Abstract
Objective
To investigate the application effect of tilt-angle low-dose ComputedTomography (CT) scanning guidance technology in the plasma radiofrequency treatment of lumbar 5-sacrum 1 (L5-S1) intervertebral disc herniation.
Methods
A total of 43 patients with L5-S1 disc herniation were included in this study and categorized into vertical-angle-guided CT (Group A, n = 21) and tilt-angle-guided CT (Group B, n = 22) groups. Percutaneous plasma L5-S1 disc radiofrequency treatment was administered. The total number of punctures and scans, operation times, and Numerical Rating Scale (NRS) pain scores (preprocedure and 3 and 30 days postprocedure) were documented.
Results
Compared with Group A, punctures and scans were fewer in Group B, and the differences were statistically significant (P = 0.0001). Moreover, the CT scan-guided total surgery time was significantly shorter in Group B than in Group A (P = 0.0001). In addition, the NRS score exhibited a statistically significant difference among preprocedure (T0), 3 day postprocedure (T1), and 30 days (T2) in Groups A (P < 0.05). The NRS score exhibited a statistically significant difference between T0 and T1 and between T0 and T2 in Group B (P < 0.05), but not between T1 and T2 in Group B (P = 0.084). At three time points (T0, T1, T2), there was no statistically significant difference between the two groups (P > 0.05).
Conclusion
The tilt-angle low-dose CT scanning technique for L5-S1 disc herniation offers the advantages of high efficiency, low damage, and low radiation, and its clinical application is recommended.
Plain Language Summary
CT-guided plasma surgery for intervertebral discs has gradually shown its importance in clinical practice. We found that the protrusion of the intervertebral disc in the lumbar 5/sacral 1 region often leads to difficulty in puncture due to its anatomical position. By adjusting the tilt angle of the CT, we increase the success rate of puncture and significantly reduce the radiation exposure to patients. The tilt-angle low-dose CT scanning technique for L5-S1 disc herniation offers the advantages of high efficiency, low damage, and low radiation. It can avoid surgical failures caused by puncture difficulties and also reduce patient exposure to radiation, strengthen awareness of patient protection during treatment.
Introduction
Chronic low back pain is a major social problem with a high economic burden and healthcare costs worldwide. Various techniques have been used to treat discogenic pain with or without lumbar disc herniation. The first percutaneous disc biopsy was performed in the 1950s. Percutaneous endoscopic techniques to access the disc were developed in the 1970s.Citation1 As this technology continues to progress, percutaneous discectomy, decompression, and fusion are rapidly replacing conventional open surgery. CT-guided percutaneous plasma discectomy using the foraminal approach is a minimally invasive procedure in which the disk is accessed through a safe triangle to ablate and thermocondensed disc tissue, thereby achieving disc decompression and alleviating the symptoms.Citation2,Citation3 Compared with conventional surgical techniques, this method offers the advantages of less damage, reduced operation time, faster recovery, and fewer complications; hence, it is used widely in clinical practice. However, in patients with lumbar 5-sacrum 1 (L5-S1) lumbar disc herniation, especially with high iliac crest, it is difficult to reach the puncture hernia target even with CT guidance, and they need to be transferred to open surgery. In this study, tilt-angle and low-dose CT scan guidance were applied for the plasma radiofrequency treatment of L5-S1 disc herniation with successful results. Compared to conventional vertical-angle CT scans, it increases the success rate of the target puncture and reduces the operation time as well as the amount of radiation exposure to the patient.
Materials and Methods
Patients
This study was approved by the Medical Ethics Committee of the Affiliated Hospital of Jiaxing University (2023-LY-540). A total of 46 patients with L5-S1 intervertebral disc herniation, including 19 men and 24 women, aged 31–75 years were initially enrolled at the Pain Department of the Affiliated Hospital of Jiaxing University from May 2023 to August 2023. They were categorized into two groups according to the type of CT scan performed. All patients read and signed the informed consent form, and their names were not disclosed in the study data. Percutaneous plasma L5-S1 disc radiofrequency treatment was performed by the same doctor for all patients.
Inclusion and Exclusion Criteria
Inclusion Criteria
1. Imaging confirmed L5-S1 disc bulging or herniation, and clinical symptoms met the diagnosis of L5-S1 lumbar discogenic pain or herniation; 2. Conservative treatment for >3 months was not effective; Numerical Rating Scale (NRS) score of ≥5, and symptoms of low-back pain or S1 nerve root stimulation; 3. Patients provided informed consent and were willing to receive surgical treatment.
Exclusion Criteria
1. Patients in poor general condition and cannot tolerate surgery; 2. Patients with skin infection or tumor at the treatment site; 3. Those with severe cardiopulmonary insufficiency or other major systemic diseases; 4. Those with lumbar instability, severe spinal stenosis, cauda equina syndrome, or other spinal disorders; 5. Those with incomplete medical records or follow-up data.
Surgical Procedure
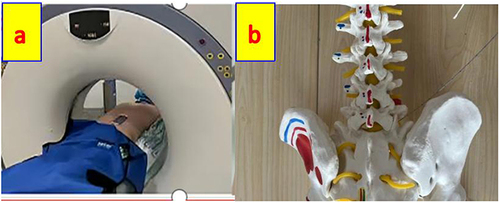
The patient was laid in a prone position on the CT imaging bed, with a pillow under the abdomen. Continuous vital sign monitoring and nasal oxygen inhalation were provided during the entire operation (). Only the surgical site was exposed, and the rest of the area was covered with lead clothing to the best possible extent. The positioning grid was fixed on the surgical area with adhesive tape. We are trying to obtain the ideal puncture path. The puncture needle will begin with the skin, cross the iliac crest, and reach the L5-S1 intervertebral disc level ().
Figure 1 The patient was laid in the prone position on the CT imaging bed, with a pillow under the abdomen, the positioning grid was fixed on the surgical area with adhesive tape as (a) CT (Siemens Joy single row, parameter 81 mas/80 kV) vertical scanning was used to locate the plane of the L5-S1 intervertebral space. The plasma needle attempt to reach the disc plane require tilt angle puncture as shown in (b).
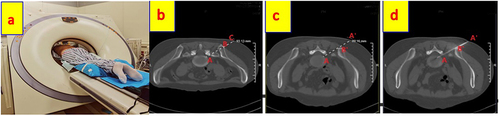
The surgical puncture process was as follows: Group A: CT (Siemens Joy single row, parameter 81 mas/80 kV) vertical scanning was used to locate the plane of the L5-S1 intervertebral space. Based on the CT images, we confirmed the target point A at the plane of L5-S1 and the cross-point B on the iliac crest and the cross-point C on the skin in the same plane (). Considering the obstruction by the iliac crest in the same plane, we lifted point C to reach the truly ideal puncture point A’ and cross B’ point at iliac crest margin ( and ). Routine disinfection napkin was applied, layer-by-layer infiltration anesthesia was administered, and the plasma puncture probe through A’ point slowly reached the A guided by vertical CT scans (). Then, plasma radiofrequency ablation surgery was performed: the needle core was pulled out, the plasma blade was inserted, and the plasma generator was connected (SPINENDOS GERMAN SD-200-SDJX0342). One gear was used, the ablation pedal was gently tapped, the pedal was quickly released, and the patient was inquired about lower-limb shock. In case of a different sensation, the blade position was adjusted to test again. During the ablation sensation, the ablation treatment was started and the blade was gradually extended to 1 cm to expand the ablation range for 20s. Gradually increase to the 2 gear and 3 gear for 20 seconds, respectively. Then, the puncture point was compressed after the needle was pulled out. After observation for 20 minutes, the patient was wheeled back to the ward. Group B: First, vertical CT scanning was used to locate the plane of the L5-S1 intervertebral space and to confirm A, B, and C points as Group A (). Second, the CT tilted angle was applied to create the puncture path without obstruction ( and ), and the determination of the angle was based on experience, to approximately 20–30 degrees. Next, the puncture point A’ was located on the skin, and the plasma puncture probe through the A’ point slowly reached the A under guidance by tilted CT scans (). Then, the same plasma radiofrequency ablation surgery was then used for Group A.
Figure 2 Based on the vertical CT scan images, we confirm the target point A, cross point B on the iliac crest and cross point C on the skin at the plane of L5/S1 (a). Because there will be obstruction by the iliac crest in the same plane, we will lift point C to reach the truly ideal puncture point A’ through cross point B’ on the iliac crest (b and c). The plasma puncture probe through A’ point slowly reached the A guided by different vertical CT scans plane (d–f).
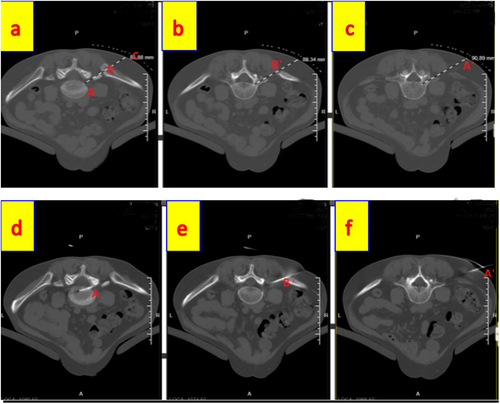
Figure 3 The vertical CT scanning was used to locate the plane of the L5-S1 intervertebral space and confirm A, B, C points (b). The CT tilted angle to make the puncture path without obstruction (a and c), Find the puncture point A’ on the skin, and the plasma puncture probe through A’ point slowly reached the A guided by tilt CT scans (d).
Observation Indexes
Numbers of Puncture: the first puncture is recorded as 1, then 1 point each per puncture.
Numbers of Scans: count the numbers from the first percutaneous puncture scan to the L5-S1 disc protrusion target puncture scans.
Puncture times: count the total times since starting the local anesthesia until the tip reaches the L5-S1 disc target and the CT scan is completed.
NRS score: collection time—preprocedure and then 3-day postprocedure and 30-day postprocedure. Score 0 = no pain, ≤3 = mild pain deemed tolerable by the patients, 4–6 = moderate pain that affected sleep, but remained tolerable, 7–10 = gradually increasing intense pain that was intolerable, and 10 = extreme intolerable pain.
Statistical Analysis
SPSS 25.0 (IBM, Chicago, USA) was used to analyze the data. The Shapiro–Wilk test was used to determine whether the measurement data conformed to a normal distribution, and the results were expressed as mean ± standard deviation (SD). On the contrary, nonnormally distributed data were expressed as the median and interquartile range. The Wilcoxon test was used to analyze the nonnormally distributed data. A paired samples t-test was used to compare the differences among the measurement data, and a chi-square test was used to compare the differences among the counting data. P < 0.05 was considered to be a statistically significant difference.
Results
Clinical Characteristics of the Patients
In this study, three patients were lost to follow-up, and a total of 43 patients at the Pain Department of the Affiliated Hospital of Jiaxing University were enrolled. L5-S1 disc bulging or herniation was confirmed in all patients, and the clinical signs met the diagnosis of L5-S1 lumbar discogenic pain or herniation. The patients were categorized into two groups (Group A = 21 patients, Group B = 22 patients) according to the method of the scan (vertical/tilt). There were no statistically significant differences in age, sex, disease duration, or body weight between the two groups (P ≥ 0.05) ().
Table 1 Compare with the General Information of the Two Groups
Puncture and Scan Numbers and Surgery Time
The first puncture was recorded as one, and one number was added for each additional puncture. The number of scans from the first percutaneous puncture scan to the L5-S1 disc protrusion target puncture scan was counted. The total number of times from the start of local anesthesia until the time when the tip reached the L5-S1 disc target point was recorded and the CT scan was completed.
Compared with Group A, puncture and scan numbers were fewer in Group B, and there were statistically significant differences (P = 0.0001). Moreover, the scan-guided total surgery time was significantly shorter in Group B than in Group A (P = 0.0001, ).
Table 2 Comparison of Observational Indicators Between the Two Groups of Patients (Puncture and Scan Numbers and Surgery Time)
Effectiveness Analysis of the NRS Score
Data on the three-time points of pain scores (NRS), namely, preprocedure and postprocedure at 3 days and 30 days, were collected. The NRS score exhibited a statistically significant difference between preprocedure (T0), 3 day postprocedure (T1), and 30 days (T2) in Groups A (; P < 0.05). The NRS score exhibited a statistically significant difference between T0 and T1, T0, and T2 in Group B (; P < 0.05), but not between T1 and T2 in Group B (; P = 0.084). At three time points (T0, T1, T2), there was no statistically significant difference between the two groups.(; P > 0.05).
Table 3 Comparison of Preoperative and Postoperative Various Time Points NRS Scores in Group A {score, M (IQR)}
Table 4 Comparison of Preoperative and Postoperative Various Time Points NRS Scores in Group B{score, M (IQR)}
Table 5 Comparison of NRS Scores Before and After Treatment Between the Two Groups
Discussion
CT-guided technology is crucial for the advancement of interventional therapy for disc herniation. However, for the L5-S1 segment, puncture localization is clinically difficult owing to its unique anatomical structure, large tilted intervertebral space, and the presence of bony obstructions in the puncture path. In the vertical-plane approach used presently in clinical practice, it is difficult for the surgeon to proceed with the puncture, and the depth and angle of the puncture have to be constantly adjusted during the procedure. Jun-Song Yang et alCitation4 used biplane oblique fluoroscopy under the C-arm to demonstrate the safety triangle. This study suggested that multiangle scanning can provide superior multidirectional observation information during operation and eliminate the blindness and uncertainty of single-plane surgery. In our study, by preoperatively assessing the relationship between the iliac bone and the L5-S1 intervertebral disc, the CT angle was rotated to avoid the high iliac crest. Furthermore, the scan showed the entry point to the L5-S1 intervertebral disc, and the angle was tilted toward the cephalad end so that the CT plane perfectly revealed the puncture pathway from the skin to the L5-S1 intervertebral disc (). During the puncture process, the puncture needle only needs to be parallel to the tilt angle of the CT and along the puncture pathway. The results signified that the number of punctures, the number of scans, and procedure time were immensely reduced by puncture guidance under tilt-angle CT scanning compared with vertical-plane scanning.
Low-temperature plasma is a treatment that has been advanced on the basis of radiofrequency technology. When the controlled energy of radiofrequency is used to form plasma near the cutter head, the nucleus pulposus has a good gasification and coagulation effect on the tissue. It can cause decompression within the intervertebral disc and can even directly reach the target point, reducing disc herniation. Owing to its low-temperature environment (42°C), which can reduce the damage to the surrounding tissues.Citation5 Furthermore, CT guidance can show the changes in the disc, aid in determining the time of the treatment, and confirm the treatment effect. In addition, some studies have observed that certain chemical transmitters in the intervertebral disc, such as nitric oxide, IL-6, prostaglandin E2, glycoprotein, β-protein, and TNF-α, play a key role in triggering neuropathic pain in the intervertebral disc.Citation6,Citation7 These proteins may take part in the immune regulation of the body and in the onset and development of chemical nerve root inflammation in lumbar disc herniation.Citation5 Plasma radiofrequency ablation within the disc may inhibit the release of chemical mediators within the disc, thereby inhibiting the development of neuropathic pain.
According to the findings of this investigation, L5-S1 puncture guided by tilt-angle CT scanning localization reduces both the number of punctures and the time taken to reach the target, which is essential for ensuring the success of the procedure. In addition, the amount of radiation exposure to the patient is reduced.Citation8 Our treatments were performed under CT, which is more precise than the C-arm; however, we must realize that there is a positive correlation between the radiation dose and the risk of disease.Citation8 In our treatment, the lowest radiation parameters were applied, as follows: tube sphere current 81 mA, tube voltage 80 kV, and CTDlvol 1.27 mGy per scan (Siemens Joy single-row helical CT, ( and ). Although it is in accordance with the annual limit of 5 mSv, it is recommended that no more than 5 scans be performed.Citation9,Citation10 This limitation enhances the requirement for the physician’s comprehension of the three-dimensional space and the optimization of the guiding technique. In this study, we were able to significantly reduce the scanning time by performing a tilt-angle scan. After CT scanning, we were able to significantly reduce the number of scans, which is important to curtail radiation exposure.
Nonetheless, there are some limitations in this study, the first is small simple sizes, we should apply this approach to clinical validation of large samples in future work. The second is a short period of follow-up, and further follow-up of the patient will be conducted in the future study. Furthermore, the tilt angle of CT was based on usual clinical experience, which can change according to the height of the iliac crest. In addition, for patients with a high iliac crest, when the highest point of the crest is located above the horizontal line of the lower edge of the L4 pedicle, the maximum CT rotation angle (−30°) is only effective in avoiding the obstruction of the high iliac crest and transverse process. Although it can facilitate intradiscal decompression of L5-S1, it cannot ensure decompression at the protruding target point during plasma radiofrequency ablation of the puncture path.
Conclusion
Tilt-angle low-dose CT scanning technique for L5-S1 disc herniation has the advantages of high efficiency, low damage, and low radiation, and its clinical application is recommended.
Ethics Approval
This study got ethical approval (2023-LY-540) from the Affiliated Hospital of Jiaxing University, and complies with the Declaration of Helsinki.
Informed Consent
All patients read and signed the informed consent before the operation, with the patient’s name withheld in this study.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
Leichao Gu and Wei Liu are co-first authors for this study. This work was supported by the Affiliated Hospital of Jiaxing University.
Additional information
Funding
References
- Choy DS. Percutaneous laser disc decompression (PLDD): 352 cases with an 8 1/2-year follow-up. J Clin Laser Med Surg. 1995;13(1):17–21. PMID: 10150569. doi:10.1089/clm.1995.13.17
- Du J, Sun Q, Wang R, et al. Observation on the efficacy of low-temperature plasma-targeted radiofrequency ablation combined with collagenase and ozone in the treatment of lumbar intervertebral disc herniation[J]. Chin J Pain Med. 2020;26(7):553–557.
- Liu J, Zheng B, Yang Y, et al. Plasma radiofrequency myeloplasty combined with ozone nucleus pulposus ablation for the treatment of discogenic pain. Tianjin Med. 2012;40(7):742–743.
- Jun-Song Y, Kai-Xuan L, Praveen K, et al. Can the Novel Lumbo-Iliac Triangle Technique Based on Biplane Oblique Fluoroscopy Facilitate Can the Novel Lumbo-Iliac Triangle Technique Based on Biplane Oblique Fluoroscopy Facilitate Transforaminal Percutaneous Endoscopic Lumbar Discectomy for Patients with L5-S1 Disc Herniation Combined with High Iliac Crest? Study 100 Patient Pain Phys. 2020;23:305–313.
- Zhoa L, Wang L, Zhu B. Analysis of the efficacy of computed tomography-guided targeted low-temperature plasma combined with collagenase in the treatment of lumbar intervertebral disc herniation. Int J Anesthesiol Resuscit. 2018;39(9):836–840.
- Xia WJ. Clinical study on the mechanism of lumbar discogenic pain. Chin Foreig Med Treat. 2017;36(2):13–15,41.
- Zhang M, Guan B, Fan H, et al. Serum proteomic analysis before and after massage treatment for lumbar disc herniation. Chin Tissue Eng Res. 2017;21(4):569–573.
- Lei ZQ, Yu JM, Ping HAN, et al. Comparative study of lumbar spine CT scanning methods and radiation dose. Chin J Radiat Med Protect. 2009;29(3):328–329.
- Wang Q, Zhao X, Song J, et al. Body modeling study of the effect of automatic tube current modulation technique on abdominal CT image quality and radiation dose[J]. Chin J Radiol. 2013;47(7):648–653.
- Wang X-H, Zhang W-M, Sun J-Z, et al. Analysis of annual cumulative CT effective dose in hospitalized patients[J]. Chin J Radiol. 2014;48(6):503–504.
