Abstract
Purpose
Differences in tidal breathing patterns have been reported between patients with chronic obstructive pulmonary disease (COPD) and healthy individuals using traditional measurement techniques. This feasibility study examined whether structured light plethysmography (SLP) – a noncontact, light-based technique – could also detect differences in tidal breathing patterns between patients with COPD and healthy subjects.
Patients and methods
A 5 min period of tidal (quiet) breathing was recorded in each patient with COPD (n=31) and each healthy subject (n=31), matched for age, body mass index, and sex. For every participant, the median and interquartile range (IQR; denoting within-subject variability) of 12 tidal breathing parameters were calculated. Individual data were then combined by cohort and summarized by its median and IQR.
Results
After correction for multiple comparisons, inspiratory time (median tI) and its variability (IQR of tI) were lower in patients with COPD (p<0.001 and p<0.01, respectively) as were ratios derived from tI (tI/tE and tI/tTot, both p<0.01) and their variability (p<0.01 and p<0.05, respectively). IE50SLP (the ratio of inspiratory to expiratory flow at 50% tidal volume calculated from the SLP signal) was higher (p<0.001) in COPD while SLP-derived time to reach peak tidal expiratory flow over expiratory time (median tPTEFSLP/tE) was shorter (p<0.01) and considerably less variable (p<0.001). Thoraco–abdominal asynchrony was increased (p<0.05) in COPD.
Conclusion
These early observations suggest that, like traditional techniques, SLP is able to detect different breathing patterns in COPD patients compared with subjects with no respiratory disease. This provides support for further investigation into the potential uses of SLP in assessing clinical conditions and interventions.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Structured light plethysmography (SLP) is a novel, noncontact method for assessing quiet “tidal” breathing. There is growing interest in the potential clinical uses of this technique, which has been applied to a number of clinical conditions and used to assess the response to intervention.Citation1–Citation3 For example, it has recently been reported that SLP can detect changes in chest wall motion in a group of lung resection patients.Citation4 The reduction in the relative contribution of the chest wall to the total tidal breath was consistent with both the site and magnitude of the resection. Furthermore, a greater increase in thoraco–abdominal asynchrony (TAA) was observed in patients undergoing a lobectomy compared with resection where less lung tissue is removed. However, as this is a relatively new field, further published evidence confirming the utility of the technique for detecting clinical differences is limited.
Before the device can be used for more novel interventions and to compare clinical groups, there is a need to evaluate differences in SLP outputs where differences in breathing patterns are known to occur. Patterns of natural breathing at rest (or “tidal breathing”) have long been reported to differ between patients with respiratory disease and healthy subjects. Evidence to support such observations has grown over the past 15 years, as a number of studies have reported the effects of conditions such as COPD on tidal breathing patterns.Citation5–Citation10
Various techniques are used to measure tidal breathing patterns, including pneumotachography (PNT), respiratory inductance plethysmography (RIP), and optoelectronic plethysmography (OEP). These vary in the source of the signal and the type of parameters that are generated. PNT, considered the gold standard for tidal breathing measurement,Citation11 measures airflow at the nose and/or mouth, producing a flow signal that can be integrated over time to give respired volumes. RIP involves the use of transducer bands placed around the subject to monitor excursions of the chest and abdomen over time, producing signals that, once calibrated, can provide estimates of flow and volume.Citation12 RIP also provides output of regional parameters such as TAA. OEP involves placement of up to 89 passive reflective markers directly on to the upper body. The movement of these markers are then recorded by multiple cameras positioned around the room and the three-dimensional (3D) coordinates of the markers are calculated.Citation13
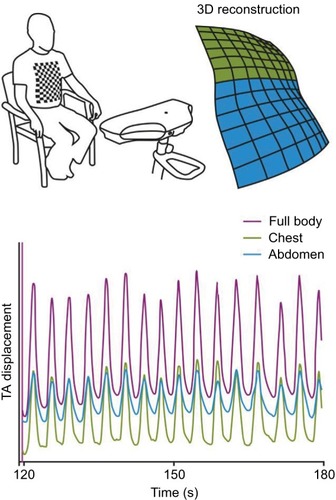
SLP does not require contact with the patient and measures tidal breathing through displacement of the thoraco–abdominal (TA) wall. A structured grid of light is projected onto the subject’s chest and abdomen, and changes in the grid pattern are captured by two digital cameras and then quantified over time. From this movement-over-time trace, timing and flow-related parameters are derived. As the projected grid can be subdivided during analysis, SLP can also provide outputs relating to the displacement of defined regions of the TA wall, such as the left and right hemithorax, ribcage, and abdomen. These regional parameters describe relative contributions of each region to the achieved TA displacement and also synchrony (or asynchrony) between regions. Furthermore, a numerical measure of within-subject variability of each parameter is also provided. More detailed information on the working principles of SLP has been described by de Boer et al.Citation14
This study examined whether SLP could detect differences in tidal breathing patterns between a cohort of patients with COPD and a cohort of healthy subjects, as has been reported in other studies using more traditional techniques.Citation5–Citation7,Citation9,Citation10
Materials and methods
Participants
All patients who were recruited to the study had previously received a clinical diagnosis of COPD from their hospital or general practitioner, in accordance with current diagnosis guidelines. Patients were recruited from general practice surgeries, hospital clinics, and hospital wards to ensure that a diverse sample of patients with the condition, and a range of severities, was included. A group of healthy subjects without a history or diagnosis of respiratory disease, and matched for age, sex, and body mass index (BMI), were also recruited. An age match was defined as an absolute difference of ≤5 years. A BMI match occurred if two individuals fell into the same BMI classification band (BMI <18.5 kg/m2 [underweight], 18.5 ≥ BMI < 25 [normal], 25 ≥ BMI < 30 [overweight], and BMI ≥30 [obese]). A sex match was scored if two individuals shared the same sex.
Individuals were excluded from the study if they had a chest wall or spinal deformity (eg, scoliosis), an apnea hypopnea index >30 (if known), a BMI >40, or any acute or chronic condition that, in the investigator’s opinion, would have limited the participant’s ability to take part in the study or would likely interfere with data acquisition (eg, a cough). All participants were fully informed of the testing procedure and provided written informed consent. The study protocol was approved by the United Kingdom Health Research Authority National Research Ethics Service (study number 11/EE/00/37). The ClinicalTrials.gov identifier is NCT02626468.
Study assessments
Each participant underwent a single assessment during which 5 min of quiet “tidal” breathing was recorded using an SLP device (Thora-3Di™, PneumaCare Ltd, Cambridge, UK). Before the assessment, participants were asked to change into a close fitting white T-shirt that followed the contours of the body although they could be assessed bare chested if they preferred. Participants were instructed to sit upright in a high-backed chair. The projected grid pattern generated by the SLP device was centered on the xiphisternum with 50% of the projected squares above and 50% below this point (taken to represent the chest and abdomen, respectively). This covered approximately the area from the clavicle to the umbilicus. Participants were then instructed not to move and to breathe naturally. Changes in the grid pattern caused by the respiratory movements of the TA wall were recorded by two cameras and quantified over time by the device. This provided a one-dimensional signal that corresponded to an individual’s tidal breathing pattern and was viewed on a computer using PneumaView-3DTM software (PneumaCare Ltd) (). This software was also used to generate a video of the 3D reconstruction of the TA wall surface.
Figure 1 Working principle of SLP.
Abbreviations: SLP, structured light plethysmography; TA, thoraco–abdominal; 3D, three dimensional.
SLP signal processing
Captured movement of the reconstructed TA surface was assessed for tracking errors caused by excessive creasing of the torso-covering white T-shirt, a lack of contrast in the projected image, or by movement. As these artifacts may affect some tidal breathing parameters, any data set which had >50% of its respiratory cycles affected by one or more of the above artifacts was excluded from further analysis. This conservative criterion was imposed to ensure that the data sets included in the study were clean.
PneumaView-3D software was used to export all SLP data accepted for further analysis into comma-separated value files, which contained information on the movement of the entire TA wall, as well as regional movements of left and right hemithorax, thorax, and abdomen. All traces were filtered using a fifth-order Butterworth band-pass filter with cutoffs at 0.05 and 5 Hz. Data were sampled at 30 Hz, which is sufficient for capturing the dynamics of TA wall movement.
A breath detection algorithm, inspired by the work of Schmidt et al and Bates et al, was used to automatically detect individual breaths on all traces.Citation15,Citation16 Peaks and troughs were detected by using the zero-crossing of the first derivative of the displacement signal. To be classed as a breath, the peak-to-peak amplitude had to be >25% of the median peak-to-peak amplitude of the entire trace. Respiratory cycles with exceedingly large or small inspiratory and/or expiratory times were deemed as outliers and excluded from analysis. An inspiratory or expiratory time xi was considered too large if its value was greater than Q3(X)+1.5×IQR(X) and too small if its value was less than Q1(X)−1.5×IQR(X), where X is the ensemble of individual inspiratory or expiratory times for each subject, Q1 and Q3 denote the first and third quartiles, respectively, and IQR is the interquartile range. To establish a one-to-one relationship between the respiratory cycles of different regional traces, cycles extracted from the movement of the entire TA wall, the left and right ribcage, thorax, and abdomen were intersected to ensure that the nth breath on any one trace corresponded to the nth breath on any of the other traces (eg, the second detected breath on the thoracic displacement trace corresponds to the second detected breath on the abdominal displacement trace). This was required for reliable and accurate quantification of regional parameters such as the relative contribution of the thorax to each breath (rCT) and TAA. The breath detection and intersection processes were also visually assessed to ensure reliability.
Tidal breathing parameters
Tidal breathing parameters included in this study were timing indices/ratios, namely respiratory rate (RR), inspiratory time (tI), expiratory time (tE), total breath time (tTot), tI/tE, and tI/tTot (duty cycle). Tidal breathing parameters relating to flow were calculated in the same way as conventional flow-based parameters, but in this case calculated from the TA wall displacement signal (analogous to volume) and the first derivative of the TA wall displacement signal (ie, displacement rate – analogous to flow). Conventional nomenclature is used to describe the tidal breathing parameters with the addition of the suffix “SLP” to indicate the origin of the source signal. The flow-based parameters are time to reach peak tidal expiratory flow rate over tE (tPTEFSLP/tE), time to reach peak tidal inspiratory flow over tI (tPTIFSLP/tI), and IE50SLP (calculated as TIF50SLP divided by TEF50SLP where the former is “tidal inspiratory flow at 50% tidal inspiratory volume” and the latter “tidal expiratory flow at 50% tidal expiratory volume”).
Further SLP parameters were calculated from regional movements of the TA wall. Here, the 3D reconstructions of the TA wall created by the SLP software were divided into an upper and lower region with equal number of grid intersections (approximately representing displacement of the thorax and abdomen) and likewise the upper region was separated into two equal top sections (reflecting displacement of the left and right thorax). Calculated regional parameters were rCT (%), left–right hemithoracic asynchrony (degrees), and TAA (degrees). Asynchronies were calculated using the Konno–Mead X–Y plots (ie, loops).Citation17,Citation18 provides a summary of the terms and abbreviations used in the study.
Table 1 List of abbreviations used for tidal breathing terminology
Statistical analysis
For each participant, every tidal breathing parameter measured over the 5 min assessment period was summarized by its median value and its IQR. Here, IQR was used as a measure of within-subject variability. For each cohort, individual data for each parameter and its variability were then combined and summarized by their median and IQR. Differences between cohorts were assessed using the Mann–Whitney U test (alpha level of p<0.05). Common language effect sizes (CLES) were calculated for parameters that differed significantly between patients with COPD and healthy subjects to further describe the ability of the parameters to distinguish COPD. CLES was selected as it does not assume normality and is easy to interpret.Citation19 The Benjamini–Hochberg procedure with a false discovery rate of 10% was employed to account for multiple comparisons.Citation20
Results
Study cohorts
Data from 31 patients with clinician-diagnosed COPD and 31 age-, BMI-, and sex-matched healthy subjects were included in the analysis. Demographics for each patient and each “matched” healthy subject are shown in . In COPD and healthy cohorts, respectively, mean age was 61.7 and 61.6 years, and mean BMI was 26.0 and 26.7 kg/m2. Each cohort included 17 males and 14 females.
Table 2 Participant demographicsTable Footnote*
SLP-measured tidal breathing parameters
Data for each tidal breathing parameter (including their within-subject variability) are summarized in . The median (IQR) number of breaths used to calculate these data for each participant was 72 (29.5) and 62 (17) in the COPD and healthy cohorts, respectively. The Mann–Whitney U test identified 10 parameters that were significantly different (p<0.05) between the two cohorts. After accounting for multiple comparisons using the Benjamini–Hochberg procedure, all of these remained statistically significant.
Table 3 Comparison of SLP-measured tidal breathing parameters between patients with COPD and age-, sex-, and BMI-matched healthy subjects
Among the timing indices/ratios measured by SLP, median tI was significantly lower in COPD patients than in healthy subjects, as was its variability (p<0.001 and p<0.01, respectively). CLES for median tI was 75.1% (indicating that 75% of COPD patients had a lower median tI when compared with healthy subjects). CLES for the variability in tI was 72.8%. Similarly, both tI-derived ratios (median tI/tE and median tI/tTot; both p<0.01) and their variability (p<0.01 and p<0.05, respectively) were reduced in the COPD group. CLES for both median tI/tE and median tI/tTot were 72.2%. CLES for variability in tI/tE and tI/tTot were 74.3% and 68.4%, respectively.
Median IE50SLP was significantly higher (p<0.001) in patients with COPD (CLES =84.6%), while median tPTEFSLP/tE (p<0.01, CLES =73.6%) and its variability (p<0.001, CLES =75.2%) were lower. provides an example of how IE50SLP could differ between a patient with COPD and its healthy counterpart. Patients with COPD also exhibited significantly greater TAA (p<0.05, CLES =68.5%). summarizes the effect sizes and their interpretation.
Figure 2 Illustration of how IE50SLP differed between a patient with COPD (right) and his or her age-, body mass index-, and sex-matched healthy subject (left).
Abbreviations: COPD, chronic obstructive pulmonary disease; IE50SLP, SLP-derived tidal inspiratory flow at 50% of inspiratory volume divided by tidal expiratory flow at 50% of expiratory volume; SLP, structured light plethysmography; TA, thoraco–abdominal; TEF50SLP, SLP-derived tidal expiratory flow at 50% of expiratory volume; TIF50SLP, SLP-derived tidal inspiratory flow at 50% of inspiratory volume.
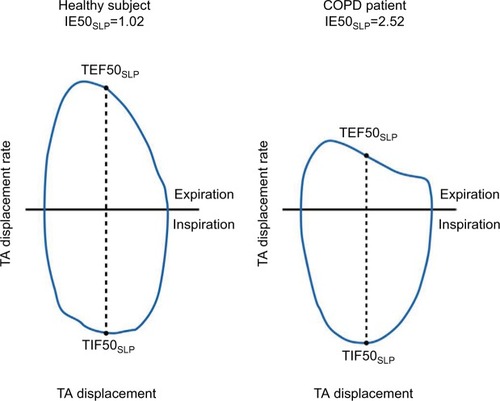
Table 4 CLES and its interpretation for parameters that differed significantly between patients with COPD and healthy subjects
Discussion
A number of studies have reported that patients with COPD can be differentiated from their healthy counterparts using tidal breathing patterns.Citation5–Citation10 Therefore, this feasibility study investigated whether parameters derived from SLP – a novel and noncontact, light-based method for measuring tidal breathing – are also able to detect differences between breathing patterns in patients with COPD and subjects with no respiratory disease. In total, 10 SLP-measured parameters were identified which differed between COPD patients and healthy individuals; the most statistically significant of which were median IE50SLP, median tI, and variability in tPTEFSLP/tE. Another key observation was that, along with the reduction in inspiratory time itself, within-subject variability of tI (and each of the ratios derived from tI) was also reduced. In addition, an increased TAA (ie, asynchrony between the thorax and abdomen) and a reduced median tPTEFSLP/tE and its variability in the COPD group were observed.
That median IE50SLP was markedly increased in the COPD cohort relative to healthy subjects is a particularly interesting finding. This parameter is calculated as TIF50SLP/TEF50SLP and can be considered analogous to the traditional “flow/volume-based” tidal breathing parameter, IE50 (the ratio of inspiratory to expiratory flow at 50% of tidal volume [TIF50/TEF50]). The effects of the COPD disease state on IE50SLP, IE50, or related parameters have not been reported before, as such parameters have mainly been described in children with asthma or other respiratory disease.Citation21 The CLES associated with IE50SLP (84.6%, approximately equivalent to an effect size of 1.4 had the distribution been normal) is very large, which is an indication of the ability of the parameter in distinguishing COPD from health. The current study also revealed a marked shortening of inspiratory time (ie, median tI) in the COPD cohort, and, as a consequence, ratios derived from this parameter (tI/tE and tI/tTot) were also reduced. A similar shortening of tI and associated ratios was recorded in COPD patients who participated in earlier studies employing PNT or OEP to measure tidal breathing.Citation6,Citation8,Citation10 Also, the median tPTEFSLP/tE was reduced in patients with COPD compared with healthy subjects. This finding is consistent with several PNT studies which showed that the analogous flow/volume-based parameter (ie, tPTEF/tE) is decreased in COPD.Citation6,Citation7,Citation9,Citation10
Three regional SLP parameters were measured in this study, one of which (TAA) was increased in patients with COPD compared with the healthy cohort. The existence of asynchrony between different sections of the TA wall has been acknowledged for many years.Citation22 For example, in 1984, Sackner et al demonstrated that TAA during both inspiration and expiration was increased in COPD patients compared with normal subjects.Citation23 Recently, Chien et al reported the same finding and also noted that TAA in COPD patients worsens during exercise, as assessed using the 6 min walk test.Citation24
Further outputs of SLP arise from calculation of within-subject variability in each of the parameters over the breathing sequence. Variability in all parameters related to tI (ie, variabilities of tI, tI/tE, and tI/tTot) as well as variability of tPTEFSLP/tE were reduced in patients with COPD compared with healthy subjects. This study measured within-subject variability in a straightforward manner by calculating the IQR of each parameter over the course of the 5 min assessment period. More sophisticated ways of detecting variability may lead to further evaluation of this phenomenon.
A risk inherent in comparing multiple different parameters between two cohorts is that one or more statistically significant result may have occurred by chance. The Benjamini–Hochberg procedure was therefore employed to account for multiple comparisons. This approach increases the confidence with which the key findings of this study can be interpreted. Based on the data presented here, it has been proposed that assessment of tidal breathing patterns via SLP may represent a novel method to facilitate identification of patients with COPD. However, further investigation is required on the diurnal or longitudinal changes within and between individuals.
SLP is noncontact, easy to perform, requires minimal patient cooperation, and, as such, may offer certain advantages over current methods of measuring tidal breathing. PNT requires direct contact with the subject via a facemask or a mouthpiece and nose clip which, as well as causing discomfort to the patient, may also lead to a “mouthpiece effect” that can influence measured parameters.Citation25,Citation26 Slippage of bands can be a problem in RIP, leading to inaccurate readings and unusable data sets.Citation27,Citation28 This technique also requires direct contact with the subject during placement and positioning of the bands. OEP is noncontact and can be used during exercise and sleep and does not require active participation of the patient;Citation13 however, placement of the markers is time-consuming and requires the TA surface to be exposed.Citation29 However, SLP can be sensitive to movement artifacts and, as such, cannot be used during activities, such as exercise or sleep. In addition, SLP does not measure absolute volume or flow but instead measures the displacement of the TA wall and the TA wall displacement rate, which are analogous to volume and flow, respectively, from which tidal breathing parameters can be derived.
The aim of this study was to determine whether SLP could detect differences in breathing patterns between patients with COPD and healthy subjects, as has been observed using traditional technologies. Validation of the SLP device was outside of the scope of this study, and further investigation will be required to determine how SLP-derived measurements are related to conventional flow-based measurements and to assess the test-retest repeatability of SLP. Such work is ongoing and preliminary findings suggest good agreement of respiratory timing indices measured by SLP and PNT, the current gold standard technique.Citation30
Conclusion
It was observed that SLP is able to detect differences in tidal breathing parameters between a group of patients with COPD and an age-, BMI-, and sex-matched cohort of healthy controls. It provides a proof of concept for more extensive study of SLP-assessed breathing patterns in COPD, and in particular, into whether there is a relationship between the magnitude of any SLP-derived parameter and the severity of disease. SLP may present a potentially useful clinical tool that can be easily performed during tidal breathing and that may help identify patients with COPD.
Author contributions
All authors contributed to study conception and/or design; interpreted the results; helped to draft, edit, and/or revise the manuscript; and approved the final version of the manuscript.
Acknowledgments
The study was sponsored by PneumaCare Ltd. The authors would like to thank Angelique Laubscher of PneumaCare Ltd for providing support with data collection. Medical writing support was provided by Alice Wareham, PhD and Rick Flemming PhD, CMPP (Aspire Scientific Ltd, Bollington, UK) and was funded by PneumaCare Ltd. Richard Iles’ current affiliation is Evelina London Children’s Hospital, Westminster Road, London, UK.
Disclosure
This paper was presented at the European Respiratory Society International Congress 2015 as a poster presentation with interim findings. The poster’s abstract was published in European Respiratory Journal 2015 46: PA2283; DOI: 10.1183/13993003.congress-2015.PA2283. RI is a shareholder of and part-time paid medical advisor to PneumaCare Ltd. RW and SMF are employees of and have share options for PneumaCare Ltd. The authors report no other conflicts of interest in this work.
References
- GhezziMTeneroLPiazzaMBodiniAPiacentiniGStructured light plethysmography: new method to evaluate expiratory flow limitation in asthmatic childrenEur Respir J201546Suppl 59PA3641
- HmeidiHChadwickELenneyWIE50 measured by structured light plethysmography (SLP) can differentiate between children with and without asthma, and can detect response to a bronchodilatorAm J Respir Crit Care Med2016193 Meeting Abstracts:A4505
- HmeidiHChadwickELenneyWStructured light plethysmography (SLP) can quantify abnormal breathing in children aged 2–12 admitted with acute asthmaAm J Respir Crit Care Med2016 193 Meeting Abstracts:A4506
- ElshafieGKumarPMotamedi-FakhrSIlesRWilsonRCNaiduBMeasuring changes in chest wall motion after lung resection using structured light plethysmography: a feasibility studyInteract Cardiovasc Thorac Surg201623454454727316661
- ChenYXinZQinCAnalysis of tidal breathing flow-volume curves in stable COPD patientsChinese J Prac Intern Med200511978980
- KostianevSHristovaAIluchevDCharacteristics of tidal expiratory flow pattern in healthy people and patient with chronic obstructive pulmonary diseaseFolia Med (Plovdiv)1999413182510658362
- MorrisMJWilliamsEMMadgwickRBanerjeeRPhillipsEChanges in lung function and tidal airflow patterns after increasing extrathoracic airway resistanceRespirology20049447448015612958
- WilkensHWeingardBLo MauroABreathing pattern and chest wall volumes during exercise in patients with cystic fibrosis, pulmonary fibrosis and COPD before and after lung transplantationThorax201065980881420805177
- WilliamsEMMadgwickRGMorrisMJTidal expired airflow patterns in adults with airway obstructionEur Respir J1998125111811239864007
- WilliamsEMPowellTEriksenMNeillPColasantiRA pilot study quantifying the shape of tidal breathing waveforms using centroids in health and COPDJ Clin Monit Comput2014281677423881418
- StickSMeasurements during tidal breathingStocksJSlyPTepperRMorganWInfant Respiratory Function TestingNew YorkWiley-Liss Inc1996117138
- PooleKThompsonHallinanHBeardsmoreCRespiratory inductance plethysmography in healthy infants: a comparison of three calibration methodsEur Respir J20001661084109011292110
- ParreiraVFVieiraDSMyrrhaMAPessoaIMLageSMBrittoRROptoelectronic plethysmography: a review of the literatureBraz J Phys Ther2012166439453
- de BoerWLasenbyJCameronJSLP: a zero-contact non-invasive method for pulmonary function testingLabrosseFZwiggelaarRLiuYTiddemanBProceedings of the British Machine Vision ConferenceAberystwythBMVA Press201085.185.12 Availble from: http://www.bmva.org/bmvc/2010/conference/paper85/paper85.pdfAccessed July 15, 2016
- BatesJHSchmalischGFilbrunDStocksJTidal breath analysis for infant pulmonary function testingEur Respir J20001661180119211292125
- SchmidtMFoitzikBWauerRRWinklerFSchmalischGComparative investigations of algorithms for the detection of breaths in newborns with disturbed respiratory signalsComput Biomed Res19983164134259843627
- KonnoKMeadJMeasurement of the separate volume changes of rib cage and abdomen during breathingJ Appl Physiol19672234074224225383
- SivanYAllenJLMeasurements of chest wall functionStocksJSlyPTepperRMorganWInfant Respiratory Function TestingNew YorkWiley-Liss Inc1996340351
- McGrawKOWongSA common language effect size statisticPsychol Bull19921112361
- BenjaminiYHochbergYControlling the false discovery rate: a practical and powerful approach to multiple testingJ R Stat Soc Series B Stat Methodol1995571289300
- TauberEFazekasTEichlerINegative expiratory pressure: a new tool for evaluating lung function in children?Pediatr Pulmonol200335316216812567383
- PrioriRAlivertiAAlbuquerqueALQuarantaMAlbertPCalverleyPMThe effect of posture on asynchronous chest wall movement in COPDJ Appl Physiol201311481066107523412901
- SacknerMAGonzalezHRodriguezMBelsitoASacknerDRGrenvikSAssessment of asynchronous and paradoxic motion between rib cage and abdomen in normal subjects and in patients with chronic obstructive pulmonary diseaseAm Rev Respir Dis198413045885936486558
- ChienJYRuanSYHuangYCYuCJYangPCAsynchronous thoraco-abdominal motion contributes to decreased 6-minute walk test in patients with COPDRespir Care201358232032622782088
- StickSMEllisELesouëfPNSlyPDValidation of respiratory inductance plethysmography (“Respitrace”®) for the measurement of tidal breathing parameters in newbornsPediatr Pulmonol19921431871911480445
- LavenezianaPLlontopCNieratM-CBellocqAStrausCSimilowskiTDisruption of tidal breathing in COPD by use of pneumotachograph and mouthpiece compared to non-contact measurement with structured light plethysmography (SLP)Eur Respir J201546Suppl 59PA511
- IlesRKhalidAKimberKWilsonRDe BoerWNon invasive measurement of respiratory rate: comparison between the Embletta® (Gold) respiband device and Thora3Di, PneumaCare LtdAm J Respir Crit Care Med2014189 Meeting Abstracts:A2935
- CarettiDMPullenPVPremoLAKuhlmannWDReliability of respiratory inductive plethysmography for measuring tidal volume during exerciseAm Ind Hyg Assoc J199455109189237977031
- VogelsRPedleyMAlivertiAIlesRNon-invasive assessment of lung function, with reference to external light-based techniquesERS Buyers GuideEuropean Respiratory Society2012 Available from: http://www.ersbuyersguide.org/articles/previous-issues/20122013/item/noninvasive-assessment-of-lung-functionAccessed December 10, 2015
- IlesRMotamedi-FakhrSDe BoerWConlonJKhalidAWilsonRCComparison of tidal breathing indices measured simultaneously using pneumotachography and structured light plethysmography (SLP)Am J Respir Crit Care Med2015191A2111
