Abstract
Background
A spinal triage assessment service may impact a wide range of patient outcomes. Investigating potential predictors of success or improvement may reveal why some people improve and some do not, as well as help to begin to explain potential mechanisms for improvements. The objective of this study was to determine which factors were associated with improved short-term self-reported pain, function, general health status, and satisfaction in people undergoing a spinal triage assessment performed by physiotherapists.
Methods
Participants with low back-related complaints were recruited from people referred to a spinal triage assessment program (N=115). Participants completed baseline questionnaires covering a range of sociodemographic, clinical, and psychological features. Self-reported measures of pain, function, quality of life, and satisfaction were completed at 4 weeks following the assessment. Determination of “success” was based on minimal important change scores of select outcome measures. Multivariate logistic regression was used to explore potential predictors of success for each outcome.
Results
Despite the complex and chronic presentation of most participants, some reported improvements in outcomes at 4 weeks post assessment with the highest proportion of participants demonstrating improvement (according to the minimal important change scores) in the Medical Outcomes Survey 36-item short-form version 2 physical component summary score (48.6%) and the lowest proportion of participants having improvements in the Numeric Pain Rating Scale (11.5%). A variety of different sociodemographic, psychological, clinical, and other variables were associated with success or improvement in each respective outcome.
Conclusion
There may be a potential mechanism of reassurance that occurs during the spinal triage assessment process as those with higher psychological distress (measured by the Fear Avoidance Beliefs Questionnaire and the Distress and Risk Assessment Measure) were more likely to improve on certain outcomes. The use of an evaluation framework guided by a biopsychosocial model may help determine potential mechanisms of action for a physiotherapy-delivered triage program.
Background
Musculoskeletal conditions such as low back pain (LBP), osteoarthritis, and other regional pain syndromes are highly prevalent and associated with a considerable burden of pain, disability, and work loss.Citation1–Citation4 An estimated one in four adults will consult primary care for a musculoskeletal problem during a 1-year period with LBP being the most common reason for consultation.Citation5 Although most people with back pain can be effectively managed in primary care, people with LBP continue to comprise a significant proportion of referrals made to secondary care specialist providers such as orthopedic surgeons.Citation6,Citation7 As many of these patients are not considered to be surgical candidates,Citation8,Citation9 it calls into question the appropriateness and efficiency of this traditional referral pathway.
New models of care provision that function at the interface between primary and secondary care and involve non-surgical specialists or other health care professionals, such as physiotherapists (PTs), providing care to people with musculoskeletal problems are increasingly being reported in the literature.Citation10–Citation13 PTs with advanced orthopedic training, often practicing with a maximized or extended scope, have been shown to be equally as effective as orthopedic surgeons for the diagnosis and non-surgical management of many musculoskeletal conditions.Citation10,Citation11,Citation14–Citation18 PTs performing this role have also contributed to reduced wait times and improved referral practicesCitation10,Citation19 with data from the United Kingdom indicating that pre-screening of patients by PTs can more than double the proportion of patients who need surgery on assessment by the surgeon.Citation20 However, research evaluating these types of programs is sparse.Citation21 The few programs studied or evaluated focus on general musculoskeletal practicesCitation10,Citation22–Citation24 or hip and knee joint arthritis management only.Citation12,Citation25 Few triage services delivered by PTs focused solely on spinal conditions are described or evaluated in the literature.Citation19,Citation26,Citation27
A triage assessment program delivered by PTs can be viewed as a complex intervention that may have the potential to impact a wide range of patient-centered outcomes.Citation28 Complex interventions may contain a number of different elements that act independently or interdependently, thus it is difficult to identify precise mechanisms that contribute to outcomes.Citation29 A systematic review examining the evidence of extended roles for a variety of health professionals, including PTs, concluded that one of the notable omissions in much of the research was a focus on health outcomes in patients.Citation30 We have recently shown that participants of a spinal triage program delivered by PTs demonstrated overall significant short-term (ie, 4 weeks) improvements in self-reported pain and general physical health as well as high satisfaction with the service; however, the reasons for these improvements remain unclear.Citation31,Citation32 Examination of potential predictors of short-term success or improvement in outcomes using a biopsychosocial model may help to shed light on why some people improve and some do not, as well as help to explain potential mechanisms of action for improvements in this relatively short time frame after the triage assessment.
A purely biomedical approach to care has been unproductive for many musculoskeletal problems, especially for those that are chronic or persistent.Citation33 The biopsychosocial model is proposed as a means to more completely understand, evaluate, and manage disability attributed to persisting health conditions such as chronic back disorders.Citation34–Citation36 A biopsychosocial approach acknowledges the interaction between physical or biological, psychological and social factors.Citation34,Citation35,Citation37,Citation38 This model draws on a broader understanding of biological and psychosocial influences on the development and persistence of pain and disability. The model does not reject a search for important pathology, but shifts the emphasis to other components of the problem.Citation33 Unfortunately, much of the outcomes research involving people with spine-related problems to date has not incorporated this multidimensional approach.
The purpose of this study was to determine which demographic, clinical, psychosocial and other factors were predictive of improved self-reported pain, function, general health status, and participant satisfaction. We used a biopsychosocial approach through the types of outcomes measured and through the type and breadth of potential predictive variables examined.
Methods
Design
We used a quasi-experimental one-group pretest–posttest observational design.Citation39 This design represented the best option to evaluate this program given that there was no accessible and equivalent control group that could be used as a comparison. The “pretest” measures were derived from a paper-based survey that was completed before the participants underwent the triage assessment and also from a clinical classification tool completed by the assessing PT. The “posttest” evaluation of outcomes was done at approximately 4 weeks following the assessment through either mail or a password protected online survey (as per the choice of the participant). The rationale for the 4-week follow-up time frame was to allow enough time for the assessment report and recommendations to be sent to the primary care provider and short enough that any treatment recommendations would likely not yet have been carried out, thus giving an indication of whether changes in outcomes could be attributable to the assessment process itself. Reminders for completion of the participant follow-up surveys were done by phone or email prompts (up to three reminders approximately 1 week apart) on the basis of the tailored design method proposed by Dillman et al.Citation40 This study was approved by the University of Saskatchewan’s Behavioural Ethics Board. Written informed consent was obtained from each participant.
Participants
The participants of the study were recruited from a convenience sample of people referred to the spinal triage program either directly from their primary care provider or via one of the participating orthopedic surgeons. The inclusion criteria included: patients referred to the spinal triage program with primarily low back related complaints; age ≥18 years and ≤80 years; and provision of informed consent. The exclusion criteria included: patients receiving third party payer funding (ie, Worker’s Compensation Board, or other) for their back related complaints; patients with primarily neck or mid back complaints; and people with language, reading, or comprehension barriers that would limit adequate completion of the study paperwork. Patients were also excluded due to other reasons such as scheduling conflicts or other medical issues.
Measures
Before undergoing the triage assessment, participants completed a battery of questionnaires covering a range of variables including: sociodemographics; clinical features; fear avoidance beliefs; depression; and somatization. Outcomes of interest were: self-perceived pain; self-perceived function; general health status; and satisfaction.
Sociodemographic and general health variables
The following sociodemographic variables were collected at intake: age; sex; marital status; highest level of educational attainment; annual household income; and employment-related variables. Employment status (paid full-time, paid part-time, unemployed, housework, disabled, student, retired), and employment type were self-reported. The intake questionnaire also included two questions with dichotomous (ie, yes/no) response options pertaining to work and LBP: “If you are not working, is this because of your low back problem?”; and “do you feel [that] your back problem is caused by your work?” A question regarding farming status was also included as rural and remote residents comprise the majority of referrals to the urban-based spinal triage service.Citation27
Also collected were the residential postal codes of participants. “Urban” residence was classified as living in a town or city with ≥10,000 residents as determined on the basis of having a number other than zero in the second position of the postal code.Citation41 All other postal codes were designated as “rural” and categorized along a continuum of relative rurality on the basis of Statistics Canada’s classification of metropolitan influence zones (MIZs). MIZs are determined by the percentage of the community population that commutes to a city or urban center for employment.Citation41 MIZs were categorized into: strong MIZ (>30% residents commute to work in an urban core [population ≥10,000]); moderate MIZ (5%–30% of residents commute to an urban core); weak MIZ (0%–5% of residents commute to work in an urban core); and no MIZ (40 or fewer residents commute to work in an urban core).Citation41 General health measures included: self-reported presence of other health conditions; height and weight (to calculate body mass index); and smoking status (ie, current, past, or never smoked).
Clinical features
Total duration of symptoms and the duration of current episode related to participants’ presenting symptoms was ascertained from the intake questionnaire. The presence and location of lower extremity symptoms (ie, pain, numbness, tingling or other) was determined from a body diagram completed by participants. Symptom location was coded into “back only”, “above knee leg referral” or “below knee referral” on the basis of the body diagram.
A clinical classification tool, derived from the diagnostic triage categories developed by international groups of expertsCitation42–Citation44 that also incorporates management recommendations, was developed in consultation with the PTs and surgeons involved in the spinal triage program. Further details regarding the clinical classification tool can be found elsewhere.Citation31
Fear avoidance beliefs
The emergence of the biopsychosocial model of LBP led Waddell et alCitation45 to develop the Fear Avoidance Beliefs Questionnaire (FABQ). The FABQ can be used to assess participants’ beliefs with regard to the effect of physical activity and work on their LBP. It consists of 16 items and patients rate their agreement with each statement on a 7-point Likert scale (0= completely disagree, 6= completely agree). The original factor analysis demonstrated two subscales: the work subscale (FABQ_W) and the physical activity subscale (FABQ_PA). The psychometric properties of the subscales are better established than the total FABQ so use of the subscales may be preferable.Citation46 The FABQ has been shown to explain unique amounts of variance in work loss and disability, after controlling for other relevant factors.Citation45 A higher score indicates more strongly held fear avoidance beliefs.
Depression and somatization
Depression and increased bodily/somatic awareness are often reported by people who experience chronic or persistent pain.Citation47 The Distress and Risk Assessment Method (DRAM)Citation48 was used in this study to identify psychological distress related to depression and somatization. The DRAM combines scores from a depression questionnaire (Modified Zung Depression Inventory) and a questionnaire pertaining to somatic symptoms (Modified Somatic Perception Questionnaire). The DRAM is a simple method of classifying patients into those showing no psychological distress, those at risk, and those who are clearly distressed either due to primarily somatic or depressive symptoms. Main et al suggest that people who are “distressed” either due to primarily depressive or somatic symptoms according to the DRAM may need more than just “physical” treatment and should be referred on for further psychological assessment.Citation48 The DRAM has also been shown to predict outcomes in primary care patients with back pain.Citation49
Self-perceived pain
The 11-point Numeric Pain Rating Scale (NPRS) ranges from 0 (“no pain”) to 10 (“worst pain imaginable”) and was used to indicate the intensity of current pain, pain at its best, and pain at its worst level over the last 24 hours.Citation50 These three ratings were averaged to arrive at an overall pain score. The scale has been shown to have adequate reliability, validity, and responsiveness in patients with LBP when the three scores are averaged.Citation51
Self-perceived function
Self-perceived function was assessed with the modified Oswestry Disability Questionnaire (ODQ), which is a condition-specific self-report questionnaire.Citation52,Citation53 Items on the ODQ focus on how much LBP is limiting activities of daily living, like sitting, standing, walking, and lifting. The ODQ was modified from the original by substituting a section regarding employment/home-making ability for the section related to sex life.Citation52–Citation54 The modified ODQ has been found to have high levels of reliability (intraclass correlation coefficient [ICC] =0.90) and responsiveness in patients with LBP.Citation52–Citation54 The ODQ is proposed to be most useful in specialty care settings or in situations in which the disability level is likely to remain relatively high throughout a trial.Citation55 Higher scores on the ODQ represent higher levels of perceived disability. Fairbank et alCitation52–Citation53 suggest that the continuous scores can be categorized into five categories of perceived disability (ie, “minimal”, “moderate”, “severe”, “crippled”, and “bed bound”/“exaggerating”). As there were no participants with ODQ scores in the highest disability category in this study, the last category was eliminated in our analysis.
Quality of life/general health status
The Medical Outcomes Survey 36-item short-form survey version 2 (SF-36v2®; non-commercial license agreement with Quality Metric Incorporated for use of SF-36v2. License number: CT113220/OP001547) was used to assess general health status.Citation56 The measure is comprised of eight interrelated health dimensions (physical functioning, role-limitations resulting from physical health problems, bodily pain, general health, vitality [energy/fatigue], social functioning, role-limitations resulting from emotional problems, and mental health [psychological distress/psychological well-being]). Two component summaries (ie, physical component summary [PCS] and mental component summary [MCS]) can be derived from the eight subscales.Citation56 The SF-36 has been shown to be a valid and reliable measure for both clinical and general populations.Citation57–Citation59 The SF-36v2® has been shown to have improved reliability over the previous SF-36 version as well as improved floor and ceiling effects in certain domains.Citation56,Citation60 Scoring of the SF-36v2® was done by transformation of raw scores into norm-based scores for each of the subscales and weighting of each subscale to produce the PCS and MCS. Higher scores represent greater health status or quality of life.
Satisfaction
Participant satisfaction with the triage program was determined through two questions developed specifically for this purpose.Citation31 The first question pertained to participants’ level of satisfaction with the service received and the second question related to their satisfaction with the recommendations that were made. Possible responses were on a 5-point Likert scale (ie, “very satisfied”, “somewhat satisfied”, “neither satisfied nor dissatisfied”, “somewhat dissatisfied” or “very dissatisfied”).
Follow-up measures
The NPRS, ODQ, and SF-36v2® were repeated at the 4-week posttest time point as the main outcomes of interest. The PCS and MCS scores were derived from the SF-36v2®. The participant satisfaction survey was also administered at that time. These measures cover domains of pain, back specific function, general well-being/quality of life and satisfaction, and align with the recommendations of various expert groups.Citation55,Citation61
Analysis
Descriptive analysis of all baseline measures and variables included frequencies and percent for categorical variables and mean, standard error, median and interquartile ranges for continuous variables. Comparisons between responders and non-responders were done with independent samples Student’s t-test or Mann–Whitney U test for continuous variables and chi-square or Fisher’s exact tests for categorical variables. The determination of “success” or improvement in select outcome measures (ie, NPRS, ODQ, PCS, MCS) was based on proposed minimal important change (MIC) or difference scores. The MIC score is defined as: “the smallest difference in score in the outcome of interest that informed patients or informed proxies perceive as important, either beneficial or harmful, and which would lead the patient or clinician to consider a change in the management”.Citation62 The proposed MIC values for the measures used in this study were derived from the recommendations of a consensus group of international experts in the field who produced guidelines for the clinical interpretation of commonly used measures for pain and back-specific function. The recommendations are as follows: 2-NPRS, 10-ODQ, 2-PCS, 3-MCS (note – units are specific to each of the measures indicated).Citation62 The individual change scores between pretest and posttest time points were recoded into those that improved a minimum of the MIC value and those that did not improve as per the MIC value for each outcome. “Improvers” for “satisfaction” were coded as follows: “somewhat satisfied” and/or “very satisfied” on both items of satisfaction questionnaire (ie, satisfaction with service and satisfaction with recommendations). The proportions (ie, percentages) in each group for each outcome were subsequently calculated.
Multivariate logistic regression was used to explore potential “predictors of success” for each outcome of interest (ie, NPRS, ODQ, PCS, MCS, satisfaction). The MIC cut-points were used to dichotomize each outcome/dependent variable into people who improved or those who did not improve. The model building process began with a bivariate analysis exploring the association of a range of sociodemographic, clinical, and other variables using either chi-square or Fisher’s exact test where appropriate. For most variables, data over the full range of each measure were collected, however for the purposes of the regression analyses most variables were transformed or recoded. shows the variables used in the bivariate analysis. Continuous variables were initially dichotomized or transformed into categorical variables based on either median values or clinically relevant cut-points in order to allow clearer interpretation of resulting odd ratios and to avoid restrictive assumptions of straight-line linearity between variables.Citation63 Also any variables that had zero cell counts in the initial bivariate analysis, were recoded by collapsing categories of the independent variable. Any variables that had a P-value of <0.25 from the bivariate analysis were considered as a candidate for the multivariate models.
Table 1 Description of variables included in bivariate analysis
Independence of variables (both among independent variables and between dependent and independent variables) is an assumption of logistic regression.Citation63 Correlation within independent variables and among baseline/pretest and posttest variables of the same measure was evaluated with Spearman’s correlation coefficient. For any independent variables that were correlated r>0.5, only the most significant variable (as per the bivariate analysis) was used in the multivariate model.Citation64 Any baseline variables that were correlated r>0.3Citation65 with the dependent outcome variable of the same measure (eg, baseline ODQ and ODQ_MIC) were also excluded from the models.
The remaining dependent variables were evaluated with logistic regression using a backward stepwise selection procedure with P-values of 0.10 to exit the model and 0.05 to enter it. Stepwise selection procedures are recommended over other model building strategies when there is an exploratory purpose to the analysis and when the relationships among dependent outcome variables and covariates are not well established or understood.Citation66,Citation67 Furthermore, a backwards selection procedure is recommended over a forward procedure due to higher risks of making Type II errors with forward selection procedures.Citation67 Goodness-of-fit of the final model was assessed by the Hosmer–Lemeshow statistical test.Citation63 The resulting models were tested for multi-collinearity by examining variance inflation factors.Citation67 The final models are presented as adjusted odds ratios (ORs) with 95% confidence intervals. Statistical analysis was done using PASW (Predictive Analytics SoftWare) Statistics Mac version 18.0.
Results
During the 8-month study intake period 198 people had an assessment through the spinal triage program. Fifty-six people were excluded and 27 people who met the inclusion criteria chose not to participate. This left a total of 115 participants, thus the overall participant rate, among those people who were eligible, was 81.0% (115/142). Among study participants, 66/115 (57.4%) opted to complete a mailed paper-based follow-up survey and 49/115 (42.6%) chose to complete an online password protected follow-up survey. A total of 108/115 participants (93.9%) completed the posttest survey. The only significant difference between these groups was “residence” with proportionately more responders having a “rural” residence (69.4% responders versus [vs] 28.6% non-responders; P=0.039). The baseline sociodemographic and health characteristics of the participants are shown in .
Table 2 Baseline sociodemographic and health characteristics
The median age of participants was 51 years, 48.7% were female and the majority was married (74.8%). Most participants (55.6%) had an educational attainment of more than grade 12, an annual household income of greater than 30 K (81.6%), had full- or part-time employment (68.7%), and had a “rural” residence (70%). Also, a relatively large proportion of the participants were farmers (27.8%). The majority of the sample had a body mass index greater than a “normal” range (73.9%), used to smoke or were current smokers (61.2%), and had two or more other chronic health conditions (58.2%) with “other bone or joint problems” being the most prevalent condition reported (62.6%). Approximately half (50.8%) of participants were in the “at risk” DRAM category with 17.4% scoring as being distressed to either somatic or depressive symptoms. Most participants (79.2%) had “moderate” to “severe” perceived disability according to the categorized ODQ scores.
Clinical baseline characteristics of the study sample can be found in . Most participants reported having relatively long total duration of symptoms (74.8% >24 months). The majority of participants had attempted a variety of non-invasive treatment modalities in the past including medication, massage therapy, chiropractic, and physiotherapy with relatively few (3.5%) reporting having past surgical intervention for their back problems. The majority of participants also reported having below knee symptoms (59.1%) indicating potential nerve root involvement. A summary of the categorization of clinical features with the clinical classification tool completed by the assessing PT can also be found in . The majority of participants were classified as having a “problem in back” (93.9%); however, there were relatively high proportions classified as “medical” (9.6%) and “spinal cord/cauda equina” (4.3%) presentations. Similarly, categorization according to the LBP triage categories demonstrated relatively high proportions of “nerve root problems” (47.0%) and “serious spine pathology” (7.0%). Further PT treatment was recommended in the majority of cases (63.5%) and “referral to the surgeon” was made in 20% of cases.
Table 3 Baseline clinical characteristics, diagnostic classification, and triage recommendations
The proportion of participants that “improved” vs those that “did not improve” is presented in and . The PCS of the SF-36v2® is the measure that had the largest proportion of participants who improved (48.6%) and the lowest proportion of participants reached an MIC threshold of improvement on the NPRS (11.5%). The majority of participants (79.6%) reported being “somewhat satisfied” and/or “very satisfied” with both the assessment service and with the recommendations.
Figure 1 Proportion of participants that improved versus those that did not improve.
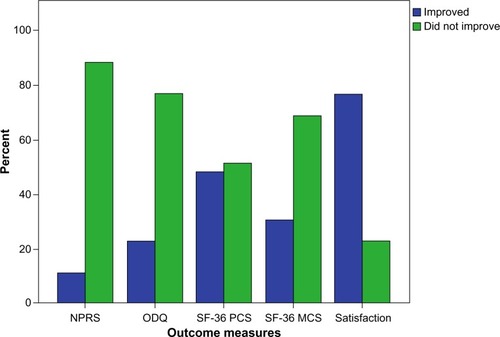
Table 4 Proportion of participants who improved versus those who did not improve
A range of 6 to 12 independent variables was found to be associated with each of the outcome measures in the bivariate analysis (results not shown). summarizes the results of the logistic regression analyses to examine which variables were associated with each outcome and retained in the multivariate models. Both crude (ie, bivariate) and adjusted (ie, multivariate) ORs of the retained variables are presented. All models had mean variance inflation factors close to 1 and no independent variable had a variance inflation factor above 2, indicating that the independence assumption was met. The following variables were associated with an improvement in NPRS at the posttest time point: urban residence (vs rural); and having nerve root pathology, serious spine- or non-spine-related pathology (vs non-specific LBP). Participants with a “moderate” or “severe” ODQ score at baseline were less likely than those with a “minimal” score to demonstrate NPRS improvements. Covariates associated with improvement in the ODQ were: being male; having an LBP duration (total and current episode) of less than 6 months; having never smoked; having a baseline SF-36 PCS <35; having a baseline FAB_Q >15; and being referred to “another specialist” as part of the management recommendations. Variables associated with improved SF-36 PCS were: having never smoked (vs used to smoke); being a current smoker (vs never smoked); and having a baseline FABQ_W >14. The following variables were associated with improved SF-36 MCS scores: being married; having <2 comorbidities; having an NPRS baseline score of <5; and an SF-36 MCS baseline score of <48. Finally, the variables associated with participant satisfaction were: age <50 years; not being married; having an educational attainment of < grade 12; being referred for a magnetic resonance imaging (MRI) or computed tomography (CT) scan; having a “minimal” ODQ score at baseline; and being in the “at risk or distressed” category of the DRAM (vs “normal”).
Table 5 Crude and adjusted estimates for improvement in perceived pain, function, general health, and satisfaction
Discussion
The aim of this study was to determine which factors were predictive of short-term (ie, 4 weeks) improved self-reported pain, function, quality of life (“physical” and “mental”), and satisfaction of participants with low back-related complaints who underwent a spinal triage assessment delivered by PTs. We used a biopsychosocial framework and approach through the types of outcomes measured and through the type and breadth of potential predictive variables examined. We have shown that a variety of different sociodemographic, psychological, clinical, and other factors were associated with success or improvement in a battery of outcomes. Our hope was that an evaluative framework informed by a biopsychosocial model would lead to a more complete and multidimensional understanding of outcomes related to this type of service.
The baseline characteristics of this study’s sample demonstrate that the people referred to the spinal triage service may not be representative of a typical person who presents with low back complaints in a primary care setting. The majority of the participants had longstanding symptoms (75% had >24 month total symptom duration), complex clinical presentations (ie, high proportion of below knee symptom referral, high proportion of other chronic conditions), high perceived disability, psychological risk factors (according to the DRAM), and low overall general well-being compared to both healthy normative populations and disease-specific norms of people with back pain/sciatica.Citation56
Despite the complex and chronic presentation of many of the participants, certain people did report improvements in outcomes at the 4-week post assessment time point with the highest proportion of participants demonstrating improvement (according to the MIC scores) in the SF-36 PCS (48.6%) and the lowest proportion of participants having improvements in the NPRS (11.5%). Even though a variety of different covariates was identified through multivariate modeling for each outcome of interest (), we will limit our discussion to a few key items as grouped by sociodemographic, clinical, and psychological variables.
Sociodemographic variables
Men were more likely than women to have improved ODQ scores at the posttest time point. This finding appears to be consistent with other research which has shown that women are more likely than men to utilize more health care for back pain, take more sick days from work, have a poor outcome after a single episode of LBP, and develop persistent, chronic pain lasting more than 3 months.Citation68,Citation69
Marital status may be a proxy indicator of social support and possibly household income. We are unaware of any other studies that have examined the impact of marital status on back pain outcomes, but our results would suggest that being married could be associated with either positive or negative outcomes depending on the type of outcome examined. For example, being married (vs not married) was associated with a positive outcome on the SF-36 MCS, but a negative likelihood of satisfaction.
With respect to place of residence, urban dwellers were more likely than rural participants to report improvement in the NPRS. People living in rural and remote locations may experience different exposures in terms of occupational and environmental factors, social factors, and access to health care.Citation70 Given the large proportion of participants from “rural” regions referred to this service and emerging research that demonstrates that rural residents, especially farmers, are at higher risk of LBP and associated disability than their urban counterparts,Citation71–Citation74 this is an important area that requires further study.
Clinical variables
The diagnostic categorization and duration of symptoms appear to have an impact on self-reported pain and function, but not on other types of outcomes. For example, having a diagnostic categorization of “nerve root”, “serious spine” or “not spine” related pathology (according to the LBP triage categories) was associated with greater likelihood of improved NPRS scores compared to those participants who were classified as having “non-specific LBP”; however, the reasons for this association are unclear. Having symptom duration (both total and current episode) of less than 6 months was associated with greater likelihood of improved ODQ scores; an unsurprising finding given that this group represents people who have had low back symptoms for less time than would be considered “chronic” or persistent and/or have recurring episodic LBP that would likely have a tendency to resolve periodically over time.
Management recommendations (eg, referral to specialist), on the other hand, may impact physical (ie, ODQ) or satisfaction outcomes (eg, MRI/CT referral). Reporting greater satisfaction with referral for advanced imaging is concurrent with other research.Citation75,Citation76 Patients expect a clear diagnosis for their LBPCitation77 and may equate a decision to not obtaining imaging in order to “provide a precise diagnosis” with low quality careCitation78 or as a message that their pain is not legitimate or important.Citation79
Psychological variables
The fear-avoidance model, as described by Vlaeyen and Linton, suggests that chronic pain is preceded by catastrophic beliefs about pain, avoidance of activities, hypervigilance, and disuse or depression.Citation80 An estimated 50% of back pain patients feel that they have some type of serious diseaseCitation35 and this belief may feed into psychological distress and fear.Citation42 Our results would appear to suggest that there may be a potential mechanism of reassurance that occurs during the spinal triage assessment process as those with higher psychological distress were more likely to improve on certain outcomes. For example, having higher FABQ scores at the baseline was associated with greater likelihood of improved ODQ (FABQ_PA) and PCS scores (FABQ_W). A baseline FABQ_W score of >14 may in fact be an independent predictor of having an improved PCS score at the posttest time point given the similarity between the crude and adjusted ORs (ie, both ORs are 2.21). Furthermore, those participants who were “at risk or distressed” according to the DRAM were more likely to report being satisfied with the service.
The role of reassurance in interactions between health care providers and patients with chronic pain is a complex process that requires further study.Citation81 Further research in this area may help to elucidate the role of reassurance in the spinal triage assessment process and other potential mechanisms for why improvements in short-term outcomes may occur. The fear-avoidance beliefs model may serve as a useful underlying theory to help guide such work.
Study limitations
The results of this study should be considered in light of its many limitations. The main limitations relate to the relatively small sample size and the methods of classification for both independent and dependent variables.
Studies that examine a large number of variables should ideally have a larger sample size so that the model derived through multivariate analysis is not “overfit” and thus result in a model that describes random error or “noise” rather than the underlying relationship. Limited sample size can result in a Type II error whereby some of the variables identified in the multivariate analysis may have been identified simply by chance.Citation64
On the other hand, it is also important that all likely variables are included in the items considered for the models to reduce the possibility of missing those that make an important contribution.Citation66 The use of a biopsychosocial model to frame the types of predictive variables measured in this study helped to ensure that many likely candidate variables were considered. According to Kleinbaum and Klein, a minimum of ten observations per predictor variable can be used as an estimate of adequate sample size.Citation64 Thus, in our study a minimum of 130 participants (based on up to 12 predictor variables entered into the multivariate analyses from the bivariate analysis) would have been needed for adequate power.
For most variables, data over the full range of each independent variable and measure were collected, however for the purposes of the regression analyses most variables were transformed or recoded to allow clearer interpretation of the resulting ORs and to avoid restrictive assumptions of straight line linearity between variables.Citation66 This recoding of many of the independent variables may have resulted in some associations between independent and outcome variables being missed or misconstrued. Also, we did not consider interaction terms in our model building strategy (mainly owing to the small sample size), thus the relationships between variables may not be entirely representative of what actually occurred.
The use of MIC scores as a threshold of improvement or “success” in the outcome measures or dependent variables may be problematic. The MIC cut-points used in this study were derived from a recent consensus of experts in the field and based on a notoriously heterogeneous body of LBP research.Citation62 The guidelines were meant to reflect empirical evidence and practicality; however, the authors indicate caution given that different MICs may be more appropriate for different patients or contexts.Citation62 In other words, had different cut-points been used to dichotomize the outcomes (or if continuous dependent outcome measures were modeled with linear vs logistic regression), the resulting covariates may be different.
A final and important limitation is that we did not account for any treatment or other interventions that the participants may have initiated during the 4-week follow-up time frame. Our rationale for this time frame was to allow enough time for the assessment report and recommendations to be sent to the primary care provider and short enough that any treatment recommendations would likely not yet have been carried out and possibly not even initiated. Given this limitation and the lack of control group, however, we cannot assume that any improvements were attributable to the assessment process itself.
Next steps
The aims of this study were primarily exploratory and further research is needed to more fully understand the longer term impacts that a spinal triage service delivered by PTs can have as well as the potential mechanisms by which improvements occurred. Further study examining outcomes and predictors of success at 6 and 12 months following the assessment is ongoing. We will then be able to ascertain whether short-term improvements following the assessment were sustainable or not and which factors may impact sustainability. Examination of potential predictors of deterioration in outcomes using a biopsychosocial model may also help to shed light on why some people do not improve. Determining whether or not participants undertook and/or had access to the health care recommendations made in the assessment will likely be an important consideration in evaluating longer term outcomes. The main role of the spinal triage program is to provide management recommendations to referring primary care providers. Thus, given that the triage program may re-direct the type of care that people receive and not deliver that care per se, determining potential “modifiable” predictors of deterioration (such as access to care) may help to alert health care providers and policy makers to gaps in optimal care pathways that may ultimately impact patient outcomes. In particular access to rehabilitation and other health care services in rural and remote communities as well as barriers to access of privately delivered care due to costs would be very relevant considerations.
Further research should incorporate a randomized controlled trial design with longitudinal follow-up along with an economic evaluation in order to fully evaluate the efficacy of a spinal triage service delivered by PTs.
Conclusion
Despite the complex and chronic presentation of many of the participants, certain people did report improvements in outcomes at the 4-week post spinal triage assessment time point with the highest proportion of participants demonstrating improvement in the SF-36 PCS score (48.6%) with the lowest proportion of participants improving according to the NPRS (11.5%). A variety of different sociodemographic, psychological, clinical, and other variables were associated with improvement in each respective outcome. Our findings suggest that there may be a potential mechanism of reassurance that occurs during the assessment process, as those with higher psychological distress were more likely to improve on certain outcomes.
A spinal triage program delivered by PTs is an example of a complex intervention whereby a number of different elements may act independently or interdependently to impact a wide range of patient-related outcomes. We have shown that examination of potential predictors of short-term success or improvement in outcomes using a biopsychosocial model may help to shed light on why some people improve and some do not, as well as help to explain potential mechanisms of action of a spinal triage service delivered by PTs.
Authors’ contributions
BB led the conception and design of the study, the acquisition, analysis, and interpretation of data and drafted the manuscript. SLG contributed to the interpretation of the data, and to the revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgments
BB was supported by the following funders during the course of this research: Canadian Institutes of Health Research (CIHR) Fellowship in Knowledge Translation, Public Health and the Agricultural Rural Ecosystem CIHR Graduate Training Program, and the Western Regional Training Centre for Health Services Research CIHR Graduate Training Program. Operational funding for this research was provided by Bourassa and Associates Rehabilitation Centre, Saskatoon, Saskatchewan, Canada. BB is currently supported by funding from the Saskatchewan Health Research Foundation, Ralston Brother’s Medical Research Trust, and the College of Medicine, University of Saskatchewan. SLG is currently supported by funding from the Public Health and the Agricultural Rural Ecosystem CIHR Graduate Training Program and the College of Medicine, University of Saskatchewan. The authors are grateful to the surgeons and PTs associated with the Wall Street Spinal Assessment Service for their support of this project. We are also thankful to Cindy Robb for her assistance with data entry and study administration. Finally, we would like to thank Drs Bonnie Janzen, Punam Pahwa, Liz Harrison, and Alice Aiken for suggestions on earlier versions of this manuscript.
Disclosure
BB and SLG are former employees of Bourassa and Associates Rehabilitation Centre, Saskatoon, Saskatchewan, Canada (where the Wall Street Spinal Assessment Service is located). The authors report no other conflicts of interest.
References
- BreivikHEisenbergEO’BrienTOPENMindsThe individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate careBMC Public Health201313122924365383
- HoyDBainCWilliamsGA systematic review of the global prevalence of low back painArthritis Rheum20126462028203722231424
- VosTFlaxmanADNaghaviMYears lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries: a systematic analysis for the Global Burden of Disease Study 2010Lancet201238098592163219623245607
- LawrenceRCFelsonDTHelmickCGEstimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part IIArthritis Rheum2008581263518163497
- JordanKPKadamKDHaywardsRPorcheretMYoungCCroftPAnnual consultation prevalence of regional musculoskeletal problems in primary care: an observational studyBMC Musculoskelet Disord20101114420598124
- HadlowATBack Pain: a problem of referralJ Bone Joint Surg Br200385-BSupp III208
- MacKayCCanizaresMDavisABadleyEHealth care utilization for musculoskeletal disordersArthritis Care Res (Hoboken)201062216116920191514
- Arthritis Community Research and Evaluation Unit [homepage on the Internet]CanizaresMMacKayMDavisAMahomedNBadleyEOrthopaedic Surgery in Ontario in the era of the wait time strategyTorontoArthritis Community Research and Evaluation Unit2007 Working report 2007-2. Available from: http://www.acreu.ca/pdf/pub5/07-02.pdfAccessed March 23, 2015
- MaymanDYenDMaximizing use of a surgical clinic for referrals of patients having back problemsCan J Surg199942211711910223072
- Daker-WhiteGCarrAJHarveyIA randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departmentsJ Epidemiol Community Health1999531064365010616677
- HattamPThe effectiveness of orthopaedic triage by extended scope physiotherapistsClinical Governance: An International Journal200494244252
- AikenABHarrisonMMAtkinsonMHopeJEasing the burden for joint replacement wait times: the role of the expanded practice physiotherapistHealthc Q2008112626318362522
- SarroARampersaudYRLewisSNurse practitioner-led surgical spine consultation clinicJ Adv Nurs201066122671267620831572
- ChildsJDWhitmanJMSizerPSPugiaMLFlynnTWDelittoAA description of physical therapists’ knowledge in managing musculoskeletal conditionsBMC Musculoskelet Disord200563215963232
- MooreJHGossDLBaxterREClinical diagnostic accuracy and magnetic resonance imaging of patients referred by physical therapists, orthopaedic surgeons, and nonorthopaedic providersJ Orthop Sports Phys Ther2005352677115773564
- BoissonnaultWGPrimary Care for the Physical Therapist: Examination and TriageToronto, CanadaElsevier Ltd2005
- HattamPSmeathamAEvaluation of an orthopaedic screening service in primary careClin Perform Qual Health Care19997312112410848384
- JibuikeOOPaul-TaylorGMaulviSRichmondPFaircloughJManagement of soft tissue knee injuries in an accident and emergency department: the effect of the introduction of a physiotherapy practitionerEmerg Med J2003201373912533365
- HouriganPGWeatherleyCRInitial assessment and follow-up by a physiotherapist of patients with back pain referred to a spinal clinicJ R Soc Med19948742132148182677
- The Chartered Society of PhysiotherapyMaking Physiotherapy CountLondon, UKThe Chartered Society of Physiotherapy2004
- DesmeulesFRoyJSMacDermidJCChampagneFHinseOWoodhouseLJAdvanced practice physiotherapy in patients with musculoskeletal disorders: a systematic reviewBMC Musculoskelet Disord20121310722716771
- O’CathainAFroggettMTaylorMPGeneral practice based physiotherapy: its use and effect on referrals to hospital orthopaedics and rheumatology outpatient departmentsBr J Gen Pract1995453963523547612338
- HendriksEJKerssensJJNelsonRMOostendorpRAvan der ZeeJOne-time physical therapist consultation in primary health carePhys Ther2003831091893114519063
- SephtonRHoughERobertsSAOldhamJEvaluation of a primary care musculoskeletal clinical assessment service: a preliminary studyPhysiotherapy201096429630221056164
- KennedyDMRobartsSWoodhouseLPatients are satisfied with advanced practice physiotherapists in a role traditionally performed by orthopaedic surgeonsPhysiother Can201062429830521886368
- WeatherleyCRHouriganPGTriage of back pain by physiotherapists in orthopaedic clinicsJ R Soc Med19989173773799771498
- BathBGronaSLJanzenBA spinal triage programme delivered by physiotherapists in collaboration with orthopaedic surgeonsPhysiother Can201264435636523997390
- KerstenPMcPhersonKLattimerVGeorgeSBretonAEllisBPhysiotherapy extended scope of practice – who is doing what and why?Physiother2007934235242
- CampbellMFitzpatrickRHainesAFramework for design and evaluation of complex interventions to improve healthBMJ2000321726269469610987780
- McPhersonKKerstenPGeorgeSA systematic review of evidence about extended roles for allied health professionalsJ Health Serv Res Policy200611424024717018199
- BathBJanzenBPatient and referring health care provider satisfaction with a physiotherapy spinal triage assessment serviceJ Multidicip Healthc20125115
- BathBPahwaPA physiotherapy triage assessment service for people with low back disorders: evaluation of short-term outcomesPatient Relat Outcome Meas2012391922915980
- CroftPPeatGVan der WindtDPrimary care research and musculoskeletal medicinePrim Health Care Res Dev201011416
- WaddellGLow back pain: a twentieth century health care enigmaSpine (Phila Pa 1976)19962124282028259112705
- WaddellGThe biopsychosocial modelWaddellGThe Back Pain Revolution2nd ednTorontoChurchill Livingstone2004265
- CiezaAStuckiGWeiglMICF Core Sets for low back painJ Rehabil Med200444Suppl697415370751
- EngelGLThe need for a new medical model: a challenge for biomedicinePsychodyn Psychiatry201240337739623002701
- ChouRShekellePWill this patient develop persistent disabling low back pain?JAMA2010303131295130220371789
- ShadishWCookTDCampbellDTExperimental and quasi-experimental designs for generalized causal inferenceBoston, MAHoughton Mifflin Company2002
- DillmanDASmythJDChristianLMInternet, mail and mixed-mode surveys: the tailored design method3rd edHoboken, New JerseyJohn Wiley and Sons Inc2009
- du PlessisVBeshiriRBollmanRClemensonHAgricultural and Rural Working Paper Series Definitions of ‘Rural’, No 61OttawaStatistics Canada Agriculture Division2002 Available from: http://www5.statcan.gc.ca/olc-cel/olc.action?ObjId=21-601-M2002061&ObjType=46&lang=en&limit=0Accessed 9 April 2015
- GreenhalghSSelfeJRed Flags: A Guide to Identifying Serious Pathology of the SpineTorontoChurchill Livingstone2006
- Clinical Standards Advisory Group (CSAG) on low back painBack Pain. Report of a CSAG Committee on Back PainLondon, UKHer Majesty’s Stationery Office1994
- BigosSAcute low back pain in adults. Clinical practice guidelineRockwille, MDUS Department of Health and Human Services1994
- WaddellGNewtonMHendersonISomervilleDMainCJA Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disabilityPain19935221571688455963
- WilliamsonEFear Avoidance Beliefs Questionnaire (FABQ)Aust J Physiother200652214916805041
- CroftPRPapageorgiouACFerrySThomasEJaysonMISilmanAJPsychologic distress and low back pain. Evidence from a prospective study in the general populationSpine (Phila Pa 1976)19952024273127378747252
- MainCJWoodPLHollisSSpanswickCCWaddellGThe Distress and Risk Assessment Method. A simple patient classification to identify distress and evaluate the risk of poor outcomeSpine (Phila Pa 1976)199217142521531554
- BurtonAKTillotsonKMMainCJHollisSPsychosocial predictors of outcome in acute and subchronic low back troubleSpine (Phila Pa 1976)19952067227287604349
- JensenMPTurnerJARomanoJMWhat is the maximum number of levels needed in pain intensity measurement?Pain19945833873927838588
- ChildsJDPivaSRFritzJMResponsiveness of the numeric pain rating scale in patients with low back painSpine (Phila Pa 1976)200530111331133415928561
- FairbankJCCouperJDaviesJBO’BrienJPThe Oswestry low back pain disability questionnairePhysiotherapy19806682712736450426
- FairbankJCPynsentPBThe Oswestry Disability IndexSpine (Phila Pa 1976)200025222940295311074683
- RolandMFairbankJThe Roland-Morris Disability Questionnaire and the Oswestry Disability QuestionnaireSpine (Phila Pa 1976)200025243115312411124727
- DeyoRABattieMBeurskensAJOutcome measures for low back pain research. A proposal for standardized useSpine (Phila Pa 1976)19982318200320139779535
- WareJEJrKosinskiMBjornerJBTurner-BowkerDMGandekBMaruishMEUser’s Manual for the SF-36v2 Health Survey2nd edLincoln, RIQualityMetric Incorporated2007
- BrazierJEHarperRJonesNMValidating the SF-36 health survey questionnaire: new outcome measure for primary careBMJ199230568461601641285753
- GarrattAMRutaDAAbdallaMIBuckinghamJKRussellITThe SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS?BMJ19933066890144014448518640
- BeatonDEHogg-JohnsonSBombardierCEvaluating changes in health status: reliability and responsiveness of five generic health status measures in workers with musculoskeletal disordersJ Clin Epidemiol199750179939048693
- JenkinsonCStewart-BrownSPetersonSPaiceCAssessment of the SF-36 version 2 in the United KingdomJ Epidemiol Community Health1999531465010326053
- BombardierCOutcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendationsSpine (Phila Pa 1976)200025243100310311124724
- OsteloRWDeyoRAStratfordPInterpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important changeSpine200833909418165753
- HosmerSLemeshowDWApplied logistic regression2nd edJohn Wiley & Sons2000
- KleinbaumDGKleinMLogistic Regression: A self-Learning text2nd edNew YorkSpringer2002
- LiangKYZegerSLLongitudinal data analysis using generalized linear modelsBiometrika19867313
- HosmerDWLemeshowSModel-Building Strategies and Methods for logistic RegressionApplied Logistic Regression2nd edTorontoJohn Wiley & Sons200091
- FieldADiscovering Statistics Using SPSS3rd edLos Angeles, CASage Publications Ltd2009
- SmithBHElliottAMHannafordPCChambersWASmithWCFactors related to the onset and persistence of chronic back pain in the community: results from a general population follow-up studySpine (Phila Pa 1976)20042991032104015105678
- LintonSJHellsingAHalldénKA population-based study of spinal pain among 35–45-year-old individuals. Prevalence, sick leave, and health care useSpine (Phila Pa 1976)19982313145714639670397
- PongRWDesmeulesMLagaceCRural-urban disparities in health: how does Canada fare and how does Canada compare with Australia?Aus J Rural Health20091715864
- ParkHSprinceNLWhittenPSBurmeisterLFZwerlingCRisk factors for back pain among male farmers: analysis of Iowa Farm Family Health and Hazard Surveillance StudyAm J Ind Med200140664665411757041
- HolmbergSStiernstromELThelinASvardsuddKMusculoskeletal symptoms among farmers and non-farmers: a population-based studyInt J Occup Environ Health20028433934512412852
- ThelinNHolmbergSNettelbladtPThelinAMortality and morbidity among farmers, nonfarming rural men, and urban referents: a prospective population-based studyInt J Occup Environ Health2009151212819267123
- BathBTraskCMcCroskyJLawsonJA biopsychosocial profile of adult Canadians with and without chronic back disorders: a population-based analysis of the 2009–2010 Canadian Community Health SurveysBiomed Res Int2014201491962124971357
- ChouRQaseemAOwensDShekellePDiagnostic Imaging for Low Back Pain: Advice for High-Value Health Care from the American College of PhysiciansAnn Intern Med2011154318118921282698
- JarvikJGHollingworthWMartinBRapid magnetic resonance imaging vs. radiographs for patients with low back pain: a randomized controlled trialJAMA2003289212810281812783911
- VerbeekJSengrsMJRiemensLHaafkensJPatients expectations for back pain: a systematic review of qualitative and quantitative studiesSpine (Phila Pa 1976)200429202309231815480147
- CarmanKLMaurerMYegianJMEvidence that consumers are skeptical about evidence-based health careHealth Aff (Millwood)20102971400140620522522
- RhodesLAMcPhillips-TangumCAMarkhamCKlenkRThe power of the visible: the meaning of diagnostic tests in chronic low back painSoc Sci Med19994891189120310220019
- VlaeyenJWLintonSJFear-avoidance and its consequences in chronic musculoskeletal pain: a state of the artPain200085331733210781906
- LintonSJMcCrackenLMVlaeyenJWReassurance: Help or hinder in the treatment of painPain20081341–25818035496
- American College of Sports Medicine: ACSM’s Guidelines for Exercise Testing and Prescription5th edBaltimoreWilliams and Wilkins1995
