Abstract
Purpose
We aimed to assess uterine and arcuate artery Doppler indices in patients with mild primary dysmenorrhea.
Patients and Methods
A total of 55 patients were included, consisting of women without dysmenorrhea (n=26, group A) and women with mild primary dysmenorrhea (n=29, group B). Doppler measurements of the uterine and arcuate arteries were performed in both groups on the 1st-2nd days and 21st-24th days (midluteal phase) of the menstrual cycle using transvaginal ultrasound and compared between the groups. The severity of dysmenorrhea was assessed using visual analog scale scores.
Results
Doppler measurements of the uterine and arcuate arteries performed on the 1st-2nd days of the menstrual cycle and the midluteal phase were similar between the groups (p>0.05). There was a significant decrease in the intragroup measurements of uterine and arcuate arteries performed on the first day of menstruation and the luteal phase in both groups (p<0.01).
Conclusion
Doppler findings of the uterine and arcuate arteries did not differ between patients with and without mild primary dysmenorrhea. The etiology of primary dysmenorrhea mainly involves ischemia and vasoconstriction, but mild primary dysmenorrhea appears to be associated with a different etiology other than decreased tissue perfusion.
Introduction
Primary dysmenorrhea (PD) refers to painful menstruation, which manifests as cramping abdominal pain not caused by any other pelvic pathological condition.Citation1 The prevalence of PD is reported to be between 45% and 95%, representing a high number of women affected worldwide.Citation2 Sometimes nausea, vomiting, headache, bloating, back pain, and diarrhea can also accompany.Citation3 Mechanisms underlying PD are reported as increased prostaglandin production and release, which causes vasoconstriction and hypercontractility, or high intrauterine pressure causing activation of vasopressin receptors leading to ischemia and subsequent pain.Citation1,Citation2,Citation4,Citation5 As can be expected, the severity of pain would increase as the degree of ischemia increases and the blood flow of the uterus would decrease. Doppler ultrasonography (USG) is used for evaluating blood flow in various parts of the body. In this examination technique, vasoconstriction or increased vascular impedance manifests with elevated Doppler indices [pulsatility index (PI) and resistance index (RI)]. Therefore, Doppler USG stands out as a good method for detecting poor perfusion and vasoconstriction, which makes it a valuable technique for the evaluation of dysmenorrhea. Elevated indices on Doppler ultrasonography would be anticipated because vasoconstriction is one of the primary mechanisms of dysmenorrhea.Citation1,Citation6,Citation7 The intensity of pain due to PD can be evaluated using a visual analog scale (VAS), with “0” defining “no pain” and “10” representing the “worst imaginable pain”. PD can be divided into three categories according to the severity of the pain: mild, moderate, and severe. VAS scores of 1–3 describe “mild” pain.Citation4,Citation8
To our knowledge, no studies have evaluated uterine blood flow in patients with mild or moderate PD separately as described according to VAS scores. Altunyurt S et al reported increased PI and RI values of uterine and arcuate arteries and Dmitrovic R et al detected higher uterine artery RI values on the first day of menstruation compared with the control group in patients with PD; women with severe symptoms were excluded.Citation9,Citation10 These studies grouped patients with moderate and mild PD together and compared them with controls. The results of these studies support the mechanism that the pain in PD occurs due to decreased blood flow resulting from vasoconstriction.
Although the pathophysiology of PD has been widely discussed in the literature, MPD has not been evaluated in this manner. Even though women with MPD have very low pain scores, our purpose of evaluating patients with MPD was to contribute to the understanding of the pathophysiology of this particular condition. In this study, we evaluated the blood flow indices of the uterine and arcuate arteries by using transvaginal color Doppler USG to investigate the possibility of causes other than vascular changes in women with MPD.
Materials and Methods
This prospective comparative Doppler study was conducted in the Obstetrics and Gynecology Clinic of Şişli Memorial Hospital, Istanbul, between March and November 2019. Fifty-five women with regular menstruation aged 20–35 years were enrolled in the study. The patients were divided into two groups according to whether they had dysmenorrhea. Group A comprised women without dysmenorrhea (n=26) and group B consisted of patients with MPD (n=29). Mild lower abdominal pain felt on the 1st-2nd days of menstruation was considered MPD.Citation4 Women who reported a VAS score between 1 and 3 were included in group B. One condition for inclusion in the study was that the patients had not used oral contraceptives in the last 3 months. Study patients were asked not to use nonsteroidal anti-inflammatory drugs (NSAIDs) for at least 24 h before each measurement.
All women included in the study were nulliparous and admitted to our clinic for routine gynecological examinations (cervical screening). Beginning of dysmenorrhea symptoms within 2 years after menarche was required for the detection of PD.
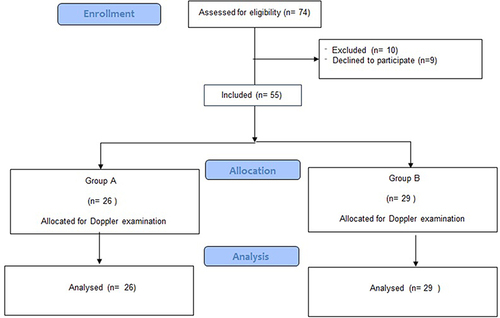
Exclusion criteria were previous abdominal surgery, abnormal uterine bleeding, genital tumor, ovarian cysts, abdominal inflammatory disorders, chronic pelvic pain, adenomyosis and endometriosis signs on USG, intrauterine device use, severe PD symptoms, diarrhea, and pain severe enough to interfere with daily activities or the use of drugs that could change blood flow, including acetylsalicylic acid.Citation11 Following the determination of their eligibility for the study, participants were scheduled for measurements on the 1st and 2nd days of menstruation and during the midluteal phase. The flow diagram of the study is presented in .
The study was approved by the Ethics Committee of Memorial Şişli Hospital (approval number: 2019/001, date: 28/02/2019) and written informed consent was obtained from all participants prior to examination.
In all women, transvaginal color Doppler measurements were conducted on both the uterine and arcuate arteries during the 1st-2nd days of the menstrual cycle, as well as during the midluteal phase, which typically falls between the 21st and 24th days of the same menstrual cycle. All Doppler measurements and USG examinations were performed by the same physician (K.Ö). Voluson S6 ultrasonography device (General Electric Ultrasound Korea, Ltd.) with an E8C endovaginal probe (3.5–11.5 MHz) was used for color Doppler measurements. In HD-Flow mode (bidirectional power Doppler), pulse repetition frequencies were adjusted to 0.9–7 kHz as needed to achieve a distinct signal. The wall motion filter cut-off frequency was set to 60 Hz to eliminate low-frequency signals and reduce artifacts. Doppler measurements were performed on one of the flow velocity waveforms after obtaining three similar consecutive waveforms.
Doppler measurements of the uterine arteries were performed at the site aligned with the internal cervical ostium and the arcuate arteries were identified at the outer layer of the myometrium.Citation9,Citation12 PI and RI values were assessed on both sides of the vessels. Each artery was measured three times and the average value was used for statistical calculations.
Statistical Analysis
The data obtained were processed using the Statistical Package for the Social Sciences software, version 22 (IBM SPSS Statistics; IBM Corporation). The normality of the data distribution was checked using the Shapiro–Wilk test. The study data were assessed using descriptive statistical techniques, including calculations for means and standard deviations. For normally distributed parameters, comparisons were conducted using the Student’s t-test, and non-normally distributed parameters were compared using the Mann–Whitney U-test. Fisher’s exact test and Chi-square tests were used to compare categorical variables. Intragroup comparisons of normally distributed parameters were performed using the paired-samples t-test, and statistical significance was considered when p < 0.05. The power analysis was based on a study by Altunyurt S et al.Citation10 As a result of the power analysis performed using the G*Power program, when the effect size, standard deviation, and α were considered 0.8, 0.05, and 0.05, respectively, for uterine artery measurements, with 80% power, the minimum number of patients was determined to be 26 for each group.
Results
The mean age of the entire study group (n=55) was 24.55±3.45 years. The mean age at the first menstruation was 12.96±1.62 (range, 11–19) years. The mean duration of menstrual periods was 4.84 (range, 3–7) days. No significant differences were detected between the groups regarding age, first menstrual age, duration of the menstrual period and body mass index (BMI) (p>0.05) ().
Table 1 Demographic Characteristics of the Groups
Unexplained infertility, which is a demographic factor that might influence dysmenorrhea was found in two and three patients, in groups A and B, respectively (Fisher’s exact test, p=0.999). Nine patients in group A and ten patients in group B were high school graduates, the others were university graduates (ꭓ2=0.00, p=0.99). There were no participants with a low-income level and all were urban residents. When comorbidities were evaluated, insulin resistance was present in six patients in group A and eight patients in group B, (ꭓ2=0.14, p=0.70). Three patients in group A and five patients in group B had hypothyroidism (Fisher’s exact test, p=0.70).
When intragroup Doppler values for the 1st-2nd menstrual day and midluteal phase were compared, significant decreases were found in the PI and RI values of the uterine and arcuate arteries in both groups. When the 1st-2nd menstrual day values were compared with the midluteal phase Doppler measurements, or the decrease in Doppler index measurements, similar values were obtained in the PI and RI values of the uterine and arcuate arteries (p>0.05). No statistically significant difference was found between the uterine and arcuate artery Doppler values of groups A and B (p>0.05). ( and ).
Table 2 Doppler Evaluation of the Groups
Table 3 The Decrease in Doppler Index Values Performed on the 1st-2nd Days and the Mid-Luteal Phase of Menstruation
Discussion
In the current study, we investigated whether there could be any reason other than vascular changes in the etiology of MPD, as determined using VAS, by evaluating the uterine and arcuate artery blood flow with color Doppler. We found that the Doppler indices of the uterine and arcuate arteries did not differ between women with and without MPD on the 1st-2nd days of menstruation or in the midluteal phase.
Dmitrović R reported elevated resistance to blood flow in the uterine, arcuate, radial, and spiral arteries in women with severe PD. This increased resistance to blood flow was observed consistently throughout the menstrual cycle.Citation1 In contrast, we found that blood flow was not altered in the uterine and arcuate arteries in women with MPD, different from those of patients with severe PD.
In a further study, increased RI was observed in the uterine, radial, and spiral arteries except for the arcuate artery on the first day of menstruation in patients with mild dysmenorrhea. Furthermore, the RI values of the uterine and arcuate arteries did not differ between the control and MPD groups in the luteal phase. However, mild dysmenorrhea was described as “pain in the lower abdomen on the first day of the cycle” without “systemic symptoms such as vomiting, diarrhea, headache, and syncope”, and women with PD were divided into two groups (mild and severe PD), without discriminating the intermediate group (moderate PD), thus MPD was not identified according to VAS scores and possibly involved women with moderate PD.Citation9 Similar to their results, in our study, the 1st-2nd menstrual day arcuate artery RI values did not differ significantly between the groups, but no difference was found in the 1st-2nd menstrual day uterine artery RI values. In line with Dmitrovic et al, we also observed similar RI values in the groups in the luteal phase for uterine and arcuate arteries.
Altunyurt et al reported significantly higher PI and RI values in the uterine and arcuate arteries in women with PD compared with controls on the first day of menstruation, but not in the midluteal phase. However, according to the severity of the pain, their study was conducted on a mixed group of patients involving both mild and moderate PD, excluding patients with severe PD.Citation10
When we look at previous articles, only one study by Dmitrovic et al included MPD as a separate group.Citation9 However, in that study, similar to Altunyurt et al, the patients were not divided into mild, moderate, and severe groups. The mild group also consisted of moderate group patients.Citation10 In our study, we included only women with MPD according to VAS scores, unlike the studies by Dmitrovic et al and Altunyurt et al. This may be a possible explanation for our divergent results from studies that reported increased uterine RI values in women with MPD on the first day of menstruation.Citation9,Citation10 Since the reason behind PD may also be increased pain perception or other factors and considering that the severity of pain is associated with decreased blood flow to the uterus, we hypothesized that blood flow of the uterus might not be altered in women with MPD.Citation3,Citation9 Therefore, only women with MPD were included in the present study. Another reason for including only patients with MPD in the study is that endometriosis is frequently observed in patients with advanced symptoms of dysmenorrhea.Citation10,Citation13
The addition of transvaginal sonography to the examination in patients with mild symptoms is a valuable method for evaluating uterine and adnexal pathologies. However, since symptoms of endometriosis may not be proportional to the severity of the disease, endometriosis may be asymptomatic or present with mild symptoms in many patients showing mild dysmenorrhea symptoms. Therefore, it may not be possible to fully exclude the presence of endometriosis with transvaginal sonography in patients with MPD.Citation14
Previous studies demonstrated increased resistance to blood flow in moderate and severe dysmenorrhea on the first day of menstruation, but in the current study, we found no difference in Doppler values between MPD patients and women without dysmenorrhea.Citation1,Citation9,Citation10,Citation15 The mechanism behind PD is accepted as the overproduction of prostaglandins, which causes hypercontractility, hypoxia, and ischemia of the myometrium.Citation2 Increased oxytocin and vasopressin levels are also involved in the pathophysiology of PD. The primary contributing factors to pain were reported as ischemia, elevated resting pressure, and elevated active pressure.Citation1 Supporting this knowledge, Uysal et al found a decrease in RI values of the uterine artery and VAS scores after three months of oral contraceptive pill use in patients with severe PD.Citation8 However, according to our results, the reason behind MPD may not be poor perfusion, rather, women with MPD may have a lower threshold for pain, as suggested by Dmitrovic et al. Granot et al stated that dysmenorrheic women had enhanced pain perception compared with women without dysmenorrhea. Thus, dysmenorrhea may also reflect enhanced pain perception.Citation3,Citation9 PD may also be caused by increased central sensitivity to pain. Some authors have regarded it as belonging to the category of central sensitivity syndromes, such as fibromyalgia and tension-type headaches. These syndromes involve an increased sensitivity to pain, even in the absence of tissue damage, inflammation, or physical lesions.Citation16,Citation17 Although not significant, Altunyurt et al detected high Doppler index values in the uterine vessels on the first day of menstruation in women without dysmenorrhea, which supports this approach.Citation10 Furthermore, it was observed that women experiencing dysmenorrhea were more susceptible to psychological conditions like depression, anxiety, and somatization.Citation3 Although we did not evaluate this point in our study, it is important to evaluate the conditions that may coexist with dysmenorrhea, which may have a role in pain perception in women with MPD.
Previous studies investigating uterine blood flow measured the radial and spiral arteries in patients with dysmenorrhea. However, from a clinical point of view, visualizing the radial and spiral arteries is difficult and not always possible in every patient and examination.Citation1,Citation9 We chose the uterine and arcuate arteries, which can be easily visualized on every USG examination, because our aim was to propose a clinically useful and easily applicable method. However, due to the easier treatment of MPD, additional evaluation with transvaginal Doppler ultrasonography may not be cost- and time-effective. Considering that this condition is more commonly observed in adolescents, it may not be suitable to evaluate these patients by transvaginal sonography, which is an uncomfortable examination in these young patients.
Our results indicate the possible role of other factors rather than ischemia in the pathophysiology of MPD, because no significant difference was found between the groups with and without MPD in all Doppler measurements. Based on the results of our study, we may say that the cause of pain is not necessarily always ischemia-related in patients with MPD but may be due to enhanced pain perception. Non-pharmacological therapeutic options may include using heating pads for menstrual cramps, getting additional rest or sleep, engaging in physical activity, practicing meditation, using aromatic oils, increasing calcium intake, and various food sources.Citation2
The limitations of our study are the small study population and the lack of psychological evaluations. Another limitation is that not all practitioners can perform a Doppler examination, thus symptoms remain the main stay of diagnosing PD. The strength is in its being the first study to investigate the arcuate and uterine arteries together with VAS examinations.
Conclusions
We found no increased resistance to blood flow in the uterine and arcuate arteries in women with MPD on 1st-2nd menstrual days of menstruation and at the midluteal phase. The etiology of primary dysmenorrhea mainly involves ischemia and vasoconstriction; however MPD appears not to be associated with these pathologies.
Abbreviations
PD, primary dysmenorrhea; USG, ultrasonography; VAS, visual analog scale; MPD, mild primary dysmenorrhea; NSAIDs, nonsteroidal anti-inflammatory drugs; PI, pulsatility index; RI, resistance index; BMI, body mass index.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We would like to thank Prof. Dr. Cenk Sayın and Assoc. Prof. Dr. Fatih Şanlıkan for their guidance and invaluable suggestions on the article.
References
- Dmitrović R. Transvaginal color Doppler study of uterine blood flow in primary dysmenorrhea. Acta Obstet Gynecol Scand. 2000;79(12):1112–1116. doi:10.1034/j.1600-0412.2000.0790121112.x
- Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21(6):762–778. doi:10.1093/humupd/dmv039
- Granot M, Yarnitsky D, Itskovitz-Eldor J, et al. Pain perception in women with dysmenorrhea. Obstet Gynecol. 2001;98(3):407–411. doi:10.1016/s0029-7844(01)01465-x
- Royo P, Alcázar JL. Three-dimensional power Doppler assessment of uterine vascularization in women with primary dysmenorrhea. J Ultrasound Med. 2008;27(7):1003–1010. doi:10.7863/jum.2008.27.7.1003
- Akerlund M. Vascularization of human endometrium. Uterine blood flow in healthy condition and in primary dysmenorrhoea. Ann N Y Acad Sci. 1994;734(1):47–56. doi:10.1111/j.1749-6632.1994.tb21735.x
- Hoskins PR. Measurement of arterial blood flow by Doppler ultrasound. Clin Phys Physiol Meas. 1990;11(1):1–26. doi:10.1088/0143-0815/11/1/001
- Guedes-Martins L, Gaio AR, Saraiva J, Cunha A, Macedo F, Almeida H. Uterine artery impedance during the first eight postpartum weeks. Sci Rep. 2015;5(1):8786. doi:10.1038/srep08786
- Uysal G, Akkaya H, Cagli F, et al. A comparison of two different oral contraceptives in patients with severe primary dysmenorrhoea. J Obstet Gynaecol. 2018;38(6):828–832. doi:10.1080/01443615.2017.1410533
- Dmitrovic R, Peter B, Cvitkovic-Kuzmic A, et al. Severity of symptoms in primary dysmenorrhea--a Doppler study. Eur J Obstet Gynecol Reprod Biol. 2003;107(2):191–194. doi:10.1016/S0301-2115(02)00372-X
- Altunyurt S, Göl M, Altunyurt S, et al. Primary dysmenorrhea and uterine blood flow: a color Doppler study. J Reprod Med. 2005;50(4):251.
- Andres MP, Borrelli GM, Ribeiro J, et al. Transvaginal Ultrasound for the Diagnosis of Adenomyosis: systematic Review and Meta-Analysis. J Minim Invasive Gynecol. 2018;25(2):257–264. doi:10.1016/j.jmig.2017.08.653
- Zaidi J, Pittrof R, Shaker A, Kyei-Mensah A, Campbell S, Tan SL. Assessment of uterine artery blood flow on the day of human chorionic gonadotropin administration by transvaginal color Doppler ultrasound in an in vitro fertilization program. Fertil Steril. 1996;65(2):377–381. doi:10.1016/S0015-0282(16)58103-5
- Sachedina A, Todd N. Dysmenorrhea, Endometriosis and Chronic Pelvic Pain in Adolescents. J Clin Res Pediatr Endocrinol. 2020;12(Suppl 1):7–17. doi:10.4274/jcrpe.galenos.2019.2019.S0217
- Vercellini P, Fedele L, Aimi G, Pietropaolo G, Consonni D, Crosignani PG. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum Reprod. 2007;22(1):266–271. doi:10.1093/humrep/del339
- Aksoy AN, Gözükara I, Kabil Kucur S. Evaluation of the efficacy of Fructus agni casti in women with severe primary dysmenorrhea: a prospective comparative Doppler study. J Obstet Gynaecol Res. 2014;40(3):779–784. doi:10.1111/jog.12221
- Yunus MB. Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Rheum. 2008;37(6):339–352. doi:10.1016/j.semarthrit.2007.09.003
- Ferries-Rowe E, Corey E, Archer JS. Primary Dysmenorrhea: diagnosis and Therapy. Obstet Gynecol. 2020;136(5):1047–1058. doi:10.1097/AOG.0000000000004096