Abstract
A systematic review of the literature on the use of regional anesthesia (RA) and patient-controlled analgesia (PCA) was conducted in patients who require orthopedic extremity procedures to determine whether either analgesic technique contributes to a delayed diagnosis of compartment syndrome (CS). A total of 34 relevant articles (28 case reports and six research articles) were identified. Of all case report articles published after 2009, the majority (75%) concluded that RA does not put the patient at an increased risk of a delayed diagnosis of CS. Of these, only two relevant prospective research studies focusing on RA or PCA and their relationship to CS were identified. Neither study resulted in any cases of CS. However, both had relatively small sample sizes. Given the lack of evidence identified in this systematic review, prospective studies or large-scale retrospective data reviews are needed to more strongly advocate the use of one modality of analgesia over the other in this patient population.
Introduction
Acute compartment syndrome (CS), a true medical emergency, is a rare, yet serious complication of certain injuries and operations.Citation1,Citation2 It is a condition in which increased pressure within a confined, nonelastic space compromises the circulation and thus the function of the tissues within that space.Citation3 Early recognition and treatment with an emergent fasciotomy is crucial, as the risk of complications such as muscle necrosis,Citation4,Citation5 neurological deficits,Citation3,Citation5,Citation6 delayed fracture union,Citation7 Volkmann ischemic contraction,Citation8 myoglobinuria,Citation8–Citation10 renal failure,Citation8–Citation12 and potentially deathCitation10,Citation11,Citation13 increases as time of tissue anoxia elapses.Citation14–Citation17 The diagnosis of CS is clinical and requires a high index of suspicion.Citation6,Citation18,Citation19 Classical symptoms of CS include pain,Citation13,Citation20–Citation25 pallor,Citation25,Citation26 paresthesias,Citation20,Citation24,Citation25,Citation27 pulselessness,Citation24 and paralysis.Citation23,Citation24 Of these cardinal signs and symptoms, pain is believed to be one of the first clinical indicators of an impending CS.Citation11,Citation24,Citation28,Citation29 Specifically, when a patient experiences pain that is progressive, not relieved by narcotics, out of proportion to examination, and with passive motion, the clinician should be attuned to the possibility of CS.Citation13,Citation21,Citation24 Regional analgesia or regional anesthesia (RA) is often used to alleviate pain in patients who have had limb injuries or interventions.Citation1,Citation30,Citation31 RA has long been the accepted practice for providing postoperative pain control in elective orthopedic procedures, particularly total joint arthroplasties, despite the risk of CS.Citation32,Citation33 There are several benefits to using RA in these patients, such as better pain control,Citation1,Citation34 saving time and costs due to shorter hospital stays and fewer nursing interventions,Citation32 and sparing patients the adverse effects of systemic opioidsCitation32 and general anesthesia.Citation1 However, some argue that RA masks the ischemic pain associated with CSCitation32,Citation35–Citation37 and therefore delays the diagnosis, putting the patient at greater risk for complications.Citation3,Citation38
Patient-controlled analgesia (PCA) is a widely accepted technique for orthopedic postoperative pain management,Citation38–Citation40 despite the risk of CS development. The main advantage of this technique is that patients control their own dosing.Citation40,Citation41 PCA provides better matching of patient need with analgesia and avoids opioid overdose and side effects.Citation41 However, it has also been argued that PCA may mask the symptoms of CS and potentially delay the diagnosis.Citation38–Citation40
Some physicians dispute the use of RA in orthopedic injuries, believing that this modality poses a greater risk than PCA for masking the signs/symptoms of CS.Citation24 Given this controversy, we decided to conduct a systematic review of the literature to compare the two pain control modalities (RA and PCA). Specifically, we set out to compare their contribution to a delayed diagnosis of CS in traumatic and elective orthopedic cases.
In our initial search, we identified 19 relevant review articles published between 1999 and 2014,Citation19,Citation23,Citation24,Citation27,Citation31,Citation42–Citation55 with three of these being case reports that included literature reviews.Citation43,Citation47,Citation51 However, none followed the currently accepted rigorous guidelines for conducting systematic reviews of the literature, including teams of reviewers or an iterative abstraction process.Citation56–Citation59 In addition, none answered our primary question as to whether RA or PCA contributes to a delayed diagnosis of CS in traumatic and elective orthopedic cases. Thus, we proceeded with a systematic review of the literature.
Methods
Literature search
We conducted a thorough and systematic review of English language literature published on the use of RA or PCA in orthopedic cases involving extremity surgeries and that include CS, between January 1, 1980, and November 2014 using CINAHL, PubMed, and Scopus.
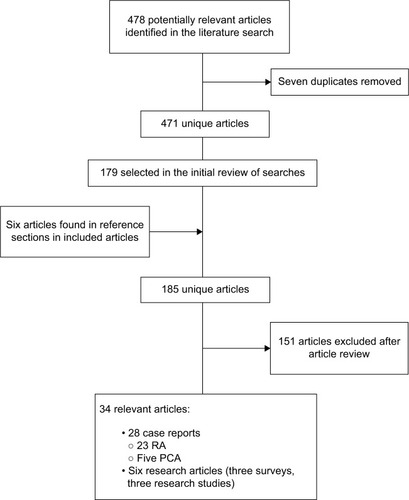
For the searches, we chose relevant controlled vocabulary and keywords to capture the concepts of RA or PCA “and” CS (complete details of the search strategy are available upon request from the authors, or in ). The search strategy identified 471 unique articles (478 total, with seven duplicates).
Table 1 Literature search methods and results for a systematic review of RA or PCA and CS
All titles were reviewed by two teams of trained reviewers for possible inclusion (EBSD and BNH; LJ and AHM). Prior to beginning the review, both reviewers agreed to err on the side of inclusion. If either reviewer selected a reference, the full text was ordered for further review. Using this strategy, 179 articles were obtained for further review. The percent agreement on initial independent selection of articles for further review was 86%. Interrater reliability using Cohen’s kappa was κ=0.67, P<0.001. The reference sections of all included articles were checked for additional potentially relevant articles, with six being identified ().
Inclusion and exclusion criteria
Articles meeting the following criteria were eligible for review: English language; published between January 1, 1980, and November 2014; focused on RA or PCA used after an orthopedic surgical procedure that also included CS in an extremity; patients aged 13 years or older; and all types of research studies and case reports. Exclusion criteria included pediatric cases aged 0–12 years of age; CS not in an extremity (ie, gluteal and abdominal) or resulting from the lithotomy position; orthopedic surgeries not involving the extremities; and letters, editorials, or commentaries.
Research studies and case reports
Teams of two independent researchers (LJ, AHM, BNH, and LEN) checked all articles for initial relevance and assigned each article to one or more categories: research study or case report. Then, a subgroup of the research team (EBSD, LAR, LJ, and AHM) met to review all included articles to determine the final inclusion and accuracy of category assignment.
Abstraction process
Trained reviewers used an iterative process to develop an abstraction form designed to confirm the final eligibility for full review, assess article characteristics, and extract data relevant to the study question. This iterative process started with two initial forms, one for case reports and one for research articles. Both forms were used by multiple reviewers (BNH, AHM, LJ, and LEN) to independently abstract data from the articles. The reviewers then met with their mentor for this study (LAR) to discuss the abstraction forms, to decide whether the form should be revised, and receive guidance related to any abstraction questions. More relevant forms were then created for abstraction. This iterative process continued until the team was confident that the abstraction forms had fields for all potentially relevant information and the team no longer had questions about abstraction of these articles.
Results
We identified 477 articles in our search and deemed 34 of them relevant to our study: 28 case reports (23 RA case reports and five PCA case reports) and six research articles (three surveys and three research studies; ).
Research studies
We identified six relevant research studies (three survey and three research studies) published between 1989 and 2012.Citation11,Citation60–Citation64 Of six research studies, three (50%) authors concluded that the use of either RA or PCA does mask the symptoms of CS,Citation11,Citation60,Citation61 one (16.7%) concluded that RA does not mask the symptoms of CS,Citation62 and two (33.3%) were unclear or did not provide relevant conclusions.Citation63,Citation64
Three (50%) were survey studies conducted in the UK.Citation11,Citation61,Citation62 Davis et alCitation11 conducted a mail-in survey of the practices of 146 consultant and 97 non-consultant grade anesthetists. The majority, 81% and 91%, respectively, replied that they use RA in all lower extremity fractions and 17% and 9%, respectively, had personally witnessed CS masked by the RA. The authors raised concerns over these regional practices, some of which were reported to be in settings without adequate compartment pressure monitoring, though no specifics about the regional techniques, medications, or cases were discussed in the survey. Thonse et alCitation61 administered questionnaires with seven clinical vignettes describing patients undergoing surgery of an extremity (elective and trauma) to 190 orthopedic surgery and anesthetist trainees. Subjects were not aware that the study was focused on the risk of delayed diagnosis of CS. A total of 114 (60%) responded, 56 of which were orthopedic surgeons and 58 anesthesiologists. They found statistically significant differences between the two groups, with anesthetists preferring local and regional nerve blocks in patients known to have a high risk of CS. In 2009, Pennington et alCitation62 conducted a telephone survey of middle-grade physicians in 171 acute care hospitals providing trauma care. Questions focused on departmental protocols and respondent experience with femoral nerve blocks for lower limb fractures. They achieved a 100% response rate and concluded that femoral nerve block is an underutilized, effective mode of analgesia following femoral fractures. Respondents reported a low incidence of CS, but urged vigilance in monitoring patients with high-energy injuries.
There were three (50%) studies conducted in the US.Citation60,Citation63,Citation64 One (33.3%) was a retrospective review conducted prior to 2000.Citation60 Iaquinto et alCitation60 reviewed 63 patients with surgical repair of a tibial fracture. These patients received postoperative epidural analgesia with local anesthetics. None of these patients developed CS.
There were two (66.7%) prospective studies.Citation63,Citation64 Weller et alCitation63 conducted the only prospective randomized study comparing epidural to patient-controlled intravenous morphine following joint replacement (total hip and knee replacement) surgery. Half (15/30) received epidural morphine and the other half (15/30) received patient-controlled intravenous morphine. They followed patients for 24 hours, during which none of the patients developed CS. This prospective study focused on the pain control and side effects of the two delivery methods of morphine but has limited relevancy to our question as there were no cases of CS discovered. In addition, the postoperative follow-up focused on intravenous and epidural morphine use with the only local anesthetic used for short-term surgical anesthesia and not postoperative analgesia. Ganesh et alCitation64 prospectively followed 217 pediatric patients, 167 of whom were children aged ≥13 years and had continuous peripheral nerve blockade after orthopedic procedures. Again, none of these patients developed CS.
Case reports
We identified 28 case report articles published between 1986 and 2013: 23 RA articles, with 29 cases and five PCA articles, with eight cases ( and ). Of 23 RA articles, 13 (56.5%) authors (representing 19 cases) concluded that RA masked the symptoms of CS,Citation32,Citation34–Citation36,Citation65–Citation74 delaying the diagnosis. However, of these 19 cases, eleven (57.8%) presented with “pain” (± other symptoms).Citation32,Citation35,Citation65,Citation67–Citation70,Citation74 In addition, while eight (42.1%) cases did not report pain, they did present with other classic symptoms of CS, such as paresthesia, altered sensation, swelling and edema, tense and shiny skin, loss of movement, or foot drop ().Citation36,Citation66,Citation71–Citation73
Table 2 Case reports identified in a systematic review of the literature on RA and CS (23 articles, with 29 cases), 1980 to November 2014
Table 3 Case reports identified in a systematic review of the literature on PCA and CS (five articles, with eight cases), 1980 to November 2014
In the remaining ten RA articles described with all available details in , eight (80%) authors (representing eight cases) concluded that RA did not mask the symptoms of CS,Citation3,Citation33,Citation47,Citation51,Citation75–Citation78 while two (20%) authors (representing two cases) provided unclear conclusions on this question.Citation20,Citation79 Eight of the 23 RA articles (34.8%) were published between 2010 and 2013.Citation3,Citation33,Citation47,Citation51,Citation67,Citation75,Citation77,Citation79 The majority of these more current articles (six of eight; 75%) did not conclude that RA masks symptoms of CS ().Citation3,Citation33,Citation47,Citation51,Citation75,Citation77
Of the five articles that describe the use of PCA, representing eight total cases detailed in , three (60%) of these authors (six cases) concluded that PCA does mask CS.Citation38–Citation40 The other two authors (two cases) were unclear on this issue ().Citation80,Citation81
Overall, of the 28 combined (RA and PCA) case report articles (representing 37 cases), 22 cases (59.5%) presented with pain (± other symptoms).Citation3,Citation32,Citation33,Citation35,Citation38,Citation47,Citation51,Citation65,Citation67–Citation70,Citation74–Citation76,Citation78,Citation79,Citation80,Citation81 In the remaining 15 cases (40.5%), patients did not present with pain but did present with other classic signs/symptoms of CS ( and ).Citation20,Citation36,Citation39,Citation40,Citation66,Citation71–Citation73,Citation77
The use of RA for trauma and orthopedic surgery remains controversial.Citation24,Citation47,Citation49–Citation51,Citation55 Of the reviewed articles, seven authors recommend that postoperative RA be used cautiouslyCitation65,Citation75 or with a lower dose of local anestheticCitation31,Citation42,Citation50,Citation54,Citation62 in patients who are at risk for the development of a CS, and five believe that nerve block should not be used when there is a possibility of a CS.Citation35,Citation38,Citation44,Citation63,Citation66 In addition, two authors support establishing a protocol or guidelines for the use of inpatient nerve blocks.Citation62,Citation64
Discussion
We conducted a systematic review of the literature on the use of either RA or PCA in orthopedic surgical cases of the extremities. Our goal was to objectively describe the current state of evidence relevant to RA and/or PCA and the development of CS. We identified 34 articles (28 case reports, three surveys, and three research studies). Of these, 19 (55.9%) concluded that RA or PCA does mask symptoms of CS,Citation1,Citation32,Citation35,Citation36,Citation38–Citation40,Citation60,Citation61,Citation65–Citation74 nine (26.5%) concluded that RA or PCA does not mask symptoms,Citation3,Citation33,Citation47,Citation51,Citation62,Citation75–Citation78 and six (17.6%) were unclear.Citation20,Citation63,Citation64,Citation79,Citation81,Citation82
However, 25 articles (73.5%) were published between 1986 and 2009. One could argue that these earlier articles do not accurately reflect current practice. When looking only at eight case report articles published after 2009, the abovementioned percentages markedly change, with one (12.5%) concluding that RA or PCA does mask symptoms of CS,Citation67 six (75%) concluding that RA or PCA does not mask symptoms,Citation3,Citation33,Citation47,Citation51,Citation62,Citation75,Citation77 and one (12.5%) was unclear.Citation79 The change in attribution in more recent publications may be due to advances in ultrasound-guided nerve blocks, making these procedures more desirable as they are often quicker and less technically challenging.Citation83,Citation84 Ultrasound-guided techniques often result in a decreased volume of local anesthetic required to achieve a successful regional block.Citation85,Citation86 In addition, the risk of misdiagnosing CS may be reduced by using continuous RA techniques, with decreased local anesthetic concentrations and using newer local anesthetics drugs.Citation27,Citation33,Citation87 Some authors have noted that ischemic pain is different from nociceptive pain, temperature discrimination, or neuropathic pain, and ischemic pain should not be masked when using RA, even with complete sensory and motor blockade.Citation51
Only two (5.9%) of the 34 identified articles were relevant prospective research studies, and neither of these reported any cases of CS.Citation63,Citation64 Despite this finding, there are possible design issues with these studies. Both had small sample sizes, which leaves open the possibility that they were underpowered to identify a difference. CS incidence has been shown to be 3.1 per 100,000, which makes CS a relatively rare event.Citation3,Citation16 A larger sample size would be required to ensure that a negative study is adequately powered. Most importantly, neither project was specifically designed to look at CS as an end point, but instead reported the lack of any CS cases as a secondary outcome. Thus, these articles were discovered with our literature search despite their only marginal relevance to our question of whether certain anesthesia techniques delay the diagnosis of CS.
On the other hand, a large prospective pediatric study does exist that supports RA.Citation82 This article was excluded from our systematic review based on our age criterion (≥13 years). But its conclusions are relevant, given the paucity of evidence in adult studies. Llewellyn and MoriartyCitation82 conducted a large prospective audit of pediatric patients with more than 10,000 epidurals, concluding that “[t]he occurrence of compartment syndrome does not appear to be masked by the presence of working [epidural infusion analgesia].”
It is evident from our systematic review that there is no clear evidence to support the use of one modality of analgesia over the other with regard to a lessened risk of developing CS. Of the cases that we deemed relevant to our study, the authors only suggested that a given modality either did or did not put the patient at greater risk of developing CS without giving objective means for drawing their conclusions. Still others did not draw a clear conclusion, and some debated whether better monitoring could have prevented the development of CS ( and ).
Some authors advocate for lower concentrations of local anesthetics in regional blockade, which might provide analgesia while improving the detection of CS.Citation31,Citation42,Citation50,Citation54,Citation62 Others advocate improved monitoring.Citation19,Citation27,Citation36,Citation39,Citation65,Citation67,Citation68,Citation71 This could include increased involvement of the RA team in postoperative care,Citation31,Citation49,Citation76 more screening of compartment pressureCitation35,Citation37,Citation65,Citation66 using advanced noninvasive techniques,Citation53 and increased frequency of nursing neurovascular checks.Citation34,Citation48
In addition, recommendations published in 2010 by British military leadership, stated that clinicians in the field should be encouraged to use regional analgesic techniques in limb trauma.Citation88 This recommendation was based on a review of their historical data that found that the majority of CS cases were identified.Citation88
Limitations
The current study is limited by the search strategy used. Specifically, the search terms we identified may not have included every relevant term. Nonetheless, the quality of our systematic review was strengthened by the development of a study protocol at the outset, which included an explicit search strategy and clear inclusion/exclusion criteria. In addition, our search was conducted by a master’s prepared librarian who searched multiple databases, and we reviewed the reference sections of all included articles. Although our strategy minimizes the risk of missing germane articles, it does not eliminate the possibility.
The study question simply cannot be answered with case reports. Scientific inferences cannot be derived from the latter, as the conclusions inevitably contain some biases stemming from the authors and journals. For instance, all case reports that reported that RA masked CSCitation32,Citation35,Citation36,Citation65,Citation66,Citation68–Citation74 were published in surgical journals. Interestingly, most reports that defended RACitation3,Citation33,Citation47,Citation51,Citation77 were published in anesthesiology or pain journals.
Unfortunately, the published literature on this topic identified by our review included only six research studies. In addition, three of these were surveys and the other three were heterogeneous in their methodology and populations. As a result, the evidence is weak at best. Finally, one would expect a highly concentrated RA infusion to have a greater chance of masking CS than a dilute infusion. However, due to the small number of actual research studies, we were not able to address this question.
Our exhaustive systematic review included a search that ended in November 2014. A simple PubMed search using our keywords to date of manuscript submission identified six additional articles that have been published from November 2014 until submission. One is a case report of a 4-year-old boy which would have been excluded from our search based on age.Citation89 Two others were case reports on adults, one with an upper extremity nerve block for distal radius fracture that did not delay the diagnosis of CS and the other a total knee arthroplasty that had an epidural for postoperative pain control that was removed after 24 hours who had CS diagnosed after 48 hours.Citation90,Citation91 Pinheiro et alCitation91 states that though the epidural described above contributed to the delayed diagnosis of CS, it was not the sole cause of the delay.
The PubMed search from November 2014 until submission date resulted in three additional articles, two review articles and one practice advisory. Gadsden and WarlickCitation92 in their review article discuss the use of RA in traumatic extremity injuries and summarized that peripheral nerve blocks do not appear to contribute to a delayed diagnosis of CS while advocating for prudent use of blocks and extra vigilance when they are used. Although a pediatric review article, Muhly et alCitation93 additionally comment that there is “theoretical evidence” that peripheral regional techniques do not hide the ischemic pain symptom of CS and that blocks can be safely used in their pediatric population with appropriate attentiveness and monitoring. The practice advisory was published in September 2015 by the European Society of Regional Anaesthesia and Pain Therapy and the American Society of Regional Anesthesia and Pain Medicine regarding controversial topics in pediatric pain medicine, including RA and CS. Although another pediatric-focused article that does not fit within the scope of our systematic review, it is important to note that these societies advocate for the use of regional anesthetic techniques in pediatric orthopedic procedures and outlines six “best practice rules” for its use, which includes use of reduced concentrations of local anesthetics, reducing the volume of local anesthetics in high-risk surgeries such as those involving the tibial compartment, using caution with additives in blocks, and close follow-up by a pain service with easily accessible compartment pressure monitoring.Citation94
Currently, there are no clear recommendations regarding the use of RA in adult patients with orthopedic extremity procedures who are at increased risk of developing CS.Citation11,Citation27,Citation95 In addition, our search identified cases and opinions suggesting that PCA contributes to a delayed diagnosis of CS. Thus, more studies are needed. Randomized prospective trials may not be appropriate given the lack of convincing evidence and the ongoing controversy regarding the safety of RA in this at-risk population. However, the widespread use of computerized medical records today makes large-scale data mining feasible. This would allow for retrospective data analysis, reviewing all cases of CS, as well as prospective comparison of similar orthopedic practices that use different analgesic techniques.
Acknowledgments
The authors thank Amos J Wright, MLS, Voluntary Associate Professor and Director, Section on the History of Anesthesia, University of Alabama at Birmingham, for his assistance in locating and obtaining articles.
Disclosure
The authors report no conflicts of interest in this work.
References
- AbbalBCapdevilaXThe use of regional anesthesia when the risk of compartment syndrome exists: Yes!DillaneDRegional Anesthesia in the Patient at Risk for Acute Compartment Syndrome. ASRA NewsPittsburgh, PAAmerican Society of Regional Anesthesia and Pain Medicine201346 Available at: https://www.asra.com/content/documents/31513_asra_may2013newsletter.pdfAccessed August 22, 2016
- HastingsHMisamoreGCompartment syndrome resulting from intravenous regional anesthesiaJ Hand Surg Am19871245595623611654
- AguirreJAGreschDPopoviciABernhardJBorgeatACase scenario: compartment syndrome of the forearm in patient with an infraclavicular catheter: breakthrough pain as indicatorAnesthesiology201311851198120523426268
- AnanthanarayanCCastroCMcKeeNSakoticGCompartment syndrome following intravenous regional anesthesiaCan J Anaesth200047111094109811097539
- BlockEFDoboSKirtonOCCompartment syndrome in the critically injured following massive resuscitation: case reportsJ Trauma19953947877917473979
- PatmanRDCompartmental syndromes in peripheral vascular surgeryClin Orthop Relat Res19751131031101192656
- Court-BrownCMcQueenMCompartment syndrome delays tibial unionActa Orthop Scand19875832492523630655
- SheridanGWMatsenFAFasciotomy in the treatment of the acute compartment syndromeJ Bone Joint Surg Am19765811121151249096
- GoldsmithALCompartment syndrome as a complication of the prolonged use of the Lloyd-Davies positionAnaesthesia19965111104810528943599
- KumarVSaeedKPanagopoulosAParkerPJGluteal compartment syndrome following joint arthroplasty under epidural anaesthesia: a report of 4 casesJ Orthop Surg2007151113117
- DavisETHarrisAKeeneDPorterKManjiMThe use of regional anaesthesia in patients at risk of acute compartment syndromeInjury200637212813316256115
- FerreiraTAPensadoADominguezLAymerichHMolinsNCompartment syndrome with severe rhabdomyolysis in the postoperative period following major vascular surgeryAnaesthesia19965176926948758168
- ElliottKGBJohnstoneAJDiagnosing acute compartment syndromeJ Bone Joint Surg Br200385-B5625632
- HarveyEJSandersDWShulerMSWhat’s new in acute compartment syndrome?J Orthop Trauma2012261269970222913965
- ParzialeJRMarinoARHerndonJHDiagnostic peripheral nerve block resulting in compartment syndrome. Case reportAm J Phys Med Rehabil198867282843355680
- WrightJGriffithsDENwabokuHCAcute compartment syndrome with an atypical presentation: a useful clinical lessonJ R Soc Med201123013
- YangJCooperMGCompartment syndrome and patient-controlled analgesia in children – analgesic complication or early warning system?Anaesth Intensive Care201038235936320369773
- Munk-AndersenHLaustrupTKCompartment syndrome diagnosed in due time by breakthrough pain despite continuous peripheral nerve blockActa Anaesthesiol Scand201357101328133024020485
- OlsonSAGlasgowRRAcute compartment syndrome in lower extremity musculoskeletal traumaJ Am Acad Orthop Surg200513743644416272268
- BezwadaHPNazarianDGBoothREJrCompartment syndrome following total knee arthroplasty: a case reportAm J Orthop200534838638816187729
- HayakawaHAldingtonDJMooreRAAcute traumatic compartment syndrome: a systematic review of results of fasciotomyTrauma200911535
- DuckworthADMitchellSEMolyneuxSGWhiteTOCourt-BrownCMMcQueenMMAcute compartment syndrome of the forearmJ Bone Joint Surg Am20129410e6322617929
- LasanianosNGKanakarisNKRobertsCSGiannoudisPVCompartment syndrome following lower limb arthroplasty: a reviewOpen Orthop J2011518119221686323
- MannionSCapdevilaXAcute compartment syndrome and the role of regional anesthesiaInt Anesthesiol Clin20104848510520881529
- CascioBMWilckensJHAinMCToulsonCFrassicaFJDocumentation of acute compartment syndrome at an academic healthcare centerJ Bone Joint Surg Am200587234635015687158
- ErdösJDlaskaCSzatmaryPHumenbergerMVécseiVHajduSAcute compartment syndrome in children: a case series in 24 patients and review of the literatureInt Orthop201135456957520401657
- MarGJBarringtonMJMcGuirckBRAcute compartment syndrome of the lower limb and the effect of postoperative analgesia on diagnosisBr J Anaesth2009102131119022795
- UlmerTThe clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder?J Orthop Trauma200216857257712352566
- HeckmanMMWhitesidesTEGreweSRRooksMDCompartment pressure in association with closed tibial fractures: the relationship between tissue pressure, compartment and the distance from the site of the fractureJ Bone Joint Surg Am1994769128512928077257
- SibellDMMurphyMMayberryJThoracic epidural infusion complicated by epidural compartment syndromeAnesthesiology200398378879012606929
- GanapathySContinuous nerve blocks for orthopedic injuriesTech Reg Anesth Pain Manag2002612732
- HaggisPYatesPBlakewayCCompartment syndrome following total knee arthroplastyJ Bone Joint Surg200688-B3331334
- CometaMAEschATBoezaartAPDid continuous femoral and sciatic nerve block obscure the diagnosis or delay the treatment of acute low leg compartment syndrome? A case reportPain Med201112582382821564511
- GuarinPLBControlling Pain. How effective are nerve blocks after orthopedic surgery? A quality improvement studyNursing20134366366
- HailerNPCompartment syndrome of the calf following total knee arthroplasty – a case report of a highly unusual complicationActa Orthop200778229329517464621
- MorrowBCMawhinneyINElliottJRTibial compartment syndrome complicating closed femoral nailing: diagnosis delayed by an epidural analgesic technique – case reportJ Trauma19943758678687966494
- WhitesidesTEPain: friend or foe?J Bone Joint Surg Am20018391424142511568208
- O’SullivanMJRiceJMcGuinnessAJCompartment syndrome without pain!Ir Med J20029512211928785
- RichardsHLangstonAKulkarniRDownesEMDoes patient controlled analgesia delay the diagnosis of compartment syndrome following intramedullary nailing of the tibia?Injury200435329629815124799
- HarringtonPBunolaJJenningsAJBushDJSmithRMAcute compartment syndrome masked by intravenous morphine from a patient-controlled analgesia pumpInjury200031538738910775698
- BallantyneJCCarrDBChalmersTCDearKBAngelilloIFMostellerFPostoperative patient-controlled analgesia: meta-analyses of initial randomized control trialsJ Clin Anesth1993531821938318237
- RosenbergADBernsteinRLPerioperative anesthetic management of orthopedic injuriesAnesthesiol Clin North America1999171171182
- KaragiannisGHardernRNo evidence found that a femoral nerve block in cases of femoral shaft fractures can delay the diagnosis of compartment syndrome of the thighEmerg Med J20052211814
- PearseMFNanchahalJAcute compartment syndrome: reducing the riskAVMA Med Legal J2008143114118
- ClarkLVarbanovaMRegional anesthesia in traumaAdv Anesth2009271191222
- KeeneDDReaWEAldingtonDAcute pain management in traumaTrauma2011133167179
- WalkerBJNoonanKJBosenbergATEvolving compartment syndrome not masked by a continuous peripheral nerve blockReg Anesth Pain Med201237439339722561421
- BlairVClarkeSNeurovascular assessment post femoral nerve block: nursing (RN) implications on fall preventionInt J Orthop Trauma Nurs20131799105
- ChoiJJLinEGadsdenJRegional anesthesia for trauma outside the operating theatreCurr Opin Anaesthesiol201326449550023673991
- KentMLBuckenmaierCCBattlefield regional anesthesia: evolution and future conceptsTech Reg Anesth Pain Manag201216184189
- KuceraTJBoezaartAPRegional anesthesia does not consistently block ischemic pain: two further cases and a review of the literaturePain Med201415231631924102987
- MannionSRegional anaesthesia for upper limb trauma: a reviewAnestezia regionalǎ pentru traumatismele membrului superior O actualizare20132014959
- SoniSJohannssonHDoes regional anaesthesia in trauma patients lead to delayed recognition of compartment syndrome?Br J Hosp Med2013746358
- TonkovicDAdamVNBaronicaRPavlovicDBDrvarZBogovicTZRegional anesthesia for trauma patientsPeriod Biol20131152139143
- FlemingIEgelerCRegional anaesthesia for trauma: an updateContin Educ Anaesth Crit Care Pain2014143136141
- HemingwayPBreretonN[webpage on the Internet]What is a Systematic Review? Available from: http://www.medicine.ox.ac.uk/ban-dolier/painres/download/whatis/Syst-review.pdfAccessed March 11, 2015
- MoherDLiberatiATetzlaffJAltmanDGThe PRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med200967e100009719621072
- RiesenbergLJusticeEMConducting a successful systematic review of the literature, part 1Nursing2014444131724646574
- RiesenbergLJusticeEMConducting a successful systematic review of the literature, part 2Nursing20144462326
- IaquintoJMPienkowskiDThornsberryRGrantSStevensDBIncreased neurologic complications associated with postoperative epidural analgesia after tibial fracture fixationAm J Orthop19972696046089316721
- ThonseRAshfordRUWilliamsIRHarringtonPDifferences in attitudes to analgesia in post-operative limb surgery put patients at risk of compartment syndromeInjury200435329029515124798
- PenningtonNGaddRJGreenNLoughenburyPRA national survey of acute hospitals in England on their current practice in the use of femoral nerve blocks when splinting femoral fracturesInjury201243684384522029946
- WellerRRosenblumMConardPGrossJBComparison of epidural and patient-controlled intravenous morphine following joint replacement surgeryCan J Anaesth19913855825861934205
- GaneshARoseJBWellsLContinuous peripheral nerve blockade for inpatient and outpatient postoperative analgesia in childrenAnesth Analg200710551234124217959949
- StreckerWBWoodMBBieberEJCompartment syndrome masked by epidural anesthesia for postoperative pain. Report of a caseJ Bone Joint Surg Am1986689144714483782218
- HyderNKesslerSJenningsAGDe BoerPGCompartment syndrome in tibial shaft fracture missed because of a local nerve blockJ Bone Joint Surg1996783499500
- AzamMQAliMSAl RuwailiMAl SayedHNCompartment syndrome obscured by post-operative epidural analgesiaClin Pract201221e1924765418
- UzelAPSteinmannGThigh compartment syndrome after intramedullary femoral nailing: possible femoral nerve block influence on diagnosis timingOrthop Traumatol Surg Res200995430931319501560
- NichollJECalzadaSBonniciAVAnterior compartment syndrome after revision hip arthroplastyJ Bone Joint Surg Br19967858128138836077
- NoorpuriBSShahaneSAGettyCJAcute compartment syndrome following revisional arthroplasty of the forefoot: the dangers of ankle-blockFoot Ankle Int200021868068210966367
- TangWMChiuKYSilent compartment syndrome complicating total knee arthroplasty: continuous epidural anesthesia masked the painJ Arthroplasty200015224124310708095
- AddisonPDLannonDNeliganPCCompartment syndrome after closure of the anterolateral thigh flap donor site: a report of two casesAnn Plast Surg200860663563818520198
- PriceCRibeiroJKinnebrewTCompartment syndromes associated with postoperative epidural analgesia. A case reportJ Bone Joint Surg19967845975998609141
- SeyboldEABusconiBDAnterior thigh compartment syndrome following prolonged tourniquet application and lateral positioningAm J Orthop19962574934968831892
- PatilloDDella RoccaGJMurthaYMCristBDPilon fracture complicated by compartment syndrome: a case reportJ Orthop Trauma2010246e54e5720502205
- KortNPvan RaayJJvan HornJRCompartment syndrome and popliteal vascular injury complicating unicompartmental knee arthroplastyJ Arthroplasty200722347247617400107
- ChidambaranVRosingJSolerXSadhasivamSTrauma from tourniquet (mis)useAnesthesiology2012117117922311093
- DunwoodyJMReichertCCBrownKLCompartment syndrome associated with bupivacaine and fentanyl epidural analgesia in pediatric orthopaedicsJ Pediatr Orthop19971732859150012
- LaReauJMRobbinsCETalmoCTMehioAKPuriLBonoJVComplications of femoral nerve blockade in total knee arthroplasty and strategies to reduce patient riskJ Arthroplasty201227456456821908171
- BaeDSKadiyalaRKWatersPMAcute compartment syndrome in children: contemporary diagnosis, treatment, and outcomeJ Pediatr Orthop200121568068811521042
- MaiDDCompartment syndrome of the right anterior thigh after primary total hip arthroplastyCan J Surg200043322622710851420
- LlewellynNMoriartyAThe national pediatric epidural auditPediatr Anaesth2007176520533
- LucasSDLe-wendlingLEnnekingFK[webpage on the Internet]Regional anesthesia for the trauma patientRaczGPain Management-Current Issues and OpinionsInTech2012261277 Available from: http://www.intechopen.com/books/pain-management-current-issues-and-opinions/regional-anesthesia-for-the-trauma-patientAccessed March 3, 2016
- WuJJLolloLGrabinskyA[webpage on the Internet]Regional anesthesia in trauma medicineAnesthesiol Res Pract201117 Available from: http://www.hindawi.com/journals/arp/2011/713281/Accessed March 3, 2016
- SalinasFVUltrasound and review of evidence for lower extremity peripheral nerve blocksReg Anesth Pain Med201035suppl 2S16S2520216021
- ReidNStellaJRyanMRaggMUse of ultrasound to facilitate accurate femoral nerve block in the emergency departmentEmerg Med Australas200921212413019422409
- KashukJLMooreEEPinskiSJohnsonJLMooreJBMorganSLower extremity compartment syndrome in the acute care surgery paradigm: safety lessons learnedPatient Saf Surg2009311119527510
- ClasperJCAldingtonDJRegional anaesthesia, ballistic limb trauma and acute compartment syndromeJ Army Med Corps201015627778
- SermeusLBoeckxSCamerlynckHSomvilleJVercauterenMPostsurgical compartment syndrome of the forearm diagnosed in a child receiving a continuous infra-clavicular peripheral nerve blockActa Anaesthesiol Belg2015661293226103739
- SoberónJRJrSisco-WiseLEDunbarRMCompartment syndrome in a patient treated with perineural liposomal bupivacaine (Exparel)J Clin Anesth2016311427185666
- PinheiroAAMarquesPMSáPMOliveiraCFda SilvaBPde SousaCMCompartment syndrome after total knee arthroplasty: regarding a clinical caseRev Bras Ortop201550447848126401507
- GadsdenJWarlickARegional anesthesia for the trauma patient: improving patient outcomesLocal Reg Anesth20158455526316813
- MuhlyWTGurnaneyHGGaneshARegional anesthesia for pediatric knee surgery: a review of the indications, procedures, outcomes, safety, and challengesLocal Reg Anesth20158859126609245
- IvaniGSureshSEcoffeyCThe European society of regional anaesthesia and pain therapy and the American society of regional anesthesia and pain medicine joint committee practice advisory on controversial topics in pediatric regional anesthesiaReg Anesth Pain Med201540552653226192549
- JohnsonDJChalkiadisGADoes epidural analgesia delay the diagnosis of lower limb compartment syndrome in children?Paediatr Anaesth2009192839119143952