Abstract
Introduction
Rectus sheath block is an emerging technique that provide effective perioperative analgesia and is related to lower perioperative opioid consumption and decrease opioid-related adverse effects. The present research is designed to explore the effect of rectus sheath block on recovery quality in patients following transabdominal midline gynecological surgery.
Methods
Ninety female patients following elective transabdominal midline gynecological surgery were enrolled. Patients were randomized to group R (n = 45) which receive preoperative ultrasound-guided RSB with 0.4% ropivacaine or group C which is control group (n = 45). The primary outcome was the quality of recovery on the first postoperative day. The quality of recovery was assessed by the 40-item Quality of Recovery questionnaire (QoR-40). Secondary outcomes included the intraoperative opioid consumption, time to first flatus and time to first discharging from bed, postoperative nausea and vomiting, and patient satisfaction.
Results
The patients in two groups had comparable baseline characteristics. Postoperative global QoR-40 scores were significantly better in group R than in group C (165.0[159.5-170.0] vs 155.0[150.0-157.0], respectively; median difference 12[95% confidence interval: 8-15, P<0.001]). Preoperative RSB reduced intraoperative opioid consumption, reduced the time to first flatus, time to first discharging from bed and the post anaesthesia care unit discharge time. Furthermore, group R showed greater patient satisfaction.
Conclusion
A single preoperative administration of RSB with ropivacaine improved the quality of recovery in patients following transabdominal midline gynecological surgery.
Plain Language Summary
Although laparoscopic surgery accounts for a higher proportion of gynecological procedures, open gynecological surgery remains irreplaceable for some patients. Recovery from open gynecological surgery is a combination of physical injuries and psychological challenges. Consequently, accelerating functional recovery, alleviating discomfort and improving the quality of recovery in such patients is a clinical issue that we need to focus on. The QoR 40 scale is a patient-reported assessment tool which evaluates the quality of recovery in five dimensions.
Ultrasound-guided rectus sheath block is a safe and effective abdominal wall nerve block for anesthesia and analgesia of umbilical and median abdominal longitudinal incisions. This study investigated the impact of rectus sheath block on the quality of postoperative recovery after open gynecological surgery using the QoR40 scale. Participants were randomized to two groups: rectus sheath block treatments and a control group receiving standard care only.
Rectus sheath block improves the quality of recovery in patients undergoing open gynecological surgery one day after surgery without adverse effects, which has successfully made rapid rehabilitation from bench to bedside.
Introduction
Many women will go through gynecological surgery in their lifetime. Laparoscopic gynecological surgery has recently become a popular technique and has significant advantages, for instance, reducing patients’ postoperative pain. However, transabdominal midline gynecological surgery is still necessary if there are intraoperative complications or abdominal adhesion. Transabdominal midline gynecological surgery results in a large wound and severe postoperative pain, hence, adequate postoperative analgesia is of great importance.
Enhanced recovery after surgery (ERAS) was first introduced by Kehlet for intestinal surgery and has since been widely used in various types of surgery. ERAS strategies recognize that opioid-induced nausea and vomiting and slowing of gastrointestinal motility which can interfere early mobilization and enteral feeding.Citation1 Indeed, as a cornerstone of ERAS, multimodal analgesia strategy is recommended and regional nerve block is an important compartment of it, providing effective pain management and, in turn, reducing the side effects associated with opioids. Ultrasound-guided rectus sheath block (RSB) was proposed as an abdominal truncal block by H. Willschke in 2006.Citation2 With the development of ultrasound, RSB has gained popularity in various abdominal surgeries due to high success rate and low complication rate.Citation3,Citation4 RSB provides analgesia effect for a midline incision by blocking the 7th to 11th intercostal nerves’ terminal branches within the rectus sheath.Citation5 Clinical studies have shown efficacy in sparing opioid consumption and accelerating recovery following RSB in laparoscopic surgery, however there are limited data on the quality of recovery after transabdominal midline gynecological surgery.Citation3,Citation4 This randomized controlled study looks forward to bring new ideas for postoperative recovery in this kind of surgery.
The 40-item quality of recovery questionnaire (QoR-40) is a dependable patient-oriented multidimensional assessment scale. It has been widely used to evaluate the quality of recovery after many kinds of surgery. The questionnaire consists of 40 items can be used to assess different aspects of recovery from anesthesia and surgery, including economic and social factors, psychological and physical aspects.Citation6,Citation7
The primary purpose of this study was to identify whether RSB could improve the quality of recovery in patients undergoing transabdominal midline gynecological surgery. And secondary outcomes were to evaluate intraoperative opioid consumption, time to first flatus and time to first discharging from bed, postoperative nausea and vomiting (PONV) and patient satisfaction.
Materials and Methods
Study Design
This trial adhered to the ethical guidelines of 1964 Helsinki Declaration and its later amendments. It was registered at Chinese Clinical Trial Registry (ChiCTR2000029163) and approved by Clinical Medical Research Ethics Committee of First Affiliated Hospital of Anhui Medical University (PJ2020-06-30).
Participants
All enrolled patients were scheduled to undergo elective transabdominal midline gynecological surgery at the first affiliated hospital of Anhui Medical University. The inclusion criteria were patients aged between 18 and 65 years with physical status of I to II according to the American Society of Anesthesiologists (ASA). Exclusion criteria included body mass index (BMI) >30 kg/m2, allergy to any drug used in this study, severe organ dysfunction, chronic analgesic use, contraindications to nerve block (coagulation disorders, puncture site infection), and refusal to participate. All enrolled patients signed a written informed consent.
Randomization and Blinding
Patients were distributed into the RSB group (group R) or control group (group C) by a random number table generated by computer. We used sealed and numbered envelopes to hide each patient’s allocation status. Three Participants implemented this study. The first participant allocated a sealed numbered envelope to each patient and then conducted RSB in patients which were allocated in group R after the induction of anesthesia. The other participants (did not know the allocation) conducted all the anesthetic management except the RSB procedure, and then assessed the outcomes.
Anesthesia Management
None of the patients received premedication. Harmonized monitoring was connected when patients were transferred into the operating room. After induction of general anesthesia with midazolam 0.02 mg/kg, propofol 2 mg/kg, sufentanil 0.4 μg/kg and rocuronium 0.8 mg/kg, laryngeal mask insertion was facilitated. All patients received intravenously injection of dexamethasone 8mg before anesthesia induction to prevent PONV. After anaesthesia induction, patients in group R received ultrasound-guided bilateral rectus sheath block with 20 mL of 0.4% ropivacaine (NAROPIN, Ropivacaine, AstraZeneca AB, Sodertalje, Sweden) on each side. Conducting a placebo block in group C would be harmful to control group, considering that RSB is an invasive procedure. Therefore, patients in group C underwent no block. Anesthesia was maintained by continuous pumping remifentanil, titrated to maintain the heart rate and mean blood pressure within 15% of baseline, propofol titrated to a Bispectral Index (between 40 and 60) (Aspect Medical Systems, Inc., Norwood, MA). Intraoperatively, cisatracurium was injected as needed.
Thirty minutes before the end of surgery, a patient-controlled intravenous analgesia (PCIA) pump (RenXian Medical Technology, Jiangsu, China) was programmed to provide a background infusion of 2 mL/h and a bolus dose of 2 mL according demand with a 15 min lockout interval. The PCIA pump was filled with sufentanil 3.75 μg/kg and flurbiprofen 1 mg/mL. All patients received PCIA for 72 h postoperatively. If the participants experienced any pain, they were instructed to press the PCIA button. Rescue analgesia was administered when the VAS score was > 50 mm even with the use of PCIA.
Interventions
RSB was administered after the induction of general anesthesia in the operation room. The patient was placed in a supine position with full exposure of the anterior abdominal wall. A wire-array probe (Model Edge; FUJIFILM SonoSite, Bothell, Washington, USA) was selected and coupling agent was applied to the probe and aseptically treated. Blocks were performed above, below and at the umbilicus depending on the specific surgical incision location. Place the probe across and perpendicular to the white line. Panning the probe horizontally outward reveals acoustic images of the lateral border of the rectus abdominis muscle, the internal oblique, the transversus abdominis muscle, and the external oblique. The 1–4 cm medial to the outer edge of the rectus abdominis muscle and the gap between the posterior rectus abdominis sheath and the rectus abdominis muscle are the target sites. We use the in-plane needle technique, the 22G puncture needle from any end of the probe into the needle tip through the rectus abdominis muscle is to enter the posterior rectus abdominis sheath, back to no blood can be injected local anesthetic. Ultrasonographically, the drug was seen to diffuse in a shuttle pattern in the superficial layers of the posterior rectus abdominis sheath.
Outcome Assessment
The primary outcome of this study was the QoR-40 questionnaire score on the first postoperative day. The QoR-40 is a 40-item scale measuring five dimensions: physical independence (5 items), pain (7 items), psychological support (7 items), emotional state (9 items) and physical comfort (12 items). Each item is rated on a 5-point Likert scale. The global QoR-40 score ranges from a minimum score of 40 (poor quality of recovery) to a maximum score of 200 (excellent quality of recovery).Citation8 It was designed to assess patients’ physical and mental condition after anesthesia and surgery, and it has been suggested as an appropriate measurement of outcome in many clinical situations.Citation9
The secondary outcomes consisted of cumulative intraoperative opioid consumption, time to first flatus, time to first discharging from bed, postoperative nausea and vomiting, and patient satisfaction. Patient satisfaction was assessed by a 10-point scale starting from 1 (poorest possible recovery) to 10 (best possible recovery) at 24 h postoperatively.
Sample Size Calculation
Previous research has reported that 10 or more difference in the global QoR-40 score was regarded as a clinically significant improvement in quality of recovery.Citation10 On the basis of preliminary experiment, we supposed that the global QoR-40 scores in group R on 24 h after surgery should be 10 points higher than those in group C. We set the predicted sample size as 37 per group according to a standard deviation of 13 and a power of 90% at an α level of 0.5. Taking into account a 20% drop-out rate, the final sample size in this trial was set at 45 per group.
Statistical Analysis
Statistical analysis were performed using SPSS 26.0 software (SPSS, Chicago, Illinois, USA). Continuous data were detected for normality of distribution via the Kolmogorov–Smirnov test. Categorical variables were reported as numbers (proportions). Continuous variables were described by the mean (standard deviation, SD) or median (interquartile range, IQR), as appropriate. To compare the differences across groups, independent-samples t-test (normal distribution), Mann–Whitney U-test (skewed distribution) and Fisher’s exact test or χ2 test (categorical variables) were undertaken. Linear regression is used to analyze the linear relationship between multiple independent variables and a dependent variable and to calculate the effect of each independent variable on the dependent variable. A two-tailed P value of less than 0.05 was considered statistically significant. The 95% confidence interval (95% CI) of the difference was given for statistical comparison.
Results
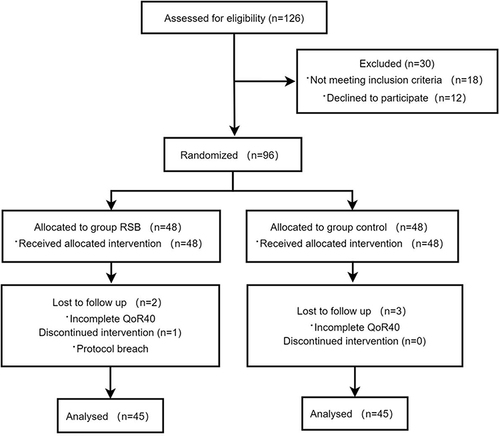
A total of 126 participants who were scheduled for elective transabdominal midline gynecological surgery between July 2020 and December 2021 were assessed for eligibility in this study. However, 30 were excluded for refusing to participate or meeting exclusion criteria. The other 96 were randomized, allocated, and treated following study protocol, with 90 patients entering the final data analysis (group R, n = 45; group C, n = 45). shows the consolidated standards of reporting trials (CONSORT) flow chart for participant recruitment. The demographic characteristics were comparable between two groups ().
Table 1 Demographic Characteristics of the Participants
The intraoperative data included the times and medications during operation were shown in . Intraoperative remifentanil dosage was less in group R compared to group C (P<0.001) (). There was no statistically significant difference in intraoperative sufentanil and propofol dosage, fluid intake and outflow, anesthesia time and operation time between the two groups ().
Table 2 Intraoperative Data
The preoperative and postoperative median (interquartile range) global QoR-40 scores are presented in . Postoperative global QoR-40 scores decreased in both groups compared with preoperative scores (P<0.001 for each). No statistically significant difference was found in the preoperative and postoperative day 3 QOR-40 scores between two groups ().
Figure 2 Global QoR-40 scores of two groups. The data are reported as the mean (SD) in each group.
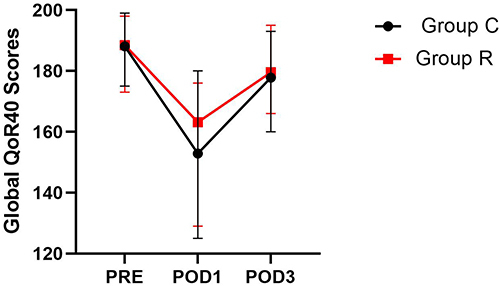
The postoperative data included global and dimensional scores of QoR-40 were shown in . Group R showed significantly better postoperative global QoR-40 scores than group C (165.0[159.5-170.0] vs 155.0[150.0-157.0], respectively; median difference 12 [P < 0.001]) (). Postoperative physical comfort and pain dimension scores were significantly higher in group R than in group C (P<0.001 for each). A significant effect of RSB was demonstrated for the global QoR-40 score and two dimension (physical comfort and pain) scores (all P<0.001). This revealed better quality of recovery with RSB. Nevertheless, scores in emotional status, physical independence and psychological support dimension were similar between groups (P=0.875, P=0.186, P=0.810) (). Compared with group C, time to first flatus and time to first discharging from bed in group R were shorter (P=0.009, P=0.035), apart form these, participants in group R met the PACU discharge criteria earlier (P= 0.047) (). Patient satisfaction scores were higher in group R (P<0.001) (). The number of participants presenting with PONV was 9 in group R and 12 in group C. There was no statistically significant difference in this aspect ().
Table 3 Postoperative Data
Multiple linear regression analysis was performed with age, group R, intraoperative remifentanil dosage and BMI as independent variables and QoR40 score on the first postoperative day as the dependent variable (). The Results of the significance test indicated that the effectiveness of RSB intervention on the QoR40 score on the first postoperative day was statistically significant (P=0.002).
Table 4 Results of Multiple Linear Regression Analysis
Discussion
This randomized, double-blind trial demonstrated that RSB was associated with higher overall QoR-40 scores in patients after transabdominal midline gynecological surgery than in controls. However, there was no statistically significant difference in QoR40 scores between two groups on the third postoperative day, which may be related to the fact that the effect of nerve block with ropivacaine had worn off by the third postoperative day. Meanwhile, in the dimension of pain, the group R score were higher than group C. This indicates that RSB may enhance recovery quality by alleviating postoperative pain. In addition, RSB provided better analgesia in the early postoperative period with fewer opioid-related side effects thus lead to the early recovery of gastrointestinal function.
The quality of recovery after surgery is not only related to pain control, but physical comfort as well. Differences in the dimension of physical comfort are likely due to PONV, tremors, sleep quality, etc. Perioperative opioid application is an important risk factor of PONV and tremors, but we did not find differences in the occurrence of PONV between two groups in this study.Citation11 Sleep quality after gynecological surgery is a vital factor which can affect postoperative recovery.Citation12 The significant difference in this domain may be contributed to the better sleep quality in group R due to the postoperative pain relief. In summary, these findings demonstrate that preoperative administration of RSB may be a promising postoperative analgesic strategy to promote early recovery and minimize the consumption of healthcare resources without increasing the incidence of adverse effects. Recovery after surgery is a complicated process that depends on patient, anesthetic and surgical factors.Citation13 Postoperative pain management is a crucial aspect of recovery after open gynecological surgery. Pain control in the early postoperative period is particularly critical. Inadequate pain control can lead to cardiopulmonary complications and increased morbidity and mortality.Citation14 In addition, the severity and duration of postoperative pain affects postoperative quality of recovery and life. The perioperative emotional state is in connection with the degree of persistent pain after surgery. This demonstrates the importance of emphasizing postoperative analgesia.Citation15 Regional anesthesia techniques provide excellent postoperative analgesia and improve the quality of postoperative recovery.Citation16 Our findings support the effectiveness of RSB as part of a multimodal analgesic strategy for transabdominal midline gynecological surgery. Apart from this, there are other effective ways to improve patients’ QoR-40 scores after surgery.Citation17
A few studies illustrated that RSB reduced patients’ opioid dosage after surgery, time to first analgesic use and incidence of PONV.Citation18,Citation19 Previous articles have concluded that RSB can provide effective analgesia after gynecological surgery. However, inconsistencies remain regarding local anesthetic dose, block plane, and block delivery time. The current literature reports that the dose of local anesthetic used for RSB is 15–20 mL per side of 0.25–0.5% ropivacaine is commonly used in clinical practice.Citation9 The dose used in this study followed the protocols commonly used in clinical applications and scientific research at our center. This trial demonstrated that patients treated with RSB had higher QoR-40 scores in the early postoperative period. This result confirmed the effects of RSB on quality of recovery after transabdominal midline gynecological surgery. In addition, patients in group R had shorter time to first flatus and shorter time to first discharging from bed and better patient satisfaction than those in group C. This may be attributed to the sparing of the opioid dosage, which in turn reduces opioid-related side effects. QoR-40 questionnaire was used to assess different dimensions of postoperative recovery in our study. Only the QoR-40 scoring system has been reported to meet eight different criteria (acceptability, reliability, feasibility, accuracy, interpretability, responsiveness, appropriateness, and validity) for measuring quality of recovery after outpatient surgery. The 40-item quality of recovery score has been recognized as applicable to many types of surgery. It is considered to be the most appropriate tool for measuring the complicated postoperative recovery process.Citation20–23
Our findings demonstrate for the first time that RSB accelerated recovery of patients undergoing transabdominal midline gynecological surgery. In initially establishing and validating the clinical utility of the global QoR-40, the designers considered a difference of 10 points or more to be indicative of a clinically relevant improvement in the quality of recovery.Citation24 Recently, Myles reported a change of 6.3 in global QoR-40 score can indicate a meaningful change in health status, which was known as minimal clinically important difference (MCID). Generally speaking, a difference of 10 point represent the equivalent of a 15% improvement in recovery quality. A median difference of 12 between group R and group C of global QoR-40 score on the first postoperative day has already exceeded the MCID.Citation25 Our results point to the fact that RSB significantly improves the postoperative health status of transabdominal midline gynecological surgery patients.
The QoR-40 questionnaire include five dimensions such as physical comfort, physical independence, psychological support, pain, and emotional status. All of these variables, with the exception of psychological support, depend primarily on the clinical and emotional status of the patient. Nevertheless, psychological support aspect primarily depend on the patients’ social status.Citation12 After surgery, QoR-40 scores of patients in both groups decreased on all subscales indicating that we should pay more attention to provide adequate psychological support during surgery. Transabdominal midline gynecological surgery is a common type of surgery worldwide. Nevertheless, strategies contributing to rapid recovery after transabdominal midline gynecological surgery have not yet been clarified. Researchers have shown that regional nerve block techniques provide excellent postoperative analgesia and also improve the quality of postoperative recovery.Citation26 For instance, TAP block enhances the recovery quality in patients following laparoscopic gynecological surgery. This article reported that patients in the TAP block group got a lower pain ratings in the early postoperative period and used fewer surgical instruments. Patients in the TAP block group were more likely to be discharged earlier from the hospital than those in the control group, with fewer opioids consumption in 24 hours after surgery.Citation27 Similar to TAP, RSB is not a new nerve block technique but is demonstrated for the first time in this study to improve the quality of recovery in the early postoperative period in patients undergoing transabdominal midline open gynecological surgery. It may provide a new feasible option for rapid postoperative recovery in this kind of patient.
No complications associated with RSB, such as puncture site infection and bleeding, local anesthetic toxicity, were occurred in this study. Indeed, ultrasound-guided RSB is a safe technique. It can be performed under deep sedation or general anesthesia to avoid undue anxiety. Unlike epidural anesthesia and paravertebral blocks, RSB can be performed safely in the presence of coagulation disorders, thereby reducing the incidence of serious complications and lowering healthcare costs.
There are also some limitations in this trial. First and foremost of all, to avoid bias, we did not assess the sensory block plane of the RSB; therefore, we may have missed some cases of block failure. Nevertheless, all RSBs were conducted by the same experienced anesthesiologist guided by ultrasound. Additionally, all of our patients were treated with appropriate multimodal analgesia and provided adequate analgesia. Second, although many researchers advocate placebo injections to minimize bias and thus improve the internal validity of a study, this may be harmful. Therefore, we did not inject placebo in the control group. Third, surgical infiltration was not performed in control group; this is not routinely used in our hospital.
Conclusions
In conclusion, our study shows that RSB improves recovery quality and promotes recovery of gastrointestinal function in patients undergoing transabdominal midline gynecological surgery. The concern about patient perceptions of recovery quality is growing. Therefore, we recommend the inclusion of RSB in a multimodal postoperative analgesic regimen. Different doses of local anesthetics for further comparative studies are urgently required to determine which method provides the best postoperative recovery outcome.
Disclosure
The authors declare no conflicts of interest in this work.
Data Sharing Statement
The authors declare that all data in the manuscript can be accessed upon request (contact e-mail: [email protected]).
Additional information
Funding
References
- Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691–697. doi:10.1001/jamasurg.2017.0898
- Willschke H, Bösenberg A, Marhofer P, et al. Ultrasonography-guided rectus sheath block in paediatric anaesthesia--a new approach to an old technique. Br J Anaesth. 2006;97(2):244–249. doi:10.1093/bja/ael143
- Yu S, Wen Y, Lin J, Yang J, He Y, Zuo Y. Combined rectus sheath block with transverse abdominis plane block by one puncture for analgesia after laparoscopic upper abdominal surgery: a randomized controlled prospective study. BMC Anesthesiol. 2024;24(1):58. doi:10.1186/s12871-024-02444-6
- Kim WJ, Mun JY, Kim HJ, et al. Surgical rectus sheath block combined with multimodal pain management reduces postoperative pain and analgesic requirement after single-incision laparoscopic appendectomy: a retrospective study. Int J Colorectal Dis. 2021;36(1):75–82. doi:10.1007/s00384-020-03725-5
- Zhu JL, Wang XT, Gong J, Sun HB, Zhao XQ, Gao W. The combination of transversus abdominis plane block and rectus sheath block reduced postoperative pain after splenectomy: a randomized trial. BMC Anesthesiol. 2020;20(1):22. doi:10.1186/s12871-020-0941-1
- Gao Y, Li H, Hu H, Xu Y, Zhou J, Liu Y. Effects of continuous fascia iliaca compartment block on early quality of recovery after total Hip arthroplasty in elderly patients: a randomized controlled trial. J Pain Res. 2022;15:1837–1844. doi:10.2147/JPR.S368285
- Yao Y, Li J, Hu H, Xu T, Chen Y. Ultrasound-guided serratus plane block enhances pain relief and quality of recovery after breast cancer surgery: a randomised controlled trial. Eur J Anaesthesiol. 2019;36(6):436–441. doi:10.1097/EJA.0000000000001004
- Kane SM, Garcia-Tomas V, Alejandro-Rodriguez M, Astley B, Pollard RR. Randomized trial of transversus abdominis plane block at total laparoscopic hysterectomy: effect of regional analgesia on quality of recovery. Am J Obstet Gynecol. 2012;207(5):419.e1–419.e4195. doi:10.1016/j.ajog.2012.06.052
- Rahiri J, Tuhoe J, Svirskis D, Lightfoot NJ, Lirk PB, Hill AG. Systematic review of the systemic concentrations of local anaesthetic after transversus abdominis plane block and rectus sheath block. Br J Anaesth. 2017;118(4):517–526. doi:10.1093/bja/aex005
- Kim MH, Kim MS, Lee JH, Kim ST, Lee JR. Intravenously administered lidocaine and magnesium during thyroid surgery in female patients for better quality of recovery after anesthesia. Anesth Analg. 2018;127(3):635–641. doi:10.1213/ANE.0000000000002797
- Choi H, Song JY, Oh EJ, Chae MS, Yu S, Moon YE. The effect of opioid-free anesthesia on the quality of recovery after gynecological laparoscopy: a Prospective Randomized Controlled Trial. J Pain Res. 2022;15:2197–2209. doi:10.2147/JPR.S373412
- Niu Z, Gao X, Shi Z, et al. Effect of total intravenous anesthesia or inhalation anesthesia on postoperative quality of recovery in patients undergoing total laparoscopic hysterectomy: a randomized controlled trial. J Clin Anesth. 2021;73:110374. doi:10.1016/j.jclinane.2021.110374
- Canıtez A, Kozanhan B, Aksoy N, Yildiz M, Tutar MS. Effect of erector spinae plane block on the postoperative quality of recovery after laparoscopic cholecystectomy: a prospective double-blind study. Br J Anaesth. 2021;127(4):629–635. doi:10.1016/j.bja.2021.06.030
- Liu Y, Xiao S, Yang H, et al. Postoperative pain-related outcomes and perioperative pain management in China: a population-based study. Lancet Reg Health West Pac. 2023;39:100822. doi:10.1016/j.lanwpc.2023.100822
- Hassett AL, Marshall E, Bailey AM, et al. Changes in anxiety and depression are mediated by changes in pain severity in patients undergoing lower-extremity total joint arthroplasty. Reg Anesth Pain Med. 2018;43(1):14–18. doi:10.1097/AAP.0000000000000682
- Zhang J, Jia D, Li W, Li X, Ma Q, Chen X. General anesthesia with S-ketamine improves the early recovery and cognitive function in patients undergoing modified radical mastectomy: a prospective randomized controlled trial. BMC Anesthesiol. 2023;23(1):214. doi:10.1186/s12871-023-02161-6
- Lu J, Wang JF, Guo CL, Yin Q, Cheng W, Qian B. Intravenously injected lidocaine or magnesium improves the quality of early recovery after laparoscopic cholecystectomy: a randomised controlled trial. Eur J Anaesthesiol. 2021;38(Suppl 1):S1–S8. doi:10.1097/EJA.0000000000001348
- Howle R, Ng SC, Wong HY, Onwochei D, Desai N. Comparison of analgesic modalities for patients undergoing midline laparotomy: a systematic review and network meta-analysis. Can J Anaesth. 2022;69(1):140–176. doi:10.1007/s12630-021-02128-6
- Hamid HKS, Ahmed AY, Alhamo MA, Davis GN. Efficacy and safety profile of rectus sheath block in adult laparoscopic surgery: a Meta-analysis. J Surg Res. 2021;261:10–17. doi:10.1016/j.jss.2020.12.003
- Bhatia K, Columb M, Wadsworth R, et al. Effect of rectus sheath block vs. spinal anaesthesia on time-to-readiness for hospital discharge after trans-peritoneal hand-assisted laparoscopic live donor nephrectomy: a randomised trial. Eur J Anaesthesiol. 2021;38(4):374–382. doi:10.1097/EJA.0000000000001337
- Kauffman JD, Nguyen ATH, Litz CN, et al. Laparoscopic-guided versus transincisional rectus sheath block for pediatric single-incision laparoscopic cholecystectomy: a randomized controlled trial. J Pediatr Surg. 2020;55(8):1436–1443. doi:10.1016/j.jpedsurg.2020.03.002
- Liang M, Xv X, Ren C, Yao Y, Gao X. Effect of ultrasound-guided transversus abdominis plane block with rectus sheath block on patients undergoing laparoscopy-assisted radical resection of rectal cancer: a randomized, double-blind, placebo-controlled trial. BMC Anesthesiol. 2021;21(1):89. doi:10.1186/s12871-021-01295-9
- Wang S, Liu P, Gao T, Guan L, Li T. The impact of ultrasound-guided bilateral rectus sheath block in patients undergoing cytoreductive surgery combined with hyperthermic intraperitoneal chemotherapy - a retrospective study. BMC Anesthesiol. 2020;20(1):197. doi:10.1186/s12871-020-01099-3
- Myles PS, Hunt JO, Nightingale CE, et al. Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesth Analg. 1999;88(1):83–90. doi:10.1213/00000539-199901000-00016
- Myles PS, Myles DB, Galagher W, Chew C, MacDonald N, Dennis A. Minimal clinically important difference for three quality of recovery scales. Anesthesiology. 2016;125(1):39–45. doi:10.1097/ALN.0000000000001158
- Hung KC, Ko CC, Hsu CW, Pang YL, Chen JY, Sun CK. Association of peripheral nerve blocks with patient-reported quality of recovery in female patients receiving breast cancer surgery: a systematic review and meta-analysis of randomized controlled studies. Can J Anaesth. 2022;69(10):1288–1299. doi:10.1007/s12630-022-02295-0
- Yap JY, Bhat M, McMullen W, Ragupathy K. Novel use of laparoscopic-guided TAP block in total laparoscopic hysterectomy. J Obstet Gynaecol. 2018;38(5):736. doi:10.1080/01443615.2018.1444402