Abstract
Osteoporosis (OP) is a pathological condition that manifests clinically as pain, fractures, and physical disability, resulting in the loss of independence and the need for long-term care. Chronic pain is a multidimensional experience with sensory, affective, and cognitive aspects. Age can affect each of these dimensions and the pain that is experienced. In OP, chronic pain appears to have sensory characteristics and properties of nociceptive and neuropathic pain. Its evaluation and treatment thus require a holistic approach that focuses on the specific characteristics of this population. Pain management must therefore include pharmacological approaches, physiotherapy interventions, educational measures, and, in rare cases, surgical treatment. Most rehabilitative treatments in the management of patients with OP do not evaluate pain or physical function, and there is no consensus on the effects of rehabilitation therapy on back pain or quality of life in women with OP. Pharmacological treatment of pain in patients with OP is usually insufficient. The management of chronic pain in patients with OP is complicated with regard to its diagnosis, the search for reversible secondary causes, the efficacy and duration of oral bisphosphonates, and the function of calcium and vitamin D. The aim of this review is to discuss the most appropriate solutions in the management of chronic pain in OP.
Introduction
Osteoporosis (OP) is a pathological condition that is characterized by a bone mineral density (BMD) level that is 2.5 SD (standard deviation) or more below the mean value (T-score =−2.5) for a young adult. OP comprises a heterogeneous group of syndromes in which the bone mass per unit volume is decreased in otherwise normal bones, rendering them more fragile and increasing their risk of fractures.Citation1,Citation2 The vertebral bodies, proximal end of the femur, distal end of the radius, and proximal end of the humerus are the sites that are most commonly affected by fragility fractures.
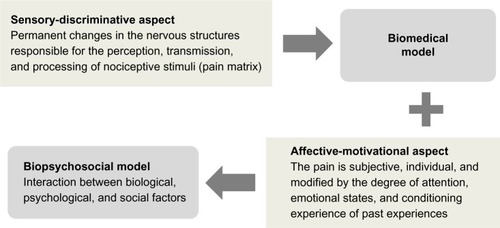
Figure 1 Mechanisms responsible for chronic pain. The interaction between permanent changes in the nociceptive system and individual psychosocial factors.
OP can manifest clinically as pain, fractures, and physical disability, resulting in the loss of independence and the need for long-term care. Recent studies have reported the prevalence of OP and osteopenia to be 10% and 36% in men aged between 60 years and 79 years and 18.5% and 44.7% in women aged between 40 years and 79 years, respectively, and an estimated 22 million women and 5.5 million men are affected by OP in the European Union.Citation3,Citation4
In elderly persons, OP and sarcopenia are often associated in both conditions, the number and size of muscle fibers are reduced, and there is a preferential loss of type II fibers.Citation5 Partial or complete age-related immobilization also increases the risk of muscle atrophy and bone loss, boosting the risk of fractures. The elderly are at greater risk of debilitating postural changes due to several factors, particularly, the involutional loss of functional muscle motor units and the higher prevalence of OP in these subjects. Moreover, as noted by Sinaki, this muscle loss can contribute to OP-related skeletal changes in this population.Citation6 Muscle weakness has been suggested to be related to a progressive decline in bone mass, with consequent axial kyphosis, even in the absence of vertebral fractures.Citation7 Based on these findings, chronic pain can result from OP-induced skeletal deformities, joint imbalance, and tension in muscular structures. Often, the most common symptom in patients with OP is severe or intolerable back pain. Large population studies have reported a link between low back pain (LBP) and OP, especially in the elderly.Citation8–Citation11
Over time, bone fragility can accelerate the onset of multiple fractures, causing a progressive loss of stature and continuous contraction of the paravertebral muscles in maintaining posture. This sequence of events results in muscle fatigue and pain that can persist, even after the fractures have healed.Citation12 Furthermore, with age, the perception and response to pain change for reasons that remain unknown. According to many groups, the pain threshold increases in elderly people.Citation13,Citation14
The frequency of chronic pain usually rises with age, affecting 41% of persons aged 65–75 years, 48% of those aged 75–84 years, and 55% of persons aged >85 years.
Based on several theories, long-term pain is the product of perceptive discoherence and, consequently, the loss of the ability to integrate sensory information.
Thus, pain is a type of feedback that raises one’s awareness and causes discomfort in activating mechanisms of homeostatic recovery.Citation15 As discussed by Craig,Citation16 pain can also be considered the result of the output of a widely distributed neural network in the brain, rather than the direct effect of sensory input that is evoked by an injury.
Chronic pain in OP has sensory characteristics (such as postural alterations, fractures, and muscle atrophy) and properties of nociceptive and neuropathic pain.Citation17 Chronic pain is a multidimensional experience with sensory, affective, and cognitive aspects, all of which interact and contribute to the final response of an individual who is subjected to pain. Age can affect each of these dimensions and the pain that is experienced. Moreover, the sensation of chronic pain can be altered by memory, expectations, and emotions.Citation18,Citation19
The evaluation and treatment of chronic pain in patients with OP thus require a holistic approach that focuses on the specific characteristics of this population, assessing their comorbidities, mental status, functional status, and independence in carrying out daily activities. Pain management must therefore include pharmacological approaches, physiotherapy interventions, and in rare cases, surgical treatment. Most rehabilitative treatments in the management of patients with OP do not evaluate pain or physical function.Citation20 Rehabilitation treatments that are based on exercises help manage these symptoms quickly without generating significant adverse effects or contraindications.Citation21
Despite the development of guidelines on the diagnosis and treatment of OP,Citation22 the management of chronic pain in these patients remains complicated. The aim of this review was to discuss the most appropriate solutions in the management of chronic pain in OP, considering recent scientific evidence on pharmacological and nonpharmacological therapies and surgical treatment.
Nonpharmacological therapy
Physical exercise
Compared with earlier beliefs, the sole purpose of rehabilitative exercises in OP is not merely to preserve or increase bone mass. Complementary and alternative approaches, such as yoga and pilates, have been proposed to improve function and reduce chronic pain in the spine.
It is essential that all exercises be performed safely, with a gradual progression of difficulty, avoiding bending and rotation of the trunk, which might be harmful and aggravate back pain.Citation23 Taking these precautions into consideration, according to Tüzün et al,Citation24 yoga is an approach that has a positive effect on pain and has physical and social benefits for patients with OP. Pilates exercises increase BMD, improve quality of life and walking distances, and relieve pain, and can thus be offered to patients with OP.Citation25 As reviewed by Wei et al,Citation26 a Wuqinxi-based exercise program of at least 6 months, five times per week for 30–60 minutes each session, can improve pain symptoms.
The standard rehabilitation treatment in patients with OP is based on correcting postural changes, preventing falls by improving balance and coordination, relieving pain, and enhancing one’s psychological well-being. Frequently, group rehabilitation is proposed to teach the exercises to the patient, allowing him or her to repeat them autonomously at home.Citation27 A recent studyCitation28 noted that group rehabilitation exercises reduce back pain and improve functional status and quality of life in postmenopausal women with OP, the results of which were maintained for up to 6 months after the end of treatment.
A recently proposed rehabilitation program considered national guidelines and recommendations on interventions that aim to prevent and treat postmenopausal OP.Citation27 The exercises included muscular stretching exercises and balance strengthening of antigravity muscles and were conducted with greater difficulty and intensity. All strengthening exercises and flexibility sessions ended with stretching exercises.
Bergland et alCitation29 suggested that exercise-based treatment in persons with spinal OP is beneficial and is associated with less pain and better quality of life, strength, and balance. Interventions ranged from simple back extension exercises to various general weight-bearing exercises, balance activities, and stretches that were combined with upper limb, trunk, and lower limb strengthening. The interventions were delivered in a class format, as a home program or as a combination of physiotherapist-led sessions and home exercise programs. There was no evidence that any of these delivery options was superior to another.Citation30–Citation36
von Stengel et al and Kronhed et al concluded that power training is superior to strength training in maintaining BMD in postmenopausal women.Citation37,Citation38
Exercises for improving axial stability include a back extension exercise program. When fragility is resolved, as Sinaki reported, back extension is performed against resistance that is applied to the upper back. The exercise regimen must always correspond to the needs of the patient: in general, an exercise program – therapeutic or recreational – must target flexibility, muscle strength, core stability, cardiovascular fitness, and gait steadiness.Citation10,Citation39
The use of tape, in association with back exercise, was recently shown to lower pain in OP: in postural taping, tape is applied to the skin to increase proprioceptive feedback on postural alignment, improve thoracic extension, reduce pain, and facilitate muscle activity and postural balance.Citation40
Postural deformities and imbalances, which occur typically in OP, are associated with muscle contractures of the spine, and soft manual tissue massage therapy with exercises improves the perceived change in back pain in these patients. Bennell et alCitation41 proposed soft tissue massage and passive accessory central posterior–anterior mobilization techniques for the thoracic spine.
Physical therapy
Physical therapy, such as the use of magnetic fields and vibration training, has been administered to treat patients with OP. There is little evidence on the use of magnetic fields in chronic pain that is associated with OP. A review by Huang et alCitation42 concluded that low-frequency PEMFs (pulsed electromagnetic fields) relieve the pain of primary OP quickly and efficiently.
Vibration training can treat OP-induced pain and improve physical fitness by increasing muscle strength, neuromuscular coordination, and balance and reducing the risk of falls, which often result in fractures, as reported by Iwamoto et al.Citation43,Citation44 The analgesic effects of whole-body vibration have also been confirmed in two other studies.Citation45,Citation46 Based on these inconsistent results, it is difficult to determine the appropriate range of frequencies for obtaining the positive effects of this therapy. However, the therapy must be initiated at lower vibration frequencies, increasing gradually throughout the therapy.Citation47
Other forms of nonpharmacological therapy that have been suggested for the management of chronic pain include cognitive-behavioral therapy and mindfulness-based interventions. Cognitive-behavioral therapy is a form of psychotherapy that is used to deepen the understanding of one’s pain and teach self-control and coping strategies (extinguishing maladaptive behavior and reinforcing positive reactions to pain). It improves pain and quality of life and reduces disabilities in patients who suffer from chronic painCitation48 and has strong therapeutic effects against chronic LBP.Citation49
Mindfulness-based interventions are based on the separation of the sensory and emotional aspects of pain and the promotion of awareness of bodily and psychological sensations within the body. Through mindful awareness and meditation, thoughts on pain can be viewed as discrete events rather than as a problem that necessitates possibly maladaptive responses. These interventions are traditionally structured as 2-hour sessions every week for a minimum of 10 weeks to establish awareness of the body, proprioceptive signals, breath, and physical sensations and develop mindful activities (such as eating, walking, and standing).Citation50
Pharmacological therapy
Chronic pain is a major public health concern with significant economic, social, and medical impacts. In the past several decades, public health authorities have recorded increased access to the emergency department and greater morbidity and mortality, secondary to medical and nonmedical overuse of pain relievers, especially opioids.Citation51
Choosing the appropriate analgesic should always be based on the intensity of chronic pain that is reported by the patient.Citation52 For cases of mild pain (numeric rating scale [NRS] ≤3), nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen is recommended, with the possibility of augmenting with adjuvants; for those with moderate pain (NRS 4–6), weak opioids with or without NSAIDs or acetaminophen are suggested, with the option of adjuvant therapy; and those with strong pain (NRS >6) should be treated with opioids and NSAIDs or acetaminophen, with possible supplementation with adjuvants. Adjuvant drugs are a class of molecules that contribute to mitigating pain, increasing the effects of analgesics.Citation53
In any case, based on the possible adverse effects, abuse, and addiction that might result from the use of certain drugs, especially opioids, it is always advisable to resort to pharmacological therapy only after nonpharmacological therapies have failed, eventually combining the two therapies (multimodal therapy) in cases of pain that are persistent and resistant to nonpharmacological treatments in augmenting and complementing the pharmacological treatment. The most frequently recommended first-line nonpharmacological therapies are physical exercises performed individually or in group initially under the guidance of a therapist and later independently at home; gymnastic and breathing activities, such as yoga and pilates; cognitive-behavioral therapy; mindfulness-based pain management; and physical therapies, such as magnetic fields, analgesic stimulation, and vibration therapy.
This treatment strategy is recommended especially for pain in patients with OP without fractures, whereas those with fractures should consider a combination of pharmacological and nonpharmacological therapies. Bisphosphonates appear to be effective; in particular, intravenous pamidronateCitation54 has sustained analgesic effects and reduces acute back pain due to recent osteoporotic vertebral fractures. In these patients, teriparatide also lowered the risk of new or worsening back pain.Citation55
NSAIDs and opioids
NSAIDs are widely used for chronic pain that is associated with fragility fractures. Nevertheless, the treatment of pain in such patients is rarely considered a priority in the therapeutic management.Citation56 Yet, in patients with OP with chronic pain, these agents have negative effects on bone metabolism and thus should not be considered first-line drugs for long periods. An estimated 70% of elderly patients and ∼20% of hospitalized patients are treated with NSAIDs.Citation57 Vestergaard et al noted that patients who take NSAIDs experience more fractures than expected.Citation58
The pharmacological action of NSAIDs and celecoxib on cyclooxygenase can have a profound effect on skeletal health, although this enzyme appears to mediate the healing of skeletal tissue, directly or indirectly, by modulating the inflammatory response.
Also, acetaminophen, the most widely prescribed analgesic and antipyretic, is associated with an increased risk of fractures, the mechanisms of which are unknown.Citation59
Treatment of pain with a peripherally acting drug, such as ibuprofen, can reduce the chronic pain that is associated with OP more effectively than a centrally acting medication, such as tramadol. Thus, it is advisable to prescribe ibuprofen rather than tramadol to treat OP-associated chronic pain in postmenopausal women, taking into account the risk of gastrointestinal side effects.Citation60
Opioids can be used to relieve moderate-to-severe OP-associated pain that is inadequately managed with more conservative or interventional methods. They are not a first-line therapy and must be taken for short periods with close monitoring to limit the risk of side effects.Citation61 Approximately 50% of all opioid users experience at least one side effect, and >20% discontinue treatment due to a serious adverse event.Citation57,Citation62 Common side effects include constipation, nausea, vomiting, pruritus, delayed gastric emptying, dizziness, sedation, tolerance, and addiction.
In the treatment of moderate pain, the World Health OrganizationCitation63 recommends weak opioids, primarily codeine and tramadol. The transdermal opioid patch is recommended for patients with continuous pain in whom oral administration is not possible. In opioid-naïve patients, treatment should be started at a low dose and titrated slowly to minimize the risk of related adverse effects. The use of long-acting opioids (eg, morphine) can provide more consistent pain relief, with less risk of addiction or abuse and better adherence. To better address the difficulties that are associated with the management of chronic pain, the physician should tailor the treatment after evaluating a patient’s history of pain and its specific effects.Citation64
Vitamin D
Vitamin D stimulates osteoblast activity; increases intestinal absorption of calcium from the diet, governing calcium metabolism and parathyroid hormone activity; and improves proximal muscle function. The rationale for vitamin D in the treatment of patients with OP is that improving skeletal health will reduce the risk of fractures and, consequently, pain.Citation65 Vitamin D mitigates musculoskeletal pain and downregulates inflammatory markers in patients with postmenopausal OP, especially after the infusion of zoledronic acid.Citation66 Persistent pain is associated with vitamin D-linked bone demineralization, myopathy, and musculoskeletal pain. Pain pathways that are associated with changes in cortical, immunological, hormonal, and neuronal levels are potentially influenced by vitamin D.Citation67
Antiresorptive drugs
Denosumab
Denosumab is a fully human monoclonal antibody that inhibits the differentiation and function of osteoclast precursors. It has been approved for postmenopausal patients who are at high risk of osteoporotic fractures.Citation68 There is little evidence of the efficacy of denosumab against chronic pain in patients with OP. Denosumab decreases bone pain after 12 months of treatment, as evidenced by visual analog scale (VAS) scores, in patients with primary and secondary OP. In addition, 12-month treatment with denosumab increases BMD in the lumbar spine and total hip.Citation69
Bisphosphonates
Bisphosphonates raise bone mass levels by inhibiting bone resorption and preventing fractures.Citation70,Citation71 They improve pain and quality of life in patients with OP, effects that are likely to be linked to their antiabsorptive activity and their capacity to suppress the production of neuropeptides, such as substance P and calcitonin gene-related peptide, and inflammatory cytokines, such as tumor necrosis factor alpha.Citation72
One bisphosphonate, alendronate, decreases pain and improves quality of life better than calcium in women with postmenopausal OP. Alendronate significantly reduces pain, based on VAS scores, and enhances quality of life compared with calcium supplementation alone.Citation73 Alendronate increases BMD and significantly alleviates joint pain and any exacerbation of back pain, suggesting that reduction in pain contributes to improvements in overall quality of life in such patients.Citation74 Another study confirmed the beneficial effects of alendronate on pain and quality of life in postmenopausal women with OP.Citation75 Alendronate increases lumbar spine BMD and mitigates chronic back pain, suppressing bone resorption in postmenopausal women with OP.Citation73 Alendronate also lowers the need for analgesics and improves daily activity functioning and mobility of the spine in patients with postmenopausal OP.Citation76 These effects suggest that switching to alendronate with cyclic etidronate leads to a greater change in lumbar BMD, bone resorption, and back pain compared with continuous treatment with cyclical etidronate in postmenopausal women with OP.Citation77
Ibandronate significantly decreases pain and stiffness and improves functional motor failure in patients with OP and concomitant gonarthrosis.Citation78 It can be administered orally and intravenously and has robust effects in alleviating bone pain. The oral and intravenous versions of ibandronate are well tolerated.
A study of patients who were treated with daily minodronate or weekly alendronate reported a significant reduction in pain, as measured on the VAS.Citation79 However, the analgesic effects were observed in more minodronate-treated patients. Minodronate performs better than alendronate in limiting bone turnover and lowers back pain in the absence of gastrointestinal side effects.Citation79 Risedronate also reduces pain and disability and improves quality of life, as assessed using the Short Form-36 survey, in postmenopausal osteoporotic women without vertebral fractures.Citation80 The relationship between LBP and OP, in the absence of vertebral fractures, remains unknown. A decrease in bone resorption correlates with improved LBP, suggesting that despite the lack of vertebral fractures, the bone loss that is due to OP can cause back pain.Citation80
Owing to their ability to improve the underlying pathogenesis of OP, bisphosphonates are considered to be a component of palliative therapy for bone pain that is associated with malignant diseases and also appear to be effective as analgesics in other nonmalignant conditions. A recent review describes the anti-inflammatory properties and the analgesic effect of clodronate with a good safety profile; it is shown to be effective on pain in patients with fragility fracturesCitation81 and to have a higher pain killer effect, compared to other analgesics, such as paracetamol, and other aminobisphosphonates, including neridronate.Citation82
Intravenous pamidronate is efficacious against chronic back pain due to osteoporotic vertebral fractures.Citation54 A study reported the efficacy of zoledronic acid in the treatment of pain in patients who were affected by LBP as a single intravenous infusion of 5 mg compared with placebo at 1 month and recommended its use only in severe disabling LBP or when symptoms are not adequately controlled with pain medication and physiotherapy.Citation83 Furthermore, in patients with postmenopausal OP, zoledronic acid reduced the number of days with back pain and limited activity due to back pain versus placebo.Citation84
Teriparatide
Teriparatide is a human parathyroid hormone analog that stimulates osteoclasts to resorb bone and affects the generation of osteoblasts, inducing the formation of new bone. It lowers the incidence of vertebral and hip fractures and has been approved for OP in patients who are at high risk of fractures.Citation85,Citation86 Eighteen months of treatment with teriparatide in patients with severe OP is associated with reduction in pain-related vertebral fractures and disability and constant and progressive improvement in quality of life, with clinically and statistically significant effects after 12 months of therapy. Although teriparatide does not alter the biomechanical factors that mediate the pathogenesis of spinal pain, it lowers the incidence of new micro- and macrofractures and strengthens the structure and quality of bone in the spine, mitigating pain and functional limitations and improving quality of life.Citation87
A meta-analysis showed that teriparatide-treated patients with OP had a lower risk of new or worse pain in the lower back compared with those who received placebo, hormone replacement therapy, or alendronate.Citation88 One study noted rapid and significant improvements in back pain and quality of life in patients who had been treated with teriparatide, effects that persisted after 18 months, also after the interruption of therapy,Citation89 and another reported that teriparatide treatment was associated with a significant reduction in back pain.Citation90 Patients with severe OP who were administered teriparatide, antiresorptives (raloxifene and bisphosphonates), or both reported significantly less LBP, although there were no differences between treatment groups with regard to the primary end point of the proportion of patients who experienced a ≥30% reduction in worst back pain at 6 months.Citation91 Teriparatide significantly increases the density of bone mass, in terms of T-score, lowering the incidence of new fractures, improving the quality of life, and decreasing the consumption of NSAIDs.Citation92
Strontium ranelate
Strontium ranelate increases BMD and tempers the risk of vertebral and nonvertebral fractures. It also enhances osteoblast function and suppresses osteoclast activity.Citation93,Citation94 Strontium ranelate significantly improves quality of life and pain compared with placebo.Citation95 One study reported that strontium ranelate has a positive anabolic effect that accelerates the healing of fractures, causing the disappearance of secondary pain after several months of treatment.Citation96 Strontium ranelate also reduces the risk of vertebral fractures by 33% over 4 years, with beneficial effects on quality of life and back pain,Citation97 and is associated with significantly less back pain and analgesic use in men with primary OP.Citation98
Long-term therapy with strontium ranelate decreases the risk of fractures and is well tolerated, with a low incidence of side effects, rendering it a suitable first-line treatment for postmenopausal women who are at high risk of fractures. It should be administered with caution in patients who are at risk of venous thromboembolism or have a rash.Citation99
Calcitonin
Calcitonin is an endogenous polypeptide hormone that inhibits bone resorption by osteoclasts. It increases bone density in postmenopausal women, predominantly at the lumbar spine, and reduces the incidence of vertebral fractures.Citation100
Few studies have demonstrated its efficacy in the treatment of chronic pain in patients with OP. A review on calcitonin in postmenopausal OP recommends short-term use, based on evidence of a link between calcitonin therapy and cancer.Citation101 Calcitonin appears to mitigate pain by acting on the central nervous system,Citation102 and when administered subcutaneously or intranasally, it has excellent analgesic effects in patients with vertebral fractures.Citation103
Raloxifene
Raloxifene is a selective estrogen receptor modulator that has estrogen and estrogen-like effects on bone and antagonizes the action of estrogen in endometrium and breast tissue. Treatment with raloxifene in postmenopausal women with OP correlates with a marked reduction in skeletal pain and analgesic consumption and improved sleep quality.Citation104 Clinical studies suggest that postmenopausal women who are on estrogen replacement therapy have a greater risk of developing LBP and its associated disability than those who are not taking estrogens. It appears that raloxifene has no influence on back pain or disability in women with postmenopausal OP.Citation105 A recent retrospective database analysisCitation104 noted similar improvements in fracture rates in cohorts of patients who were treated with alendronate or raloxifene, demonstrating a lower risk of breast cancer in those who were given raloxifene. The side effects of raloxifene include a greater risk of fatal stroke and venous thromboembolism.Citation105
Surgical treatments
Percutaneous vertebroplasty is commonly used to treat vertebral fractures due to OP, and although its superiority over conservative treatment remains debated, it generates better results than conservative treatment with regard to pain and function in women aged ≥60 years with OP.Citation106 Up to 51% of fractures in women and 24% of those in men are attributable to OP hip fractures and their resulting disabilities.Citation107 Many patients with severe OP undergo hip arthroplasty, and good results have been obtained with cemented and uncemented femoral implants. Uncemented implants appear to be more affected by periprosthetic fractures, and both types are subject to a greater risk of dislocation.Citation108
Conclusion
Today, a single-track approach to chronic pain in patients with OP is no longer conceivable. The standard modality in OP is to combine pharmacological and nonpharmacological therapies. Exercises for improving axial stability must always be proposed, and the exercise regimen should correspond to the needs of the patient, who has to be instructed by the therapist on home exercise programs to improve his self-management of chronic pain. As discussed, nonpharmacological treatments include various approaches (such as mind-body exercises) that have shown good efficacy. Other recommended approaches for the management of chronic pain are cognitive-behavioral therapy and mindfulness-based interventions to teach the patient to learn how to accept pain and find strategies to react to it properly. Concerning the recommendations on time course of drug in patients with chronic pain affected by OP, the generic precautions given in analgesics guidelines for each single drug should be applied. For example, the duration of therapy with paracetamol should not exceed 4–5 days in order to avoid adverse effects. In general, the therapy with analgesic and anti-inflammatory drugs must be limited to the shortest possible period of time.Citation109
In conclusion, the preferred pharmacological treatment for chronic pain in patients with OP is bisphosphonates, particularly alendronate, followed by denosumab, strontium ranelate, and teriparatide.
Disclosure
The authors report no conflicts of interest in this work.
References
- KanisJAMcCloskeyEVJohanssonHOdenAMeltonLJ3rdKhaltaevNA reference standard for the description of osteoporosisBone200842346747518180210
- TarantinoUCaponeAPlantaMThe incidence of hip, forearm, humeral, ankle, and vertebral fragility fractures in Italy: results from a 3-year multicenter studyArthritis Res Ther2010126R22621190571
- MaggiSNoaleMGianniniSESOPO Study GroupESOPO Study Group Quantitative heel ultrasound in a population-based study in Italy and its relationship with fracture history: the ESOPO studyOsteoporos Int200617223724416142503
- StrömOBorgströmFKanisJAOsteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA)Arch Osteoporos201165915522886101
- TarantinoUBaldiJCeliMOsteoporosis and sarcopenia: the connectionsAging Clin Exp Res201325Suppl 1S93S9524046056
- SinakiMMusculoskeletal challenges of osteoporosisAging (Milano)19981032492629801735
- SinakiMBreyRHHughesCALarsonDRKaufmanKRBalance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strengthOsteoporos Int20051681004101015549266
- Fernández-de-las-PeñasCHernández-BarreraVAlonso-BlancoCPrevalence of neck and low back pain in community-dwelling adults in Spain: a population-based national studySpine201136E213E21921079541
- ChouYCShihCCLinJGChenTLLiaoCCLow back pain associated with sociodemographic factors, lifestyle and osteoporosis: a population-based studyJ Rehabil Med2013451768023052969
- SinakiMPfeiferMPreisingerEThe role of exercise in the treatment of osteoporosisCurr Osteoporos Rep20108313814420574788
- NagaeMHiragaTWakabayashiHWangLIwataKYonedaTOsteoclasts play a part in pain due to the inflammation adjacent to boneBone20063951107111516769263
- KimDHVaccaroAROsteoporotic compression fractures of the spine; current options and considerations for treatmentSpine J20066547948716934715
- GasikRStyczy skiTSpecifics of pharmacological treatment of back pains in people of old agePolski Merkuliusz Lekarski200621124394397
- KołodziejWBio psycho social functioning of people in old age and social stereotypes and prejudice concerning ageing and old ageNowickaASelected Problems of People in Old AgeKrakówOficyna Wydawnicza Impuls20065571
- MelzackRPain and the neuromatrix in the brainJ Dent Educ200165121378138211780656
- CraigADPain mechanisms: labeled lines versus convergence in central processingAnnu Rev Neurosci20032613012651967
- DziechciaMBalicka-AdamikLFilipRThe problem of pain in old ageAnn Agric Environ Med2013Spec no. 1353825000839
- IannettiGDMourauxAFrom the neuromatrix to the pain matrix (and back)Exp Brain Res2010205111220607220
- CraigADHow do you feel now? The anterior insula and human awarenessNat Rev Neurosci2009101597019096369
- HoweTESheaBDawsonLJExercise for preventing and treating osteoporosis in postmenopausal womenCochrane Database Syst Rev20117CD00033321735380
- PedersenBKSaltinBThe evidence for prescribing exercise as therapy in chronic diseaseScand J Med Sci Sports200616Suppl 136316451303
- HernlundESvedbomAIvergårdMOsteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA)Arch Osteoporos2013813624113837
- SinakiMYoga spinal flexion positions and vertebral compression fracture in osteopenia or osteoporosis of spine: case seriesPain Pract2013131687522448849
- TüzünSAktasIAkarirmakUSipahiSTüzünFYoga might be an alternative training for the quality of life and balance in postmenopausal osteoporosisEur J Phys Rehabil Med2010461697220332729
- AngınEErdenZCanFThe effects of Clinical Pilates Exercises on bone mineral density (BMD), physical performance and quality of life of women with postmenopausal osteoporosisJ Back Musculoskelet Rehabil201528484985826406222
- WeiXXuAYinYZhangRThe potential effect of Wuqinxi exercise for primary osteoporosis: a systematic review and meta-analysisMaturitas201582434635426386831
- BonaiutiDArioliGDianaGSIMFER rehabilitation treatment guidelines in postmenopausal and senile osteoporosisEura Medicophys200541431533716474287
- PaolucciTMoroneGIosaMEfficacy of group-adapted physical exercises in reducing back pain in women with postmenopausal osteoporosisAging Clin Exp Res201426439540224338597
- BerglandAThoresenHKåresenREffect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomised controlled trialOsteoporos Int20102261863187121060992
- ChienYCYangRSTsauoJYHome-based trunk-strengthening exercise for osteoporotic and osteopenic postmenopausal women without fracture–a pilot studyClin Rehabil2005191283615704506
- GoldDTShippKMPieperCFDuncanPWMartinezSLylesKWGroup treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized clinical trialJ Am Geriatr Soc20045291471147815341548
- HongoMItoiESinakiMEffect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: arandomized controlled trialOsteoporos Int200718101389139517572835
- MadureiraMMTakayamaLGallinaroALCaparboVFCostaRAPereiraRMBalance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trialOsteoporos Int200718441942517089080
- MalmrosBMortensenLJensenMBCharlesPPositive effects of physiotherapy on chronic pain and performance in osteoporosisOsteoporos Int1998832152219797905
- PapaioannouAAdachiJDWinegardKEfficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis related vertebral fracturesOsteoporos Int200314867768212879220
- SinakiMBreyRHHughesCALarsonDRKaufmanKRSignificant reduction in risk of falls and back pain in osteoporotic-kyphotic women through a spinal proprioceptive extension exercise dynamic (SPEED) programMayo Clin Proc200580784985516007888
- von StengelSKemmlerWKalenderWAEngelkeKLauberDDifferential effects of strength versus power training on bone mineral density in postmenopausal women: a 2-year longitudinal studyBr J Sports Med20074110649655 discussion 65517550916
- KronhedA-CGHallbergIÖdkvistLEffect of training on health-related quality of life, pain and falls in osteoporotic womenAdv Physiother2009113154165
- SinakiMExercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall preventionPM R201241188288823174554
- BautmansIVan ArkenJVan MackelenbergMMetsTRehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosisJ Rehabil Med201042212913520140408
- BennellKLMatthewsBGreigAEffects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trialBMC Musculoskelet Disord20101111120044932
- HuangLQHeHCHeCQChenJYangLClinical update of pulsed electromagnetic fields on osteoporosisChin Med J (Engl)2008121202095209919080282
- IwamotoJTakedaTSatoYUzawaMEffect of whole-body vibration exercise on lumbar bone mineral density, bone turnover, and chronic back pain in post-menopausal osteoporotic women treated with alendronateAging Clin Exp Res200517215716315977465
- IwamotoJSatoYTakedaTMatsumotoHWhole body vibration exercise improves body balance and walking velocity in postmenopausal osteoporotic women treated with alendronate: Galileo and Alendronate Intervention Trail (GAIT)Musculoskelet Neuronal Interact2012123136143
- LiuHLiuYYangLCurative effects of pulsed electromagnetic fields on postmenopausal osteoporosisSheng Wu Yi Xue Gong Cheng Xue Za Zhi20143114852 Chinese24804483
- KlarnerAvon StengelSKemmlerWEffects of two different types of whole body vibration on neuromuscular performance and body composition in postmenopausal womenDtsch Med Wochenschr2011136422133213921990056
- RuanXYJinFYLiuYLPengZLSunYGEffects of vibration therapy on bone mineral density in postmenopausal women with osteoporosisChin Med J (Engl)2008121131155115818710630
- EhdeDMDillworthTMTurnerJACognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for researchAm Psychol201469215316624547801
- HanscomDABroxJIBunnageRDefining the role of cognitive behavioral therapy in treating chronic low back pain: an overviewGlobal Spine J20155649650426682100
- Kabat-ZinnJAn outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary resultsGen Hosp Psychiatry19824133477042457
- KolodnyACourtwrightDTHwangCSThe prescription drug opioid and heroin crisis: a public health approach to an epidemic of addictionAnnu Rev Public Health20153655957425581144
- World Health OrganizationCancer Pain Relief2nd edGenevaWHO1996
- VellucciRMediatiRDBalleriniGUse of opioids for treatment of osteoporotic painClin Cases Miner Bone Metab201411317317625568648
- GangjiVAppelboomTAnalgesic effect of intravenous pamidronate on chronic back pain due to osteoporotic vertebral fracturesClin Rheumatol199918326626711206358
- UlivieriFMBack pain treatment in post-menopausal osteoporosis with vertebral fracturesAging Clin Exp Res200719Suppl 3212318180603
- IolasconGCisariCMorettiAFrizziLGimiglianoRGimiglianoFNSAIDs and opioids in management of fragility fracturesAging Clin Exp Res201325Suppl 1S97S10024046027
- GenéECalvetXMoronARecommendations for the use of anti-inflammatory drugs and indications for gastroprotection in emergency departmentsEmergencias2009214295300
- VestergaardPHermannPJensenJEEikenPMosekildeLEffects of paracetamol, non-steroidal anti-inflammatory drugs, acetylsalicylic acid, and opioids on bone mineral density and risk of fracture: results of the Danish Osteoporosis Prevention Study (DOPS)Osteoporos Int20122341255126521710339
- WilliamsLJPascoJAHenryMJParacetamol (acetaminophen) use, fracture and bone mineral densityBone20114861277128121396491
- KrockerDUllrichHButtgereitFInfluence of adjuvant pain medication on quality of life in the treatment of postmenopausal osteoporosisOrthopade200837543543918427773
- LabiancaRSarzi-PuttiniPZuccaroSMCherubinoPVellucciRFornasariDAdverse effects associated with non-opioid and opioid treatment in patients with chronic painClin Drug Investig201232Suppl 15363
- ScheimanJMFendrickAMPractical approaches to minimizing gastrointestinal and cardiovascular safety concerns with COX-2 inhibitors and NSAIDsArthritis Res Ther20057Suppl 4S23S2916168078
- Vargas-SchafferGIs the WHO analgesic ladder still valid? Twenty-four years of experienceCan Fam Physician2010566e202e205
- OralAKüçükdeveciAAVarelaEOsteoporosis. The role of physical and rehabilitation medicine physicians. The European perspective based on the best evidence. A paper by the UEMS-PRM Section Professional Practice CommitteeEur J Phys Rehabil Med201349456557724084415
- LappeJMDaviesKMTravers-GustafsonDHeaneyRPVitamin D status in a rural postmenopausal female populationJ Am Coll Nutr200625539540217031008
- CatalanoAMorabitoNAtteritanoMBasileGCucinottaDLascoAVitamin D reduces musculoskeletal pain after infusion of zoledronic acid for postmenopausal osteoporosisCalcif Tissue Int201290427928522350110
- PlotnikoffGAQuigleyJMPrevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal painMayo Clinic Proc2003781214631470
- CummingsSRSan MartinJMcClungMRFREEDOM TrialDenosumab for prevention of fractures in postmenopausal women with osteoporosisN Engl J Med2009361875676519671655
- PetranovaTSheytanovIMonovSNestorovaRRashkovRDenosumab improves bone mineral density and microarchitecture and reduces bone pain in women with osteoporosis with and without glucocorticoid treatmentBiotechnol Biotechnol Equip20142861127113726019600
- RogersMJCrockettJCCoxonFPMönkkönenJBiochemical and molecular mechanisms of action of bisphosphonatesBone2011491344121111853
- BlackDMThompsonDEBauerDCFracture Intervention TrialFracture risk reduction with alendronate in women with osteoporosis: the fracture intervention trial. FIT research groupJ Clin Endocrinol Metab200085114118412411095442
- IwamotoJTakedaTSatoYUzawaMEffects of alendronate on metacarpal and lumbar bone mineral density, bone resorption, and chronic back pain in postmenopausal women with osteoporosisClin Rheumatol200423538338915278749
- DursunNDursunEYalcinSComparison of alendronate, calcitonin and calcium treatments in postmenopausal osteoporosisInt J Clin Pract200155850550911695068
- KawateHOhnakaKAdachiMAlendronate improves QOL of postmenopausal women with osteoporosisClin Interv Aging2010512313120458350
- IwamotoJMakitaKSatoYTakedaTMatsumotoHAlendronate is more effective than elcatonin in improving pain and quality of life in postmenopausal women with osteoporosisOsteoporos Int201122102735274221104227
- RozkydalZJanicekPThe effect of alendronate in the treatment of postmenopausal osteoporosisBratisl Lek Listy20031041030931315055730
- IwamotoJTakedaTIchimuraSUzawaMEarly response to alendronate after treatment with etidronate in postmenopausal women with osteoporosisKeio J Med200352211311912862363
- AlekseevaLIZaitsevaEMSharapovaEPEvaluation of the efficacy and tolerance of ibandronic acid in patients with osteoarthrosis in the knee joints concurrent with osteoporosis: a pilot studyTer Arkh2013855303623819336
- YoshiokaTOkimotoNOkamotoKSakaiAA comparative study of the effects of daily minodronate and weekly alendronate on upper gastrointestinal symptoms, bone resorption, and back pain in postmenopausal osteoporosis patientsJ Bone Miner Metab201331215316023076293
- OhtoriSAkazawaTMurataYRisedronate decreases bone resorption and improves low back pain in postmenopausal osteo porosis patients without vertebral fracturesJ Clin Neurosci201017220921320044258
- MuratoreMCalcagnileFQuartaEAntalgic efficacy of the bisphosphonates in vertebral fractures of recent onsetOsteoporos Int200415Suppl 1S121
- MuratoreMCanaparoRDella PepaCBisphosphonates antalgic activity in recent vertebral fracture: a clodronate vs neridronate comparisonOsteoporos Int200415Suppl 1S119
- KoivistoKKyllönenEHaapeaMEfficacy of zoledronic acid for chronic low back pain associated with Modic changes in magnetic resonance imagingBMC Musculoskelet Disord2014156424588905
- CauleyJABlackDBoonenSHORIZON Pivotal Fracture GroupHORIZON Pivotal Fracture Group. Once-yearly zoledronic acid and days of disability, bed rest, and back pain: randomized, controlled HORIZON Pivotal Fracture TrialJ Bone Miner Res201126598499221542001
- D’AmelioPTamoneCSassiFTeriparatide increases the maturation of circulating osteoblast precursorsOsteoporos Int20122341245125321617993
- DevogelaerJPBoutsenYManicourtDHBiologicals in osteoporosis: teriparatide and parathyroid hormone in women and menCurr Osteoporos Rep20108315416120563900
- IolasconGGimiglianoFMalavoltaNEffectiveness of teriparatide treatment on back pain-related functional limitations in individuals affected by severe osteoporosis: a prospective pilot studyClin Cases Miner Bone Metab20129316116523289031
- NevittMCChenPDoreRKReduced risk of back pain following teriparatide treatment: a meta-analysisOsteoporos Int200617227328016142502
- Fahrleitner-PammerALangdahlBLMarinFFracture rate and back pain during and after discontinuation of teriparatide: 36-month data from the European Forsteo Observational Study (EFOS)Osteoporos Int201122102709271921113576
- LyritisGMarinFBarkerCEUROFORS Study GroupBack pain during different sequential treatment regimens of teriparatide: results from EUROFORSCurr Med Res Opin20102681799180720482322
- SongpatanasilpTMumtazMChhabraHYuMSorsaburuSBack pain in patients with severe osteoporosis on teriparatide or antiresorptives: a prospective observational study in a multiethnic populationSingapore Med J201455949350125273935
- ManueleSSorbelloLPuglisiNThe teriparatide in the treatment of severe senile osteoporosisArch Gerontol Geriatr200744Suppl 124925817317460
- MeunierPJRouxCSeemanEThe effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosisN Engl J Med2004350545946814749454
- BonnelyeEChabadelASaltelFJurdicPDual effect of strontium ranelate: stimulation of osteoblast differentiation and inhibition of osteoclast formation and resorption in vitroBone200842112913817945546
- KaufmanJMAudranMBianchiGEfficacy and safety of strontium ranelate in the treatment of osteoporosis in menJ Clin Endocrinol Metab201398259260123341486
- NegriALSpivacowFRHealing of subtrochanteric atypical fractures after strontium ranelate treatmentClin Cases Miner Bone Metab20129316616923289032
- MeunierPJRouxCOrtolaniSEffects of long-term strontium ranelate treatment on vertebral fracture risk in postmenopausal women with osteoporosisOsteoporos Int200920101663167319153678
- RingeJDDorstAFarahmandPEfficacy of strontium ranelate on bone mineral density in men with osteoporosisArzneimittelforschung201060526727220533764
- CianferrottiLD’AstaFBrandiMLA review on strontium ranelate long-term antifracture efficacy in the treatment of postmenopausal osteoporosisTher Adv Musculoskel Dis201353127139
- CranneyATugwellPZytarukNOsteoporosis Methodology Group and The Osteoporosis Research Advisory GroupMeta-analyses of therapies for postmenopausal osteoporosis. VI. Meta-analysis of calcitonin for the treatment of postmenopausal osteoporosisEndocr Rev200223454055112202469
- DownsRWJrBellNHEttingerMPComparison of alendronate and intranasal calcitonin for treatment of osteoporosis in postmenopausal womenJ Clin Endocrinol Metab20008551783178810843152
- ShibataKTakedaMItoATakedaMSagaiHOvariectomyinduced hyperalgesia and antinociceptive effect of elcatonin, a synthetic eel calcitoninPharmacol Biochem Behav19986023713769632219
- BlauLAHoehnsJDAnalgesic efficacy of calcitonin for vertebral fracture painAnn Pharmacother200337456457012659616
- ScharlaSOertelHHelsbergKKesslerFLangerFNickelsenTSkeletal pain in postmenopausal women with osteoporosis: prevalence and course during raloxifene treatment in a prospective observational study of 6 months durationCurr Med Res Opin200622122393240217257453
- PapadokostakisGKatonisPDamilakisJHadjipavlouADoes raloxifene treatment influence back pain and disability among postmenopausal women with osteoporosis?Eur Spine J2005141097798115834592
- Macías-HernándezSIChávez-AriasDDMiranda-DuarteACoronado-ZarcoRDiez-GarcíaMPPercutaneous vertebroplasty versus conservative treatment and rehabilitation in women with vertebral fractures due to osteoporosis: a prospective comparative studyRev Invest Clin20156729810325938842
- MetcalfeDThe pathophysiology of osteoporotic hip fractureMcgill J Med2008111515718523524
- MearsSCManagement of severe osteoporosis in primary total hip arthroplastyGeriatr Orthop20132299104
- GewandterJSDworkinRHTurkDCResearch designs for proof-of-concept chronic pain clinical trials: IMMPACT recommendationsPain201415591683169524865794

