Abstract
Purpose
Accurate and precise needle placement is of utmost importance in interventional radiology. However, targeting can be challenging due to, eg, tissue motion and deformation. Steerable needles are a possible solution to overcome these challenges. The present work studied the clinical need for steerable needles. We aimed to answer three subquestions: 1) What are the current challenges in needle placement? 2) What are allowable needle placement errors? and 3) Do current needles need improvement and would steerable needles add clinical value?
Methods
A questionnaire was administered at the Annual Meeting of Cardiovascular and Interventional Radiology Society of Europe in 2016. In total, 153 respondents volunteered to fill out the survey, among them 125 (interventional) radiologists with experience in needle placement.
Results
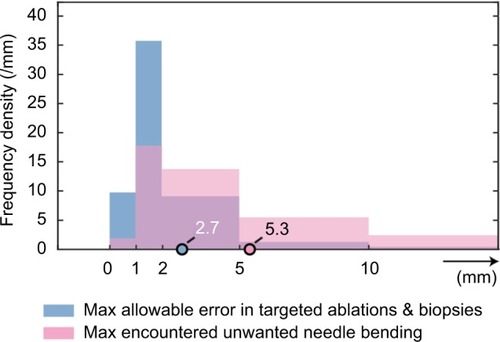
1) Current challenges in needle placement include patient-specific and technical factors. Movement of the target due to breathing makes it most difficult to place a needle (90%). 2) The mean maximal allowable needle placement error in targeted lesions is 2.7 mm. A majority of the respondents (85%) encounter unwanted needle bending upon insertion. The mean maximal encountered unwanted needle bending is 5.3 mm. 3) Needles in interventional radiology need improvement, eg, improved needle visibility and manipulability, according to 95% of the respondents. Added value for steerable needles in current interventions is seen by 93% of the respondents.
Conclusion
Steerable needles have the potential to add clinical value to radiologic interventions. The current data can be used as input for defining clinical design requirements for technical tools, such as steerable needles and navigation models, with the aim to improve needle placement in interventional radiology.
Introduction
In interventional radiology, needles are placed under image guidance into organs to treat or diagnose patients, eg, in thermal ablation and biopsy procedures, respectively. However, accurate and precise needle placement is challenging, due to several patient-specific and technical factors, such as tissue motion and deformation. Solutions to challenges in needle placement can, eg, be found in developments in imaging, improved instruments and guiding tools, and better training. One proposed technical innovation to overcome some of the challenges in needle placement, and thus decreasing the needle placement error in interventional radiology, is a steerable needle. Such a needle would not only help in decreasing the placement error, but also in reducing the number of punctures and lowering the overall procedure time.
Background on steerable needles and mechanisms
Several medical engineering research groups are working on the development of steerable needles. According to research, these needles can be used to correct unwanted needle bending and lesion motion,Citation2,Citation3 actively steer around anatomical obstacles,Citation2 or even reach anatomical targets that are not accessible using conventional needles.Citation4,Citation5
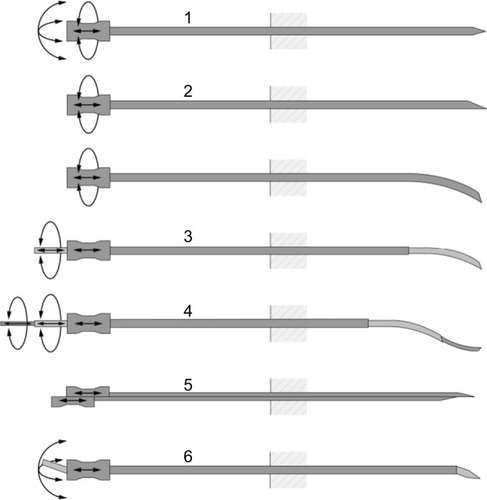
An extensive review on design choices in needle steering is given by van de Berg et al.Citation1 shows various passive and active needle steering mechanisms. Examples of passive steering mechanisms are manipulation at the base of the needle and asymmetric bevel tip needles. Examples of active mechanisms include precurved needle stylets, active cannulas, programmable bevel tips, and tendon-actuated active needle tips. In addition, an overview of needle-like instruments for steering through solid organs is given by Scali et al.Citation6
Figure 1 Examples of steerable needles and their degrees of freedom in actuation.
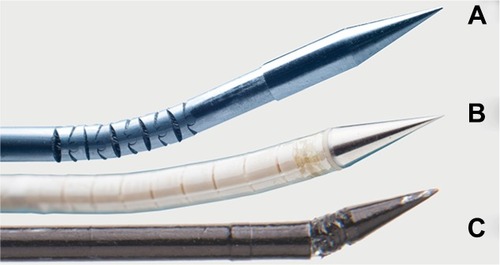
Examples of three steerable needle prototypes with tendon-actuated active needle tips are given in . Typically, these needles can be manipulated at the base of the needle to change the direction of the needle tip, after which the shaft of the needle follows upon insertion. They range from 0.8 mm to about 3 mm in diameter and have roughly the same diameter as needles that are currently clinically used in interventional radiology (~0.5–2.5 mm). Steerable needle prototypes can either be manually inserted,Citation7–Citation9 robotically controlled,Citation10,Citation11 or inserted with a hybrid approach.Citation12,Citation13
Figure 2 Examples of steerable needle prototypes.
Notes: (A) A steerable needle with stainless steel segments, (B) an MRI-compatible steerable needle, and (C) a needle with a steerable tip positioned on top of a miniature ball joint (all prototypes designed and fabricated in the MISIT lab of the Delft University of Technology, the Netherlands).
Steerable needles have mostly been tested in experimental settings with the use of a phantom material or animal tissue. For example, Majewicz et alCitation14 studied the repeatability of tip-steerable needle insertions in ex vivo and in vivo canine prostate, kidney, and liver tissue. On top of that, some experiments have been performed in a clinical environment. Podder et alCitation15 studied the dosimetric benefit of a curvilinear distribution of seeds for low-dose-rate prostate brachytherapy, by inserting the seeds using a smart bevel tip needle into patients. Furthermore, Murphy et alCitation16 described the novel use of a curved steerable needle to access symptomatic osseous lesions in the pelvis and sacrum of seven patients.
Rationale and goal
Nowadays, steerable needles are technically feasible to make and produce. However, the current general purpose steerable needle may not be the optimal solution, as a result of 1) the wide variety of clinical tasks in which needles are used in interventional radiology, 2) the case-specific level of task difficulty, and 3) the physiological and anatomical variations within and among patients. Instead, specialized instrument designs may have to be developed to aid specific clinical tasks. To develop such clinically relevant technical tools to improve needle placement, we need more insight into the clinical practice, such as the challenges in needle placement, the magnitude of needle placement errors, and the difficulties in interventions. The clinical view of experts on this matter is crucial for defining the proper indications for needle steering in clinical practice, but also for retrieving the right design criteria for these needles.
Therefore, the goal of the current study was to provide insight into the experts’ view on needle placement errors in interventional radiology and their view on the clinical applicability of steerable needles, by means of a questionnaire. The main question that is aimed to be answered is as follows: Is there a clinical need for steerable needles in interventional radiology? This question was divided into three subquestions:
What are the challenges in needle placement in interventional radiology?
What is the acceptable needle placement error in current clinical practice?
Do current needles in interventional radiology need improvement, and when and where would steerable needles add clinical value?
Methods
Research tool and respondents
A questionnaire was constructed by medical engineers and pretested by interventional radiologists. A summarized version of the questionnaire can be found in . The questionnaire was divided in accordance to the subquestions. The section focused on the added value of steerable needles was only filled out by the respondents that shared the opinion that steerable needles would be of added value. All questions were multiple choice, with the ability to add comments, if necessary. Questions regarding the opinion of the respondents were either yes/no questions, or Likert-type (ordinal data) questions with five items.
The questionnaire was conducted at the Annual Meeting of Cardiovascular and Interventional Radiology Society of Europe in 2016, at the technical exhibition. Visitors were asked to fill out the questionnaire and were told that the study investigated the view of clinical experts on needle placement in general and their view on the clinical applicability of steerable needles. In addition, a demonstration of several steerable needle prototypes was given, to familiarize the participants with this concept. Potential participants were approached personally. Data were collected by self-completion of paper questionnaires with the surveyors present.
Review for this research by an institutional review board and written informed consent from the respondents was not required, as we did not record any personal details of the respondents. Furthermore, all data were anonymously processed and archived to ensure privacy of the respondents.
Data analysis
Response data were analyzed using Matlab 2016b. All (sub) questions were checked for missing data. The percentage of missing data was calculated per question and reported when higher than 20%.
Ordinal Likert-type data are displayed using diverging stacked bar charts. Row counts, ie, the number of radiologists that answered the specific question, are provided for each individual subquestion. Answers were sorted based on the frequencies of positive answers.
Unequal interval data are presented using frequency density histograms with different bin width. Mean values were calculated by multiplying the central x-values of the bin width to the corresponding frequency, after which the summation of these products was divided by the total number of respondents. The mean values were compared among subquestions.
The data from the remaining multiple choice questions regarding clinical interventions are illustrated using bar graphs. Frequencies of the answers to the yes/no questions were calculated and are presented in text.
Results
Descriptive statistics
In total, 153 persons filled out the questionnaire voluntarily. A majority of them were (interventional) radiologists with experience in needle placement (n=125, 82%), and were included for further analysis. Other respondents included, but were not limited to, surgeons, medical doctors, and students. The (interventional) radiologists consisted of participants from 40 different countries, with different levels of experience: they all had at least 1 year of experience, whereas 50% of the respondent group had over 10 years of experience.
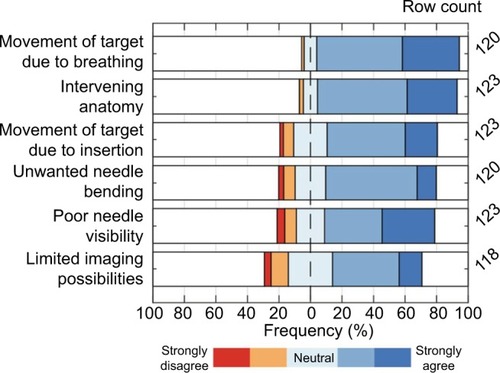
Challenges in needle placement
Respondents experience challenges in needle placement in interventional radiology. The overall agreement with each complicating factor is shown in . These factors can be divided into patient-specific and technical factors. Examples of patient-specific characteristics that make it difficult to reach a target are movement of the target due to breathing of the patient, intervening anatomy between needle tip and target (eg, ribs and large blood vessels), and movement of the target upon needle insertion. Examples of technical factors are unwanted needle bending/deflection inside tissue, poor needle visibility, and limited imaging possibilities. The figure shows that 90% of the respondents (strongly) agree that the target reachability is complicated by target movements due to breathing, whereas 57% (strongly) agree that the current limits to imaging possibilities play a role. In general, patient-specific factors make it more difficult to reach a target than technical factors, according to the radiologists.
Needle placement errors
The aforementioned factors can contribute to needle placement errors, ie, the difference between the needle tip position and its intended position. The respondents were asked to indicate the maximal allowed needle placement error when targeting lesions and to estimate the maximally encountered unwanted needle bending. The results are depicted in . Note that three percent of the respondents indicated that zero error is accepted in needle placement. The mean maximal acceptable error was 2.7 mm, as indicated by the circle in the figure. Significant unwanted needle bending in interventions is experienced by 85% of the respondents. The maximal encountered unwanted needle bending is shown in the same figure, by means of the pink bars. The mean maximal encountered unwanted needle bending in interventions was 5.3 mm.
Figure 5 Frequency density distribution of the maximal allowable placement error (mean 2.7 mm) and the maximal encountered unwanted needle bending (mean 5.3 mm).
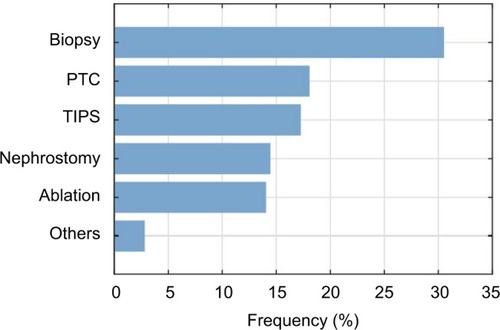
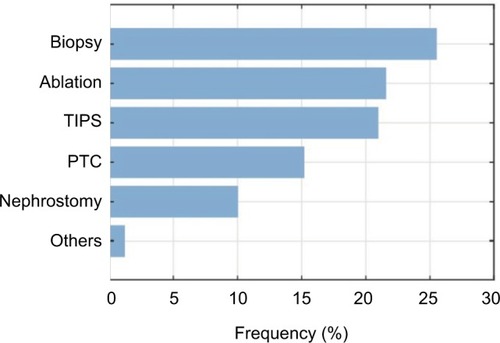
illustrates the procedures in which the respondents encounter significant needle bending. Biopsies were named the most common ones (>30%), whereas the other procedures were relatively close to each other, and named less frequently.
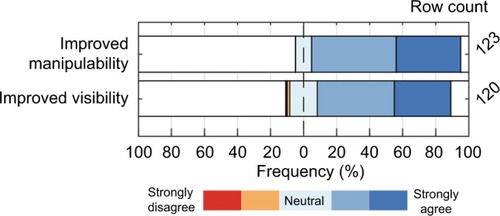
Improving needles
Most radiologists (95%) share the opinion that current needles in interventional radiology need improvement. The respondents were asked to indicate the extent of their agreement on improvement aspects. In , it can be seen that within the respondent group, the desire for an improved needle manipulability/steerability was even larger than the desire for an improved needle visibility. The percentages of the respondents that (strongly) agreed with these desires were 90% and 81%, respectively.
Figure 7 The extent of agreement on “needles in radiology should have improved manipulability and/or improved visibility.”
A majority of the respondent group (93%) see added value for steerable needles in interventional radiology. Their preferred actuation method for steerable needles would be manual (91%), with a minority in favor of robotic (9%). However, a preference, here, was indicated by only 42% of the respondents.
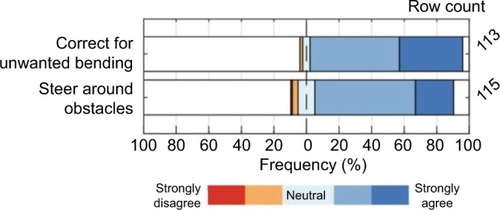
shows the added value of steerable needles, according the respondent group. The greater number of respondents (94%) agree to some extent that these needles would be helpful to correct for unwanted needle bending to steer actively toward the target, whereas 85% of the respondents agree on this for steering around anatomic obstacles.
Figure 8 The extent of agreement on “the added value of a steerable needle is its ability to correct for unwanted bending and/or steer around obstacles.”
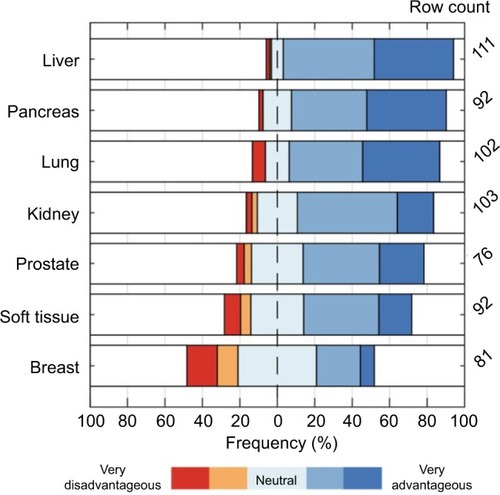
In addition, the respondents were asked to assess the potential benefit of steerable needles for targeted lesions. Results are shown in . According to the respondents, a steerable needle would be most advantageous for interventions in the liver (91% advantageous, 3% disadvantageous) and least advantageous for interventions in the breast (31% advantageous, 27% disadvantageous). Missing data of more than 20% were found for the prostate and breast.
Figure 9 The extent of agreement on “steerable needles would be advantageous for targeted lesions in the specified organs.”
shows the respondents’ view toward the question: “for which specific interventions would a steerable needle be of added value?” The most frequently named was the biopsy procedure, with 25.5%, whereas nephrostomy and others were named less frequently.
Figure 10 Frequency bar chart of the interventions in which a steerable needle would be of added value (n=125).
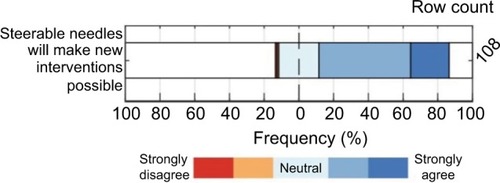
Finally, respondents were asked to what extent they agreed on the following statement: “steerable needles would make new interventions possible,” and the results are shown in . Seventy five percent of the radiologists (strongly) agreed on this, whereas 2% (strongly) disagreed.
Discussion
This is the first time, to the authors’ knowledge, that a structured research has been carried out on the challenges in needle placement in interventional radiology, and the view of clinical experts on steerable needles, by means of a questionnaire. The present study revealed the most prevalent and important problems in needle placement in interventional radiology.
Limitations of the study should be taken into account when interpreting the results. First, no exact response rate could be given, due to the fact that the questionnaires were manually administered at the Annual Meeting of Cardiovascular and Interventional Radiology Society of Europe. Second, the respondents that were willing to fill out the questionnaire may be biased in favor of new technologies such as steerable needles. However, given the large number of respondents, it is assumed that the presented survey sample gives a representative image of the interventional radiologists’ view.
Although most questions had high completion rates, the percentage of missing data was higher than 20% for the question regarding preferred actuation method for steerable needles. Moreover, the row counts for prostate and breast, as shown in , are below 80% (61% and 65%, respectively). Possible explanations could be the low familiarity with the associated interventions and or definitions.
In the current large-scale questionnaire among radiologists, it has been demonstrated that the alleged minimally required accuracy for needle placement is not sufficiently reached in clinical practice. The respondents ranked possible factors that can contribute to needle placement errors. Among respondents, steerable needles were considered a viable alternative to improve current interventions.
It should be noted that the developments in image guidance systems needed for steerable needle imaging were not part of the focus of the presented work. Nonetheless, we stress the importance of reliable and robust imaging systems to be used with steerable needles, as these needles move out-of-plane in conventional two dimensional ultrasound imaging. We believe that 3D ultrasound will be a good solution to this problem, only if the resolution is improved. A recent study showed that needles with arrays of kerfs, often found in compliant joint structures of tip-steered needles, have better contrast-to-noise ratio on ultrasound images than smooth surface needles.Citation17 Another solution would be automatic image guidance to keep the needle tip in plane.Citation18
The findings of the current study can guide medical engineers in their developments of technical tools to improve needle placement accuracy and precision in clinical practice. More specifically, this will result in improved understanding of the clinical context for engineers to work with and could result in enhanced clinical design requirements for steerable needles and other technical tools in interventional radiology.
Conclusion
The answers to the questions stated in the “Introduction” section are as follows:
Challenges in needle placement in interventional radiology concern patient-specific and technical factors. Remarkably, the respondents found patient-specific factors more of a challenge than the technical factors. For people involved in the development of new medical tools for interventional radiology, the take-home message is therefore to focus not only on improving imaging quality and needle visibility, but also on finding solutions for patient-specific challenges. One could think of steerable needles that can be steered during insertion, but also path planners that incorporate breathing motion of the patient and tissue properties.
Significant unwanted needle bending is experienced by the majority of the interventional radiologists (85%). Unwanted needle bending complicates placing the needle at the right spot, induces repuncturing, and thus increases procedure time. The mean maximal encountered unwanted needle bending in interventional procedures is 5.3 mm. However, the mean acceptable needle placement error in targeted lesions is considered as small as 2.7 mm. This implies that unwanted needle bending, which is only one complicating factor in needle placement, is higher than what is considered acceptable.
Current needles in interventional radiology need improvement, according to 95% of the (interventional) radiologists. One might think of improved manipulability/steerability, but also improved needle visibility. According to 93% of the respondents, steerable needles would be of added value in interventional radiology. More specifically, most clinical added value can be found for biopsies and ablations in livers. In addition to these conclusions, most of the interventional radiologists foresee that steerable needles not only would add clinical value to current procedures, but also would make new interventions possible.
All in all, we can conclude that steerable needles have the potential to add clinical value to current procedures, with the aim to improve needle placement in interventional radiology.
Acknowledgments
We thank all respondents at CIRSE Congress 2016 for filling out our questionnaire and giving valuable clinical feedback, as well as the organizing committee of CIRSE for allowing us to attend the technical exhibition to conduct this study. This work was supported by the Netherlands Organization for Scientific Research (NWO) (nr. 12709).
Disclosure
The authors report no conflicts of interest in this work.
References
- van de BergNJvan GerwenDJDankelmanJvan den DobbelsteenJJDesign choices in needle steering – a reviewIEEE/ASME T Mech201520521722183
- WebsterRJIIIMemisevicJOkamuraAMDesign considerations for robotic needle steeringProceedings of the 2005 IEEE International Conference on Robotics and Automation, 2005ICRA 2005Barcelona, SpainIEEE200535883594
- KratchmanLBRahmanMMSaundersJRSwaneyPJWebsterRJIIIToward robotic needle steering in lung biopsy: a tendon-actuated approachProceedings of the Society of Photographic Instrumentation Engineers (SPIE), Medical Imaging: Visualization, Image-Guided Procedures, and ModelingFebruary 2011Florida, USA
- CowanNJGoldbergKChirikjianGSRobotic needle steering: design, modeling, planning, and image guidanceRosenJHannafordBSatavaRMSurgical Robotics - Systems, Applications, and VisionsNew YorkSpringer2011557582
- ReedKBMajewiczAKallemVRobot-assisted needle steeringIEEE Rob Autom Mag2011183546
- ScaliMPuschTPBreedveldPDodouDNeedle-like instruments for steering through solid organs: A review of the scientific and patent literatureProc Inst Mech Eng H2017231325026528056627
- OkazawaSEbrahimiRChuangJSalcudeanSERohlingRHand-held steerable needle deviceIEEE/ASME Trans Mech2005103285296
- van de BergNJDankelmanJvan den DobbelsteenJJEndpoint accuracy in manual control of a steerable needleJ Vasc Interv Radiol2017282276283.e227720573
- SearsPDupontPA steerable needle technology using curved concentric tubesIEEE/RSJ International Conference on Intelligent Robots and SystemsBeijing, China9–15 October 200628502856
- NeubachZShohamMUltrasound-guided robot for flexible needle steeringIEEE Trans Biomed Eng201057479980519709957
- GilbertHBNeimatJWebsterRJIIIConcentric tube robots as steerable needles: achieving follow-the-leader deploymentIEEE Trans Robot201531224625826622208
- RossaCTavakoliMIssues in closed-loop needle steeringControl Eng Pract2017625569
- RossaCUsmaniNSlobodaRTavakoliMA hand-held assistant for semiautomated percutaneous needle steeringIEEE Trans Biomed Eng20176463764828113208
- MajewiczAMarraSPvan VledderMGBehavior of tip-steerable needles in ex vivo and in vivo tissueIEEE Trans Biomed Eng2012592705271522711767
- PodderTKDickerAPHutapeaPDarvishKYuYA novel curvilinear approach for prostate seed implantationMed Phys20123941887189222482610
- MurphyDTKorzanJROuelletteHALiuDMClarksonPWMunkPLDriven around the bend: novel use of a curved steerable needleCardiovasc Intervent Radiol201336253153523070100
- van de BergNJSánchez-MargalloJALangøTvan den DobbelsteenJJCompliant joint echogenicity in ultrasound images: towards highly visible steerable needlesProc SPIE 10576X Medical Imaging2018
- KallemVCowanNJImage guidance of flexible tip-steerable needlesIEEE Trans Robot200925119119620431694