Abstract
Background
The scope of regional anesthesia fellowship programs has not been analyzed but may provide insights that could improve fellowship training and standards.
Methods
Regional anesthesia fellowship directors across the world were asked to complete a comprehensive survey that detailed the range of educational and practical experience and attitudes as well as assessment procedures offered in their programs.
Results
The survey response rate was 66% (45/68). Overall, the range of activities and the time and resources committed to education during fellowships is encouraging. A wide range of nerve block experience is reported with most programs also offering acute pain management, research, and teaching opportunities. Only two-thirds of fellowships provide formal feedback. This feedback is typically a formative assessment.
Conclusion
This is the first survey of regional anesthesia fellowship directors, and it illustrates the international scope and continuing expansion of education and training in the field. The results should be of interest to program directors seeking to benchmark and improve their educational programs and to faculty involved in further curriculum development.
Keywords:
Background
Interest in regional anesthesia (RA) has enjoyed resurgence in recent years, particularly with the introduction of the portable ultrasound machine.Citation1,Citation2 Quality education and training in RA techniques are essential to ensure safe and effective utilization of these techniques. Research has shown that traditional anesthesia residency programs rarely provide trainees with sufficient clinical experience and training to confidently utilize RA techniques when they begin independent consultant practice.Citation3–Citation5 This learning gap has driven demand for more advanced training. In response, the number of institutions offering fellowship positions in RA has grown, and these programs are available worldwide.
Guidelines for fellowship training in RA were first published by the American Society of RA (ASRA) in 2005.Citation6 The purpose of this effort was to recommend an organizational and educational framework to promote modern and comprehensive fellowship training in RA and pain medicine. The guidelines recommend a number of scholarly and practice-based learning activities, which may be incorporated into a fellowship program. Since there is no requirement to follow these when developing an RA fellowship,Citation7 the clinical and theoretical instruction and range of experience offered across programs may vary widely.
The purpose of this study is to survey RA fellowship directors around the world. The primary aim is to establish the range, consistency, and quality of education programs and experience available in these programs. The secondary aims are to illuminate the major barriers to establishing formalized teaching programs and to gauge expert opinion on the most important educational objectives and resources for RA fellows. We postulate that there is a highly variable approach to RA education and experience across fellowship programs, which may affect the quality of the fellowship experience. This data will be of interest worldwide to fellowship directors seeking to benchmark and improve their educational programs and to faculty involved in further curriculum development. The results will also be of interest to potential fellows who need a standard when choosing programs.
Methods
Ethics approval to undertake a survey of worldwide RA fellowship directors was obtained from the Sunnybrook Health Sciences Center research ethics board. Directors of all RA fellowship programs known to the authors from around the world were asked to complete the survey. Potential participants were identified from the ASRA database for RA fellowships, comprehensive Google searches for international RA fellowship positions (keywords: “regional anesthesia” and “fellowship”), and word-of-mouth referral, starting from those known to the authors. Eligible respondents were required to have a RA fellowship program in place at the time of completion of the survey. Participants were aware that the information they provided would be held individually confidential but that the pooled information would be analyzed and undergo publication.
Fellowship directors were contacted by email and asked to complete an Internet-based survey.Citation8 Initial emailing was conducted in November 2011. The survey was open for 60 days, and nonresponders received a first reminder email after 15 days and a final reminder after 40 days.
The survey was organized into six major sections: (1) demographic information (country, fellowship positions per year, years of fellowship, experience of faculty); (2) educational experience (time allocated, range of didactic and practical education activities, availability of educational resources, involvement of nonanesthesia personnel in education); (3) attitudes toward education (importance, optimum time to be allocated, rating the usefulness of various educational activities); (4) extent of experience in peripheral blockade (range and quantity, level of supervision); (5) extent of nontechnical experience (research, teaching, acute pain service, pediatric and obstetric experience); and (6) fellow assessment (whether a formal assessment process exists and how often, what methods are utilized, and what is the best means for assessment).
Data from the survey were collected into a database (Microsoft Excel 2011; Microsoft Corporation, Redmond, WA, USA) for analysis. The data was summarized by proportions and percentages or median and interquartile range (IQR). Data are rounded to the nearest whole.
Results
Sixty-eight international RA fellowship directors were contacted (USA, 39; Canada, 11; UK/Ireland, 6; Europe, 2, Australia/New Zealand, 10). A total of 45 responses were returned, for an overall response rate of 66%. Three respondents did not have a RA fellowship program and were therefore excluded resulting in a report based on 42 international RA fellowship directors. Not all respondents answered every question. For questions where there were less than 42 responses, proportions, and calculation of percentages were based on the number of answers to each question.
Respondent characteristics
The distribution and characteristics of respondents are shown in . No responses were obtained from continental Europe; otherwise, respondents represent a good spread of international RA fellowship programs, albeit with the greatest proportion from North America. Over 80% of programs offer only one to two positions per year. Although 50% of programs have been established for 5 or more years, there are still a number of newer programs appearing. Almost 90% of programs had at least one staff anesthesiologist who had completed formal RA fellowship training. The RA workload varied widely across the surveyed institutions, ranging from 200 to 25,000 RA procedures performed per year, with a median of approximately 4000 (IQR 2655–5344).
Table 1 Respondent characteristics
Education
On a five-point Likert scale, rating the overall importance of a formal education program during RA fellowship training, 14/41 (34%) rated it as “extremely important,” 10/41 (24%) “very important,” 13/41 (32%) “moderately important,” 4/41 (10%) “slightly important,” and 0/41 “not at all important.” Only two programs (5%) did not allocate any time for educational activities (not including research). While 13 programs (31%) provided 8 or more hours of education per week, the median time allocated was 5 hours per week (IQR 2–8 hours). When asked, “How many hours per week should be scheduled for RA education sessions?” only 1/41 respondents (2%) selected “none,” with a median of 4 hours (IQR 1–7 hours). A wide range of educational activities, resources, and personnel are utilized across the surveyed fellowship programs (see ). The most common didactic activity was journal club and evidence-based medicine review in 34 (81%) programs, while live model sonography was the most common practical education activity, utilized in 35 (83%) programs. Twenty-six (62%) utilized nonanesthesia staff in the delivery of their educational program, with pain specialists most commonly involved. The pooled average rating of importance for each educational activity is presented in . Live model sonography workshops were rated as the most important overall teaching method for RA fellowships.
Figure 1 Education activity versus mean rating of importance.
Abbreviation: EBM, evidence-based medicine.
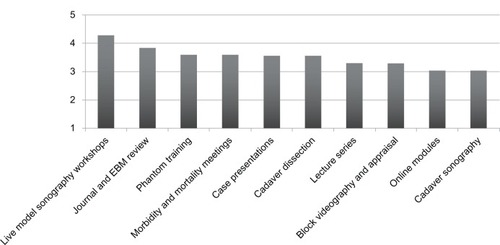
Table 2 Educational activities, resources, and personnel
Experience
The number of blocks (excluding neuraxial) performed or supervised by fellows varied widely. Although most participated in more than 15 blocks per week, a number of programs offered less experience (see ). Of the blocks performed by fellows, the majority were supervised by staff anesthesiologists. In 29/41 (71%) of programs, fellows kept a compulsory logbook of block experience. The extent of fellow block experience is presented in . Of the techniques surveyed, the femoral nerve block is the most commonly performed lower limb block, and the interscalene block is the most commonly performed upper limb block. Most fellowship programs offered RA experience outside orthopedic surgery, with vascular, thoracic, and pediatric experience being the most common (see ). Almost all fellows participated in acute pain service rounds, resident RA teaching, and research activities during their program. When offered, the time allocated for research activities was 0.5 day per week in 11/34 (32%), 1 day in 19/34 (56%), 2 days in 3/34 (9%), and more than 2 days per week in 1/34 (3%).
Figure 2 Nerve blocks versus mean experience offered during fellowship. The y-axis represents the respondent’s claimed frequency of practice for each particular block at their institution with a score of 1 being never performed and a score of 7 being commonly performed.
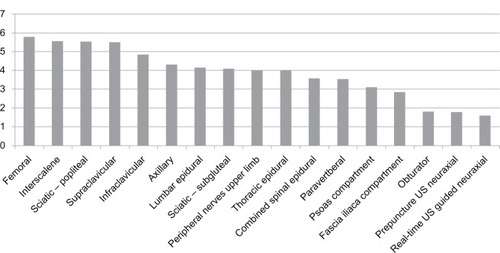
Table 3 Clinical and nonclinical experience
Evaluation
Most programs had processes for formal evaluation of their fellows (see ). Feedback was usually provided every quarter. Of the various assessment methods surveyed, evaluation by supervising staff anesthesiologists and logbook review were the most commonly used methods in 28/28 (100%) and 22/28 (79%) programs, respectively (see ). Other assessment methods listed by respondents included resident evaluation of fellow teaching and European Society of RA diploma. When asked, “Should there be a standard process for the formal evaluation of RA fellow knowledge and clinical competency?” the majority (32/41) of fellowship directors answered yes. Respondents were asked to rank the usefulness of six methods for fellow assessment. The majority of the respondents to this question (87%) gave “evaluation by supervising staff anesthesiologist,” the highest average rating.
Table 4 Fellow assessment
Discussion
RA fellowships are found across the world, though some fellowships were not identified in this survey. North America accounts for the majority of positions, which suggests that the ASRA plays a central role in providing direction and guidance in RA fellowships locally and internationally. While many regional fellowship programs are now well established, there is still a large number that have emerged over recent years as demand for advanced training in the field continues to grow.
Overall, the range of activities and the time and resources committed to education during RA fellowships is encouraging. Most programs provide a combination of didactic and practical education, with didactic activities being more common. This is not surprising since these sessions, which include lecture series, journal review, or case discussions are inexpensive and are generally easy to schedule. Although didactic teaching has been the tradition in medical education, there is a shift towards greater emphasis on practical education, particularly in the technical disciplines.Citation9 Proficiency in RA necessitates acquisition of technical skills in addition to the theoretical knowledge, and as yet there is no consensus on the best way to acquire this technical competence.Citation10,Citation11
Live model sonography is a popular educational activity among fellowship programs. This too is unsurprising as it is inexpensive and easy to organize, and participants can quickly learn sonographic anatomy, which is fundamental to the practice of ultrasound-guided RA. One limitation is that it does not allow for training in real-time, probe-needle alignment. Cadaveric specimens, appropriately prepared, can be used as a realistic model for ultrasound-guided RA.Citation12 Without time constraints or patient discomfort, confidence and skill in tracking the needle to the target can be achieved in a stress free environment. It is especially useful for the rehearsal of more technically difficult blocks or those that are infrequently encountered. Cadaver sessions are popular with trainees and are a proven educational tool in the anesthetic literature.Citation2,Citation13 Cadaveric sonography is offered in a number of fellowship programs, but it may in some cases prove to be exceptionally difficult to achieve due to cost and inaccessibility. Pooling resources and participants between collaborating institutions may make this a feasible activity for more fellowship programs. On the other hand, advancement in RA simulation technology may fill this learning gap and prove to be more cost effective and easier to administer in the longer term.Citation14
RA fellowships offer a wide range of block experience. In general, there is well-balanced exposure to lower and upper limb techniques. Ultrasound-assisted neuraxial blocks are among the most infrequently performed techniques amongst fellows. There is no consensus on the optimum number of blocks required to achieve competency in RA procedures, yet all programs exceed the minimum standard expected for a typical anesthesia residency program.Citation8 Large variations do exist, with some programs reporting fewer than five blocks per fellow per week. Although we continue to use block numbers performed as a serious measure of competence, as Joseph Neal pointed out in his 2011 Carl Koller address, there are many other important aspects to consider in RA training.Citation15 These features are not easy to measure in a survey. Compared to previous surveys,Citation16 it is encouraging to see improved opportunities for fellow colleagues to acquire experience outside orthopedic RA, with pediatric, thoracic, and obstetric RA commonly seen. Almost all fellows are involved in acute pain service rounds, teaching, and research.
One surprising finding was the high level of direct supervision of fellows during block performance. As a technical discipline, RA requires the acquisition of procedural skills that can only be learned through practice and repetition. How much of this practice should be supervised directly, and how much should be carried out independently are important questions. While close supervision may offer opportunities for bedside teaching and possibly improved block success and safety, it can limit independence and negatively impact confidence and proficiency when fellows transition to autonomous practice.Citation17,Citation18 In a series of studies examining motor learning, individuals who were given feedback after every trial of performing simple tasks learned faster than individuals who were given summary feedback after a series of trials.Citation19–Citation21 Once the feedback was discontinued, however, the individuals who had only received feedback after a group of trials maintained their performance at a much higher level, suggesting that heavily supervised motor learning can limit skill retention and proficiency in the longer term.
Overall two-thirds of programs formally assessed their RA fellows, despite the recommendations of guidelines such as those of the ASRA curriculum. Where fellow assessment was undertaken, the processes seem to be more formative in nature, with staff evaluation universally employed. Nevertheless, at least three-quarters of programs include a practical examination or assessment and 14% hold a theory examination or assessment as part of their evaluation. Logbook review was also commonly utilized although no universal benchmark for adequate scope of experience exists.
The ideal means for fellow assessment is unclear.Citation22 The benefit of formative assessments that primarily focus on subjective feedback of performance is that they promote reflection and typically encourage further learning. The drawback is that the assessments can suffer from bias, produce a wider range of qualitative results based on individual experiences – not necessarily related to the curriculum – and are more difficult to process into a cohesive evaluation. Summative assessments are useful because they can act as an incentive for learning a specified curriculum and can effectively shape a standardization process.Citation23 Disadvantages of summative assessments are they can be expensive and complex to introduce and maintain, and they tend to ossify the learning experience leading trainees to become focused on knowing only what is necessary to pass an exam or to achieve a particular set of objectives to the detriment of the spirit of learning and research.
The majority of the respondents (78%) would favor a standardized evaluation process that would require them to prepare their RA fellows for a summative end of training assessment.Citation24 Instituting standard assessments (eg, an international exam) for RA fellows may appear, on the surface, a simple and robust process that could be relatively easily administered. There would, nonetheless, be some major drawbacks. Cooperation and agreement between stakeholders would be a challenge. Cost and administration are also key logistical barriers. Perhaps more importantly, what is the value of theoretical examination in a field where practical skills and technical ability play an equal or more vital role in proficiency? Even if a simple and effective means to ensure standards in RA fellowship education could be agreed upon, this might not necessarily advance the field. An evolution in this direction may foster a culture of exclusivity that could limit growth of the field and ultimately decrease the likelihood for patients to benefit from a larger pool of physicians who have the skills and confidence to utilize RA.
Limitations
Despite the great lengths taken to identify every RA fellowship program worldwide, there are undoubtedly a number that were missed. Although ASRA publishes a list of all their affiliated fellowships, even this list was not comprehensive. We were not able to identify any such consolidated listings outside North America, so we relied on internet searches and word-of-mouth for identification. Almost certainly underrepresented are RA fellowships in non-English-speaking countries.
This study had a response rate of 66% which is very good compared to the average rate for online surveys of 12%–26% reported by Scott et al;Citation25 there is also an even distribution of respondents across different countries. These results, nevertheless, may contain bias if (1) fellowships with poorer education and experience chose not to respond or (2) responders reported favorably to disguise inadequacies in their programs; both cases would lead to overly positive results. Also, the response may be biased by structural variations in training; Europe for instance does not have as many dedicated regional fellowships as North America, but clinical training in RA is achieved in many centers to a high standard during “residency” or postgraduate clinical training. Inconsistent reporting may compromise the transparency and reproducibility of survey reports as well.Citation26 A concurrent survey of the RA fellows themselves might provide a more frank opinion on the quality of the fellowship experience, but it too would suffer from inherent bias and would present greater logistical challenges to complete. A further limitation is that there is no control and comparison group. The survey of RA fellows by Neal et alCitation16 in 2005 cannot be fairly used, given the different questions asked and the separation of time. The authors feel obliged to acknowledge that their own fellowship program and fellowship programs with shared academic affiliations were included in this study.
Conclusion
This survey illustrates the international scope and continuing expansion of education in the field of RA and points toward a promising future for this subspecialty. The results should be of interest to RA fellowship directors seeking to benchmark and improve their programs, and to faculty involved in further curriculum development. While the survey also demonstrates that there are key experiences common across RA fellowship programs, wide variation does exist. Any effort toward the promotion of standards across RA fellowship programs must closely consider the nature and significance of this variation.
Curriculum guidelines have yet to demonstrate improved outcomes in medical education and training,Citation27,Citation28 and even when curricula are published it is not always mandatory to follow them. Have curriculum guidelines such as those established by ASRA helped to achieve a more comprehensive and standard RA fellowship model? It is hard to say without comparative data. Nevertheless, our survey suggests that the majority of programs offer RA fellows a broad range of educational and practical experience. For the foreseeable future, individual institutions will be responsible for maintaining the quality of their program and ensuring appropriate standards are achieved by their RA fellows.
Disclosure
The authors report no conflicts of interest in this work.
References
- SitesBDNealJMChanVUltrasound in regional anesthesia: where should the “focus” be set?Reg Anesth Pain Med200934653153319901765
- MarhoferPHarrop-GriffithsWKettnerSCKirchmairLFifteen years of ultrasound guidance in regional anaesthesia: part 1Br J Anaesth2010104553854620364022
- BartusseckEFatehiSMotschJGrauTSurvey on practice of regional anaesthesia in Germany, Austria, and Switzerland. Part 1: quality assurance and training conceptsAnaesthesist2004539836846 German15235789
- KopaczDJNealJMResidency training: the year 2000Reg Anesth Pain Med200227191411799499
- SmithMPSprungJZuraAMaschaETetzlaffJEA survey of exposure to regional anesthesia techniques in American anesthesia residency training programsReg Anesth Pain Med199924111169952089
- HargettMJBeckmanJDLiguoriGANealJMEducation Committee in the Department of Anesthesiology at Hospital for Special SurgeryGuidelines for regional anesthesia fellowship trainingReg Anesth Pain Med200530321822515898023
- Regional Anesthesiology and Acute Pain Medicine Fellowship Directors GroupGuidelines for fellowship training in Regional Anesthesiology and Acute Pain Medicine: Second Edition, 2010Reg Anesth Pain Med201136328228821519314
- SurveyMonkeyCreate surveys. Get answers Available from: http://www.surveymonkey.comAccessed May 01, 2013
- SmithHMKoppSLJacobAKTorsherLCHeblRDesigning and Implementing a Comprehensive Learner–Centered Regional Anesthesia CurriculumReg Anesth Pain Med2009342889419282705
- BrökingKWaurickRHow to teach regional anesthesiaCurr Opin Anaesthesiol200619552653016960486
- KesslerJBolgerAFGrayATAn essential skillReg Anesth Pain Med200631649850017138190
- TsuiBCDillaneDPillayJRamjiAKWaljiAHCadaveric ultrasound imaging for training in ultrasound-guided peripheral nerve blocks: lower extremityCan J Anaesth200754647548017541078
- LirkPColvinJMBieblMEvaluation of a cadaver workshop for education in regional anesthesiaAnaesthesist2005544327332 German15711813
- ShortenGDO’SullivanOSimulation for training in ultrasound-guided peripheral nerve blockadeInt Anesthesiol Clin2010484213320881524
- NealJMEducation in regional anesthesia; caseloads, simulation, journals, and politics: 2011 Carl Koller lectureReg Anes Pain Med2012376647652
- NealJMKopaczDJLiguoriGABeckmanJDHargettMJThe training and careers of regional anesthesia fellows – 1983–2002Reg Anesth Pain Med200530322623215898024
- JohnsonTCounterbalancing clinical supervision and independent practice: case studies in learning thoracic epidural catheter insertionBr J Anaesth2010105677277620739323
- KennedyTJRegehrGBakerGRLingardLAProgressive independence in clinical training: a tradition worth defending?Acad Med200580Suppl 10S106S11116199447
- SchmidtRAYoungDESwinnenSShapiroDCSummary knowledge of results for skill acquisition: support for the guidance hypothesisJ Exp Psychol Learn Mem Cogn19891523523592522520
- SchmidtRAYoungDEMethodology for motor learning: a paradigm for kinematic feedbackJ Mot Behav1991231132414766528
- SchmidtRALeeTDAugmented feedbackMotor Control and Learning: A Behavioral Emphais5th edChampaign, ILHuman Kinetics2011393405
- EpsteinRMAssessment in medical educationN Engl J Med2007356438739617251535
- GlickmanCDGordonSPRoss-GordonJMSuperVision and Instructional Leadership: A Developmental Approach7th edBoston, MAAllyn and Bacon2009
- BodenhamAREditorial II: Ultrasound imaging by anaesthetists: training and accreditation issuesBr J Anaesth200696441441716549625
- ScottAJeonSHJoyceCMA randomised trial and economic evaluation of the effect of response mode on response rate, response bias, and item non-response in a survey of doctorsBMC Med Res Methodol20111112621888678
- StoryDAGinVna RanongVPoustieSJonesDANZCA Trials GroupInconsistent survey reporting in anesthesia journalsAnesth Analg2011113359159521778334
- GrabowskiWSReddRACunninghamBEHartshorneMFTimmonsJHTruwitCLA categorical course curriculum for radiology residenciesInvest Radio11988234312315
- ChudgarSMCoxCEQueLGAndolsekKKnudsenNWClayASCurrent teaching and evaluation methods in critical care medicine: has the Accreditation Council for Graduate Medical Education affected how we practice and teach in the intensive care unit?Crit Care Med2009371496019050627