Abstract
Chronic musculoskeletal pain conditions are multifaceted, and approximately 20% of the adult population lives with severe chronic pain, with a higher prevalence in women and in lower income groups. Chronic pain is influenced by and interacts with physical, emotional, psychological, and social factors, and a biopsychosocial framework is increasingly applied in clinical practice. However, there is still a lack of assessment procedures based on the activated neurobiological pain mechanisms (ie, the biological part of the biopsychosocial model of pain), which may be a necessary step for further optimizing outcomes after treatments for patients with chronic pain. It has been suggested that chronic pain conditions are mainly driven by alterations in the central nervous system with little or no peripheral stimuli or nociception. In contrast, other authors argue that such central alterations are driven by peripheral alterations and nociceptive input. Microdialysis is an in vivo method for studying local tissue alterations and allows for sampling of substances in the interstitium of the muscle, where nociceptor free nerve endings are found close to the muscle fibers. The extracellular matrix plays a key role in physiologic functions of cells, including the primary afferent nociceptor. The present review mainly concerns the results of microdialysis studies and how they can contribute to the understanding of activated peripheral nociceptive and pain mechanisms in humans with chronic pain. The primary aim was to review molecular studies using microdialysis for the investigation of human chronic muscle pain, ie, chronic masticatory muscle pain, chronic trapezius myalgia, chronic whiplash-associated disorders, and chronic widespread pain/fibromyalgia syndrome. Several studies clearly showed elevated levels of serotonin, glutamate, lactate, and pyruvate in localized chronic myalgias and may be potential biomarkers. These results indicate that peripheral muscle alterations are parts of the activated pain mechanisms in common chronic pain conditions. Muscle alterations have been reported in fibromyalgia syndrome and chronic widespread pain, but more studies are needed before definite conclusions can be drawn. For other substances, results are inconclusive across studies and patient groups.
Background
Living with chronic pain
Chronic musculoskeletal pain conditions are multifaceted, and approximately 20% of the adult population lives with severe chronic pain,Citation1 with higher prevalence in women and in lower income groups.Citation2,Citation3 The 12-month prevalence of neck pain in the general population and in the working population is generally between 30%–50% while the 12-month prevalence of activity limiting pain is estimated to 2%–14%.Citation4–Citation6 Prevalent chronic pain conditions in the population are: neck–shoulder pain, including chronic trapezius myalgia (10%–20%);Citation7 chronic whiplash-associated disorders (1.5%);Citation8 and chronic widespread pain (5%–10%).Citation9 The prevalence of fibromyalgia syndrome (FMS) – a subgroup of chronic widespread pain – is 1%–4%.Citation10 Chronic masticatory muscle pain has a prevalence of approximately 10% in the population, with two-thirds being women.
Patients with these pain conditions describe widespread negative consequences: significant pain intensity; depressive symptoms; weakness; sleep-related problems; sick-leave; loss of enjoyment of life in general; and decreased emotional well-being, etc.Citation11–Citation13 Years lived with disability is a measure of nonfatal health outcomes from diseases and injuries. Pain conditions caused 21% of the years with disability globally.Citation14 Low back pain was the leading single cause for years lived with disability, followed by major depressive disorder, iron deficiency anemia, and neck pain.Citation14
Biopsychosocial model of pain
Acute and chronic pain is influenced by and interacts with physical, emotional, psychological, and social factors, and a biopsychosocial framework is increasingly applied in clinical practice.Citation15–Citation18 The biopsychosocial framework is seen as increasing the potential for developing better treatments and interventions. However, assessment procedures based on the activated neurobiological pain mechanisms are still lacking (ie, the bio part of the biopsychosocial model of pain); these are necessary to further optimize improvements for patients with chronic pain.
Diagnoses of chronic pain conditions
In clinical practice, physicians are obliged to classify the pain condition using the International Classification of Diseases, 10th edition (ICD-10). The diagnoses in the field of pain are vague, reflecting mainly duration and time aspects, such as chronic cervicalgia (chronic pain in the neck). Some studies have attempted to standardize criteria for diagnoses according to ICD-10.Citation2 Several authors have called attention to the need for diagnoses based on activated pain mechanisms to improve outcomes of treatments.Citation19,Citation20 To address this need, the first step may be to classify nociceptive, neuropathic, psychogenic, or idiopathic pain even though distinct and validated criteria are lacking, especially for chronic pain.
Generally, chronic muscle pain diagnoses are settled by careful anamnesis and clinical examinations that reveal tender muscle at palpation, corresponding to the reported painful areas. For the diagnostics of chronic masticatory muscle pain, clinicians rely on patient reports, questionnaires, and semi-objective findings. In the Research Diagnostic Criteria for Temporomandibular Disorders, the most recent classification for chronic masticatory muscle pain, there are only two chronic masticatory muscle pain diagnoses – myalgia and myofascial pain with referral.Citation21 The same criteria are used for both diagnoses, but myofascial pain has pain referral as an additional criteria.
The trapezius muscle is often used in morphological, electromyographical, and biochemical studies of myalgia; it is an important clinical structure and is easily accessible for invasive investigations. As trapezius myalgia is not a distinct diagnosis, according to ICD-10, researchers have used various criteria for its definition. Our group has used a standardized process to identify patients with chronic trapezius myalgia.Citation22
The following ICD-10 diagnoses have been used to recruit patients with chronic trapezius myalgia: neck myalgia (M 79.1); cervicalgia (M 54); and cervicobrachial syndrome (M 53.1). If there are other simultaneous diagnoses, patients are excluded from the study. The potential research patients are then examined using a standardized clinical examination, using distinct inclusion and exclusion criteria to identify chronic trapezius myalgia and to exclude other conditions.Citation22 Sometimes, chronic trapezius myalgia is part of a more extensive clinical picture, such as chronic widespread pain and/or FMS.
Chronic whiplash-associated disorders are diagnosed, based upon an anamnesis of trauma and neck pain. The severity is classified using the Quebec Criteria.Citation23 A revised classification system for all types of neck pain conditions has been presented.Citation24 A prominent proportion (40%–50%) of those with acute whiplash-associated disorders will develop a chronic pain condition.Citation25,Citation26
According to the American College of Rheumatology, the definition of chronic widespread pain is pain that is present in the left and right sides of the body, above and below the waist, and in the axial skeleton, all of which have lasted for at least 3 months.Citation27 FMS is a subgroup of chronic widespread pain and, additionally, fulfils certain criteria for widespread hyperalgesia (tender point palpation). Comorbidities are common in chronic widespread pain and FMS.Citation28
Neurobiological alterations in chronic pain
Acute pain results from a complex integrated series of events at peripheral and central levels. Acute pain mechanisms might not necessarily be valid in intermittent or chronic pain. Pace et al classified chronic pain into: 1) nociceptive/inflammatory pain; and 2) neuropathic pain.Citation29 There are also differences in the clinical presentation – eg, with respect to pulse reactions and nausea – of pain located to the skin and to muscles, as pointed out by Mense and Gerwin.Citation30 The present review mainly discusses nociceptive/inflammatory muscle pain. Chronic pain is more complex than acute pain as extensive plastic changes of the pain transmission system can occurCitation31,Citation32 and by the modification of psychological and contextual factors.Citation33–Citation38
According to the taxonomy of the International Association for the Study of Pain, a nociceptor is defined as: “… a high-threshold sensory receptor of the peripheral somatosensory nervous system that is capable of transducing and encoding noxious stimuli.”Citation39 Small diameter, slowly conducting afferent nerve fibers from skeletal muscle, free nerve endings of group III (Aδ), and group IV afferent (C) fibers transmit nociceptive information and have to be excited to elicit pain.Citation40 These nociceptors are sensitive to substances released from tissues subject to various types of damages and deformations.Citation41–Citation43 Nociceptors respond to: single or combinations of stimuli; noxious mechanical stimuli; temperature; and chemical substances, such as H+, serotonin (5-HT), bradykinin (BKN), glutamate, substance P (SP), nerve growth factor (NGF), adenosine triphosphate (ATP), and potassium (K+).Citation42–Citation44 In situations of trauma or inflammation, a combination of substances – the inflammatory “soup” – acts on the nociceptors.Citation44 The nociceptor is not a static detector as plastic changes can occur, such as peripheral sensitization.Citation41 A sensitized nociceptor has a lowered threshold for activation and can thus be activated by stimuli that are normally innocuous.Citation42,Citation43 According to mainly animal studies, H+, nitrogen oxide (NO), K+, ATP, NGF, tumor necrosis factor alpha (TNF-α), interleukin 6 (IL-6), prostaglandin E2 (PGE2), and glutamate are involved in the process of peripheral sensitization.Citation43–Citation45 Thus, several substances appear to have both algesic and sensitization effects, eg, 5-HT, glutamate, and K+.
Studies also report that there are substances with anti-inflammatory roles, eg, certain cytokines (IL-10, IL-4, IL-13, and IL-1 receptor antagonists), fatty acid metabolites (eg, prostaglandins, leukotoxins, resolvins, protectines, endocannabinoids, and N-acylethanolamines [NAEs]) and endogenous opioids.Citation46–Citation51 The algesic and sensitizing substances act on specific receptors of the nociceptors, eg, G protein-coupled receptors, receptor tyrosine kinases, and ionotropic receptors/ion channels.Citation52 Sensitization can be accompanied by an increase in the sensitive area.Citation42 Activation of silent nociceptors has also been reported.Citation53 Possibly nociceptors, due to induced gene transcription and protein synthesis, can drive pain in the absence of noxious stimuli.Citation41 In this review, we will focus on the biochemical muscle alterations associated with chronic muscle pain.
The impulses in the nociceptors are conveyed to second order neurons in the spinal medulla.Citation54–Citation56 At spinal level, the signal may be modulated, either amplified or attenuated, by different interneuronal pathways. If an adequate excitation of the second-order neuron occurs, the input will be transmitted to different areas of the central nervous system. Different tracts of the spinal cord have the ability to transmit nociceptive information to the central nervous system.Citation54
Different structures in the brain – the pain matrixCitation57–Citation59 – are dynamically involved in processing the nociception and perception of pain.Citation60 Important areas of pain matrix appear to be anterior cingulate cortex, medial cingulate cortex, insula, prefrontal cortex, and primary and secondary somatosensory cortex (S2). In patients with chronic pain conditions, alterations in connectivity, morphological, and biochemical changes in the pain matrix have been reported.Citation61–Citation64 The activation of glia cells and neuroglial interactions are now also emerging as mechanisms associated with chronic pain.Citation65
Descending supraspinal control of the spinal nociception originates from several brain regions,Citation60,Citation66 and this control can be altered due to behavioral, emotional, and pathological states.Citation32,Citation37,Citation60,Citation66–Citation69 A facilitating shift of the descending system has been reported for patients with persistent pain.Citation32,Citation37,Citation66–Citation70 Alterations in the regulation and activation of inhibitory substances, eg, endorphins, gamma-aminobutyric acid, endocannabinoids, and related substances (eg, NAEs), may also contribute to disturbances in pain inhibition. Due to the above and other processes, patients with chronic pain show a clinical picture associated with signs of hyperexcitability (central sensitization) to nociception and other stimuli. One consequence of central sensitization is that the central nervous system can change pain – eg, amplification, duration, degree, and spatial extent – so that pain no longer directly reflects the peripheral noxious situation.Citation71
Several authors have suggested that chronic pain conditions and, in particular, FMS can be driven by the above briefly described alterations in the central nervous system with little or no peripheral stimuli or nociception.Citation72–Citation74 Other authors have presented data indicating that central alterations are driven by peripheral alterations and nociceptive input.Citation71,Citation75–Citation77
Microdialysis technique
Pain is a subjective experience and semi-objective methods like muscle palpation or assessment of pressure pain thresholds have limited sensitivity and often do not correlate with pain intensity.Citation78 Microdialysis offers a potential in vivo method for studying local tissue alterations before the substances of interest are diluted and cleared by the circulatory system. The technique allows for continuous sampling of substances in the interstitium of the muscle. It has recently been pointed out that the extracellular matrix plays a key role in physiologic functions of cells, including the primary afferent nociceptor.Citation79 The trapezius, masseter, vastus lateralis, and gastrocnemius muscles have been investigated in humans with chronic muscle pain conditions. The present review mainly concerns the results of microdialysis studies and how they can contribute to the understanding of activated peripheral nociceptive and pain mechanisms in humans with chronic pain.
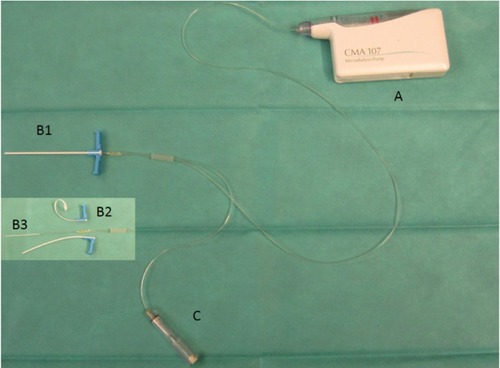
The technique is performed in awake subjects and has been described in detail elsewhere.Citation80–Citation82 Briefly, the skin and the subcutaneous tissues above the muscle under investigation are anesthetized with a local injection (eg, 0.5 mL of Xylocaine® [20 mg/mL]) without adrenaline, and care is taken not to anesthetize the underlying muscle. Thereafter, a thin catheter is implanted in the muscle tissue and slowly perfused with a solution (perfusate) via an infusion pump (). The microdialysis catheter consists of a hollow cannula to which the tip (a semi-permeable dialysis membrane) is attached. During the perfusion molecules in the extracellular space diffuse passively across the membrane and may be collected at the outlet of the microdialysis catheter.Citation82 This fluid, labeled the dialysate, reflects the composition of the extracellular space.
Figure 1 Microdialysis catheter.
To determine the concentrations of small molecules (eg, lactate, pyruvate, glutamate, and glucose), a catheter with a 20 kDa cut-off is suitable while a catheter with a 100 kDa cut-off is preferred for determination of larger molecules.Citation83 Factors that can affect the concentration (recovery) of a substance in the dialysate are: the flow rate; the diffusion rate through the tissue; the area and weight cut-off of the dialysis membrane; and the composition of the perfusate. A low flow rate results in higher relative recovery while a high flow rate results in lower relative recovery. At a very low flow (ie, 0.3 μL/minute), the recovery is near 100%. Detailed descriptions of relative recovery (RR) can be found elsewhere.Citation81,Citation82,Citation84 Adding dextran or albumin to the perfusate can enhance RR for charged molecules, such as peptides and cytokines. Nutritive muscle blood flow can be estimated by the microdialysis ethanol technique using 3H2O instead of ethanol.Citation85,Citation86 The ratio of 3H2O in the dialysate and the perfusate (the outflow-to-inflow ratio) varies inversely with the local blood flow in the tissue.Citation85,Citation86 The small volumes of dialysate obtained require both analytical capacity in small volumes and a predetermination of the substances of interest.
Aim
The primary aim is to review molecular studies using microdialysis for the investigation of human chronic muscle pain, ie, chronic trapezius myalgia, chronic masticatory muscle pain, and chronic widespread pain/FMS.
Methods
Criteria for inclusion and exclusion
We have included studies that focused on chronic pain conditions affecting trapezius and masticatory muscles. To be included, the studies had to use microdialysis and had to investigate at least one patient group and one healthy control group. In the present study, we mainly have reported studies with respect to baseline differences between patient groups and control groups.
Search strategy
We have used the following search strategy in PubMed – ([muscle OR pain] AND microdialysis) OR (muscle AND pain AND induced) AND (Humans[MeSH] AND (Clinical Trial[ptyp] OR meta-analysis[ptyp] OR Review[ptyp]) AND English[lang] AND adult[MeSH] AND “last 10 years”[PDat]).Citation81 From this search, the titles and abstracts were scrutinized. If the articles were relevant and necessary, they were read for further evaluation. We also checked reference lists of these articles and included relevant articles.
Results
lists and briefly describes some characteristics for the included studies. Different types of molecules have been investigated – algesic and inflammatory and metabolic and antinociceptive substances. From the studies in , it has been concluded that an overwhelming proportion of subjects are women. Most studies have investigated the trapezius muscle in local/regional or widespread pain conditions.
Table 1 Studies of chronic myalgia in humans sorted after muscle investigated
Algesic and inflammatory substances
Chronic masseter myalgia
In myofascial temporomandibular disorders, significantly higher glutamate levels were found in the patient group.Citation87
Chronic trapezius myalgia
Two out of three studies have reported increased interstitial muscle concentration of glutamate in the trapezius muscle.Citation22,Citation88,Citation89 The study that did not report any differenceCitation88 was markedly smaller than the two other studies,Citation22,Citation89 which may indicate a power problem.
The interstitial muscle concentration of 5-HT in the trapezius was significantly increased in all studies investigating this substance in chronic trapezius myalgia.Citation22,Citation89–Citation92
Increased levels of BKN in myofascial pain patients with active trigger points have been reported; the levels were higher in the trapezius (with pain) than in a pain-free distant muscle.Citation90,Citation91 It should be noted that these studies were small. Two larger studies could not confirm their results.Citation89,Citation93 In the latter studies, the authors did not investigate active trigger points in the trapezius.
Interstitial levels of kallidin (KAL) have only been investigated in one study and significantly higher levels were found in chronic trapezius myalgia.Citation93
No consistent pattern has been reported for the levels of K+ in chronic trapezius myalgia.Citation89,Citation94,Citation95
SP and calcitonin gene-related peptide (CGRP) concentrations were increased in active trigger points in the trapezius, and these levels were higher in the aching trapezius than in a distant pain-free muscle.Citation90,Citation91
The two trapezius muscle studies investigating PGE2 found no increases,Citation88,Citation96,Citation97 but one of the studies was small,Citation88 and the other study may have had methodological problems due to the fact that the authors did not compensate for the relative recovery.Citation96,Citation97
Several studies of chronic trapezius myalgia have investigated cytokines, but the largest studies have not found elevated levels of cytokines.Citation89,Citation95 Shah et al found significant differences of cytokines for active trigger points.Citation90,Citation91 These authors also have compared the levels of cytokines in the myalgic trapezius (trigger points) with a muscle without pain and found higher levels in the aching muscle. These studies, however, have very small sample sizes.
Chronic whiplash-associated disorders
To our best knowledge, only one cohort of patients with chronic whiplash-associated disorders has been investigated and presented in two studies.Citation93,Citation98 The 5-HT and IL-6 were significantly higher in chronic whiplash-associated disorders than in controls.Citation98 No group differences were found in the concentrations of K+, glutamate, BKN, or KAL.Citation93,Citation98
FMS
FMS had increased 5-HT levels and leukotriene B4 (LTB4) levels in the masseter muscle.Citation99,Citation100
Metabolic substances and blood flow
Chronic trapezius myalgia
Most studies concerning chronic trapezius myalgia reported increases in the interstitial concentrations of lactate.Citation22,Citation89,Citation94,Citation96,Citation97 Methodological problems may exist in the studies conducted by Flodgren et alCitation96,Citation97 with respect to relative recovery as mentioned previously.Citation81
Also, for pyruvate, a majority of chronic trapezius myalgia studies found increased interstitial concentrations of pyruvate.Citation22,Citation89,Citation94,Citation96,Citation97 Two studies found no significant group differences for pyruvate.Citation96,Citation97
Chronic whiplash-associated disorders
No significant alterations were found in the interstitial concentrations of lactate and pyruvate of the trapezius muscle in patients with chronic whiplash-associated disorders.Citation98
Chronic widespread pain including FMS
Three studies investigated chronic widespread pain/FMS patients with respect to metabolic substances. The vastus lateralis muscle – not reported if painful at rest or with altered local pain thresholds – was investigated in patients with FMS, and no differences in concentrations of lactate compared to controls were found.Citation101 Two larger studies have investigated the trapezius muscle in chronic widespread pain/FMS.Citation102,Citation103 In the first study, significantly higher interstitial concentrations of lactate and pyruvate were found,Citation102 while the other study reported significantly increased interstitial muscle concentrations of lactate in chronic widespread pain patients.Citation103 The latter study also investigated concentrations of glucose and glycerol, but no group differences were found. Hence, the metabolic studies indicate alterations in lactate metabolism in the trapezius with chronic widespread pain/FMS.
Blood flow in chronic myalgia
Despite most chronic trapezius myalgia studies reporting significant increases in lactate, there is not a consistent picture with respect to blood flow in this pain condition or in chronic widespread pain/FMS using the microdialysis technique.Citation22,Citation89,Citation94,Citation103
Antinociceptive substances
Few studies have targeted muscle levels of pain-inhibitory signalling molecules. The N-acylethanolamines (NAEs) is a family of endogenous lipid mediators that are involved in the regulation of inflammation and pain.Citation49 The most thoroughly investigated of the NAEs is N-arachidonoylethanolamine (anandamide [AEA]), which interacts with cannabinoid receptors and also can target transient receptor potential (vanilloid-1) receptors. Other examples of NAEs are N-palmitoylethanolamine (PEA), N-stearoylethanolamine (SEA), and N-oleoylethanolamine. Two studies have investigated the interstitial muscle levels of NAEs and reported increased levels of SEA and PEA in chronic trapezius myalgia compared to controls.Citation104,Citation105 The results for chronic widespread pain indicated alterations in mobilization of PEA and SEA as a consequence of exercise compared to controls.Citation105 Hence, patients with chronic neck pain showed significantly higher levels of these substances postexercise than patients with chronic widespread pain.
Omics methods for analyzing biochemical milieu of muscle interstitium
Recently, microdialysis studies have applied omics methods to investigate the interstitium of human myalgic muscle. Both proteomic and metabolomics studies have been published indicating that these methods can be used to identify new interesting substances and processes associated with chronic myalgia.Citation106,Citation107 The proteomic study found that prominent proportions of the 97 identified proteins were at least two-fold higher or lower in chronic trapezius myalgia and in chronic widespread pain (50% and 30%, respectively).Citation106 Several of the identified proteins are known to be involved in nociceptive/inflammatory processes, eg, creatine kinase, NGF, carbonic anhydrase, myoglobin, fatty acid binding protein, and actin aortic smooth muscle.
Discussion
Important conclusions based on the identified studies were:
Several studies of local/regional muscle pain conditions indicated that 5-HT, glutamate, lactate, and pyruvate were increased in patients with chronic myalgia.
Studies of chronic widespread pain/FMS have reported peripheral muscle alterations in 5-HT and lactate.
Other investigated substances have only been reported in single studies or with conflicting results.
5-HT
All studies investigating 5-HT () found significantly increased levels of this substance in the whole spectrum of severity of chronic trapezius myalgia, including chronic whiplash-associated disorders and in chronic masticatory muscle pain. The 5-HT is involved both in central and peripheral processes of nociception and hyperalgesia.Citation108 Whether 5-HT has an analgesic or hyperalgesic action depends on the cell type and the type of receptor it targets. In the periphery, 5-HT is released from platelets and mast cells due to tissue damage,Citation42 and it sensitizes afferent nerve fibers.Citation108–Citation111 The intramuscular administration of 5-HT into human muscle induces pain.Citation112 There are several receptor classes and subclasses of 5-HT and especially the 5-HT3 receptor has attracted interest. But also 5-HT1, 5-HT2, and 5-HT7 have been discussed with respect to myalgia. In conclusion, the available microdialysis studies of chronic myalgia indicate that 5-HT is involved in chronic muscle pain.
Glutamate
Glutamate, a pain modulator in the human central nervous system, acts via the N-methyl-D-aspartate (NMDA), 2-amino-3-(3-hydroxy-5-methyl-isoxazol-4-yl) propanoic acid (AMPA), and kainate receptorsCitation113–Citation115 and appears to influence peripheral pain processing.Citation116–Citation123 These receptors are also present on peripheral nerve terminals. Glutamate is released from peripheral afferent nerve terminals.Citation124 Injections of glutamate increase pain intensity.Citation120,Citation125
Three studies of chronic myalgia reported significantly higher interstitial concentrations of glutamate,Citation22,Citation87,Citation89 while a fourth small study found no significant group difference.Citation88 A possible difference between subjects of these studies may contribute to the inconsistent glutamate finding. Pain history, present pain, and clinical muscular neck status of the subjects were sparsely presented in the fourth study.Citation88 It has been suggested that the elevation of interstitial muscle glutamate alters pain sensitivity in healthy humans and is associated with pain symptoms in some chronic noninflammatory muscle pain conditions.Citation126 The available microdialysis studies mainly support the conclusions of that review.
Interstitial concentrations of glutamate were not increased in the trapezius of chronic whiplash-associated disorders.Citation98 Conflicting results with respect to glutamate have been reported in patients with chronic widespread pain/FMS.Citation102,Citation103 One difference between chronic trapezius myalgia and the two other conditions might be the more widespread hyperalgesia in chronic whiplash-associated disorders and chronic widespread pain/FMS.Citation127
Lactate and pyruvate
The majority of studies concerning chronic trapezius myalgia have reported increases in the metabolites lactate and pyruvate. Often-suggested explanations for the higher concentration of lactate are insufficient oxygen supply and anaerobic conditions, but there is not a consistent picture with respect to blood flow in this pain condition or in chronic widespread pain/FMS using microdialysis or other techniques.Citation22,Citation89,Citation94,Citation103,Citation128–Citation130 Reduction in tissue oxygenation in FMSCitation131 and in chronic trapezius myalgiaCitation132 may result in higher pyruvate and higher lactate concentrations, due to a shift toward an anaerobic state. Hence, alterations in oxygen supply cannot be excluded as a factor of importance, but other factors can also contribute, eg, decreased fitness level, increased muscle activation, and/or damaged mitochondria. Changes in the lactate-pyruvate metabolism may result in higher pyruvate levels.Citation133 A lower fitness level is another explanation as this means more frequent reliance on anaerobic metabolism. However, it is unknown if a general deconditioning in the two pain conditions of chronic trapezius myalgia and chronic widespread pain/FMS involves the postural trapezius. The aerobic capacity of a muscle is largely determined by the number of mitochondria and their enzymes.Citation134 The mitochondrial density increases as a result of exercise, and an increased density results in enhanced aerobic capacity.Citation135 Both in FMS and chronic trapezius myalgia, the trapezius muscle fibers can appear with alterations in mitochondrial content and distribution.Citation131,Citation132,Citation136,Citation137
Lactate participates in the detection of exercise stress before tissue damage occurs and can be exchanged rapidly among tissue compartments where it may be oxidized as a fuel or reconverted to form pyruvate or glucose.Citation138–Citation140 Lactic acid is dissociated at body pH.Citation141 Inflamed as well as ischemic tissues show lowered pH.Citation142,Citation143 Acid-sensing ion channels (ASIC) are considered transducers for nociception and mechanosensation.Citation138 Lactate appears to facilitate the response of acid-sensing ion channels-3 (ASIC-3) to low pH.Citation138 Lactate exposure leads to reactive oxygen species (ROS) generation and can be harmful or beneficial, depending on the level or persistence of ROS.Citation144–Citation146 Hence, one possibility is that the increased lactate induces, eg, ROS, which directly interacts with the nociceptive system or, in turn, activates the algesics.Citation147 Other possible receptors for low pH are transient receptor potential cation channel subfamily V member 1 (TRPV1), transient receptor potential cation channel subfamily V member 4 (TRPV4), short transient receptor potential channel 4 (TRPC4) and short transient receptor potential channel 5 (TRPC5).Citation142,Citation143,Citation148
To summarize, most studies of myalgic trapezius muscles show significant increases in interstitial levels of lactate and pyruvate.
Conflicting or inconclusive results for other investigated substances
SP and CGRP
Two small studies of active trigger points of myofascial pain reported significant increases in SP and CGRP.Citation90,Citation91 Both SP and CGRP are involved as mediators of neurogenic inflammation and hyperalgesia.Citation149 SP stimulation can result in the production of inflammatory mediators and proinflam-matory cytokines,Citation149,Citation150 which – in turn – can stimulate the production of SP.Citation151 More studies investigating the peripheral roles of SP and CGRP in chronic myalgia are needed.
K+
When reviewing the literature, no consistent pattern of increased K+ was found in patients with chronic trapezius myalgiaCitation89,Citation94,Citation95 or with chronic whiplash-associated disorders. Increased interstitial K+ levels may be related to muscle pain.Citation152 In acute tissue trauma, K+ is a component of the “inflammatory soup” and is characterized as an algesic substance.Citation153 The role of K+ in chronic myalgia pain is unclear at the moment.
BKN and KAL
BKN and KAL are kinins that are produced by the kallikrein-mediated enzymatic cleavage of kininogen.Citation43,Citation154,Citation155 The two kinins have been suggested as algesic kinins involved in muscle pain. Animal studies have shown that BKN can have both algogenic and sensitizing functions with respect to the nociceptors.Citation154,Citation156 Four studies investigating the interstitial concentrations of BKN and/or KAL were found.Citation89–Citation91,Citation93 The difference in results with respect to BKN among these studies could be because the alterations in BKN might be very localized, ie, in the trigger points,Citation90,Citation91 and not generally found in the aching trapezius muscle.Citation89,Citation93 KAL was only investigated in one study and increased in chronic trapezius myalgia but not in the trapezius of chronic whiplash-associated disorders.Citation93 Clearly, more pathophysiological in vivo studies are necessary to understand the roles of BKN and KAL for nociception and pain in patients with chronic muscle pain.
Prostaglandins and leukotrienes
Eicosanoids are substances produced in various cell types in response to tissue trauma by the breakdown of arachidonic acid in the cell wall, leading to the formation of prostaglandins and leukotrienes. Both these substances are suggested as potential pain mediators in chronic myalgia. PGE2 has been of particular interest for inflammatory pain and in delayed onset muscle soreness. The probable role of PGE2 is as a sensitizer of nociceptors. However, we only found two studies investigating this substance in chronic myalgia and neither found increased levels.Citation96,Citation100 In patients with FMS, one study reported significantly elevated levels of LTB4 in the masseter muscle.Citation100 In conclusion, the roles of prostaglandins and leukotrienes in chronic myalgia are unclear; more studies of these substances may be needed.
Cytokines
Several direct and indirect pathways link cytokines with nociception and hyperalgesia.Citation43,Citation157,Citation158 Four studies investigated cytokines in chronic trapezius myalgia, but significant differences were only found for active trigger points.Citation90,Citation91 Larger studies have not found elevated levels of cytokines.Citation89,Citation95 The latter studies might have had technical problems due to the catheters used. On the other hand, increased IL-6 was found in the chronic whiplash-associated disorders study using the same type of custom-made catheters.Citation98 The study by Helmy et al indicates the need to carefully review methodology aspects when determining the levels of cytokines.Citation159
NAEs
Knowledge about peripheral antinociceptive processes in human chronic myalgia is very insufficient. Two studies, partly using the same subjects, found significant increases in two NAEs in the chronic trapezius myalgia and alterations in the mobilization of these two substances in chronic widespread pain.Citation104,Citation105 Larger studies also focusing on other NAEs and other myalgic muscles are necessary before any definite conclusions can be drawn with respect to chronic myalgia.
Future perspectives
Several of the microdialysis studies identified in the present review have few subjects, which entails the risk of low power and inconclusive results. Results also need to be confirmed by independent groups to be valid. Patient cohorts need to be better characterized with respect to inclusion and exclusion criteria, diagnoses and their criteria, pain severity, psychological stress, work participation, and sick leave. There is also a need to better characterize the physical fitness level of the subject and, if possible, the daily activity pattern of the investigated muscle, eg, with respect to working tasks. A global measure of the severity of the investigated pain condition can be an advantage when comparing studies.
The subjects of microdialysis studies are nearly exclusively women, which reasonably is a consequence of the higher prevalence of the most chronic myalgias in women. Hence, future studies ought to include men and compare mediator levels between sexes.
Another factor to consider may be diurnal variations in some biomarker levels, which should be controlled for by taking samples at the same time of the day. Tissue fluid levels of biomarkers may also be influenced by factors such as age, sex, menstrual cycle, food intake, and body mass, which must be considered in future studies.
Reasonably, a number of substances can be released and altered in the milieus of the nociceptors. Only a limited number of substances have been investigated using the microdialysis technique and are reviewed in the present review. Hence, other substances could be of importance for the genesis and maintenance of chronic muscle pain. Even though there are a few studies concerning NAEs and endocannabinoids there is a surprising gap concerning more well-known inhibitory endogenous substances such as opioids. There is also a lack of studies concerning anti-inflammatory cytokines and other fatty acid metabolites, eg, prostaglandins, leukotoxins, resolvins, and protectins. Hitherto, the limited volumes of dialysate obtained have made it impossible to analyze more than certain single biomarkers. The development of more sensitive methods that can combine analyses of several pain-related substances will probably improve knowledge about peripheral mechanisms behind chronic myalgia. Methods from the omics field using nano liquid chromatography or capillary electrophoresis in combination with mass spectrometry may be important tools to understand the complex relationship of the substances involved in chronic myalgia. Pain research will increasingly turn to this powerful technology that could hopefully provide novel and exciting insights in the field.
The development of omics methods also emphasizes the need to use multivariate data analysis. The omics methods are capable of measuring hundreds or even thousands of substances simultaneously. Traditional statistical methods assume markedly higher numbers of subjects than dependent variables, but the omics methods produce the opposite, ie, markedly more dependent and intercorrelated variables than subjects. Hence, using partial least squares regression analyses, cluster analysis, and principal component analysis may represent a complementary approach to the traditional statistical methods for a better understanding of the complex biochemical alterations that may occur in chronic musculosk-eletal pain and when sensitization processes may be present in the group with myalgia but not in healthy controls. In future larger studies, it is important to investigate group differences. These studies also need to consider that when comparing a muscle with chronically sensitized nociceptors with a healthy muscle, no group differences may exist for a substance – even though correlations may exist between the substance under consideration and habitual pain intensities and pain thresholds in the patient group.
Conclusion
After reviewing the literature, it can be concluded that several studies clearly show elevated levels of 5-HT, glutamate, lactate, and pyruvate in localized chronic myalgias. Several alterations in metabolites and algesics have been reported in chronic widespread pain/FMS, but more studies using different designs of the microdialysis sessions are needed before more definite conclusions can be drawn about the interstitial muscle milieu in these pain conditions. For other substances, results are inconclusive across studies and patient groups.
Acknowledgments
No financial or personal relationships have inappropriately influenced this work. This study was supported by: the Swedish Council for Working Life and Social Research (2010-0683, 2007-0760); the Swedish Research Council (2010-2893); the Swedish Rheumatism Association; the Swedish Dental Association; the Karolinska Institutet; and Linköping University. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- BreivikHCollettBVentafriddaVCohenRGallacherDSurvey of chronic pain in Europe: prevalence, impact on daily life, and treatmentEur J Pain200610428733316095934
- LarssonBSøgaardKRosendalLWork related neck-shoulder pain: a review on magnitude, risk factors, biochemical characteristics, clinical picture and preventive interventionsBest Pract Res Clin Rheumatol200721344746317602993
- GerdleBBjörkJHenrikssonCBengtssonAPrevalence of current and chronic pain and their influences upon work and healthcare-seeking: a population studyJ Rheumatol20043171399140615229963
- CôtéPvan der VeldeGCassidyJDBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersThe burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersSpine (Phila Pa 1976)200833Suppl 4S60S7418204402
- CroftPRLewisMPapageorgiouACRisk factors for neck pain: a longitudinal study in the general populationPain200193331732511514090
- Hogg-JohnsonSvan der VeldeGCarrollLJBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersThe burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersSpine (Phila Pa 1976)200833Suppl 4S39S5118204398
- LidgrenLPreface: neck pain and the decade of the bone and joint 2000–2010J Manipulative Physiol Ther200932Suppl 2S2S319251065
- GuezMHildingssonCNilssonMToolanenGThe prevalence of neck pain: a population-based study from northern SwedenActa Orthop Scand200273445545912358121
- GerdleBBjörkJCösterLHenrikssonKHenrikssonCBengtssonAPrevalence of widespread pain and associations with work status: a population studyBMC Musculoskelet Disord2008910218627605
- JesusCAFederDPeresMFThe role of vitamin D in pathophysiology and treatment of fibromyalgiaCurr Pain Headache Rep201317835523801008
- CasarettDKarlawishJSankarPHirschmanKAschDADesigning pain research from the patient’s perspective: what trial end points are important to patients with chronic pain?Pain Med20012430931615102235
- RobinsonMEBrownJLGeorgeSZMultidimensional success criteria and expectations for treatment of chronic pain: the patient perspectivePain Med20056533634516266354
- TurkDCDworkinRHRevickiDIdentifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with painPain2008137227628517937976
- VosTFlaxmanADNaghaviMYears lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010Lancet201238098592163219623245607
- DworkinRHTurkDCFarrarJTIMMPACTCore outcome measures for chronic pain clinical trials: IMMPACT recommendationsPain20051131–291915621359
- World Health OrganizationInternational Classification of Functioning, Disability and HealthGenevaWorld Health Organization2001 Available from: http://www.disabilitaincifre.it/documenti/ICF_18.pdfAccessed September 10, 2103
- WaddellG1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back painSpine (Phila Pa 1976)19871276326442961080
- PincusTKentPBronfortGLoiselPPranskyGHartvigsenJTwenty-five years with the biopsychosocial model of low back pain-is it time to celebrate? A report from the twelfth international forum for primary care research on low back painSpine (Phila Pa 1976)201338242118212323970112
- MaxMBTowards physiologically based treatment of patients with neuropathic painPain19904221311371701044
- WoolfCJBennettGJDohertyMTowards a mechanism-based classification of pain?Pain19987732272299808347
- OhrbachRGonzalezYListTMichelottiASchiffmanEDiagnostic Criteria for Temporomandibular Disorders (DC/TMD). Clinical Examination ProtocolInternational RDC-TMD Consortium2013 Available from: http://www.rdc-tmdinternational.org/Portals/18/protocol_DC-TMD/DC-TMD%20Protocol%20-%202013_06_02.pdfInternational Research Diagnostic Criteria for Temporomandibular Disorders Consortium Network2014Accessed September 10, 2103
- RosendalLLarssonBKristiansenJIncrease in muscle nociceptive substances and anaerobic metabolism in patients with trapezius myalgia: microdialysis in rest and during exercisePain2004112332433415561388
- SpitzerWOSkovronMLSalmiLRScientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its managementSpine (Phila Pa 1976)199520Suppl 81S73S7604354
- GuzmanJHurwitzELCarrollLJBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersA new conceptual model of neck pain: linking onset, course, and care: the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersSpine (Phila Pa 1976)200833Suppl 4S14S2318204387
- CarrollLJHolmLWHogg-JohnsonSBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersCourse and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersSpine (Phila Pa 1976)200833Suppl 4S83S9218204405
- KamperSJRebbeckTJMaherCGMcAuleyJHSterlingMCourse and prognostic factors of whiplash: a systematic review and meta-analysisPain2008138361762918407412
- WolfeFSmytheHAYunusMBThe American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria CommitteeArthritis Rheum19903321601722306288
- KatoKSullivanPFEvengårdBPedersenNLChronic widespread pain and its comorbidities: a population-based studyArch Intern Med2006166151649165416908799
- PaceMCMazzarielloLPassavantiMBSansonePBarbarisiMAurilioCNeurobiology of painJ Cell Physiol2006209181216741973
- MenseSGerwinRDMuscle pain versus skin painMenseSGerwinRMuscle Pain: Understanding the MechanismsBerlinSpringer2010812
- ReichlingDBLevineJDCritical role of nociceptor plasticity in chronic painTrends Neurosci2009321261161819781793
- KunerRCentral mechanisms of pathological painNat Med201016111258126620948531
- GrachevIDFredricksonBEApkarianAVAbnormal brain chemistry in chronic back pain: an in vivo proton magnetic resonance spectroscopy studyPain200089171811113288
- WoolfCJSalterMWNeuronal plasticity: increasing the gain in painScience200028854721765176910846153
- HuntSPMantyhPWUnderstanding the neurobiology of chronic pain: molecular and cellular biologyGiamberardinoMAPain 2002 – An updated Review: Refresher Course SyllabusSeattleIASP Press2002237247
- Petersen-FelixSCuratoloMNeuroplasticity – an important factor in acute and chronic painSwiss Med Wkly200213221–2227327812362284
- Wilder-SmithOHTassonyiEArendt-NielsenLPreoperative back pain is associated with diverse manifestations of central neuroplasticityPain200297318919412044615
- Schmidt-WilckeTVariations in brain volume and regional morphology associated with chronic painCurr Rheumatol Rep200810646747419007538
- International Association for the Study of Pain [homepage on the Internet]IASP Taxonomy1994 [updated May 22, 2012]. Available from: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698Accessed September 10, 2103
- MenseSThe pathogenesis of muscle painCurr Pain Headache Rep20037641942514604500
- WoolfCJMaQNociceptors – noxious stimulus detectorsNeuron200755335336417678850
- MenseSNociception from skeletal muscle in relation to clinical muscle painPain19935432412898233542
- CoutauxAAdamFWillerJCLe BarsDHyperalgesia and allodynia: peripheral mechanismsJoint Bone Spine200572535937116214069
- MenseSAlgesic agents exciting muscle nociceptorsExp Brain Res200919618910019139871
- MominAMcNaughtonPARegulation of firing frequency in nociceptive neurons by pro-inflammatory mediatorsExp Brain Res20091961455219350231
- CunhaJMCunhaFQPooleSFerreiraSHCytokine-mediated inflammatory hyperalgesia limited by interleukin-1 receptor antagonistBr J Pharmacol200013061418142410903985
- PooleSCunhaFQSelkirkSLorenzettiBBFerreiraSHCytokine-mediated inflammatory hyperalgesia limited by interleukin-10Br J Pharmacol199511546846887582491
- VerriWAJrCunhaTMParadaCAPooleSCunhaFQFerreiraSHHypernociceptive role of cytokines and chemokines: targets for analgesic drug development?Pharmacol Ther2006112111613816730375
- PacherPBátkaiSKunosGThe endocannabinoid system as an emerging target of pharmacotherapyPharmacol Rev200658338946216968947
- PiomelliDSassoOPeripheral gating of pain signals by endogenous lipid mediatorsNat Neurosci201417216417424473264
- SerhanCNPetasisNAResolvins and protectins in inflammation resolutionChem Rev2011111105922594321766791
- LinleyJERoseKOoiLGamperNUnderstanding inflammatory pain: ion channels contributing to acute and chronic nociceptionPflugers Arch2010459565766920162302
- SchaibleHGRichterFEbersbergerAJoint painExp Brain Res2009196115316219363606
- AlmeidaTFRoizenblattSTufikSAfferent pain pathways: a neuroanatomical reviewBrain Res200410001–2405615053950
- JiRRKohnoTMooreKAWoolfCJCentral sensitization and LTP: do pain and memory share similar mechanisms?Trends Neurosci2003261269670514624855
- GangadharanVKunerRPain hypersensitivity mechanisms at a glanceDis Model Mech20136488989523828645
- LeeMCTraceyIUnravelling the mystery of pain, suffering, and relief with brain imagingCurr Pain Headache Rep201014212413120425201
- LegrainVIannettiGDPlaghkiLMourauxAThe pain matrix reloaded: a salience detection system for the bodyProg Neurobiol201193111112421040755
- IannettiGDMourauxAFrom the neuromatrix to the pain matrix (and back)Exp Brain Res2010205111220607220
- OssipovMHDussorGOPorrecaFCentral modulation of painJ Clin Invest2010120113779378721041960
- SchweinhardtPBushnellMCPain imaging in health and disease – how far have we come?J Clin Invest2010120113788379721041961
- ApkarianAVPain perception in relation to emotional learningCurr Opin Neurobiol200818446446818835354
- BalikiMNSchnitzerTJBauerWRApkarianAVBrain morphological signatures for chronic PainPLoS One2011610e2601022022493
- NapadowVKimJClauwDJHarrisREDecreased intrinsic brain connectivity is associated with reduced clinical pain in fibromyalgiaArthritis Rheum20126472398240322294427
- JiRRBertaTNedergaardMGlia and pain: is chronic pain a gliopathy?Pain2013154Suppl 1S10S2823792284
- HeinricherMMTavaresILeithJLLumbBMDescending control of nociception: Specificity, recruitment and plasticityBrain Res Rev200960121422519146877
- PorrecaFOssipovMHGebhartGFChronic pain and medullary descending facilitationTrends Neurosci200225631932512086751
- RenKDubnerRDescending modulation in persistent pain: an updatePain20021001–21612435453
- RobinsonDAZhuoMGenetic analysis of pain mechanismsCrit Rev Eukaryot Gene Expr200212427529512641396
- JulienNGoffauxPArsenaultPMarchandSWidespread pain in fibromyalgia is related to a deficit of endogenous pain inhibitionPain20051141–229530215733656
- WoolfCJCentral sensitization: implications for the diagnosis and treatment of painPain2011152Suppl 3S2S1520961685
- BradleyLAPathophysiology of fibromyalgiaAm J Med2009122Suppl 12S22S3019962493
- PeterselDLDrorVCheungRCentral amplification and fibromyalgia: disorder of pain processingJ Neurosci Res2011891293420936697
- SmithHSHarrisRClauwDFibromyalgia: an afferent processing disorder leading to a complex pain generalized syndromePain Physician2011142E217E24521412381
- SchneiderGMSmithADHooperAMinimizing the source of nociception and its concurrent effect on sensory hypersensitivity: an exploratory study in chronic whiplash patientsBMC Musculoskelet Disord2010112920144214
- StaudRNagelSRobinsonMEPriceDDEnhanced central pain processing of fibromyalgia patients is maintained by muscle afferent input: a randomized, double-blind, placebo-controlled studyPain20091451–29610419540671
- StaudRIs it all central sensitization? Role of peripheral tissue nociception in chronic musculoskeletal painCurr Rheumatol Rep201012644845420882373
- WallinMLiedbergGBörsboBGerdleBThermal detection and pain thresholds but not pressure pain thresholds are correlated with psychological factors in women with chronic whiplash-associated painClin J Pain201228321122121750459
- ReichlingDBGreenPGLevineJDThe fundamental unit of pain is the cellPain2013154Suppl 1
- UngerstedtUMicrodialysis – principles and applications for studies in animals and manJ Intern Med199123043653731919432
- GerdleBLarssonBPotential muscle biomarkers of chronic myalgia in humans – a systematic review of microdialysis studiesKhanTKBiomarkerOpen access: InTech2012103132
- ErnbergMGerdleBPeripheral Algesic Substances in Musculoskeletal Pain Assessed by MicrodialysisGraven-NielsenTArendt-NielsenLMusculoskeletal Pain – Basic Mechanisms and ImplicationsIASP Press2014In press
- WaelgaardLPharoATønnessenTIMollnesTEMicrodialysis for monitoring inflammation: efficient recovery of cytokines and anaphylotoxins provided optimal catheter pore size and fluid velocity conditionsScand J Immunol200664334535216918704
- OlaussonPGerdleBGhafouriNKarlssonLLarssonBGhafouriBRelative recovery over time – an in vivo microdialysis study of human skeletal muscleScand J Clin Lab Invest2013731101623088726
- HicknerRCBoneDUngerstedtUJorfeldtLHenrikssonJMuscle blood flow during intermittent exercise: comparison of the microdialysis ethanol technique and 133Xe clearanceClin Sci (Lond)199486115258306547
- StallknechtBDonsmarkMEnevoldsenLHFluckeyJDGalboHEstimation of rat muscle blood flow by microdialysis probes perfused with ethanol, [14C]ethanol, and 3H2OJ Appl Physiol19998631054106110066723
- CastrillonEEErnbergMCairnsBEInterstitial glutamate concentration is elevated in the masseter muscle of myofascial temporomandibular disorder patientsJ Orofac Pain201024435036021197506
- FlodgrenGMCrenshawAGAlfredsonHGlutamate and prostaglandin E2 in the trapezius muscle of female subjects with chronic muscle pain and controls determined by microdialysisEur J Pain20059551151516139179
- LarssonBRosendalLKristiansenJResponses of algesic and metabolic substances to 8 h of repetitive manual work in myalgic human trapezius musclePain2008140347949019006649
- ShahJPDanoffJVDesaiMJBiochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger pointsArch Phys Med Rehabil2008891162318164325
- ShahJPPhillipsTMDanoffJVGerberLHAn in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscleJ Appl Physiol (1985)20059951977198416037403
- GhafouriBLarssonBKSjörsALeanderssonPGerdleBUInterstitial concentration of serotonin is increased in myalgic human trapezius muscle during rest, repetitive work and mental stress – an in vivo microdialysis studyScand J Clin Lab Invest201070747848620712520
- GerdleBHilgenfeldtULarssonBKristiansenJSøgaardKRosendalLBradykinin and kallidin levels in the trapezius muscle in patients with work-related trapezius myalgia, in patients with whiplash associated pain, and in healthy controls – A microdialysis study of womenPain2008139357858718657364
- SjøgaardGRosendalLKristiansenJMuscle oxygenation and glycolysis in females with trapezius myalgia during stress and repetitive work using microdialysis and NIRSEur J Appl Physiol2010108465766919894061
- RosendalLKristiansenJGerdleBIncreased levels of interstitial potassium but normal levels of muscle IL-6 and LDH in patients with trapezius myalgiaPain20051191–320120916297553
- FlodgrenGMCrenshawAGHellströmFFahlströmMCombining microdialysis and near-infrared spectroscopy for studying effects of low-load repetitive work on the intramuscular chemistry in trapezius myalgiaJ Biomed Biotechnol2010201051380320625491
- FlodgrenGMHellströmFBFahlströmMCrenshawAGEffects of 30 versus 60 min of low-load work on intramuscular lactate, pyruvate, glutamate, prostaglandin E(2) and oxygenation in the trapezius muscle of healthy femalesEur J Appl Physiol200697555756516767442
- GerdleBLemmingDKristiansenJLarssonBPeolssonMRosendalLBiochemical alterations in the trapezius muscle of patients with chronic whiplash associated disorders (WAD) – a microdialysis studyEur J Pain2008121829317459742
- ErnbergMHedenberg-MagnussonBAlstergrenPKoppSThe level of serotonin in the superficial masseter muscle in relation to local pain and allodyniaLife Sci199965331332510447217
- Hedenberg-MagnussonBErnbergMAlstergrenPKoppSPain mediation by prostaglandin E2 and leukotriene B4 in the human masseter muscleActa Odontol Scand200159634835511831483
- McIverKLEvansCKrausRMIspasLSciottiVMHicknerRCNO-mediated alterations in skeletal muscle nutritive blood flow and lactate metabolism in fibromyalgiaPain20061201–216116916376018
- GerdleBSoderbergKSalvador PuigvertLRosendalLLarssonBIncreased interstitial concentrations of pyruvate and lactate in the trapezius muscle of patients with fibromyalgia: a microdialysis studyJ Rehabil Med201042767968720603699
- GerdleBLarssonBForsbergFChronic widespread pain: increased glutamate and lactate concentrations in the trapezius muscle and plasmaClin J Pain201430540942023887335
- GhafouriNGhafouriBLarssonBHigh levels of N-palmitoylethanolamide and N-stearoylethanolamide in microdialysate samples from myalgic trapezius muscle in womenPLOS One2011611e2725722125609
- GhafouriNGhafouriBLarssonBStenssonNFowlerCJGerdleBPalmitoylethanolamide and stearoylethanolamide levels in the interstitium of the trapezius muscle of women with chronic widespread pain and chronic neck-shoulder pain correlate with pain intensity and sensitivityPain201315491649165823707281
- OlaussonPGerdleBGhafouriNLarssonBGhafouriBIdentification of proteins from interstitium of trapezius muscle in women with chronic myalgia using microdialysis in combination with proteomicsPLoS One2012712e5256023300707
- HadréviJGhafouriBSjörsAComparative metabolomics of muscle interstitium fluid in human trapezius myalgia: an in vivo microdialysis studyEur J Appl Physiol2013113122977298924078209
- SommerCSerotonin in pain and analgesia: actions in the peripheryMol Neurobiol200430211712515475622
- ErnbergMSerotonergic Receptor involvement in Muscle Pain and HyperalgesiaGraven-NielsenTArendt-NielsenLMenseSFundamentals of Musculoskeltal Pain1st edSeattleIASP Press2008139153
- GiordanoJRogersLVPeripherally administered serotonin 5-HT3 receptor antagonists reduce inflammatory pain in ratsEur J Pharmacol19891701–283862612565
- TaiwoYOLevineJDSerotonin is a directly-acting hyperalgesic agent in the ratNeuroscience19924824854901534874
- ErnbergMHedenberg-MagnussonBKuritaHKoppSEffects of local serotonin administration on pain and microcirculation in the human masseter muscleJ Orofac Pain200620324124816913434
- CoggeshallRECarltonSMReceptor localization in the mammalian dorsal horn and primary afferent neuronsBrain Res Brain Res Rev199724128669233541
- HudspithMJGlutamate: a role in normal brain function, anaesthesia, analgesia and CNS injuryBr J Anaesth19977867317479215028
- QuinteroGCAdvances in cortical modulation of painJ Pain Res2013671372524092997
- CarltonSMPeripheral excitatory amino acidsCurr Opin Pharmacol200111525611712535
- VarneyMAGereauRW4thMetabotropic glutamate receptor involvement in models of acute and persistent pain: prospects for the development of novel analgesicsCurr Drug Targets CNS Neurol Disord20021328329612769620
- CairnsBESessleBJHuJWCharacteristics of glutamate-evoked temporomandibular joint afferent activity in the ratJ Neurophysiol20018562446245411387390
- CairnsBEHuJWArendt-NielsenLSessleBJSvenssonPSex-related differences in human pain and rat afferent discharge evoked by injection of glutamate into the masseter muscleJ Neurophysiol200186278278911495950
- CairnsBEWangKHuJWSessleBJArendt-NielsenLSvenssonPThe effect of glutamate-evoked masseter muscle pain on the human jaw-stretch reflex differs in men and womenJ Orofac Pain200317431732514737876
- SvenssonPCairnsBEWangKGlutamate-evoked pain and mechanical allodynia in the human masseter musclePain2003101322122712583864
- SvenssonPWangKArendt-NielsenLCairnsBESessleBJPain effects of glutamate injections into human jaw or neck musclesJ Orofac Pain200519210911815895833
- TegederLZimmermannJMellerSGeisslingerGRelease of algesic substances in human experimental muscle painInflamm Res200251839340212234056
- MillerKEHoffmanEMSutharshanMSchechterRGlutamate pharmacology and metabolism in peripheral primary afferents: physiological and pathophysiological mechanismsPharmacol Ther2011130328330921276816
- GazeraniPWangKCairnsBESvenssonPArendt-NielsenLEffects of subcutaneous administration of glutamate on pain, sensitization and vasomotor responses in healthy men and womenPain2006124333834816919390
- CairnsBEDongXThe role of peripheral glutamate and glutamate receptors in muscle painJ Musculoskelet Pain2008161–28591
- Arendt-NielsenLGraven-NielsenTCentral sensitization in fibromyalgia and other musculoskeletal disordersCurr Pain Headache Rep20037535536112946288
- ElvinASiösteenAKNilssonAKosekEDecreased muscle blood flow in fibromyalgia patients during standardised muscle exercise: a contrast media enhanced colour Doppler studyEur J Pain200610213714416310717
- LundNBengtssonAThorborgPMuscle tissue oxygen pressure in primary fibromyalgiaScand J Rheumatol19861521651733462905
- SandbergMLindbergLGGerdleBPeripheral effects of needle stimulation (acupuncture) on skin and muscle blood flow in fibromyalgiaEur J Pain20048216317114987626
- BengtssonAThe muscle in fibromyalgiaRheumatology (Oxford)200241772172412096218
- LarssonBBjörkJKadiFLindmanRGerdleBBlood supply and oxidative metabolism in muscle biopsies of female cleaners with and without myalgiaClin J Pain200420644044615502688
- PhilipAMacdonaldALWattPWLactate – a signal coordinating cell and systemic functionJ Exp Biol2005208Pt 244561457516326938
- WeibelERHoppelerHExercise-induced maximal metabolic rate scales with muscle aerobic capacityJ Exp Biol2005208Pt 91635164415855395
- NorrbomJExercise and Regulation of Mithochondrial Biogenesis Factors in Human Skeletal Muscle [doctoral thesis]Stockholm, Karolinska Institute2008
- BengtssonAHenrikssonKGLarssonJMuscle biopsy in primary fibromyalgia. Light-microscopical and histochemical findingsScand J Rheumatol1986151162421398
- LarssonBBjörkJHenrikssonKGGerdleBLindmanRThe prevalences of cytochrome c oxidase negative and superpositive fibres and ragged-red fibres in the trapezius muscle of female cleaners with and without myalgia and of female healthy controlsPain2000842–337938710666544
- KimTJFremlLParkSSBrennanTJLactate concentrations in incisions indicate ischemic-like conditions may contribute to postoperative painJ Pain200781596616949881
- GladdenLBLactate metabolism: a new paradigm for the third millenniumJ Physiol2004558Pt 153015131240
- RobergsRAGhiasvandFParkerDBiochemistry of exercise-induced metabolic acidosisAm J Physiol Regul Integr Comp Physiol20042873R502R51615308499
- CairnsSPLactic acid and exercise performance: culprit or friend?Sports Med200636427929116573355
- EisenhutMWallaceHIon channels in inflammationPflugers Arch2011461440142121279380
- LeeYLeeCHOhUPainful channels in sensory neuronsMol Cells200520331532416404144
- BarbieriESestiliPReactive oxygen species in skeletal muscle signalingJ Signal Transduct2012201298279422175016
- CruzRSde AguiarRATurnesTPenteado Dos SantosRde OliveiraMFCaputoFIntracellular shuttle: the lactate aerobic metabolismScientificWorldJournal2012201242098422593684
- LanzaIRNairKSMitochondrial function as a determinant of life spanPflugers Arch2010459227728919756719
- Kallenborn-GerhardtWSchröderKGeisslingerGSchmidtkoANOXious signaling in pain processingPharmacol Ther2013137330931723146925
- SchaibleHGEbersbergerANaturaGUpdate on peripheral mechanisms of pain: beyond prostaglandins and cytokinesArthritis Res Ther201113221021542894
- SacerdotePLevriniLPeripheral mechanisms of dental pain: the role of substance PMediators Inflamm2012201295192022474402
- HarrisonSGeppettiPSubstance pInt J Biochem Cell Biol200133655557611378438
- IannoneFLapadulaGObesity and inflammation – targets for OA therapyCurr Drug Targets201011558659820199391
- Graven-NielsenTMcArdleAPhoenixJIn vivo model of muscle pain: quantification of intramuscular chemical, electrical, and pressure changes associated with saline-induced muscle pain in humansPain1997691–21371439060024
- MarchandSThe Phenomenon of Pain1st editionSeattleIASP Press2012
- WangHEhnertCBrennerGJWoolfCJBradykinin and peripheral sensitizationBiol Chem20063871111416497159
- RiedelWNeeckGNociception, pain, and antinociception: current conceptsZ Rheumatol200160640441511826734
- LevineJDReichlingDBPeripheral mechanisms of inflammatory painWallPDMelzackRTextbook of Pain4th edEdinburghChurchill Livingstone19995984
- SommerCKressMRecent findings on how proinflammatory cytokines cause pain: peripheral mechanisms in inflammatory and neuropathic hyperalgesiaNeurosci Lett20043611–318418715135924
- UçeylerNSchäfersMSommerCMode of action of cytokines on nociceptive neuronsExp Brain Res20091961677819290516
- HelmyACarpenterKLSkepperJNKirkpatrickPJPickardJDHutchinsonPJMicrodialysis of cytokines: methodological considerations, scanning electron microscopy, and determination of relative recoveryJ Neurotrauma200926454956119196175
