Abstract
In obese persons, general and specific musculoskeletal pain is common. Emerging evidence suggests that obesity modulates pain via several mechanisms such as mechanical loading, inflammation, and psychological status. Pain in obesity contributes to deterioration of physical ability, health-related quality of life, and functional dependence. We present the accumulating evidence showing the interrelationships of mechanical stress, inflammation, and psychological characteristics on pain. While acute exercise may transiently exacerbate pain symptoms, regular participation in exercise can lower pain severity or prevalence. Aerobic exercise, resistance exercise, or multimodal exercise programs (combination of the two types) can reduce joint pain in young and older obese adults in the range of 14%–71.4% depending on the study design and intervention used. While published attrition rates with regular exercise are high (∼50%), adherence to exercise may be enhanced with modification to exercise including the accumulation of several exercise bouts rather than one long session, reducing joint range of motion, and replacing impact with nonimpact activity. This field would benefit from rigorous comparative efficacy studies of exercise intensity, frequency, and mode on specific and general musculoskeletal pain in young and older obese persons.
Introduction
Obesity negatively impacts the musculoskeletal system.Citation1 Excessive weight increases mechanical stress to the joints and tissues of the body,Citation2 and induces physical limitations and bodily pain. Self-reported bodily pain symptoms increase with progressively higher body mass index (BMI) values.Citation3 The confluence of pain and weight-related physical discomfort exacerbates the decline in physical function. This is a serious issue because chronic pain mediates obesity-induced impairment and the eventual decline of fitness and health-related quality of life.Citation4–Citation6
Obesity rates in the US are 35% for adults and 17% for youth, and only 21% of Americans meet the recommended levels of physical activity for health.Citation7 This is a serious issue because the loss of muscle strength due to inactivity contributes to worsening joint pain in adults.Citation8 Moreover, adults, especially women, with high fat mass-to-muscle ratios have widespread musculoskeletal painCitation9 and have higher rates of physical inactivity.Citation10 Often, obese adults suffer from negative psychological outlook, which perpetuates sedentary behavior. For obese children, pain reduces mobility, participation in exercise, and overall happiness.Citation6 Children with BMI values exceeding the 95th percentile reported double the prevalence of pain than nonobese counterparts (44.8% vs 19.1%), and the pain is related to skeletal deformity and musculoskeletal dysfunction.Citation11 Emerging evidence suggests that obesity mediates pain and the psychological state through a mechanism of inflammation.Citation12 This focused review describes this proposed relationship between obesity, musculoskeletal pain, inflammation, and psychological status. Exercise solutions that reduce chronic pain are presented.
Effects of pain on physical activity in obesity
Obesity is associated with comorbidities and discomforts that can negatively affect psychological well-being and perceptions about staying physically active.Citation13,Citation14 These include heart disease and heart failure, fibromyalgia, asthma, gout, diabetes, anxiety, and depression. Increased muscle effort can trigger physical discomforts such as dyspnea, chest pain, muscle fatigue, and psychological discomforts such as stigma, fear of falling, and low self-efficacy.Citation14–Citation16 This is problematic for practitioners and those affected because physical activity and exercise are main tenets of weight management programs and long-term health.Citation13
Both obese children and adults experience pain symptoms most frequently in the axial and load-bearing segments of the body such as the neck, low back,Citation10,Citation17,Citation18 and lower limb.Citation6,Citation19,Citation20 Chronic joint pain can also occur in the non-weight-bearing joints of the upper body such as the shoulder and hand,Citation10,Citation19 and in the facets of the lumbar spine.Citation21 Obese persons suffer from multisite pain,Citation22 and morbidly obese are over twice as likely to report consistent, severe pain symptoms than normal weight individuals.Citation23 Longitudinal evidence shows that high BMI precedes and independently predicts foot joint painCitation20 and knee pain.Citation24
Chronic musculoskeletal pain hinders participation in regular exercise programsCitation25,Citation26 and performance of normal functional tasks.Citation27,Citation28 Among obese disabled women, 63.6% reported that the major personal barrier to increasing physical activity levels is pain.Citation29 Population-based cohorts show that irrespective of age, race, and sex, obese people with joint pain are 44% more likely to be physically inactive.Citation30 Pain may exacerbate the obesity-related barriers to participation in exercise (stigma, embarrassment, lack of motivation, physical discomfort).Citation31 For example, excessive weight compresses axial structures and load-bearing joints and misaligns the bone-to-bone interfaces in joints, especially in the knee and spine.Citation2,Citation32 Gross motor tasks that involve moving significant knee flexion and extension to move the body vertically (eg, stair ascent and descent, timed-up-and-go activities, chair rise, getting in and out of a car, rising from a supine position on the floor, picking up objects from the floor) are especially difficult for the obese individual.Citation27,Citation33,Citation34 Even more refined movements such as a one-legged stance or cutting toenails are more challenging with rising BMI values.Citation27 Some of these activities require static positions such as standing, whereas others involve transient loading such as stairs or walking. When pain is present, the discomfort of both single- and dual-limb tasks in obesity can reinforce negative views about being active. Hence, a challenge for practitioners is how to motivate obese patients to overcome the barriers and work through exercise discomforts sufficiently to elicit physical functional improvements.
With activities of daily living, there are compensatory responses to musculoskeletal pain that include less movement excursion (eg, short steps and less joint motion),Citation35 slower velocity of movement and initiation of gait,Citation36,Citation37 co-contraction of muscles, and asymmetric loading.Citation35,Citation36,Citation38 Slower execution of movement is a method of minimizing peak forces and impulse of force loading. In people with unilateral or bilateral joint pain of the knee,Citation39 motion is achieved with asymmetric joint flexion angles at the knee, hip adduction moments and internal rotation, and toe out angles. Pain causes individuals to change movement patterns during daily tasks to offload the painful limb and overload the non-affected limb. People with chronic hip pain who perform actions like sit-to-stand reduce the impact force by 18% on the painful limb and increase the moments of the knee of the non-affected limb by 19%.Citation40 In addition to joint loading, a functional compensation to pain is alteration of the flexion–extension activation of muscles surrounding a painful joint. Specifically, maximum flexion moments are reduced during mid-stance phase of walking, perhaps to offset the load-induced pain.Citation38 Deterioration of normal gait and mobility disability may be affected by the combined stressors of lower body joint pain.Citation41
Interrelated obesity factors that contribute to chronic musculoskeletal pain
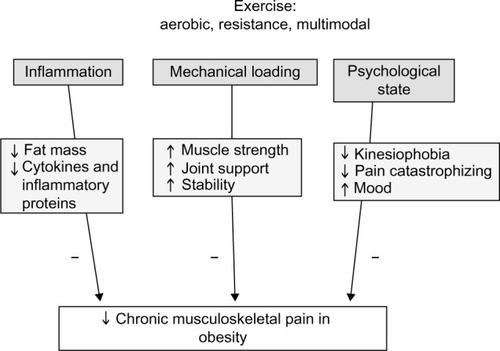
Among several potential mechanisms that may mediate the relationships between pain in obesityCitation42 are mechanical loading,Citation43 inflammation,Citation44 and psychological status.Citation23,Citation45 Obesity itself is associated with high mechanical stresses on the bodyCitation26 and high tissue inflammation.Citation46 Moreover, obesity is associated with several negative psychological alterations that include pain catastrophizing and fear of movement due to pain. It has recently been suggested that there is an interrelationship between mechanical loading, chronic pain, inflammation, and psychological status.Citation1,Citation38,Citation47 It remains unclear, however, whether the inflammation and psychological stress directly contribute to obesity, or whether obesity results in inflammation and stress that propagate weight gain. shows the proposed relationships between these factors. Obesity increases musculoskeletal stress and inflammation and reduces psychological health. Each factor, however, may also independently and directly impact the other factors in this relationship. For example, depression or chronic mental stress may lead to systemic inflammation and disinterest in healthy lifestyle habits. Alternatively, obesity can produce low self-efficacy and self-worth, both of which lead to psychological stress and inflammation. In each situation, the intersection of these collective factors is strongly related to pain in the musculoskeletal system.
Figure 1 Proposed relationships between mechanical loading, inflammation and psychological state in obesity-related musculoskeletal pain
Abbreviations: TNF-α, tumor necrosis factor-α; CRP, C-reactive protein.

Mechanical loading
Body weight is directly related to the loading on the musculoskeletal system. Overweight and obesity increase the risk by two to four times for clinically important joint pain increase over 2 years compared to normal weight.Citation48 With progressively higher classification of obesity, compressive loading increases across joints. In knee osteoarthritis (OA), people with class 2+ obesity have greater peak compressive knee forces than overweight people (2,293 N vs 2,182 N).Citation49 This compression is accompanied by greater, although not significant, knee shear forces and patellofemoral forces acting at the knee.Citation49 Obese persons have been shown to have inadequate strength to control loading and maintain normal alignment of joints. Subsequently, aberrant biomechanics during locomotor tasks occur. In the feet, muscle weakness precludes adequate arch support, and the foot jointsCitation50 experience excessive and unaccustomed compressive plantar loading.Citation11,Citation51 In peripheral joints like the knee, there is a relative strength deficit of the knee flexors and extensors which contributes to misalignment of the tibiofemoral joint (favoring genu valgum).Citation49 The combination of the loading and poor mechanics directly increases the tissue stresses to the articular cartilage and connective tissues within the joints. Obesity can induce joint pain by these pathomechanical mechanisms:Citation52 1) altered distribution of weight loading occurs on cartilaginous areas of joint unaccustomed to loading and 2) loading may intensify across a small cross-sectional area of the joint and focally cause tissue damage. Because there is a compensatory offloading from painful areas to areas that are not in pain, there is an eventual progression of mechanical stress and pain to the loaded area.
In axial joints, the distribution of adipose tissue can shift the center of mass and affect mechanical alignment of axial joints. For example, abdominal adiposity shifts the center of mass forwardCitation53 and increases the posterior mechanical loading to structural areas of the spine that articulate, such as the facet joints of the vertebrae. Back pain is the net result. Even with upper body tasks, scapular kinematics are different in obese people compared to people with healthy weight. Scapulorthoracic motion comprises greater scapular upward rotation in obesity during arm lift and when lifting an object.Citation54 While this movement strategy is a compensation to manage arm mass, this aberrant pattern is related to shoulder rotator cuff tears and pain.Citation54
Soft tissues are also victims of obesity-loading stress. Intervertebral disks are susceptible to degeneration in obese people, but the mechanism for disk breakdown remains speculative.Citation9 Obesity compresses the vertebral column and narrows disk spaces, and progression of the degeneration includes neuroforaminal stenosis and altered biomechanics,Citation55 both of which may contribute to pain. Achilles, patella, and elbow tendinopathies are related to the presence of the metabolic syndrome.Citation47 Magnetic resonance imaging showed that the prevalence of tendon and ligamentous pathologies of the ankle is 1.59 times higher in persons with BMI >25 kg/m2 compared to people with lower BMI values.Citation56
Inflammation
Inflammation is a state that fosters nociception in damaged musculoskeletal tissues and prevents healing.Citation47 Inflammation can be an activator of pain in obesity, and conversely can be activated by obesity-related mechanical stressors in tissue. Cytokines can activate central nervous system tissues and mediate a “sickness response”, fatigue, depressive symptoms, and hyperalgesia.Citation57 Chronic pain stresses and exhausts the hypothalamic–pituitary axis (HPA), leading to perpetual reactivation of a sensitized stress response.Citation12 Hypocortisolism normally occurs after a stressful event, but over the long term, cortisol responses are delayed. Cortisol dysfunction results in systemic inflammation, and inflammation itself initiates and prolongs pain.Citation58 This endocrine response can be intensified in people who exaggerate their responses to pain. For example, hypervigilance to pain, catastrophizing, negative thinking, or maladaptive thoughts or avoidant-coping strategies are behaviors that are related to frequent or prolonged stimulation of the HPA.Citation12
Pro-inflammatory proteins such as cytokines are released by immune cells, adipocytes, and other tissues.Citation57 C-reactive protein (CRP) and interleukins (ILs) are elevated in persons with chronic musculoskeletal pain (low back pain [LBP], knee pain, foot pain, joint pain)Citation19,Citation42,Citation59 and more so in obese persons compared to persons with normal weight. Obese people have high adipose tissue volume in the viscera and the intramuscular and perimuscular spaces. Excess fat volume effects are insidious in nature as they produce high levels of CRP, tumor necrosis factor-α (TNF-α), IL-6, IL-1β, and leptin, among others.Citation46 High levels of these biomarkers are directly related to pain severity in persons with joint disease.Citation60 Both systemic adipose tissue volume and local fat deposition may cause inflammation in areas that develop pain. As BMI and fat volume increase, the macrophages enter adipose tissue and are activated to behave like an infection is present.Citation47 This state of “adisopathy” (sick fat tissue) promotes increased tissue pain. Some fat depots near joints act as local mediators of pain, such as the infrapatellar fat pad. This pad is highly innervated by C-fiber neurons that secrete substance P, which mediates pain and activates immune cells and local production of IL-6 and TNF-α.Citation61 Thus, one explanation for non-weight-bearing joint pain in obese people may be a consequence of chronic inflammation. It is unclear how generalized exercise can reduce pain in non-weight-bearing joints.
The state of tissue loading impacts the level of inflammation. Both sedentary living and excessive loading activate systemic inflammation.Citation47 When tissues are excessively loaded and aberrant gait patterns occur, degradation of the cartilaginous matrix begins, and inflammatory cytokines are released into the joint space and cause inflammation.Citation62 Breakdown products from damaged extracellular matrix (fibronectin, hyaluranons) trigger release of TNF-α, IL-1β, IL-6, IL-8, and matrix metalloproteinases that perpetuate tissue damage.Citation61 One of the most studied models of this phenomenon is in knee OA. With repeated loading trauma to the knee, inflammatory mediators are released from the synovium and cartilage of the joint. Cytokines, prostaglandins, proteolytic enzymes, and leukotrienes are released into the synovial fluid, and this promotes pain onset.Citation61 This type of process also occurs in vertebral disks in persons with back pain. Systemic biomechanical loading with obesity can damage the disk and promote accumulation of breakdown products and tissue inflammation.Citation55 Inflammatory processes propagate disk degeneration and structural instability. Nociception is increased when fat-derived neuropeptides are released.
Psychological outlook
In both young and old obese persons, pain is associated with relatively low psychosocial health when compared with persons with normal weight.Citation63 Common characteristics in obese persons with pro-inflammatory conditions include fatigue, lethargy, social withdrawal, and irritability.Citation47 Negative factors associated with increased prevalence of pain and multisite pain are obesity, anxiety, and depression.Citation64 Moreover, pain symptoms are worse in obese people with the same musculoskeletal condition. For example, obese people with rheumatoid arthritis have higher pain levels, disability, and lower self-efficacy than nonobese people with rheumatoid arthritis.Citation65
Inflammation is interconnected with negative psychological status. Hyperalgesia may be due to systemic elevations of inflammatory cytokines in the body. Variation in depression levels of obese people is explained 20% by elevated CRP.Citation66 Anxiety and depression are directly related to circulating levels of IL-6 and CRP in obese people.Citation67 Cytokines can mediate other behavioral changes that can contribute to sedentary behavior including sadness, social-behavioral withdrawal, and anhedonia.Citation68 In obesity, there is a prolonged activation of cytokine production, which contributes to chronic pain.
Obesity is related to avoidance of physical activity, disability, and worsening of pain.Citation1 With repeated pain exposures, catastrophizing may occur. Pain catastrophizing is an exaggerated negative orientation to harmful stimuli.Citation69 People who catastrophize magnify the focus on pain, amplify pain sensations and experience pain that is more unpleasant, and feel helpless when pain is present.Citation70 Morbidly obese patients with joint pain are more likely to engage in pain-catastrophizing behavior.Citation69,Citation71 Often, catastrophizing leads to maladaptive behaviors such as activity avoidance that perpetuate continued weight gain and physical inactivity.Citation69,Citation70 Pain catastrophizing may initiate a pathway of development of fear of movement (kinesiophobia) due to pain and reduce self-efficacy for performing physical tasks.Citation70
Kinesiophobia and activity avoidance–adaptation behaviors can be triggered during daily weight-bearing activities such as walking, functional tasks, or transfers.Citation72 It has been shown that morbidly obese adults with kneeCitation73 and chronic back painCitation63 experience 13%–18% higher fear levels compared to nonobese or less obese adults. Kinesiophobia is a predictor for ambulatory pain and perceived disability but not necessarily for physical function.Citation74 Despite physical potential, kinesiophobia interferes with voluntary participation in regular physical activity.
Exercise interventions for chronic musculoskeletal pain
Regular exercise has been identified as primary prevention against over 35 chronic conditions including obesity, joint pain-related conditions, and anxiety and depression. Exercise stimulation can positively impact chronic pain mediators by exerting anti-inflammatory effects,Citation67 increasing muscle strength and muscle coordination, and improving psychological outlook.Citation67 A systematic literature search using PubMed was conducted to identify articles of exercise programs for pain in obese persons that were published between the years 1980 and 2014. The search terms “obese and chronic pain” initially resulted in 804 articles. Of these articles, it was noted that a majority of research in this population and chronic pain was associated with degenerative joint disease such as OA. Additional search terms were added to refine our article consortium such as “exercise”, “musculoskeletal”, “knee”, “spine”, “foot”, “shoulder”, and “elbow”. Each of the articles was read by the authors to determine whether the study was relevant for this review. A total of 15 intervention studies were included in this review of the use of exercise to combat chronic pain in obese individuals (). Fourteen were exercise-based interventions for specific joint pain, and one used exercise for general musculoskeletal pain in obese persons.Citation75 An important point is that several of these identified studies included weight management or weight loss programs that contained exercise as a main component of the program.Citation76
Table 1 Summary of exercise programs to treat chronic musculoskeletal pain in obese individuals
Exercise programs can include resistance exercise (RX; the use of weight or resistance to overload muscle), aerobic exercise (AX; repetitive motions of large muscle groups sufficient to increase heart rate), or multimodal activities consisting of a combination of RX and AX modes. A substantial amount of evidence exists, evaluating the effectiveness of RXs and AXs to treat and reduce pain in obese individuals with OACitation2,Citation77–Citation83 and other forms of chronic pain.Citation19,Citation32,Citation79 However, the literature addressing chronic pain in obesity itself is limited. Most of the research has focused on exercise treatment of one painful musculoskeletal area or joint. The following sections present the use of exercise and physical activity to combat chronic pain in this population. provides a summary of the effects of exercise programs on musculoskeletal pain symptoms in obese individuals.
Exercise for chronic LBP
Of the estimated 34 million Americans suffering from chronic LBP, 64.3% of respondents were overweight or obese.Citation84 It has also been reported that chronic LBP in the obese population is a significant contributor to fear avoidance behaviors and further increases in functional disability.Citation85 Therefore, reducing pain associated with LBP in obese persons can stunt the vicious pain disabling and weight gain cycle experienced by obese individuals.
Two recent analyses were performed that compared different resistance protocols for chronic LBP in obese persons.Citation86,Citation87 Abdominally obese adults aged 6–85 years with chronic LBP were randomized to total body resistance (TOTRX; ten upper and lower body RXs and lumbar extension), isolated lumbar extension exercise (LEXT; participants performed lumbar extension only), or the non-exercise control group (CON). All participants received the standard of care, pamphlets, and education materials on physical activity guidelines and weight loss benefits.Citation86 Resting and pain with activity were measured during walking, stair climbing, and chair rise. Greater reductions in resting average back pain levelsCitation87 and walking pain were achieved with TOTRX and LEXT compared to CON (60.5% and 42.0% vs 6.4%, respectively).Citation86 Pain with chair rise was decreased by 49.8% in TOTRX group compared to the other groups (3.7% and 0.3% reduction).Citation86 Pain during functional tasks was also significantly decreased in the TOTRX group compared to the others.Citation86 In these studies, participants did not lose weight despite pain relief. Subsequent studies should focus on whether or not there is additive pain relief with exercise and weight loss compared to each individually.
Based on our search of the literature, there were no other studies examining the effects of exercise to reduce LBP in obese individuals. Minimal evidence exists supporting the use of back extension exercises in the general population with LBP.Citation88 However, the data presented above combined with previously accepted protocols for therapeutic interventions in LBP are encouraging and suggest that RXs combined with targeted back extension exercises can significantly reduce pain in the obese individual safely and effectively while minimizing pain medication use.Citation86 Importantly, additional benefits of RX for LBP include a significant reduction in perceived disability due to pain as shown by improved Roland Morris Disability and Oswestry Disability Index scores, significantly lower pain catastrophizing,Citation86 and faster gait speed.Citation87 When back strength increased more than 20% from baseline, pain levels improved more than if back strength did not increase more than 20% with either TOTRX or LEXT.Citation87 From the functional perspective, lumbar strength gains are related to walking endurance improvements. The collective benefits of RX for chronic LBP in obesity may translate to a better quality of life and interest in additional healthy lifestyle behaviors in this population. Long-term studies can address this issue.
Exercise for chronic hip pain
Limited evidence exists specifically targeting exercises for chronic hip painCitation82 in obese persons. There are presently no randomized controlled trials examining the effects of using exercise for reducing OA-related hip pain in the general population.Citation82 To our knowledge, one intervention study investigated the exercise effects on hip pain reduction in obese persons.Citation76 Paans et alCitation76 combined an 8-month multi-modal exercise program with dietary weight loss to combat hip pain and physical function in obese persons. The exercise program consisted of moderate-to-intense AX (treadmill, bike, stepper, rowing machines) and RX.Citation76 All participants received the same intervention, but specifics were modified to accommodate individual needs and abilities. There was no control group; participants were compared to their baseline scores to assess improvements. Significant improvements were observed at the 8-month follow-up for both pain and functional abilities based on the Western Ontario McMaster Osteoarthritis Index (WOMAC) and Medical Outcomes Short Form 36 (SF-36).Citation76 Pain domains of the WOMAC and the SF-36 decreased by 36.6% and 25.4%, respectively.Citation76 Other benefits for hip pain included 32.6%–47.1% improvements in perceived physical function as on the WOMAC and SF-36, respectively.Citation76 Walking mobility improved by 11.1% at 8-month follow-up.Citation76 These results are promising, but due to the lack of a control group and separate analysis of exercise vs weight loss alone, further evidence is needed to definitively state the effects of exercise reducing pain in obese individuals with hip OA. Further research is warranted to understand the specific mechanisms of pain relief in hip OA.
Exercise interventions for chronic knee pain
Approximately 60 million Americans have knee OA,Citation2 and about 10%–30% of these individuals have such severe pain that their functional ability is restricted leading to disability.Citation2 The addition of a BMI ≥30 kg/m2 increases the risk of developing knee OA fourfold compared to healthy weight individuals.Citation89 Chronic knee pain perpetuates activity avoidance and additional weight gain. Hence, preventing and/or restoring functional capacity while mitigating pain in obese patients is critical for prolonged adherence to exercise programs.
Both AXCitation90 and RXCitation91–Citation93 programs of varying duration from 2 months to 24 months can significantly reduce knee pain. AX-based interventions used walkingCitation90 or aquatic running– cycling exerciseCitation94 as the primary stimulus. Aquatic exercise appears to confer rapid knee pain relief within 2 months compared to walking over a 12-month duration. RX-based programs have used low resistance weights, therapy bands, or pneumatic machines to induce pain relief.Citation91–Citation93,Citation95 While AX activates muscles about the knee in a linear anteroposterior direction, RX activates multiple muscle groups about the knee and in joints above and below the knee to improve strength across different planes of motion. RX may act by correcting muscle strength deficits and knee instability, thereby allowing the affected individual to engage in more activity with less pain.Citation95 One report showed that pain relief may be greater in people who have neutral knee alignment compared to varus alignment,Citation93 suggesting that other treatments such as bracing may increase effectiveness of RX on pain relief. Supervised and home-based programs are effective in increasing quadriceps strength and reducing pain over the long term.Citation95
Multimodal exercise programs have been used alone or combined with other treatments such as dietary modification, weight loss, or pain-coping skills training to treat knee pain.Citation71,Citation96,Citation97 Both AX and RX activities are combined together during single-exercise sessions in alternating or sequential fashion. Exercise is important for long-term maintenance of mobility and walking endurance.Citation98 Pain severity, inflammatory cytokine levels such as IL-6, and body weight are lowered more with exercise and dietary modification compared to either treatment alone.Citation96,Citation98 One study examined the independent and combined effects of multimodal exercise and pain-coping skill training on pain and functional outcomes in obese people with knee OA over 6 months.Citation71 The combined treatments were superior with respect to producing greater reductions in self-reported pain, physical function, joint stiffness, pain catastrophizing, and greater improvements in self-efficacy and psychological outlook than each treatment alone.Citation71 The use of multimodal exercise for pain relief is effective for knee pain in obese people, but exercise benefits may be enhanced with the addition of dietary restriction or pain-coping skills.
Exercise for generalized or whole body pain
Presently, there is limited research assessing the effects of exercise on generalized pain in obesity. One investigation was designed to test the use of a “musculoskeletal pain physical therapy program” prior to entering a weight management program.Citation75 The weight management protocol included daily caloric restriction to 1,200–1,800 kcal/day and multimodal exercise (AX three times per week, RX two times per week). Snow et alCitation75 reported that patients who received the intervention had a reduction in mean bodily pain by 56% prior to participation. During the weight management phase, the intervention and control groups experienced similar weight loss, depression scores, and exercise capacity.Citation75 In contrast to expectations, the intervention group did not demonstrate greater weight loss or ability to exercise at higher intensities. It is possible that the participants achieved their goal of pain reduction and perceived that the intervention was a success. Additional research could examine what biochemical or psychobiological factors may be favorably altered by therapy programs or different exercise programs. This information could help practitioners and therapists determine the best exercise strategy to manage pain in obese patients.
Mechanisms of exercise improvement of musculoskeletal pain
summarizes the potential exercise-related mechanisms underlying pain in children and adults. Each positive change in one mechanism favorably contributes to the others. Reductions in body weight with AX can reduce mechanical loading and structural damage to the weight-bearing joints and tissues,Citation2 thereby reducing the inflammatory response to damage. RX corrects strength deficits around painful joints and may help restore normal joint kinematics. Reduction of visceral, subcutaneous, and local body fat volumes with AX lowers the production of circulating pro-inflammatory cytokines and proteins.Citation99 Regular participation in high-intensity intermittent physical activity lowers systemic levels of inflammatory cytokines (CRP, IL-6, and TNF-α), but the greatest anti-inflammatory benefit occurs with the multimodal exercise.Citation100 RX increases self-efficacy and reduces depression symptoms,Citation1 which lower stress and HPA activity. Total mood disturbance is attenuated, and several psychosocial domains such as tension, anger, vigor, fatigue body areas satisfaction, and physical self-concept are significantly improved with supervised exercise.Citation101 These positive changes enhance stress reduction and complement physical adaptations to exercise that collectively contribute to pain relief in obese persons. Future studies can examine whether there are “responders” to exercise who are able to make better improvements in specific mechanisms and thereby experience better pain relief than “nonresponders”.
Solutions for increasing exercise adherence in obese individuals
The American College of Sports Medicine,Citation102 the American Dietetic Association,Citation103 and the American Heart AssociationCitation104 provide evidence-based recommendations for physical activity prescriptions for significant weight loss and maintenance. However, adherence to exercise is a challenge for obese persons, as shown by attrition rates ranging from 43.5% (children)Citation105 and 50% (adults).Citation101 There are several possible solutions to help improve adherence and increase the enjoyment of exercise and physical activity. First, tailoring exercise programs to accommodate the needs and abilities of obese individuals is recommended.Citation106 Modifications to the specific exercises may be necessary to offset the acute pain with mechanical loading. For example, RXs can be performed within the non-painful range of motion (reduce the overall motion of the knee extension or flexion exercise). Second, walking or running can be painful for obese persons, but incline walking at slower speeds is less painful or not painful,Citation107 which fosters adherence. As weight is reducedCitation108 or pain improves, speed, duration, and frequency of AX can increase. Third, on days when musculoskeletal pain flares occur, the use of nonimpact exercise may be more comfortable than impact exercise. Examples of this include aquatic treadmill, cycle or pool exercise classes, elliptical machines, or Nordic ski machines. Fourth, sustained or continuous exercise may be more uncomfortable than several smaller exercise boutsCitation109 to accumulate the cardiovascular or strength stimulus necessary to accumulate benefit and pain relief. Longer bouts of sustained low- or moderate-intensity exercise may prolong pain, but shorter more intense exercise may decrease the load-bearing exposure time. Fifth, the exercise program should not progress more than 5%–10% of weekly mileage or duration. This threshold has been proposed to permit bone tissues to “rest” and avoid mechanical failure.Citation109 Studies that determine the reasons for obese persons failing to maintain exercise levels with or without pain relief would help practitioners identify obese patients who may need additional interventions to promote adherence.
For individuals experiencing pain too disabling for regular movement, pain reduction is paramount for breaking the cycle of pain-related inhibition of exercise. Depending on the location of the pain and the severity, several medications may be used to reduce pain to make exercise more tolerable. For example, nonsteroidal anti-inflammatory medications such as ibuprofen, naproxen, or aspirin can help control inflammatory processes associated with obesity and pain severity. Procedural treatments such as intra-articular injections of corticosteroids and hyaluronic acid preparations into the knee, hip, or shoulder may be used for immediate and long-term pain relief, thereby allowing the individual to exercise, burn calories, and improve function.Citation1
Exercise-induced joint pain should not persist or increase by 24 hours after exercise, which is an indication that the musculoskeletal system was not prepared for the exercise, or physical days will permit the individual to make a self-assessment of the pain response.Citation109 If an obese person with preexisting mild joint pain starts activity (<3 points out of a 10-point scale), similar guidelines apply: the pain should not worsen during the exercise session or last into the next day. If the pain causes a limp or a compensatory gait change, the exercise volume must be reduced, or the exercise must be stopped until a normal gait pattern is achieved. It has been suggested that strengthening exercise or RX be initiated prior to starting a formal AX program to help develop muscle strength, joint support, and stability.Citation109 Control of exercise pain and functional ability may foster enjoyment of exercise and better adherence.
Conclusion
Obesity is associated with general and specific musculoskeletal pain. There is an interrelationship between mechanical loading, chronic pain, inflammation, and psychological status in obese persons. AX, RX, or multimodal exercise programs can reduce joint pain in young and older obese adults in the range of 14%–71.4% via one or more of these three potential mechanisms. While adherence to regular exercise is low, several methods to increase adherence include modification of exercise including splitting up exercise duration into smaller bouts, reducing joint range of motion, and minimizing impact activity. Additional research is necessary to determine the following: 1) if there are characteristics of responders to exercise that favor weight loss and long-term pain relief; 2) if there are additive effects of exercise and weight loss on musculoskeletal pain severity; and 3) if the quality of life can be improved with exercise-induced pain relief. This field would benefit from rigorous comparative efficacy studies of exercise intensity, frequency, and mode on specific and general musculoskeletal pain in young and older obese persons.
Disclosure
The authors report no conflicts of interest in this work.
References
- VincentHKAdamsMCBVincentKRHurleyRWMusculoskeletal pain, fear avoidance behaviors, and functional decline in obesity: potential interventions to manage pain and maintain functionReg Anesth Pain Med201338648149124141874
- VincentKRVincentHKResistance exercise for knee osteoarthritisPM R201245 SupplS45S5222632702
- AndersenRECrespoCJBartlettSJBathonJMFontaineKRRelationship between body weight gain and significant knee, hip, and back pain in older AmericansObes Res200311101159116214569039
- HeoMAllisonDBFaithMSZhuSFontaineKRObesity and quality of life: mediating effects of pain and comorbiditiesObes Res200311220921612582216
- AnandacoomarasamyACatersonIDLeibmanSInfluence of BMI on health-related quality of life: comparison between an obese adult cohort and age-matched population normsObesity200917112114211819390522
- SmithSMSumarBDixonKAMusculoskeletal pain in overweight and obese childrenInt J Obes20143811115
- JohnsonNBHayesLDBrownKHooECEthierKACDC National Health Report: leading Causes of Morbidity and Mortality and Associated Behavioral Risk and Protective Factors-United States, 2005–2013MMWR Surveill Summ20146332725356673
- GlassNATornerJCFrey LawLAThe relationship between quadriceps muscle weakness and worsening of knee pain in the MOST cohort: a 5-year longitudinal studyOsteoarthr Cartil20132191154115923973125
- YooJJLimSHChoNHKimHARelationships between body mass index, fat mass, muscle mass, and musculoskeletal pain in community residentsArthritis Rheumatol201466123511352025185757
- NilsenTILHoltermannAMorkPJPhysical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: longitudinal data from the Nord-Trøndelag health studyAm J Epidemiol2011174326727321633119
- De Sá PintoALDe Barros HolandaPMRaduASVillaresSMLimaFRMusculoskeletal findings in obese childrenJ Paediatr Child Health200642634134416737474
- HannibalKEBishopMDChronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitationPhys Ther201494121816182525035267
- EganAMMahmoodWAFentonRBarriers to exercise in obese patients with type 2 diabetesQJM2013106763563823525164
- GrovenKSEngelsrudGDilemmas in the process of weight reduction: exploring how women experience training as a means of losing weightInt J Qual Stud Health Well-Being2010225
- SallinenJLeinonenRHirvensaloMLyyraT-MHeikkinenERantanenTPerceived constraints on physical exercise among obese and non-obese older peoplePrev Med200949650651019833148
- ShelbyRASomersTJKeefeFJPellsJJDixonKEBlumenthalJADomain specific self-efficacy mediates the impact of pain catastrophizing on pain and disability in overweight and obese osteoarthritis patientsJ Pain200891091291918602871
- LementowskiPWZelicofSBObesity and osteoarthritisAm J Orthop200837314815118438470
- GrotleMHagenKBNatvigBDahlFAKvienTKObesity and osteoarthritis in knee, hip and/or hand: an epidemiological study in the general population with 10 years follow-upBMC Musculoskelet Disord2008913218831740
- DeereKCClinchJHollidayKObesity is a risk factor for musculoskeletal pain in adolescents: findings from a population-based cohortPain201215391932193822805779
- GayACullifordDLeylandKArdenNKBowenCJAssociations between body mass index and foot joint pain in middle-aged and older women: a longitudinal population-based cohort studyArthritis Care Res2014661218731879
- JentzschTGeigerJSlankamenacKWernerCMLObesity measured by outer abdominal fat may cause facet joint arthritis at the lumbar spineJ Back Musculoskelet Rehabil Epub2014624
- Fowler-BrownAWeeCCMarcantonioENgoLLeveilleSThe mediating effect of chronic pain on the relationship between obesity and physical function and disability in older adultsJ Am Geriatr Soc201361122079208624329819
- HittHCMcMillenRCThornton-NeavesTKochKCosbyAGComorbidity of obesity and pain in a general population: results from the southern pain prevalence studyJ Pain20078543043617337251
- ZhangWMcWilliamsDFInghamSLNottingham knee osteoarthritis risk prediction modelsAnn Rheum Dis20117091599160421613308
- PainHWilesRThe experience of being disabled and obeseDisabil Rehabil200628191211122017005482
- VincentHKRaiserSNVincentKRThe aging musculoskeletal system and obesity-related considerations with exerciseAgeing Res Rev201211336137322440321
- Evers LarssonUMattssonEFunctional limitations linked to high body mass index, age and current pain in obese womenInt J Obes Relat Metab Disord200125689389911439305
- GarverMJFochtBCDialsJWeight status and differences in mobility performance, pain symptoms, and physical activity in older, knee osteoarthritis patientsArthritis2014201437590924963401
- RimmerJHHsiehKGrahamBCGerberBSGray-StanleyJABarrier removal in increasing physical activity levels in obese African American women with disabilitiesJ Womens Health2010191018691876
- Centers for Disease Control and Prevention (CDC)Arthritis as a potential barrier to physical activity among adults with obesity – United States, 2007 and 2009MMWR Morb Mortal Wkly Rep2011601961461821597454
- BallKCrawfordDOwenNToo fat to exercise? Obesity as a barrier to physical activityAust N Z J Public Health200024333133310937415
- AtchisonJWVincentHKObesity and low back pain: relationships and treatmentPain Manag201221798624654621
- TsuritaniIHondaRNoborisakaYIshidaMIshizakiMYamadaYImpact of obesity on musculoskeletal pain and difficulty of daily movements in Japanese middle-aged womenMaturitas2002421233012020976
- SharkeyJROryMGBranchLGSevere elder obesity and 1-year diminished lower extremity physical performance in homebound older adultsJ Am Geriatr Soc20065491407141316970650
- VitonJ-MTimsitMMesureSMassionJFranceschiJ-PDelarqueAAsymmetry of gait initiation in patients with unilateral knee arthritisArch Phys Med Rehabil200081219420010668774
- ConstantinouMBarrettRBrownMMillsPSpatial-temporal gait characteristics in individuals with hip osteoarthritis: a systematic literature review and meta-analysisJ Orthop Sports Phys Ther2014444291B724450373
- HillsAPParkerAWGait characteristics of obese childrenArch Phys Med Rehabil19917264034072059108
- AndriacchiTPFavreJThe nature of in vivo mechanical signals that influence cartilage health and progression to knee osteoarthritisCurr Rheumatol Rep2014161146325240686
- MillsKHettingaBAPohlMBFerberRBetween-limb kinematic asymmetry during gait in unilateral and bilateral mild to moderate knee osteoarthritisArch Phys Med Rehabil201394112241224723747645
- EitzenIFernandesLNordslettenLSnyder-MacklerLRisbergMAWeight-bearing asymmetries during Sit-To-Stand in patients with mild-to-moderate hip osteoarthritisGait Posture201439268368824238750
- MarksRObesity profiles with knee osteoarthritis: correlation with pain, disability, disease progressionObesity20071571867187417636106
- ButterworthPAUrquhartDMCicuttiniFMFat mass is a predictor of incident foot painObesity2013219E495E49923512967
- MessierSPGutekunstDJDavisCDeVitaPWeight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritisArthritis Rheum20055272026203215986358
- KaurJA comprehensive review on metabolic syndromeCardiol Res Pract2014201494316224711954
- MarcusDAObesity and the impact of chronic painClin J Pain200420318619115100595
- CesariMKritchevskySBBaumgartnerRNSarcopenia, obesity, and inflammation – results from the Trial of Angiotensin Converting Enzyme Inhibition and Novel Cardiovascular Risk Factors studyAm J Clin Nutr200582242843416087989
- SeamanDRBody mass index and musculoskeletal pain: is there a connection?Chiropr Man Therap20132115
- ParadowskiPTEnglundMLohmanderLSRoosEMThe effect of patient characteristics on variability in pain and function over two years in early knee osteoarthritisHealth Qual Life Outcomes200535916188034
- MessierSPPaterMBeaversDPInfluences of alignment and obesity on knee joint loading in osteoarthritic gaitOsteoarthritis Cartilage201422791291724857973
- MonteiroMGabrielRAranhaJNeves e CastroMSousaMMoreiraMInfluence of obesity and sarcopenic obesity on plantar pressure of postmenopausal womenClin Biomech2010255461467
- FabrisSMFaintuchJBrienzeSLAre knee and foot orthopedic problems more disabling in the superobese?Obes Surg201323220120422986802
- AndriacchiTPMündermannASmithRLAlexanderEJDyrbyCOKooSA framework for the in vivo pathomechanics of osteoarthritis at the kneeAnn Biomed Eng200432344745715095819
- MenegoniFGalliMTacchiniEVismaraLCavigioliMCapodaglioPGender-specific effect of obesity on balanceObesity200917101951195619325540
- GuptaMDashottarABorstadJDScapula kinematics differ by body mass indexJ Appl Biomech201329438038522923369
- SamartzisDKarppinenJCheungJLotzJDisk degeneration and low back pain: are they fat-related conditions?Global Spine J2013030313314424436864
- GalliMMProtzmanNMMandelkerEMMalhotraASchwartzEBrigidoSAComparing tendinous and ligamentous ankle pathology in atraumatic overweight and nonoverweight patients: a comprehensive MRI reviewFoot Ankle Spec20147644945625005703
- IrwinMRInflammation at the intersection of behavior and somatic symptomsPsychiatr Clin North Am201134360562021889682
- ArranzL-IRafecasMAlegreCEffects of obesity on function and quality of life in chronic pain conditionsCurr Rheumatol Rep201416118
- BriggsMSGivensDLSchmittLCTaylorCARelations of C-reactive protein and obesity to the prevalence and the odds of reporting low back painArch Phys Med Rehabil201394474575223187041
- BasSFinckhAPuskasGJAdipokines correlate with pain in lower limb osteoarthritis: different associations in hip and kneeInt Orthop201438122577258325005460
- SokoloveJLepusCMRole of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretationsTher Adv Musculoskelet Dis201352779423641259
- GoldringMBOteroMInflammation in osteoarthritisCurr Opin Rheumatol201123547147821788902
- VincentHKOmliMRDayTHodgesMVincentKRGeorgeSZFear of movement, quality of life, and self-reported disability in obese patients with chronic lumbar painPain Med201112115416421087405
- HoftunGBRomundstadPRRyggMFactors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the Young-HUNT Study 2008J Pain201213987488322832694
- SomersTJWrenAABlumenthalJACaldwellDHuffmanKMKeefeFJPain, physical functioning, and overeating in obese rheumatoid arthritis patients: do thoughts about pain and eating matter?J Clin Rheumatol201420524425025036564
- DalyMThe relationship of C-reactive protein to obesity-related depressive symptoms: a longitudinal studyObesity (Silver Spring)201321224825023404927
- CapuronLPoitouCMachaux-TholliezDRelationship between adiposity, emotional status and eating behaviour in obese women: role of inflammationPsychol Med20114171517152820961476
- SlavichGMIrwinMRFrom stress to inflammation and major depressive disorder: a social signal transduction theory of depressionPsychol Bull2014140377481524417575
- SomersTJKeefeFJPellsJJPain catastrophizing and pain-related fear in osteoarthritis patients: relationships to pain and disabilityJ Pain Symptom Manage200937586387219041218
- SomersTJKeefeFJCarsonJWPellsJJLaCailleLPain catastrophizing in borderline morbidly obese and morbidly obese individuals with osteoarthritic knee painPain Res Manag200813540140618958312
- SomersTJBlumenthalJAGuilakFPain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled studyPain201215361199120922503223
- Gooberman-HillRWoolheadGMacKichanFAyisSWilliamsSDieppePAssessing chronic joint pain: lessons from a focus group studyArthritis Care Res2007574666671
- VincentHKLambKMDayTITillmanSMVincentKRGeorgeSZMorbid obesity is associated with fear of movement and lower quality of life in patients with knee pain-related diagnosesPM R20102871372220709300
- VincentHKSeayANMonteroCConradBPHurleyRWVincentKRKinesiophobia and fear-avoidance beliefs in overweight older adults with chronic low-back pain: relationship to walking endurance – part IIAm J Phys Med Rehabil201392543944523478452
- SnowRRuaneJLaLondeMRandomized trial assessing the impact of a musculoskeletal intervention for pain before participating in a weight management program. [Miscellaneous Article]J Cardiopulm Rehabil Prev201030317318020040884
- PaansNvan den Akker-ScheekIDillingRGEffect of exercise and weight loss in people who have hip osteoarthritis and are overweight or obese: a prospective cohort studyPhys Ther201393213714623023813
- DoiTAkaiMFujinoKEffect of home exercise of quadriceps on knee osteoarthritis compared with nonsteroidal antiinflammatory drugs: a randomized controlled trialAm J Phys Med Rehabil200887425826918356618
- EscalanteYGarcía-HermosoASaavedraJMEffects of exercise on functional aerobic capacity in lower limb osteoarthritis: a systematic reviewJ Sci Med Sport201114319019821111676
- EscalanteYSaavedraJMGarcía-HermosoASilvaAJBarbosaTMPhysical exercise and reduction of pain in adults with lower limb osteoarthritis: a systematic reviewJ Back Musculoskelet Rehabil201023417518621079296
- EttingerWHJrBurnsRMessierSPA randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST)JAMA1997277125318980206
- FarrJNGoingSBMcKnightPEKasleSCusslerECCornettMProgressive resistance training improves overall physical activity levels in patients with early osteoarthritis of the knee: a randomized controlled trialPhys Ther201090335636620056719
- FransenMMcConnellSExercise for osteoarthritis of the kneeCochrane Database Syst Rev20084CD00437618843657
- FransenMMcConnellSLand-based exercise for osteoarthritis of the knee: a metaanalysis of randomized controlled trialsJ Rheumatol20093661109111719447940
- StrineTWHootmanJMUS national prevalence and correlates of low back and neck pain among adultsArthritis Care Res2007574656665
- VincentHKSeayANMonteroCConradBPHurleyRWVincentKRFunctional pain severity and mobility in overweight older men and women with chronic low-back pain – part IAm J Phys Med Rehabil201392543043823478453
- VincentHKGeorgeSZSeayANVincentKRHurleyRWResistance exercise, disability, and pain catastrophizing in obese adults with back painMed Sci Sports Exerc20144691693170125133997
- VincentHKVincentKRSeayANConradBPHurleyRWGeorgeSZBack strength predicts walking improvement in obese, older adults with chronic low back painPM R20146541842624211698
- MiltnerOWirtzDCSiebertCHStrengthening lumbar extensors – therapy of chronic back pain – an overview and meta-analysisZ Orthop Ihre Grenzgeb2001139428729311558044
- BrosseauLWellsGATugwellPOttawa panel evidence-based clinical practice guidelines for the management of osteoarthritis in adults who are obese or overweightPhys Ther201191684386121493746
- BrosseauLWellsGAKennyGPThe implementation of a community-based aerobic walking program for mild to moderate knee osteoarthritis: a knowledge translation randomized controlled trial: part II: clinical outcomesBMC Public Health201212107323234575
- ForoughiNSmithRMLangeAKSinghMAFVanwanseeleBProgressive resistance training and dynamic alignment in osteoarthritis: a single-blind randomised controlled trialClin Biomech (Bristol Avon)20112617177
- McKnightPEKasleSGoingSA comparison of strength training, self-management, and the combination for early osteoarthritis of the kneeArthritis Care Res20106214553
- LimB-WHinmanRSWrigleyTVSharmaLBennellKLDoes knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trialArthritis Rheum200859794395118576289
- LimJ-YTchaiEJangS-NEffectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trialPM R20102872373120709301
- JenkinsonCMDohertyMAveryAJEffects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trialBMJ2009339b317019690345
- MessierSPMihalkoSLLegaultCEffects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the idea randomized clinical trialJAMA2013310121263127324065013
- OyeyemiALBody mass index, pain and function in individuals with knee osteoarthritisNiger Med J201354423023524249947
- MessierSPLoeserRFMillerGDExercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion TrialArthritis Rheum20045051501151015146420
- CamposRMde MelloMTTockLAerobic plus resistance training improves bone metabolism and inflammation in adolescents who are obeseJ Strength Cond Res201428375876624263653
- NimmoMALeggateMVianaJLKingJAThe effect of physical activity on mediators of inflammationDiabetes Obes Metab201315s3516024003921
- AnnesiJJWhitakerACWeight loss and psychologic gain in obese women – participants in a supported exercise interventionPerm J2008123364521331208
- DonnellyJEBlairSNJakicicJMManoreMMRankinJWSmithBKAppropriate physical activity intervention strategies for weight loss and prevention of weight regain for adultsMed Sci Sports Exerc200941245947119127177
- SeagleHMStrainGWMakrisAReevesRSAmerican Dietetic AssociationPosition of the American Dietetic Association: weight managementJ Am Diet Assoc2009109233034619244669
- RaoGBurkeLESpringBJNew and emerging weight management strategies for busy ambulatory settings a scientific statement from the American Heart Association endorsed by the society of behavioral medicineCirculation2011124101182120321824925
- SolaKBrekkeNBrekkeMAn activity-based intervention for obese and physically inactive children organized in primary care: feasibility and impact on fitness and BMIScand J Prim Health Care201028419920420831452
- KhojaSSSuskoAMJosbenoDAPivaSRFitzgeraldGKComparing physical activity programs for managing osteoarthritis in overweight or obese patientsJ Comp Eff Res20143328329924969155
- HaightDJLernerZFBoardWJBrowningRCA comparison of slow, uphill and fast, level walking on lower extremity biomechanics and tibiofemoral joint loading in obese and nonobese adultsJ Orthop Res201432232433024127395
- MillerGDNicklasBJDavisCLoeserRFLenchikLMessierSPIntensive weight loss program improves physical function in older obese adults with knee osteoarthritisObesity20061471219123016899803
- VincentHKVincentKRConsiderations for initiating and progressing running programs in obese individualsPM R20135651351923790819