Abstract
Introduction
Minimally invasive sacroiliac (SI) joint fusion has become the mainstay treatment for chronic refractory sacroiliac joint dysfunction. Multiple procedures are now available including transfixing procedures with implants placed in the lateral or posterolateral transiliac trajectories, and intra-articular procedures with devices and/or allograft placed via a dorsal approach. To date, the published literature on the lateral approach has been primarily by surgeons. This retrospective chart review aims to evaluate the safety and preliminary effectiveness when the procedure is performed by physicians trained in interventional pain management.
Methods
Retrospective analysis of patients who underwent lateral SI joint fusion using a lateral transiliac approach between December 2022 and September 2023 by a single physician. Data on demographics, perioperative details, complications, and postoperative outcomes were collected and analyzed. The study was reviewed by WCG IRB and received an exemption authorization.
Results
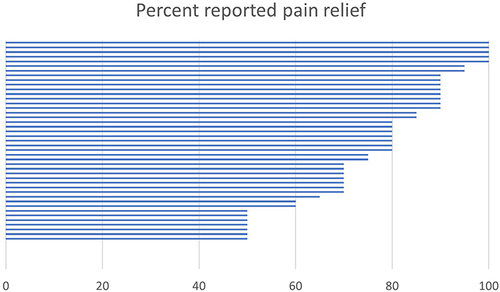
Medical charts were reviewed for the first 49 consecutive cases performed. Mean (SD, range) age was 64 (11, 34–83), BMI was 32.5 (8.4), 59% were female, 35% were smokers, and 82% were on opioids at baseline. Mean (SD) operative time was 40 (11) minutes and all procedures were performed at an ambulatory surgery center under monitored anesthesia care. No device- or procedure-related complications occurred. Mean follow up was 175 days; Mean (SD) baseline reported pain was 9 (1.5) on a 0–10 numerical rating scale. At follow up, 88% of the patients reported ≥50% pain relief. Six patients who reported 0% relief suffer from multiple pain generators and are on long term opioids.
Conclusion
Results of this single center experience support the safety of lateral SI joint fusion using a threaded implant when performed by interventional pain management physicians. However, further prospective studies with larger sample sizes and longer follow-ups are warranted to validate these findings.
Introduction
Sacroiliac joint (SIJ) dysfunction is a recognized source of chronic lower back pain. Over the past decade, minimally invasive SIJ fusion has become the mainstay treatment for chronic refractory SIJ dysfunction. Multiple minimally invasive surgical procedures are now available to fuse the SI joint. These are typically described as 1) transfixing, 2) intra-articular/interpositional and 3) spanning. Transfixing devices may be placed from a lateral, a posterolateral, or a posteromedial trajectory. Transfixing devices cross two bone cortices on one side of the joint, cross the SI joint, and end in the bone on the opposite side of the joint. Intra-articular procedures involve placement of implants, either metallic devices or machined bone allografts, into the SI joint from a posterior trajectory. Spanning implants have structural elements that engage both the ilium and sacrum (thus “spanning”) but do not transfix the joint. The large body of literature, including a recent systematic review and meta-analysis of 2851 patients across 57 studies, supports the safety and effectiveness of SIJF using transfixing or intraarticular implants when performed in accordance with evidence-based guidelines and techniques.Citation1,Citation2
Until recently, SIJ fusion was performed primarily by surgeons using the lateral transfixing procedure. However, treatment of SIJ dysfunction is experiencing rapid growth as new procedures and implants have become available and the scope of other specialties expands. In 2021, the first report of SIJ stabilization using a dorsally placed allograft performed by interventional pain management physicians was published.Citation3 This was quickly followed in 2022 with a publication describing interim results of a prospective trial of the same procedure.Citation4 Long term outcomes have yet to be published.
The number and type of surgical spine procedures performed by interventional pain management (IPM) physicians has grown substantially in recent years.Citation5 IPM physicians now routinely perform surgical procedures to decompress the spinal canal and stabilize vertebral body fractures, many of which involve placement of metal implants. This physician specialty has been quick to adopt the posterior intra-articular procedure for SI joint fusion as the surgical anatomy avoids the soft tissues of the lateral buttock and is thought to be associated with a lower risk and rate of complications, including major bleeding. The risk of vascular injury to the superior gluteal artery (SGA) branches has been raised as a potential concern with the lateral transfixing procedure, but the rhetoric is unsubstantiated as the incidence was reported at 0.039% in a large meta-analysis.Citation1
There is growing interest in the lateral transfixing procedure as there may be clinical, biomechanical, and biologic advantages. The lateral procedure is well established with over ten years of clinical evidence, encompassing multiple international randomized controlled trials, prospective studies, and real world evidence, including 5 year outcomes and robust radiographic evidence of bony fusion.Citation1,Citation6–9 Furthermore, intraoperative imaging is straightforward and implant placement can be verified on x-ray as well as advanced imaging. To our knowledge, there have been no studies of the lateral transfixing procedure published by this specialty. Thus, the purpose of this retrospective chart review is to evaluate the safety and preliminary effectiveness of lateral SIJF performed by physicians trained in interventional pain management.
Methods
This retrospective chart review encompasses the first 49 consecutive cases of minimally invasive lateral transfixing SIJ fusion placing multiple 3D printed threaded titanium implants (iFuse TORQ, SI-BONE, Inc., Santa Clara, CA) by a single pain management physician between December 2022 and September 2023. Patient demographics, perioperative details including blood loss, and postoperative follow-up were extracted from the medical record. Complications within the perioperative period, including infection, neurovascular injury, and hardware-related issues were analyzed. Postoperative adverse events, patient-reported outcomes, and reoperations were also documented. This retrospective chart review study received an IRB exemption from the Western Copernicus Group (WCG). Patient consent was not required for medical record review. The study was conducted according to the Declaration of Helsinki.
Surgical Procedure
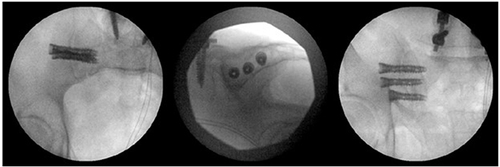
Lateral MIS SIJ fusion was performed under monitored anesthesia care (MAC) using porous 3D printed threaded titanium implants (iFuse TORQ Implant system, SI-BONE, Inc., Santa Clara, CA). The procedure was performed with the patient in a prone position with the hips and chest supported on transverse bolsters. After the patient was positioned, pelvic inlet, outlet, and lateral images were obtained. Skin markings overlying the radiographic landmarks of the alar lines/iliac cortical densities and the mid sacral body were made. After standard prepping and draping of the operative field, the skin, subcutaneous, and deep tissues were infiltrated with Marcaine with epinephrine. An approximately 2.5 cm skin incision was made and a guide pin was passed through the tissue to the lateral ilium under lateral fluoroscopic imaging. The guide pin was advanced with a mallet approximately 2 cm into the ilium. Imaging was switched to the pelvic inlet view to verify proper trajectory. The guide pin was advanced to the SI joint, and placement was verified in the pelvic outlet view before advancing the pin to a depth just lateral to the S1 neuroforamen. The soft tissue dilator was placed over the pin to spread the gluteal fascia and muscle fibers. A depth gauge to determine the implant length was placed over the guide pin and advanced to the lateral ilium. The soft tissue protector was placed over the depth gauge and advanced to the lateral ilium, after which the depth gauge was removed. Throughout the remaining steps of the procedure, care was taken to keep the soft tissue protector docked on the lateral ilium at all times. Remaining in the pelvic outlet view, the implant, attached to the driver, was advanced over the pin and through the soft tissue protector until fully seated. The driver was disengaged from the implant, and was removed along with the soft tissue protector, leaving the guide pin in place. The short barrel of the 15 mm parallel pin guide was placed over the guide pin and utilized to help position the subsequent (second) guide pin. Identical steps were used to place the second and the third implants.
Results
A total of 49 consecutive cases were reviewed. Mean (SD, range) patient age was 64 years (11, 34–83), BMI was 32.5 (8.4), 59% were female, 35% were smokers, and 82% were on opioids at baseline (). Prior spine surgery was not uncommon; 32.7% of the patients had a history of spine surgery. Prior SIJ fixation with allograft on the contralateral side was present in 16% of the patients. One patient presented for lateral SIJ fusion after presenting with recurrent SIJ pain after bilateral SIJ fixation with allograft placed in the dorsal portion of the joint.
Table 1 Demographics
All patients underwent lateral transfixing SI joint fusion under monitored anesthesia care at an ambulatory surgery center (). All but two patients had three implants placed; one patient had two implants and one patient had three threaded implants and one triangular titanium implant. Mean (SD) operative time was 40 (10) minutes and blood loss was minimal (<10 cc) in all cases (). No device or device-placement related complications occurred. After an unremarkable surgical procedure, one patient with a history of atrial fibrillation became tachycardic after approximately 10 minutes in the recovery room. The patient was transferred to a hospital for observation and was discharged the following day without sequelae.
Table 2 Perioperative Characteristics
Mean follow up was 175 days (SD 124, range 30–458 days). Pain scores are recorded at baseline on 0–10 NRS scale (0= no pain, 10= worst pain) and as percentage pain relief at follow up. Mean (SD) baseline reported pain was 9 (1.5) on a 0–10 scale. At follow up, 88% of the patients reported ≥50% pain relief. Individual scores are presented in . Six patients reported 0% relief; all suffer from multiple pain generators and were on long term opioids before undergoing SIJF.
Discussion
The findings of this retrospective chart review suggest that lateral transfixing SIJF using a titanium, porous 3D printed threaded implant is safe and effective when performed by interventional pain physicians with adequate training and experience. Patient outcomes were consistent with other real-world reports of SIJ fusion.Citation1 In our case series with an average of four-month follow up, 86% reported at least 50% pain relief. Six reported no discernable improvement; all suffer from multiple pain generators and were on long term opioids. They reported difficulty discerning their SIJ pain from other sources of low back pain. There were no device or procedure-related adverse events and no cases of excessive bleeding. A single unrelated post-operative event occurred: A 79yo male with a history of atrial fibrillation experienced tachycardia shortly after he was transferred to the recovery room. Out of an abundance of caution, the patient was transferred to the hospital for further observation. He was discharged the following day without sequelae.
Percutaneous placement of metallic implants across the SIJ for treatment of SIJ trauma was popularized in the mid 1990’s.Citation10 Reported complications are primarily related to implant malposition, including violation of the S1 or S2 neuroforamen, and L5 nerve injury above or ventral to the sacral cortex.Citation11 In a large meta-analysis, the rate of malposition was 0.429% for laterally placed implants and 0.2% for posterior interpositional implants.Citation1 Injury to the lateral branches of the superior gluteal artery (SGA) have also been reported and sensationalized in the interventional community despite a 0.039% rate of bleeding requiring surgery.Citation1 While this did not occur in the current case series, it is a risk and thus physicians should be informed on the topic. Injury to the SGA vascular tree is not common; case reports utilizing iliosacral screws to repair unstable pelvic ring injuries in the setting of trauma have reported injury to the SGACitation12,Citation13 and post-operative development of pseudoaneurysm of the SGA.Citation14,Citation15 Similar iatrogenic vascular injury has been reported during bone marrow aspiration.Citation16,Citation17 CollingeCitation18 published a cadaveric study that described an 18% incidence of injury to the lateral SGA bundle. The applicability of these findings in a patient population is questionable. The study was performed in embalmed cadavers; the fixed soft tissues are less likely to be mobilized as would occur in an actual surgical procedure. Moreover, the study reported on the SGA bundle as opposed to only arterial vessel injuries.
EbraheimCitation19 and more recently MahatoCitation20 reported cadaveric studies relating the vascular anatomy of the SGA bundle to the osseous ilium and the underlying iliac articular surface of the SI joint. Both the superficial branch of the SGA and the superior division of the deep branch of the SGA are frequently located in the zone of implant placement at both the S1 and S2 levels. Several authors have utilized CTA (CT angiography) and virtual placement of implants to model potential vascular injury rates. Consistent with the cadaveric studies, a significant number of patients had either superior deep branch or superficial branch vessels in the implant target zones at the levels of S1,Citation21 S2,Citation22 and S3.Citation23 Injuries to these branches would typically result in modest hemorrhage during the procedure, but would rarely be life threatening. Rather, these injuries may present as a perioperative hematoma, which have been described in rigorously controlled prospective clinical studies. On rare occasions, in surgeries for treating pelvic trauma using iliosacral screws, injury to vessels in the pelvis/abdomen have been reported. These injuries, while exceedingly rare, could be life threatening. Examination of the Manufacturer and User Facility Device Experience (MAUDE) database for SIJ fusion revealed 3 deaths. Upon investigation, two of these deaths were a result of intra-abdominal injury from pin advancement and one was unrelated to the implant or SI joint fusion procedure. There are currently no reports of deaths due to gluteal artery injury. However, major bleeding during a lateral SIJ fusion procedure has been reported.Citation24 A good understanding of the 3D osseous anatomy and appropriate imaging are critical to minimize these types of injuries.
Sacral dysmorphism has been implicated as potential anatomic variant that may increase the risk of vascular injury.Citation24 However, other authors question the relationship of dysmorphic anatomy to increased vascular risk.Citation23 Few clinical studies have reported “real world” data on the incidence of lateral vascular injury secondary to SI joint fixation and those reported rates are low 0.6–1.2%.Citation13,Citation25
Proper surgical technique and soft tissue protective tools and sleeves for the surgical instruments utilized during the procedure have been espoused as critical for safely performing iliosacral fixation since adoption of this procedure.Citation10 Thoughtful surgical approaches and surgical techniques may minimize/prevent complications.Citation12,Citation13,Citation18,Citation19,Citation26 This attitude and perspective aligns well with the basic principles of minimally invasive procedures, regardless of specialty training. Lateral SIJ fusion as performed herein utilized instruments specifically designed to protect the soft tissue, including a soft tissue dilator used to spread the gluteus fascia and the underlying muscle fibers, a depth gage/obturator, and a soft tissue protector. In addition, care was utilized to place the guide pin through the muscle in a single pass and to withdraw, reposition, and replace the guide pin if a different position was desired. Lateral transfixing SIJF has mostly been performed by orthopedic or neurosurgeons. With the expansion in scope of practice and procedures available to interventional pain physicians, many have begun to adopt the lateral procedure despite a general negative rhetoric. The procedure is straightforward with clear imaging landmarks and the ability to quickly verify implant position. While the accuracy of implant placement has not yet been reported with allograft products, either poor initial placement or implant subsidence has been reported when revised with metal devices.Citation27 Compared with a posterolateral approach using metallic implants or a dorsal approach using bone products, laterally placed implants may result in a biomechanical advantage. Implants placed laterally transfix the joint and anchor into areas of higher density bone (ilium and sacral body).Citation28 The depth and breadth of the vast clinical literature supporting the lateral procedure includes two RCTsCitation6,Citation29,Citation30 multiple multicenter prospective studies,Citation7,Citation8,Citation31–33 as well as long term (five year) clinical and radiographic results.Citation34 This wealth of literature supports the safety and effectiveness of this procedure. The results of our early case series are reflective of the currently published literature.
Patients presenting to a pain management clinic may suffer with multiple pain generators. Patients with multiple pain generators should be counseled that the overall impact of SIJ fusion may be limited in this situation. Limitations of the current case series must be acknowledged, such as the retrospective design, limited follow-up, and potential selection bias.
Conclusion
This single-center retrospective review highlights the safety and effectiveness profile of SIJ fusion in our patient cohort. No perioperative complications occurred, affirming the procedure’s safety when performed by interventional physicians with training. Further prospective studies with larger sample sizes and extended follow-up are warranted to corroborate these findings.
Disclosure
Dr Michael W Jung is a consultant for SI-Bone. The author reports no other conflicts of interest in this work.
References
- Whang PG, Patel V, Duhon B, et al. Minimally Invasive SI joint fusion procedures for chronic SI joint pain: systematic review and meta-analysis of safety and efficacy. Int J Spine Surg. 2023:8543. doi:10.14444/8543
- Lorio MP. editor’s introduction: update on current sacroiliac joint fusion procedures: implications for appropriate current procedural terminology medical coding. Int J Spine Surg. 2020;14(6):853–859. doi:10.14444/7136
- Sayed D, Balter K, Pyles S, Lam CM. A multicenter retrospective analysis of the long-term efficacy and safety of a novel posterior sacroiliac fusion device. J Pain Res. 2021;14:3251–3258. doi:10.2147/JPR.S326827
- Calodney AK, Azeem N, Buchanan P, et al. Six month interim outcomes from SECURE: a single arm, multicenter, prospective, clinical study on a novel minimally invasive posterior sacroiliac fusion device. Expert Rev Med Devices. 2022;19:451–461. doi:10.1080/17434440.2022.2090244
- Naidu RK, Chaturvedi R, Engle AM, et al. Interventional spine and pain procedure credentialing: guidelines from the American society of pain & neuroscience. J Pain Res. 2021;14:2777–2791. doi:10.2147/JPR.S309705
- Polly DW. Minimally invasive sacroiliac joint fusion vs. conservative management for chronic sacroiliac joint pain. J Spine Surg Hong Kong. 2019;5(3):381–383. doi:10.21037/jss.2019.06.10
- Duhon BS, Bitan F, Lockstadt H, Kovalsky D, Cher D, Hillen T. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int J Spine Surg. 2016;10. doi:10.14444/3013
- Patel V, Kovalsky D, Meyer SC, et al. Minimally invasive lateral transiliac sacroiliac joint fusion using 3D-printed triangular titanium implants. Med Devices Evidence Res. 2019;12:203–214. doi:10.2147/MDER.S205812
- Graham Smith A, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013;7(1):14. doi:10.1186/1750-1164-7-14
- Routt MLC, Simonian PT, Inaba J. Iliosacral screw fixation of the disrupted sacroiliac joint. Tech Orthop. 1995;9(4):300–314. doi:10.1097/00013611-199400940-00010
- Routt MLC, Simonian PT, Inaba J. Iliosacral screw complications. Oper Tech Orthop. 1997;7(7):206–220. doi:10.1016/S1048-6666(97)80060-2
- Altman DT, Jones CB, Routt M. Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999;13(3):220–227. doi:10.1097/00005131-199903000-00011
- Marmor M, Lynch T, Matityahu A. Superior gluteal artery injury during iliosacral screw placement due to aberrant anatomy. Orthopedics. 2010;33(2):117–120. doi:10.3928/01477447-20100104-26
- Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma. 1997;43(1):146–149. doi:10.1097/00005373-199707000-00037
- Maled I, Velez R, Lopez R, Batalla L, Caja VL. Pseudoaneurysm of the superior gluteal artery during iliosacral screw fixation. Acta Orthop Belg. 2007;73(4):544–547.
- Bain BJ. Morbidity associated with bone marrow aspiration and trephine biopsy - a review of UK data for 2004. Haematologica. 2006;91(9):1293–1294.
- Yap WT, Jeffrey RB. Sonographic diagnosis of a superior gluteal artery arteriovenous fistula and pseudoaneurysm after bone marrow biopsy. J Ultrasound Med. 2016;35(5):1104–1106. doi:10.7863/ultra.15.08048
- Collinge C, Coons D, Aschenbrenner J. Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: an anatomical cadaver study. J Orthop Trauma. 2005;19(2):96–101. doi:10.1097/00005131-200502000-00005
- Ebraheim NA, Lu J, Yang H, Heck BE, Yeasting RA. Anatomic considerations of the second sacral vertebra and dorsal screw placement. Surg Radiol Anat SRA. 1997;19(6):353–357. doi:10.1007/BF01628500
- Mahato NK. Topographic localization of the sacroiliac joint and superior gluteal artery branches on the posterolateral ilium. Clin Anat N Y N. 2023;36:971–976. doi:10.1002/ca.24005
- Zhao P, Wang X, Chen X, Guan J, Wu M. Preoperative CT simulation of iliosacral screws for treating unstable posterior pelvic ring injury. BMC Musculoskelet Disord. 2022;23(1):220. doi:10.1186/s12891-022-05155-6
- Zhao Y, You L, Lian W, et al. Anatomical relation between S1 sacroiliac screws’ entrance points and superior gluteal artery. J Orthop Surg. 2018;13(1):15. doi:10.1186/s13018-018-0713-5
- Eastman JG, Kuse QA, Routt MLC, Shelton TJ, Adams MR. Superior gluteal artery injury risk from third sacral segment transsacral screw insertion. Eur J Orthop Surg Traumatol Orthop Traumatol. 2021. doi:10.1007/s00590-021-03073-2
- Maxwell G, Lyon KA, Bhenderu LS, Schuchart G, Desai R. Sacral dysmorphism increases the risk of superior gluteal artery injury in percutaneous sacroiliac joint fusion: case report and literature review. Cureus. 2021;13(11):e19532. doi:10.7759/cureus.19532
- Rysavý M, Pavelka T, Khayarin M, Dzupa V. Iliosacral screw fixation of the unstable pelvic ring injuries. Acta Chir Orthop Traumatol Cech. 2010;77(3):209–214. doi:10.55095/achot2010/042
- Maslow J, Collinge C. Risks to the superior gluteal neurovascular bundle during iliosacral and transsacral screw fixation: a computed tomogram arteriography (CTA) Study. J Orthop Trauma. 2017;31:640–643. doi:10.1097/BOT.0000000000000996
- Kranenburg A, Garcia-Diaz G, Cook JH, et al. Revision of failed sacroiliac joint posterior interpositional structural allograft stabilization with lateral porous titanium implants: a multicenter case series. Med Devices Auckl NZ. 2022;15:229–239. doi:10.2147/MDER.S369808
- Payne C, Jaffee S, Swink I, et al. Comparative analysis of the lateral and posterolateral trajectories for fixation of the sacroiliac joint-a cadaveric study. J Orthop Surg. 2020;15(1):489. doi:10.1186/s13018-020-02013-w
- Dengler J, Kools D, Pflugmacher R, et al. 1-year results of a randomized controlled trial of conservative management vs. Minimally invasive surgical treatment for sacroiliac joint pain. Pain Physician. 2017;20:537–550. doi:10.36076/ppj.20.5.537
- Dengler J, Kools D, Pflugmacher R, et al. Randomized trial of sacroiliac joint arthrodesis compared with conservative management for chronic low back pain attributed to the sacroiliac joint. J Bone Joint Surg Am. 2019;101(5):400–411. doi:10.2106/JBJS.18.00022
- Duhon BS, Cher DJ, Wine KD, Lockstadt H, Kovalsky D, Soo CL. Safety and 6-month effectiveness of minimally invasive sacroiliac joint fusion: a prospective study. Med Devices Evidence Res. 2013;6:219–229. doi:10.2147/MDER.S55197
- Rappoport LH, Helsper K, Shirk T. Minimally invasive sacroiliac joint fusion using a novel hydroxyapatite-coated screw: final 2-year clinical and radiographic results. J Spine Surg. 2021;7(2):155–161. doi:10.21037/jss-20-627
- Cross WW, Delbridge A, Hales D, Fielding LC. Minimally invasive sacroiliac joint fusion: 2-year radiographic and clinical outcomes with a principles-based SIJ fusion system. Open Orthop J. 2018;12(1):7–16. doi:10.2174/1874325001812010007
- Whang PG, Darr E, Meyer SC, et al. Long-term prospective clinical and radiographic outcomes after minimally invasive lateral transiliac sacroiliac joint fusion using triangular titanium implants. Med Devices Auckl NZ. 2019;12:411–422. doi:10.2147/MDER.S219862