Abstract
The anterior cutaneous branches of the thoracolumbar spinal nerves enter the rectus sheath at its lateral border and perforate the muscle after travelling a short distance in the ventral direction. In this anatomical case series, we show that dye injection at the medial margin did not lead to reliable impregnation of the target nerves. The local anesthetic should therefore be injected at the lateral edge of the rectus sheath. Preceding surgical procedures to the ventral abdominal wall may affect the craniocaudal spread of local anesthetic.
Basic anatomical knowledge
The skin of the abdominal wall is innervated by the segments Th7 to L2, medially by the mammillary line through the anterior cutaneous branches and laterally by the mammillary line through the lateral cutaneous branches of the associated spinal nerves.Citation1 These are mixed nerves, which also innervate the muscles of the abdominal wall.
The anterior cutaneous branches travel between the transversus abdominis and internal oblique abdominis muscle (). They also branch and communicate widely within the transversus abdominis plane, especially along larger vessels such as the deep circumflex iliac artery (transversus abdominis plane plexus) and the epigastric arteries (rectus sheath plexus). Therefore, all nerves running along the anterior abdominal wall are mixed segmental nerves.Citation2
Figure 1 Transducer position, course of the anterior cutaneous branches (yellow) and instillation of local anesthetic (red).
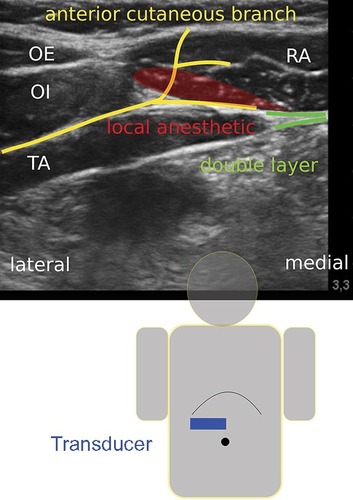
The rectus abdominis muscle is innervated by the segments Th7 to Th12 (Th5 to L1). At the lateral edge of the rectus sheath, the anterior cutaneous branches divide into superficial (innervation of the skin) and deep branches, which enter laterally into the rectus sheath. From that point, they travel a short distance behind the rectus abdominis muscle before perforating ventrally and reaching the innervation area of the anterior abdominal wall. Within the rectus sheath, they give off branches to the posterior aspect of the rectus sheath and to the rectus abdominis muscle (: right side). This muscle is subdivided ventrally by tendinous intersections into several (usually three to four) segments.Citation1 Therefore, local anesthetic must be applied posteriorly to the rectus abdominis muscle and ventrally to a clearly visible double layer in order to achieve a sufficient craniocaudal spread. This double layer consists of the aponeuroses of the transversus and the internal oblique abdominis muscles ().
Methods
The investigations were performed at the Institute of Anatomy, University of Rostock, Germany. Six ultrasound-guided rectus sheath blocks were performed on three unfixed donor cadavers, which had been designated for education or research, using 20 mL of Alcian blue.
The linear transducer (38 mm, 6–13 MHz from Sonosite, Bothell, WA, USA) was placed in the transverse plane between the xiphoid and the umbilicus above the rectus abdominis muscle (). The injections were performed using an in-plane technique either at the medial (in lateral direction) or at the lateral (in medial direction) edge of the rectus abdominis muscle with a SonoPlex® 21G×100 mm cannula from Pajunk, Geisingen, Germany. The ultrasound-optimized needle was placed between the rectus abdominis muscle and the posterior leaf (double layer) of the rectus sheath (: right side, injection from lateral to medial).
Ethical statement
This research was exempt from review by an ethics committee, because it did not include studies on living humans or animals.
Results
The results are summarized in . Injections at the lateral edge of the rectus sheath (first cadaver, right side [1R], second cadaver, right side [2R], third cadaver, left side [3L]) generally resulted in complete impregnation of the target nerves (). An exception to this was observed with preparation 3R. In this case, the rectus abdominis muscle had lipomatous degeneration (as a result of partial denervation) following a conventional cholecystectomy and was adhered to the posterior leaf of the rectus sheath. Therefore, the spread of the dye was restricted in the cranial direction (). Injections from medial to lateral did not result in the staining of the target nerves in both cases (1L and 2L) ().
Figure 2 Anterior cutaneous branches (acb) impregnated by the dye (injection from lateral).
Abbreviations: acb-a, penetrating the posterior leaf of the rectus sheath; acb-b, giving off a branch to the posterior rectus sheath; acb-c, penetrating the rectus abdomins muscle.
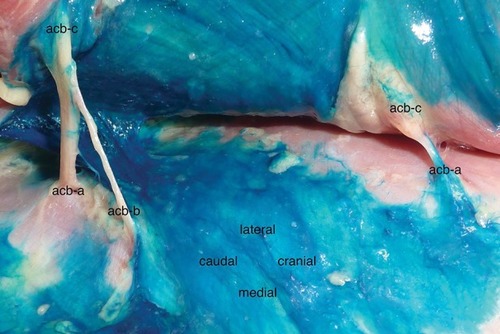
Figure 3 Lipomatous degeneration of the rectus abdominis muscle (“RA”) and restricted spread of the injectant in the cranial direction.
Abbreviation: acb, anterior cutaneous branch.
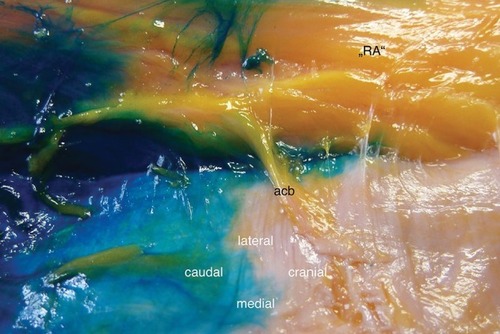
Figure 4 Anterior cutaneous branches (acb) without staining (injection from medial).
Abbreviations: acb-a, penetrating the posterior leaf of the rectus sheath; acb-c, penetrating the rectus abdominis muscle.
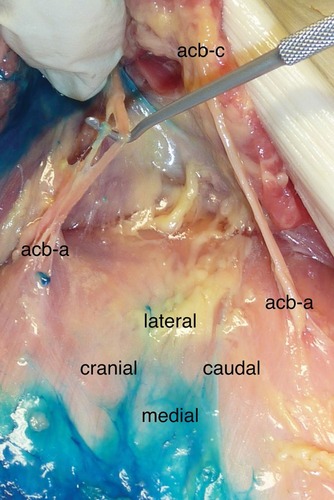
Table 1 Impregnation of the intercostal nerves (anterior cutaneous branches) inside the rectus sheath following the injection of 20 mL Alcian blue
Discussion
Rectus sheath blockades are established analgesic procedures, especially in pediatric anesthesia.Citation3,Citation4 Recent studies show better postoperative analgesia for rectus sheath blocks compared to local wound infiltration for children undergoing umbilical hernia repair.Citation5,Citation6 In relation to adults, the target compartment is small and the local anesthetic may spread more evenly in the craniocaudal and mediolateral direction. However, current studies also describe the intraoperative performance of rectus sheath blocks by the surgeon.Citation7,Citation8
In adults, this technique allows for a minor surgical procedure of the anterior abdominal wall without the need of additional general anesthesia (eg, minor revisions after midline laparotomy, umbilical hernia repair, or insertion of peritoneal dialysis catheters in high-risk patients).Citation9 The sono-anatomic landmarks are clearly defined, and the spread of the injected local anesthetic can be visualized immediately.Citation10 An ultrasound-guided technique potentially avoids complications such as intraperitoneal injection or accidental punctures of the epigastric vessels.Citation11
For truncal blocks, the duration of the blockade has been prolonged by continuous infusion or the use of liposomal bupivacaine in clinical trials or individual cases.Citation12–Citation14 These techniques can provide reasonable analgesia for selective major abdominal procedures when epidural anesthesia is contraindicated. Rectus sheath catheters can be placed in the craniocaudal or lateromedial direction without obstructing the sterile coverage of the surgical area. With regard to an improved or prolonged analgesic effect contradictory results were reported for the addition of dexmedetomidine or dexamethasone to local anesthetics.Citation15–Citation17 In the randomized study by Hamada et al, adding dextran to levobupivacaine decreased the risk of levobupivacaine toxicity (lower plasma concentrations) while providing better analgesia (lower resorption rate).Citation18
Does the chosen approach influence the spread of the injectate and the success rate for rectus sheath blocks? Manassero et al examined the spread of local anesthetic in adult patients undergoing umbilical hernia repair.Citation9 They performed the block (20 mL of levobupivacaine 0.375% + epinephrine 5 μg/mL) at T10-level in a medial to lateral direction, with the aim to deposit the local anesthetic near the lateral border of the rectus sheath. Local anesthetic spread was evaluated ultrasonographically and scored from 0 to 4 (local anesthetic from T9- to T11-level, bilaterally). The overall success rate (no intraoperative supplementation with mepivacaine 1% at cutaneous incision) was 53.3%. In patients with local anesthetic spread score 4 (26.6%), the success rate was 75%. The authors discuss two possible explanations for their results. First, the nerves within the rectus sheath are mixed segmental nerves, due to diverse anastomoses during their course along the anterolateral abdominal wall.Citation2 This requires a larger craniocaudal spread of the injectate within the rectus sheath, which can be achieved by larger local anesthetic volumes, a multi-injection technique, or craniocaudal needle guidance. A second possible cause is aberrant cutaneous branches that are formed before the rectus sheath and run anterior to the rectus abdominis muscle in the subcutaneous tissue.Citation1 These anatomical variants led to the concept of a para-umbilical block.Citation19 Furthermore, a superiority of transversus abdominis plane (TAP) blocks to rectus sheath blocks could be postulated. For postoperative analgesia following umbilical hernia repair in children, the superiority of TAP blocks over rectus sheath blocks has not yet been proven.Citation20
The range of possible regional anesthesia techniques for surgical interventions on the anterolateral abdominal wall is extensive, ranging from neuraxial blocks to local wound infiltration.Citation21–Citation27 These include the intravenous infusion of lidocaine (off-label use), selective nerve blocks (eg, iliohypogastric and ilioinguinal nerve), thoracic-paravertebral, ventral (eg, subcostal transversus abdominis plane and rectus sheath blocks), and dorsal fascial plane blocks. Newer methods (dorsal approach) such as the erector spinae plane and quadratus lumborum block (QLB) have yet to be validated in clinical and anatomical studies. A potential benefit could be the retrograde spread into the thoracic-paravertebral space, as shown in the cadaver study by Dam et al for the transmuscular QLB. This may expand the anesthetic field to include the sympathetic trunk.Citation26,Citation27
The choice of regional anesthesia technique for abdominal surgery is influenced by many factors. Previous operations on the abdominal wall, even outside of the rectus sheath, may compromise the spread of injected local anesthetic. In this situation, alternative procedures should be considered.
Conclusion
For ultrasound-guided rectus sheath blocks, the local anesthetic should be injected at the lateral edge of the rectus sheath, usually at the level of the surgical incision (due to the possibility of restricted craniocaudal spread). A lateral approach avoids the accidental puncture of the epigastric artery.
Acknowledgments
The Helios Research Centre provided financial support for the work.
Supplementary material
Disclosure
The authors report no conflicts of interest in this work.
References
- LoeweneckHFeifelGvon LanzTWachsmuthWPraktische Anatomie [Practical Anatomy] Ein Lehr- und Hilfsbuch der anatomischen Grundlagen ärztlichen HandelnsBerlinSpringer-Verlag20043357 German
- RozenWMTranTMAshtonMWBarringtonMJIvanusicJJTaylorGIRefining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wallClin Anat200821432533318428988
- de Jose MariaBGötzensVMabrokMUltrasound-guided umbilical nerve block in children: a brief description of a new approachPaediatr Anaesth2007171445017184431
- WillschkeHKettnerSPediatric regional anesthesia: abdominal wall blocksPaediatr Anaesth2012221889222077146
- DingemanRSBarusLMChungHKUltrasonography-guided bilateral rectus sheath block vs local anesthetic infiltration after pediatric umbilical hernia repair: a prospective randomized clinical trialJAMA Surg2013148870771323760519
- GurnaneyHGMaxwellLGKraemerFWGoebelTNanceMLGaneshAProspective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repairBr J Anaesth2011107579079521856778
- LitzCNFarachSMFernandezAMPercutaneous ultrasound-guided vs. intraoperative rectus sheath block for pediatric umbilical hernia repair: a randomized clinical trialJ Pediatr SurgIn press2017
- LandmannAVisoiuMMalekMMDevelopment of a novel technique for bilateral rectus sheath nerve blocks under laparoscopic-guidanceJ Pediatr SurgIn press2017
- ManasseroABossolascoMMeineriMUguesSLiarouCBertolacciniLSpread patterns and effectiveness for surgery after ultrasound-guided rectus sheath block in adult day-case patients scheduled for umbilical hernia repairJ Anaesthesiol Clin Pharmacol201531334935326330714
- WebsterKUltrasound-guided rectus sheath block - analgesia for abdominal surgeryUpdate in Anaesthesia2010261217
- AbrahamsMDerbyRHornJLUpdate on ultrasound for truncal blocks: a review of the evidenceReg Anesth Pain Med201641227528826866299
- ShidoAImamachiNDoiKSakuraSSaitoYContinuous local anesthetic infusion through ultrasound-guided rectus sheath cathetersCan J Anaesth201057111046104720803110
- TsuiBCGreenJSIpVHUltrasound-guided rectus sheath catheter placementAnaesthesia201469101174117525204242
- HutchinsJLKeshaRBlancoFDunnTHochhalterRUltrasound-guided subcostal transversus abdominis plane blocks with liposomal bupivacaine vs. non-liposomal bupivacaine for postoperative pain control after laparoscopic hand-assisted donor nephrectomy: a prospective randomized observer-blinded studyAnaesthesia201671893093727238859
- AmmarASMahmoudKMEffect of adding dexamethasone to bupivacaine on transversus abdominis plane blocks for abdominal hysterectomy: a prospective randomized controlled trialSaudi J Anaesth20126322923323162395
- DingWLiWZengXEffect of adding dexmedetomidine to ropivacaine on ultrasound-guided dual transversus abdominis plane block after gastrectomyJ Gastrointest SurgIn press2017
- HuangSHLuJGanHYLiYPengYGWangSKPerineural dexamethasone does not enhance the analgetic efficacy of ultrasound-guided subcostal transversus abdominis plane block during laparoscopic cholecystectomyHepatobiliary Pancreat Dis Int201615554054527733325
- HamadaTTsuchiyaMMizutaniKLevobupivacaine-dextran mixture for transversus abdominis plane block and rectus sheath block in patients undergoing laparoscopic colectomy: a randomized controlled trialAnaesthesia201671441141626919568
- CourregesPPoddevinFLecoutreDPara-umbilical block: a new concept for regional anaesthesia in childrenPaediatr Anaesth1997732112149189966
- ToriiNTachibanaKIwasakiMTakeuchiMKinouchiKUltrasound-guided rectus sheath block vs. transversus abdominis plane block in children undergoing umbilical hernia repairMasui201665656056527483647
- BørglumJGögenürIBendtsenTFAbdominal wall blocks in adultsCurr Opin Anaesthesiol201629563864327429253
- El-BoghdadlyKMadjdpourCChinKJThoracic paravertebral blocks in abdominal surgery – a systematic review of randomized controlled trialsBr J Anaesth2016117329730827543524
- HebbardPDTransversalis fascia plane block, a novel ultrasound-guided abdominal wall nerve blockCan J Anaesth200956861862019495909
- HebbardPDBarringtonMJVaseyCUltrasound-guided continuous oblique subcostal transversus abdominis plane blockade: description of anatomy and clinical techniqueReg Anesth Pain Med201035543644120830871
- WeibelSJokinenJPaceNLEfficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysisBr J Anaesth2016116677078327199310
- ChinKJAdhikarySSarwaniNForeroMThe analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repairAnaesthesia201772445246028188621
- DamMMorigglBHansenCKHoermannRBendtsenTFBørglumJThe pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver studyAnesth AnalgIn press2017
