Abstract
Introduction
Rib fractures are a common sequelae of chest trauma and are associated with significant morbidity. The erector spinae nerve block (ESB) has been proposed as an alternative first-line regional technique for rib fractures due to ease of administration and minimal complication profile. We aimed to investigate the current literature surrounding this topic with a focus on pain and respiratory outcomes.
Methods
A comprehensive literature search was performed on the Medline, Embase, Web of Science, Scopus, and Cochrane databases. Keywords of “erector spinae block” and “rib fractures” were used to form the search strategy. Papers published in English investigating ESB as an analgesic intervention for acute rib fracture were included. Exclusion criteria were operative rib fixation, or where the indication for ESB was not rib fracture.
Results
There were 37 studies which met the inclusion criteria for this scoping review. Of these, 31 studies reported on pain outcomes and demonstrated a 40% decrease in pain scores post administration within the first 24 hours. Respiratory parameters were reported in 8 studies where an increase in incentive spirometry was demonstrated. Respiratory complication was not consistently reported. ESB was associated with minimal complications; only 5 cases of haematoma and infection were (incidence 0.6%) reported, none of which required further intervention.
Discussion
Current literature surrounding ESB in rib fracture management provides a positive qualitative evaluation of efficacy and safety. Improvements in pain and respiratory parameters were almost universal. The notable outcome from this review was the improved safety profile of ESB. The ESB was not associated with complications requiring intervention even in the setting of anticoagulation and coagulopathy. There still remains a paucity of large cohort, prospective data. Moreover, no current studies reflect an improvement in respiratory complication rates compared to current techniques. Taken together, these areas should be the focus of any future research.
Introduction
Rib fractures are a common sequelae of blunt thoracic trauma and are associated with significant morbidity and mortality.Citation1 These injuries are more common in older, frail patients with multiple medical co-morbidities who often suffer poorer clinical outcomes. Suboptimal analgesia can lead to severe impairment of normal respiratory mechanics, with reduced tidal volumes and difficulty clearing pulmonary secretions contributing to atelectasis, hypoxia, pneumonia, and eventual respiratory failure.Citation2 This is particularly challenging in an elderly population where surgical intervention or admission to a high dependency setting for respiratory support may not be of clinical benefit. Effective analgesia reduces these risks, and to this end, a multimodal regime is often employed, with oral analgesia and intravenous opioid as first-line options, followed by administration of regional blockade.Citation3 Each method is associated with risks, such as sedation and respiratory depression with intravenous opioids and hypotension, spinal cord injury, hematoma, infection, and local anesthetic toxicity being associated with regional anesthetic techniques.Citation4 In addition, neuraxial techniques are often contraindicated in patients receiving oral anti-coagulants and in those with vertebral fractures. Neuraxial techniques can also be of minimal utility in the context of poly-trauma where positioning options are limited and hemodynamic instability may be present.Citation5
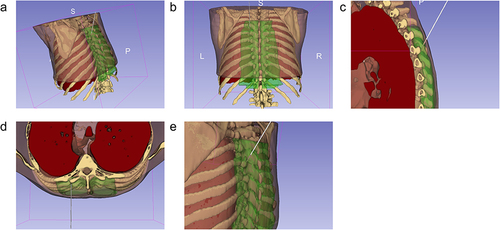
Erector spinae blocks (ESB) have been proposed as an alternative first-line regional analgesia technique for use in rib fracture management. Since its inception in 2016,Citation6 it has seen a wide range of applications from traumaCitation7 to elective surgery which includes abdominal, thoracic, breast and orthopaedic procedures.Citation8–12 The erector spinae muscles are a group of stabilisers which lie between the vertebral spinous and transverse processes in the thorax, in close proximity to the dorsal rami of the intercostal nerves, along with the paravertebral space. ESB involves an injection of local anaesthetic under ultrasound guidance into the erector spinae fascial plane. The needle tip is directed at the posterior aspect of the lateral portion of the transverse process at the desired level, with subsequent injection of local anaesthetic hydrodissecting the fascial plane deep to the erector spinae muscle while remaining superficial to the vertebral transverse process. A representation of the anatomy is presented in , rendered using 3D slicer (Version 5.2.2, 2023), an open source segmentation software and a sample CT chest dataset.Citation13 The mechanism of action is thought to be related to local anaesthetic spread causing blockade of the lateral cutaneous and intercostal nerves, along with potential diffusion into the paravertebral space.Citation14,Citation15 The proposed advantages of ESB are in its ease of use, and safety profile. Current blocks involve instrumenting in close proximity to neurovascular structures around the spine, and the pleural space, resulting in complications such as dural puncture, hypotension, local anaesthetic toxicity and pneumothorax.Citation16
Figure 1 Needle placement for the erector spinae block at the level of T6 on the left, with the needle represented in grey, erector spinae muscles in green, lung in red, thoracic vertebrae and ribs in white, and the thorax in pink. Views presented are (a) posterior view from the left, (b) posterior view, (c) sagittal transection viewed from the left, (d) axial transection viewed from above, and (e) a view of the needle with the patient upright. All images created using 3D slicer (version 5.2.2, 2023) an open-source software, with the segments created using a sample CT chest dataset.
The literature surrounding ESB in rib fractures is predominantly comprised of case reports and case series, with few large-scale studies having been published. This review aims to investigate the available literature on the topic to assess clinical outcomes and safety profile, and to guide future research in the area.
Methods
This study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) and Joanna Briggs Institute (JBI) guidelines for scoping reviews, and registered in the Open Science Framework prior to commencement.
Search Strategy
A comprehensive literature search was performed by two reviewers (VP, MJ) to identify appropriate articles for review and inclusion in this study, with a third reviewer (BO) consulted for conflicts. Using the OVID platform, the MEDLINE and EMBASE databases were used to refine the search strategy utilising keywords and MeSH terms relating to “rib fractures”, and “erector spinae blocks” with the aid of Austin Health Library. The search strategy is shown in Appendix A. Scopus, Web of Science, and the Cochrane databases were then searched using the developed strategy.
Inclusion Criteria
All papers investigating the use of ESB as an analgesic intervention for acute rib fractures and recorded clinical outcomes were included. Studies which involved patients undergoing ESB at the time of surgical fixation were excluded due to the confounding impact of the procedure. All article types available in English except for conference abstracts were eligible for inclusion in this review.
Data Extraction
Data were extracted independently and recorded by two reviewers (MJ, VP) on a standardised excel spreadsheet. The data points recorded were as follows:
- Article data: author, year, type of article, number of patients involved
- Demographic data: age, gender, anticoagulation status
- Injury data: mechanism, number/location of additional injuries, number of ribs fractured, unilateral or bilateral rib fractures
- Block data: location of administration, anaesthetic agent/volume/dose, catheter vs single injection, time from injury, unilateral or bilateral block, block indication, complications
- Pain outcomes: pain scores, opioids usage, rescue analgesia/intervention
- Respiratory outcomes: spirometry, intervention, complications
- Admission data: hospital length of stay (LOS), intensive care unit (ICU) LOS, mortality
Statistical Analysis
Due to the heterogeneity of time points, measurement tools used, and outcomes recorded, statistical analysis focused on a descriptive comparison of available studies, with further quantitative analyses not feasible in this study. Variables are presented as whole numbers, or as percentages with the denominator based on the number of studies that reported the desired outcome. Weighted mean percentage change, calculated as the percentage change between two time points of the desired value with weighting proportional to the size of the investigated patient cohort in each study, was used to compare pain scores and respiratory outcomes. Conversion of median and interquartile range to mean and standard deviation was performed using the method presented by Wan et alCitation17 to allow comparison between studies.
Results
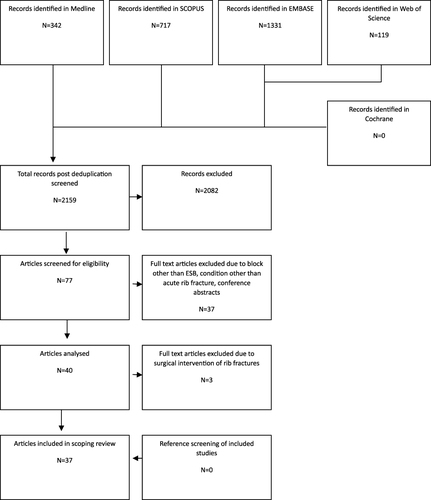
A PRISMA flowchart of the search is shown in . The final search was performed on 22 November 2022.
The initial search of the literature yielded 2159 studies due to the broad nature of the search parameters. Screening of abstracts resulted in 77 papers, following which 40 studies were excluded due to incorrect block or injury, surgical fixation, or for being presented in a conference abstract format. Of the 37 studies included, 10 were case reports,Citation18–27 12 were case series,Citation28–39 5 were cohort studies,Citation7,Citation40–43 2 were randomized controlled trials (RCT),Citation44,Citation45 1 was a prospective interventional study,Citation46 and 7 were letters to the editor.Citation47–53 The majority of studies were published after 2020, with 29% being published in 2022. A summary of the results of the cohort studies is shown in .
Table 1 Summary of Key Findings in the Prospective and Retrospective Cohort Studies
Demographic Data
A total of 802 patients with a mean age of 60 years across 37 studies were included in this review. 72% of which were male. Each patient had a mean (standard deviation, SD) of 6 (3) rib fractures, with 87% having unilateral injury. The most common mechanisms of injury were motor vehicle accident, and falls. Additional injury was reported in 168 patients with 1 additional injury in 60 patients, 2 additional injuries reported in 27, 3 additional injuries in 14, and 4 or more injuries in 10 patients. 28% of patients had additional chest trauma, 11% with head injury, 8% with intra-abdominal injury, 19% with spinal injury, and 30% with additional limb injury.
Block Characteristics
Block technique was similarly described in all papers, with patients in the seated or lateral position with ultrasound guidance in the parasagittal plane. Whilst a majority of blocks were performed in the intensive care setting, ESBs were safely administered in multiple locations including the hospital ward, operating theatre, via fluoroscopy,Citation29 and the prehospital retrieval setting.Citation27 Local anaesthetic regimes varied between studies, with the most common agents being ropivacaine and bupivacaine. 15–100mL of 0.2–1% ropivacaine or 15–40mL of 0.25–0.5% bupivacaine were used for single shot injections, with some studies adding adrenaline or steroid. Ropivacaine 0.2% was used in 16 studies as the agent for catheter infusion in a combination of background and bolus regimes. Bupivacaine 0.125% and 0.1% ropivacaine also saw use. 80% of blocks administered were in the form of catheter insertion, with infusion duration ranging from 0.6 to 12 days.
The main indication for ESB was as an analgesic intervention either for uncontrolled pain or as a preventative measure, with 9 studies reporting usage of the technique as a rescue measure for patients in respiratory failure.Citation18,Citation20–22,Citation24,Citation28,Citation33,Citation34,Citation47 The majority of blocks were administered within the first 48 hours of presentation.
Pain Outcomes
Twenty-eight studies reported objective changes in pain score post administration of ESB using various scoring scales including Numerical Rating Scale (NRS), Visual Analogue Scale (VAS), Defence and Veteran Pain (DVP) score, and a 4 point verbal score.Citation7,Citation18–25,Citation27–31,Citation33,Citation34,Citation36–39,Citation42,Citation44–49,Citation53 Due to the heterogeneity of scales and time points used to evaluate pain, an average weighted percentage change in pain scores was calculated. The mean reduction in pain scores from pre-block baseline was approximately 40% within the first 24 hours. Six studies reported pain scores 24 to 48 hours post block, maintaining an average reduction of 21% from pre block baseline, while a further five studies reported pain scores over 72 hours post block reporting an average 43% reduction in pain score.
Opioid use within the first 24 hours post procedure showed similar results. Five studiesCitation7,Citation22,Citation24,Citation47,Citation53 compared pre block opioid requirements with that of the first 24 hours post block which showed a trend towards a 34% reduction in opioid requirement; however, no studies reported statistical significance for this outcome. However, most notably, five studies reported nil further analgesic requirement post administration of ESB.Citation21,Citation28,Citation30,Citation36,Citation48
Respiratory Outcomes
Eight studies reported on respiratory function testing pre- and post administration of ESB showing an overall trend of improved values post ESB.Citation7,Citation21,Citation24,Citation26,Citation37,Citation39,Citation44,Citation46 Adhikary et al reported an average improvement in incentive spirometry of 590mL which was maintained over the first 3 days post block.Citation7 This result was reflected in the study by Syal et alCitation39 who reported a similar magnitude of improvement in their measurements of inspiratory capacity. Sharipova et alCitation37 demonstrated a slight improvement in forced vital capacity (FVC) in 2 patients from 34 to 41%, and 40 to 47% of predicted post ESB, however the remaining two patients saw no change and a slight decrease.
Respiratory complication was not consistently reported throughout the studies. Mladenovic et alCitation41 reported an incidence of respiratory complication of 19% with pneumonia being the most common presentation. 5.5% of this cohort experienced respiratory failure, with the key finding in this study being that ESB delivered after 48hrs post admission being associated with higher rates of complication and increased ICU LOS. Four studies reported patients being rapidly weaned from respiratory supports, including one patient being extubated successfully post ESB despite previous failure due to inadequate analgesia.Citation21,Citation22,Citation33,Citation34
Block Safety
No studies included in this review reported a major adverse event following ESB. Three studiesCitation42,Citation43,Citation50 reported complications in the form of block failure (n = 25), infection (n = 3), and haematoma (n = 2); however, none required any further intervention. Of note, no cases of hypotension, local anaesthetic toxicity, dural puncture, or pneumothorax were reported. Elawamy et alCitation45 in a comparative RCT demonstrated 6 cases of hypotension, 2 cases of bradycardia, and 3 vascular punctures in a cohort of 30 patients receiving thoracic paravertebral blocks (TPVB), with no complication demonstrated in the ESB cohort. Seven studiesCitation19,Citation20,Citation25,Citation33,Citation35,Citation40,Citation43 included patients on prophylactic/therapeutic anticoagulation or had ESB administered in the setting of coagulopathy. Three papers,Citation38,Citation44,Citation45 including both RCTs, excluded this patient cohort. A cohort of 249 patients investigated by Dultz et al and White et al,Citation40,Citation43 including 89 patients receiving anticoagulation or with concurrent coagulopathy revealed only 4 patients complicated by haematoma or infection. None of these patients required further intervention. Five further studies included patients with anticoagulation with only 1 further case of infection arising from them. No reports of dural puncture, local anaesthetic toxicity, hypotension, or pneumothorax were reported.
Discussion
The available data suggests that ESB is an effective analgesic technique which is safe despite the fact that it is used in high-risk patients. However, it lacks large scale, prospective data to support its use.
A multitude of trials and meta-analyses have shown the efficacy of ESB as an analgesic adjunct in thoracic, abdominal, breast, orthopaedic, and cardiac surgery.Citation54,Citation55 These studies demonstrate a reduction in pain scores post operatively with associated reductions in opioid use and opiate-induced nausea and vomiting. These findings are also seen when ESB is applied as analgesia for rib fracture with improvements in pain scores, opioid use, and respiratory parameters being consistently demonstrated. Its effectiveness in the setting of multi trauma is also demonstrated with multiple studies reporting improved pain scores in the presence of further injury in close proximity to the chest wall. Early administration of ESB in this context may also reduce the incidence of respiratory deterioration as suggested by Mladenovic et al.Citation41 The clinical significance of this should be highlighted as rib fractures are often seen in older, frailer patients in whom escalation of invasive ventilation and prolonged ICU admission may not provide long-term benefit. Furthermore, the ability to successfully administer ESB within a number of environments from the operating theatre to the emergency department and even a prehospitalCitation27 setting reflect its versatility and ease of use.
The current literature on ESB in rib fractures suggests that ESB is at least comparable to current techniques, with an improved safety profile. Randomised control trials conducted by El Malla et alCitation44 and Elawamy et alCitation45 demonstrated that ESB is as effective as serratus anterior block (SAB) and TPVB respectively, with comparable pain outcomes. This is supported by data published by Murray et alCitation42 and Riley et alCitation50,Citation51 comparing ESB to TPVB, SAB, and opioid analgesia in retrospective matched cohort studies. In terms of block safety, no complications from administration of ESB with systemic consequences were reported. A 2% complication rate of infection and haematoma was demonstrated in the two largest cohort studies investigating safety,Citation40,Citation43 while Elawamy et alCitation45 demonstrated a higher complication rate in TPVB compared to ESB. Studies conducted by Dultz et alCitation40 and White et alCitation43 also suggest that use of ESB in patients on anticoagulant medication, or concurrent coagulopathy, a contraindication to many available neuraxial techniques, is safe. This reflects research in other specialties in which ESB has been successfully utilized without complication in patients with thrombocytopenia,Citation56,Citation57 coagulopathy,Citation58–60 therapeutic anticoagulation,Citation61 or antiplatelet therapy.Citation62 For example, Adhikary et al demonstrated no haemorrhagic complications in a case series of 5 patients receiving ESB while on intravenous heparin therapy post thoracotomy and left ventricular assist device implantation.Citation63 The ability to continue anticoagulation peri-block also confers clinical advantages in the trauma setting, where missed doses of venous thromboembolism prophylaxis increases the risk of thrombotic events.Citation64,Citation65
While this scoping review demonstrates favourable qualitative analysis of ESB, there remain many domains in which data is lacking. The ultimate goal of analgesic regimes in the conservative management of rib fractures is to prevent respiratory deterioration, an outcome which was sparsely reported within the current studies. Further, there have been only 3 prospective studies,Citation44–46 two of which compared ESB to another regional technique. The majority of remaining studies are retrospective cohort studies or case series without a comparator group. As such, extrapolating the clinical efficacy of ESB versus the current gold standard remains difficult. The optimal timing, local anaesthetic regime, and the cohort of patients in which ESB would provide the most benefit are also yet to be fully explored.
Conclusion
In conclusion, while the current results show promise, the heterogeneity of reported outcomes and lack of large scale prospective trials preclude a firm recommendation of best practice for ESB use in rib fracture management. ESB has demonstrated benefits of ease of use being applied in a variety of settings and has comparable efficacy compared to TPVB and SAB. Moreover, ESB has an improved complication profile. Future studies should aim to determine the impact of ESB on respiratory complications, the optimal timing of administration, the optimal regime for administration and the safety of this regional technique.
Abbreviations
ESB, erector spinae block; PRISMA, Preferred reporting items for systematic reviews and meta analyses; JBI, Joanna Briggs Institute; LOS, length of stay; ICU, intensive care unit; RCT, randomised control trial; SD, standard deviation; NRS, numerical rating scale; VAS, visual analogue scale; DVP, Defence and Veterans pain; FVC, forced vital capacity; SAB, serratus anterior block; TPVB, thoracic paravertebral block.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors would like to thank the Department of Anaesthesia, Austin Health for their support of this paper. The authors would also like to acknowledge the efforts of the Austin Health Library team for their assistance with the search strategy.
Additional information
Funding
References
- Coary R, Skerritt C, Carey A, Rudd S, Shipway D. New horizons in rib fracture management in the older adult. Age Ageing. 2019;49(2):161–167. doi:10.1093/ageing/afz157
- Ho AM, Ho AK, Mizubuti GB, Klar G, Karmakar MK. Regional analgesia for patients with traumatic rib fractures: a narrative review. J Trauma Acute Care Surg. 2020;88(1):e22–e30. doi:10.1097/TA.0000000000002524
- Thiruvenkatarajan V, Cruz Eng H, Adhikary SD. An update on regional analgesia for rib fractures. Curr Opin Anaesthesiol. 2018;31(5):601–607. doi:10.1097/ACO.0000000000000637
- Chin KJ. Thoracic wall blocks: from paravertebral to retrolaminar to serratus to erector spinae and back again - A review of evidence. Best Pract Res Clin Anaesthesiol. 2019;33(1):67–77. doi:10.1016/j.bpa.2019.02.003
- Bhalla PI, Solomon S, Zhang R, Witt CE, Dagal A, Joffe AM. Comparison of serratus anterior plane block with epidural and paravertebral block in critically ill trauma patients with multiple rib fractures. Trauma Surg Acute Care Open. 2021;6(1):e000621. doi:10.1136/tsaco-2020-000621
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627. doi:10.1097/AAP.0000000000000451
- Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: a retrospective cohort study. Anaesthesia. 2019;74(5):585–593. doi:10.1111/anae.14579
- Daghmouri MA, Akremi S, Chaouch MA, et al. Bilateral erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Pain Pract. 2021;21(3):357–365. doi:10.1111/papr.12953
- Pirsaharkhiz N, Comolli K, Fujiwara W, et al. Utility of erector spinae plane block in thoracic surgery. J Cardiothorac Surg. 2020;15(1):91. doi:10.1186/s13019-020-01118-x
- Talawar P, Kumar A, Bhoi D, Singh A. Initial experience of erector spinae plane block in patients undergoing breast surgery: a case series. Saudi J Anaesth. 2019;13(1):72–74. doi:10.4103/sja.SJA_560_17
- Tulgar S, Selvi O, Senturk O, Serifsoy TE, Thomas DT. Ultrasound-guided erector spinae plane block: indications, complications, and effects on acute and chronic pain based on a single-center experience. Cureus. 2019;11(1):e3815. doi:10.7759/cureus.3815
- Liang X, Zhou W, Fan Y. Erector spinae plane block for spinal surgery: a systematic review and meta-analysis. Korean J Pain. 2021;34(4):487–500. doi:10.3344/kjp.2021.34.4.487
- Fedorov A, Beichel R, Kalpathy-Cramer J, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging. 2012;30(9):1323–1341. doi:10.1016/j.mri.2012.05.001
- Gadsden J. The erector spinae plane block: the case of the elusive mechanism of action. Can J Anaesth. 2021;68(3):288–292. doi:10.1007/s12630-020-01876-1
- Onishi E, Toda N, Kameyama Y, Yamauchi M. Comparison of clinical efficacy and anatomical investigation between retrolaminar block and erector spinae plane block. Biomed Res Int. 2019;2019:2578396. doi:10.1155/2019/2578396
- Freise H, Van Aken HK. Risks and benefits of thoracic epidural anaesthesia. BJA. 2011;107(6):859–868. doi:10.1093/bja/aer339
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. doi:10.1186/1471-2288-14-135
- Almeida C, Francisco E, Cunha P, Vieira L, Antunes P. Single continuous erector spinae plane block for multiple rib, clavicle, and scapula fractures: a case report. Saudi J Anaesth. 2022;16(4):497–499. doi:10.4103/sja.sja_290_22
- Espahbodi E, Sanatkar M, Yekta RA. Erector spine block (Esb) for pain relief in a patient with multiple ribs fracture. Acta Med Iran. 2020;58(2):83–84.
- Gluncic V, Bonasera L, Gonzalez S, Lukic IK, Candido K. Combination of the T7 unilateral erector spinae plane block and T10 bilateral retrolaminar blocks in a patient with multiple rib fractures on the right and T10–12 Vertebral compression fractures: a case report. Local Reg Anesth. 2021;14:99–102. doi:10.2147/LRA.S312881
- Gursoy C, Kuscu Y, Demirbilek SG. Pain management for traumatic rib fractures with ESP block in ICU. JCPSP. 2020;30(3):318–320. doi:10.29271/jcpsp.2020.03.318
- Klesius L, Schroeder K. Effective analgesia with bilateral erector spinae plane catheters for a patient with traumatic rib and spine fractures. Case Rep Anesthesiol. 2019;2019:1–3. doi:10.1155/2019/9159878
- Kumar R, Sharma A, Bansal R, Kamal M, Sharma L. Ultrasound-guided continuous erector spinae plane block in a patient with multiple rib fractures. Turk. J. Anaesthesiol Reanim. 2019;47(3):235–237. doi:10.5152/TJAR.2018.46794
- Liu R, Clark L, Bautista A. Unilateral bilevel erector spinae plane catheters for flail chest: a case report. A a Pract. 2020;14(7):e01211. doi:10.1213/XAA.0000000000001211
- Thompson MH, Hodson G, Ashken TW, Ng SC. Bi-level erector spinae plane catheters for multiple rib fractures in a high-risk patient. Arch Clin Cases. 2020;7(1):1–4. doi:10.22551/2020.26.0701.10164
- Xu JL, Con J, Hou J, Parikh SB, Junge JM, Dotzauer B. Ultrasound-guided erector spinae plane block using long-range multi-orifice catheter for chest wall pain management in patients with multiple rib fractures. Am Surg. 2019;85(1):E6–E8. doi:10.1177/000313481908500103
- Ibbotson WJ, Greenberg R, Brendt P. Erector spinae block for chest trauma in aeromedical prehospital and retrieval medicine. Prehosp Disaster Med. 2020;35(4):454–456. doi:10.1017/S1049023X20000540
- Gurbuz H, Demir N. Erector spinae plane catheter for pain management of multiple rib fractures: anecdotal records of cases with blunt chest trauma. AGRI. 2022;34(3):217–221. doi:10.14744/agri.2020.39327
- Jadon A, Swarupa CP, Amir M. Fluoroscopic-guided erector spinae plane block: a feasible option. Indian J Anaesth. 2018;62(10):806–808. doi:10.4103/ija.IJA_411_18
- Jones MR, Urits I, Shnider MR, Matyal R. Confirmation of erector spinae plane block analgesia for 3 distinct scenarios: a case report. A a Pract. 2019;12(5):141–144. doi:10.1213/XAA.0000000000000865
- Kumar G, Kumar Bhoi S, Sinha TP, Paul S. Erector spinae plane block for multiple rib fracture done by an emergency physician: a case series. Australas J Ultrasound Med. 2021;24(1):58–62. doi:10.1002/ajum.12225
- Luftig J, Mantuani D, Herring AA, Dixon B, Clattenburg E, Nagdev A. Successful emergency pain control for posterior rib fractures with ultrasound-guided erector spinae plane block. Am J Emerg Med. 2018;36(8):1391–1396. doi:10.1016/j.ajem.2017.12.060
- Mizubuti GB, Camiré D, Ho AMH, Breton S, Klar G. Erector spinae plane block when neuraxial analgesia is contraindicated by clotting abnormalities. Ann Thorac Cardiovasc Surg. 2021;112(4):e245–e7. doi:10.1016/j.athoracsur.2021.01.043
- Nandhakumar A, Nair A, Bharath VK, Kalingarayar S, Ramaswamy BP, Dhatchinamoorthi D. Erector spinae plane block may aid weaning from mechanical ventilation in patients with multiple rib fractures: case report of two cases. Indian J Anaesth. 2018;62(2):139–141. doi:10.4103/ija.IJA_599_17
- Riley B, Malla U, Snels N, et al. Novel chest wall blocks for severe chest wall injuries in older persons: a case series. Trauma. 2022;24(3):257–261. doi:10.1177/14604086211032877
- Schultz C, Yang E, Mantuani D, Miraflor E, Victorino G, Nagdev A. Single injection, ultrasound-guided planar nerve blocks: an essential skill for any clinician caring for patients with rib fractures. Trauma Case Rep. 2022;41:1. doi:10.1016/j.tcr.2022.100680
- Sharipova VK, Fokin IV, Sattarova FK, Parpibayev FO. Erector spinae plane fascial block in multiple rib fractures (Case report). Obs Reanimatol. 2020;16(5):22–29. doi:10.15360/1813-9779-2020-5-22-29
- Surdhar I, Jelic T. The erector spinae plane block for acute pain management in emergency department patients with rib fractures. Can J Emerg Med. 2022;24(1):50–54. doi:10.1007/s43678-021-00203-x
- Syal R, Mohammed S, Kumar R, Jain N, Bhatia P. Continuous erector spinae plane block for analgesia and better pulmonary functions in patients with multiple rib fractures: a prospective descriptive study. Braz J Anesthesiol. 2022;2022:1.
- Dultz LA, Ma R, Dumas RP, et al. Safety of erector spinae plane blocks in patients with chest wall trauma on VTE prophylaxis. J Surg Res. 2021;263:124–129. doi:10.1016/j.jss.2021.01.020
- Mladenovic J, Erskine RN, Riley B, et al. The association between erector spinae plane block timing and reduced rib fracture related respiratory complications: a cohort study. J Clin Anesth. 2022;82:110940. doi:10.1016/j.jclinane.2022.110940
- Murray N, Swierczek J, Riley B, et al. Erector spinae plane versus paravertebral catheter techniques for rib fracture analgesia: a pilot matched cohort study. Trauma;2022. 146040862211068. doi:10.1177/14604086221106849
- White LD, Riley B, Davis K, et al. Safety of continuous erector spinae catheters in chest trauma: a retrospective cohort study. Anesth Analg. 2021;133(5):1296–1302. doi:10.1213/ANE.0000000000005730
- El Malla DA, Helal RAF, Zidan TAM, El Mourad MB. The effect of erector spinae block versus serratus plane block on pain scores and diaphragmatic excursion in multiple rib fractures. a prospective randomized trial. Pain Med. 2022;23(3):448–455. doi:10.1093/pm/pnab214
- Elawamy A, Morsy MR, Ahmed MAY. Comparison of thoracic erector spinae plane block with thoracic paravertebral block for pain management in patients with unilateral multiple fractured ribs. Pain Physician. 2022;25(6):483–490.
- Palachick BJ, Carver RA, Byars DV, Martyak MT, Collins JN. Erector spinae plane blocks for traumatic rib fractures: a prospective, interventional study. Am Surg. 2022;88(9):2124–2126.
- Beh Z, Lim S, Lim W, Sitaram P. Erector spinae plane block as analgesic adjunct for traumatic rib fractures in intensive care unit. Indian J Anaesth. 2020;64(12):1086–1089. doi:10.4103/ija.IJA_1110_20
- Diwan S, Nair A. Unilateral erector spinae plane block for managing acute pain arising from multiple unilateral injuries: a case report. Indian J Anaesth. 2020;64(1):79–80. doi:10.4103/ija.IJA_609_19
- Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118(3):474–+. doi:10.1093/bja/aex013
- Riley B, Malla U, Snels N, et al. Erector spinae and serratus anterior blocks for the management of rib fractures: a retrospective exploratory matched study. Am J Emerg Med. 2020;38(8):1689–1691. doi:10.1016/j.ajem.2020.01.007
- Riley B, Malla U, Snels N, et al. Erector spinae blocks for the management of rib fractures: a pilot matched study. J Clin Anesth. 2020;63:1. doi:10.1016/j.jclinane.2020.109780
- Tseng V, Zhang X, Burke C, Xu JL. Erector spinae plane block as a rescue analgesic technique for multiple rib fractures after failed serratus anterior plane block. Minerva Anestesiol. 2019;85(9):1036. doi:10.23736/S0375-9393.19.13718-2
- Xu L, Basireddy S, Villanueva C, Horn A, Tsui BCH. Thoracic epidural anesthesia versus continuous erector spinae plane block for traumatic rib fracture analgesia: a retrospective cohort study. J Clin Anesth. 2021;75:110519. doi:10.1016/j.jclinane.2021.110519
- Cai Q, Liu GQ, Huang LS, et al. Effects of erector spinae plane block on postoperative pain and side-effects in adult patients underwent surgery: a systematic review and meta-analysis of randomized controlled trials. Int J Surg. 2020;80:107–116. doi:10.1016/j.ijsu.2020.05.038
- Krishna SN, Chauhan S, Bhoi D, et al. Bilateral erector spinae plane block for acute post-surgical pain in adult cardiac surgical patients: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2019;33(2):368–375. doi:10.1053/j.jvca.2018.05.050
- Anido Guzman J, Becerra Cayetano A, Donoso Dominguez M. Erector spinae plane block for postoperative rescue analgesia in patients with coagulation disorders. Minerva Anestesiol. 2021;87(3):369–370. doi:10.23736/S0375-9393.20.15016-8
- Ayub A, Talawar P, Kumar R, Bhoi D, Singh AY. Erector spinae block a safe, simple and effective analgesic technique for major hepatobiliary surgery with thrombocytopenia. Egypt J Anaesth. 2018;34(4):169–172. doi:10.1016/j.egja.2018.08.001
- Arun N, Singh S. Is ESP block an answer for upper abdominal surgeries where epidural analgesia can’t be used? J Anaesthesiol. 2020;36(1):117–118.
- Maddineni U, Maarouf R, Johnson C, Fernandez L, Kazior MR. Safe and effective use of bilateral erector spinae block in patient suffering from post-operative coagulopathy following hepatectomy. Am J Case Rep. 2020;21:e921123. doi:10.12659/AJCR.921123
- Wyatt K, Elattary T. The erector spinae plane block in a high-risk Ehlers-Danlos syndrome pediatric patient for vascular ring repair. J Clin Anesth. 2019;54:39–40. doi:10.1016/j.jclinane.2018.10.031
- Mudarth M, Satyapriya V, Coffman J, et al. Continuous erector spinae plane block for analgesia after thoracotomy for lung transplantation in an anticoagulated patient. Case Rep Anesthesiol. 2021;2021:6664712. doi:10.1155/2021/6664712
- De Cassai A, Ieppariello G, Ori C. Erector spinae plane block and dual antiplatelet therapy. Minerva Anestesiol. 2018;84(10):1230–1231. doi:10.23736/S0375-9393.18.12815-X
- Adhikary SD, Prasad A, Soleimani B, Chin KJ. Continuous erector spinae plane block as an effective analgesic option in anticoagulated patients after left ventricular assist device implantation: a case series. J Cardiothorac Vasc Anesth. 2019;33(4):1063–1067. doi:10.1053/j.jvca.2018.04.026
- Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American society of regional anesthesia and pain medicine evidence-based guidelines (fourth edition). Reg Anesth Pain Med. 2018;43(3):263–309. doi:10.1097/AAP.0000000000000763
- Louis SG, Sato M, Geraci T, et al. Correlation of missed doses of enoxaparin with increased incidence of deep vein thrombosis in trauma and general surgery patients. JAMA Surg. 2014;149(4):365–370. doi:10.1001/jamasurg.2013.3963