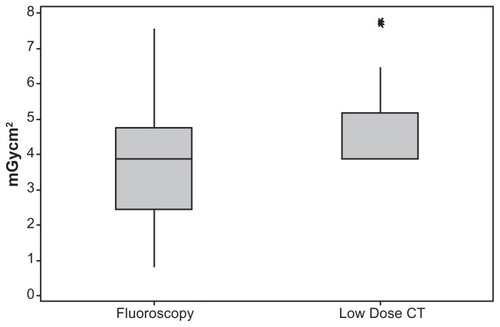
Statistical analyses were performed using SPSS statistical software (v 17.0; IBM, Armonk, NY). Descriptive and graphic analyses were provided for the radiation doses (mGycm2) for all groups (CT-guided conventional intervention mode, CT-guided low dose mode, and pulsed-fluoroscopy-guided SI joint injections). The radiation dose calculations of the two groups (pulsed-fluoroscopy vs low-dose CT) were compared with the Mann–Whitney U-test (α level = 0.05; H0: n1 = n2; H1: n1 ≠ n2).
Anatomical and technical considerations
The sacroiliac joint is a complex diarthrodial joint, consisting of bilateral asymmetric and incongruent corresponding joint surfaces of the ilium and the sacrum. Its multiplanar orientation, irregular joint gap, facultative accessory auricular surfaces or partial ankylosis make blind and fluoroscopy-guided intra-articular injections difficult.Citation10,Citation11 The joint is partly synovial and partly a syndesmosis, surrounded by thick dorsal and interosseous ligaments.Citation12 Together with the variability in surface orientation, they contribute to joint stability. Because the upper two-thirds of the SI joint become fibrotic during adulthood, most interventionalists prefer the caudal portions of the joint for intra-articular injections.Citation5,Citation10,Citation13
Standard protocols for CT-guided spinal injections usually start with a topogram acquisition. The purpose of topogram acquisition is to provide a gross anatomic orientation and selection of the area of interest for further scanning (spiral scan), reconstruction, and intervention. We modified all of these steps in the following manner:
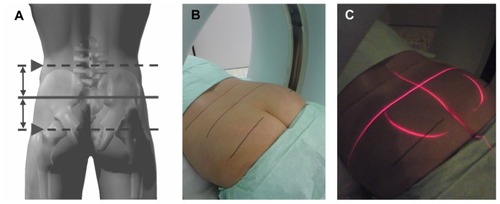
Because the gross anatomic SI joint localization can be estimated by palpable anatomic landmarks, the topogram acquisition as used in standard CT-guided interventions was abandoned. The topogram would result in a high level of radiation without significant gain in information. The SI joint location can be approximated by palpation of the following landmarks: sacrum, sacral cornua, and the posterior superior iliac spine. Based on the palpation of these landmarks, the length of the joint can be estimated. To be more precise, we developed a simple technique: to achieve an injection into the caudal portions of the joint, the patient is placed in prone position and the iliac crests and major trochanters of the femur are palpated bilaterally. A virtual horizontal midline is drawn between these structures. This line marks the height of the lower portions of the SI joints. The correct position of the CT-scanner is achieved when the scanner target-laser overlaps the drawn midline where the joint is expected and the topography is controlled by palpation of the sacral cornua located about 4–5 cm caudal to this line (see ).
No further scanning or reconstructions are needed. The biopsy mode is used with reduced energy and tube current to 50 mA and 80 kV for single shot scans. It is helpful to place both introducer needles (if performing bilateral SI joint injection) so that they cross the marked line (or the overlapping laser line) where the SI joints are expected before the first scan. This step provides a control of the right location (height) and simultaneously allows targeting along the marked line.
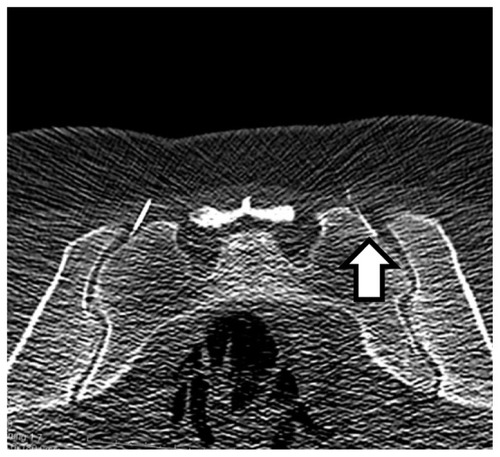
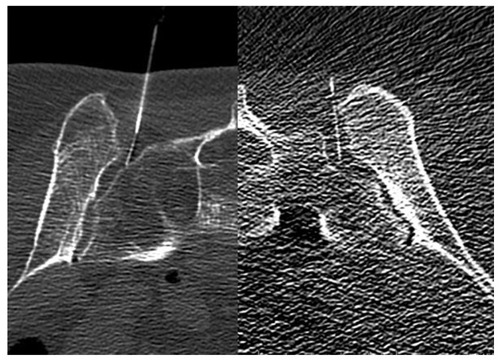
An average of 3–4 scans is needed for an injection into both SI joints. Despite the reduced image contrast, the bony structures and the needle are still visible even when using the thinnest needle caliber of 29 gauge (see and ).
Results
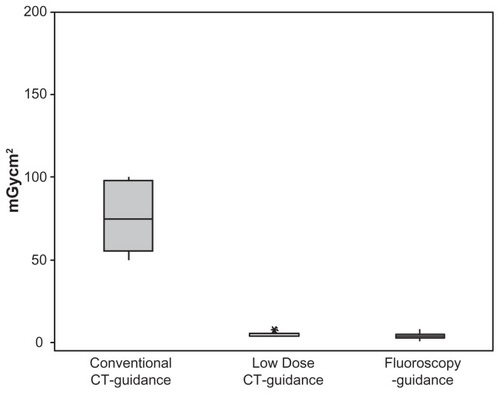
A total of 30 patients (22 female and 8 male, age 36–78 years, mean BMI 28.10, 95% confidence interval [CI]: 21.75–34.45) underwent bilateral CT-guided SI joint injections in the low-dose protocol in January 2012. The calculated mean radiation dose for these interventions was 4.57 mGycm2 (median = 3.890, 95% CI: 4.13–8.24, SD = 1.67), using an average of 3–4 scans per procedure. Retrospective data analyses of 30 bilateral pulsed-fluoroscopy-guided SI joint injections, performed in December 2011 presented a mean radiation dose of 3.73 mGycm2 (median = 3.895, 95% CI = 0–6.34, SD = 2.58). The five bilateral SI joint injections in conventional CT-intervention mode presented a mean radiation dose of 76.27 mGycm2 (95% CI: 49.31–103.24, SD = 21.72).
Using the established low-dose protocol for CT-guided intra-articular SI joint injections, the mean radiation dose could be reduced to 5.99% of the level used in conventional CT-guided biopsy mode for spinal interventions, achieving an average dose reduction of 94.01%. The calculated levels of the radiation doses could be approximated to the levels of pulsed fluoroscopy-guidance (see and ). When comparing the calculated radiation doses between the pulsed-fluoroscopy group and the low-dose CT group with the Mann–Whitney U-test, no significant difference between the groups was found (P = 0.1055, alpha level = 0.05). The technique was simple to perform, fast, and reproducible. After a short learning curve, intervention times (first scan to injection of medication) ranging 70–150 seconds were reached. Intra-articular needle positioning was achieved in all patients. Despite the decreased image quality, the injections could be performed even in obese patients and in patients with severe osteoporosis. These factors are usually limiting the radiation dose reduction in other spinal injections. There were no intra- or postprocedural complications.
Discussion
CT-guided SI joint injection radiation doses can be approximated to pulsed fluoroscopy levels using the technique and protocol described above. The learning curve for this technique is fast, the technique is easy to perform, and reproducible. Mean radiation doses of 4.57 mGycm2 (95% CI: 4.13–8.24) were achieved. The available data from literature suggest different radiation dose exposures in spinal interventions. While Shepherd et al describe general radiation doses of 199 mGycm2, Schmid et al calculated average radiation doses of 1.51–3.53 mSv (corresponding to 100.67–235.33 mGycm2) for conventional CT-guided injections and 0.22–0.43 mSv (corresponding to 14.67–28.67 mGycm2) for low-dose CT-guided injections and 0.1 mSv (corresponding to 6.67 mGycm2) for pulsed-fluoroscopy-guided injections.Citation14,Citation15 Leng et al calculated average skin radiation doses of 195 mGy for CT-guided injection procedures.Citation16 Hendrix et al calculated radiation doses ranging between 12–30 mGy in fluoroscopy-guided SI joint injections, while Vassiliev et al and Acho et al calculated mean skin radiation doses of 108 mGy and 37.4 mGy, respectively, based on phantom studies in fluoroscopically guided SI joint injections.Citation13,Citation17,Citation18 Compared to the protocol described in this study, a large reduction of the radiation dose could be achieved.
Despite the fact that most studies suggest that the level of fluoroscopy utilization is below a level of elevated concern, long-lasting effects of such radiation exposure are uncertain.Citation19,Citation20 Using fluoroscopy-guidance in spinal injections leads to radiation exposure of larger areas of the body in patients (back and pelvis) and the interventionalist (eg, hands, eyes, lower extremity).Citation19–Citation22 Radiation doses and exposure in CT-guided interventions are usually higher than in fluoroscopy-guided interventions. Due to the standardized use of fluoroscopy-guidance in SI joint injections in our department, the conventional CT-guidance was performed only in exceptional cases (eg, sacroiliitis, SI joint arthritis [five cases]), when strictly intra-articular application of medications was needed – therefore, the small number of five conventional CT-guided injections may be a possible limitation of this study. CT-guidance is, despite the higher exposure to radiation, still the most precise technique for intra-articular injections. Using the low-dose technique and protocol, significant reduction of radiation could be achieved, along with the benefit of precise needle positioning.
Disclosure
The authors report no conflicts of interest in this work.
References
- HansenHCMcKenzie-BrownAMCohenSPSwicegoodJRColsonJDManchikantiLSacroiliac joint interventions: a systematic reviewPain Physician200710116518417256029
- SchwarzerACAprillCNDerbyRThe false-positive rate of uncontrolled diagnostic blocks of the lumbar zygapophysial jointsPain1994581952007816487
- van der WurffPMeyneWHagmeijerRHClinical tests of the sacroiliac jointManual Ther2000528996
- RiddleDLFreburgerJKEvaluation of the presence of sacroiliac joint dysfunction using a combination of tests: a multicenter intertester reliability studyPhys Ther20028277278112147007
- DussaultRGKaplanPAAndersonMWFluoroscopy-guided sacroiliac joint injectionsRadiology2000214127327710644136
- HodgeJCMiscellaneous procedures: sacroiliac joint arthrographyHodgeJCMusculoskeletal imaging: diagnostic and therapeutic proceduresBasel, SwitzerlandKargerLandes Systems1997226227
- TheodoridisTInjection therapy of the spine without imagingDer Orthopäde2007367386
- BraunJBollowMSeyrekbasanFComputed tomography guided corticosteroid injection of the sacroiliac joint in patients with spondyloar-thropathy with sacroiliitis: clinical outcome and follow-up by dynamic magnetic resonance imagingJ Rheumatol1996236596648730123
- CuiYXiaoZShuxiaWComputed tomography guided intraarticular injection of etanercept in the sacroiliac joint is an effective mode of treatment of ankylosing spondylitisScand J Rheumatol201039322923220109079
- GuptaSDouble needle technique: An alternative method for performing difficult sacroiliac joint injectionsPain Physician20111428128421587331
- ForstSLWheelerMTFortinJDVilenskiJAThe sacroiliac joint: Anatomy, physiology and clinical significancePain Physician20069616816700283
- WalkerJMThe sacroiliac joint: A critical reviewPhys Ther1992729039161454866
- HendrixRWLinPJKaneWJSimplified aspiration or injection technique for the sacro-iliac joint. Brief NoteJ Bone Joint Surg198264A8124912527130238
- ShepherdTMHessCPChinCTGouldRDillonWPReducing Patient Radiation Dose during CT-Guided Procedures: Demonstration in Spinal Injections for PainAm J Neuroradiol201132101776178221920858
- SchmidGShmitzABorchardtDEffective Dose of CT- and Fluoroscopy-Guided Perineural/Epidural Injections of the Lumbar Spine: A Comparative StudyCardiovasc Intervent Radiol200629849116228853
- LengSChristnerJACarlsonSKRadiation Dose Levels for Interventional CT ProceduresAm J Radiol20111971w97w103
- VassilievDBlackwoodMKincelDPatient entrance skin dose during three most common fluoroscopy-guided pain proceduresReg Anesth Pain Med200328
- AchoSvan der MerweBvan der MerweDSkin doses in fluoroscopically guided interventional procedures in back pain managementS Afr Radiogr200947179
- BotwinKPThomasSGruberRDRadiation exposure of the spinal interventionalist performing fluoroscopically guided lumbar transforaminal epidural steroid injectionsArch Phys Med Rehab200283697701
- ManchikantiLCashKAMossTLRiveraJPampatiVSRisk of whole body radiation exposure and protective measures in fluoroscopically guided interventional techniques: A prospective evaluationBMC Anesthesiol200331212904269
- BotwinKPFreemanEDGruberRDRadiation exposure to the physician performing fluoroscopically guided caudal epidural steroid injectionsPain Physician2001434334816902680
- MaheshMFluoroscopy: patient radiation exposure issuesRadiographics20012141033104511452079