Abstract
Purpose
This study was performed to investigate the primary patency rate and catheter-related problems associated with use of the femoral vein as a route for tunneled hemodialysis catheterization compared with those of the right internal jugular vein as the first-choice route in patients undergoing maintenance hemodialysis.
Patients and methods
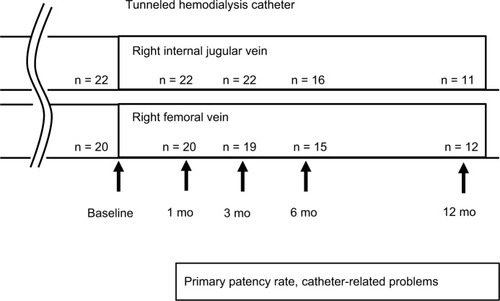
Twenty-two patients underwent placement of indwelling tunneled hemodialysis catheters in the right internal jugular vein as the first option for maintenance hemodialysis, and 20 patients underwent placement in the right femoral vein as the second option. The primary patency rate of the catheters and catheter-related problems at 1, 3, 6, and 12 months after placement were investigated.
Results
The 1-, 3-, 6-, and 12-month primary patency rates of the tunneled hemodialysis catheters in the right internal jugular vein were 95.5%, 95.5%, 81.3%, and 58.3%. The primary patency rates of the catheters in the right femoral vein were 95.0%, 89.5%, 86.7%, and 66.7%. There were no statistically significant differences in the primary patency rates at 1, 3, 6, and 12 months or in catheter-related problems between the right internal jugular vein and right femoral vein.
Conclusion
The primary patency rate and catheter-related problems of indwelling tunneled hemodialysis catheters placed in the right femoral vein were not different from those in the right internal jugular vein in patients undergoing maintenance hemodialysis. These results suggest that the right femoral vein might be a useful option for placement of indwelling tunneled hemodialysis catheters in patients undergoing maintenance hemodialysis.
Introduction
The number of patients with end-stage chronic kidney disease requiring hemodialysis is increasing worldwide.Citation1 Vascular access is necessary for conductance of hemodialysis. A native arteriovenous fistula or, when this is difficult to establish, an arteriovenous graft is considered the preferable vascular access for maintenance hemodialysis because these access sites are durable with repeated use and have less risk of access-related problems such as access failure and infection. However, many patients with end-stage chronic kidney disease have concomitant diseases that impair blood vessels, such as diabetes mellitus and arteriosclerosis.Citation2 In these patients, a tunneled hemodialysis catheter may be selected for vascular access because an arteriovenous fistula or arteriovenous graft would be difficult to establish using the patient’s impaired blood vessels. In addition, a tunneled hemodialysis catheter is reportedly useful for vascular access in patients with acute kidney injury,Citation3 patients with end-stage chronic kidney disease who require temporary vascular access for transient hemodialysis before renal transplantation, and patients who must wait for the development of an arteriovenous fistula or arteriovenous graft for maintenance hemodialysis after an operation. A previous study showed that a tunneled hemodialysis catheter should be employed in patients who are expected to have an indwelling hemodialysis catheter for more than 14 days.Citation4
The right internal jugular vein has been recommended as the first option for placement of a tunneled hemodialysis catheter because it runs in a straight line at a superficial site in the neck, resulting in high accessibility and fewer catheter-related problems.Citation5 For patients with problems such as occlusion of the right internal jugular vein, insertion of a pacemaker in the right chest, or difficulty maintaining the required surgical position, use of the left internal jugular vein or bilateral femoral veins may be considered.Citation5 Among these veins, the left internal vein and left femoral vein run crookedly; thus, they may be associated with a risk of catheter-related complications. Indeed, the left internal jugular vein reportedly has a higher risk of catheter-related difficulties than the right internal jugular vein.Citation5–Citation7 Although several studies have been performed to investigate the femoral vein as a route for tunneled hemodialysis catheterization in patients undergoing maintenance hemodialysis, the availability and risk of the right femoral vein for an indwelling tunneled hemodialysis catheter has not been fully clarified.Citation8–Citation11 In the present study, we retrospectively compared the primary patency rate and catheter-related problems of the right femoral vein versus the right internal jugular vein as the first-option route for tunneled hemodialysis catheterization in patients undergoing maintenance hemodialysis.
Materials and methods
This retrospective cohort study was performed in a single dialysis center to investigate the availability of the right femoral vein as a route for tunneled hemodialysis catheterization in patients undergoing maintenance hemodialysis from May 2013 to June 2016 in Hidaka Hospital. This study was performed in accordance with the ethical principles of the Declaration of Helsinki and was approved by the ethics committee of Hidaka Hospital. The patient consent to review their medical records was not required by the ethics committee of Hidaka Hospital because this study examined a retrospective cohort by analyzing the past medical history. The patient data were kept confidential.
Tunneled hemodialysis catheter
The tunneled hemodialysis catheter used for both the bilateral internal jugular veins and bilateral femoral veins was 19 cm long with a 12.5-French bore size (Soft-Cell; C. R. Bard Inc., Murray Hill, NJ, USA) (). All catheter insertions and placements were performed by transplant surgeons from our hemodialysis center using a Seldinger guidewire technique with ultrasound guidance in the fluoroscopy suite of Hidaka Hospital. In accordance with the Japanese Society for Dialysis Therapy Guidelines of Vascular Access Construction and Repair for Chronic Hemodialysis, the right internal jugular vein was selected as the first-choice access vein because it has high accessibility and a straight route in the neck, resulting in high patency and fewer catheter-related problems such as catheter dysfunction and infection.Citation5 In patients with complications such as occlusion of the right internal jugular vein, insertion of a pacemaker in the right chest, or difficulty maintaining the required surgical position for placement of an indwelling tunneled hemodialysis catheter, the right femoral vein was selected as the second option. The tip of the indwelling tunneled hemodialysis catheter in the right femoral vein was confirmed to be localized in the inferior vena cava, on the more cranial side of the joint portion of the right and left femoral veins. The exit site of the indwelling tunneled hemodialysis catheter in the right femoral vein was located at the skin 8–10 cm caudal to the right inguinal ligament. When use of the right internal jugular vein and right femoral vein was problematic, the left internal jugular vein and left femoral vein were selected as the third and fourth options, respectively. The tunneled hemodialysis catheter was used during hemodialysis and locked with 2,000 units (2.0 ml) of heparin solution in both the venous- and arterial-side tubes after each hemodialysis session. The patients were advised to maintain a clean vascular access site and avoid bending the tunneled hemodialysis catheter. The patients could bend their hips, but they were advised not to squat.
Primary patency rate of tunneled hemodialysis catheter and catheter-related problems
The primary patency rate of the tunneled hemodialysis catheters and catheter-related problems, including catheter dysfunction and infection, were investigated at 1, 3, 6, and 12 months after catheter insertion. Catheter dysfunction was defined when the blood flow rate was <120 ml/min despite an attempt to salvage the catheter by urokinase injection into the catheter. When catheter dysfunction was diagnosed, the catheters were removed. Catheter-related infections included exit site infections and bloodstream infections. An exit site infection was defined as the presence of flare, swelling, and existence of pus at the exit site in the skin. When an exit site infection was diagnosed, the exit site was washed with normal saline solution. A bloodstream infection was diagnosed when a blood culture was positive for bacterial pathogens and other infectious sites were not observed or not likely to be the origin of the bacteria. When a bloodstream infection was diagnosed, the catheters were removed.
Patients
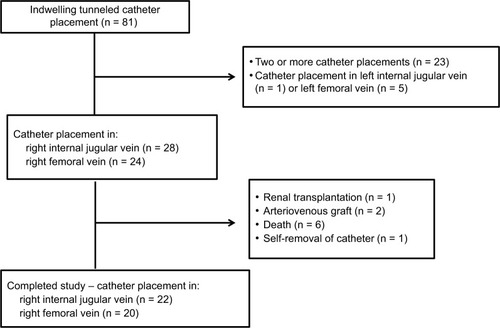
The patient flow chart is shown in . Eighty-one patients underwent maintenance hemodialysis with an indwelling tunneled hemodialysis catheter in the internal jugular vein or femoral vein from May 2013 to June 2016 in Hidaka Hospital. Of these 81 patients, 23 were excluded from this study because they had a history of indwelling tunneled hemodialysis catheter placement before the study period, and 6 were excluded because the tunneled hemodialysis catheter was placed in the left internal jugular vein as a third option (1 patient) or left femoral vein as a fourth option (5 patients). During the observation period, we also excluded 10 patients who underwent renal transplantation (1 patient), underwent arteriovenous grafting (2 patients), died of catheter-unrelated diseases (6 patients), and removed the tunneled hemodialysis catheter because of delirium (1 patient). The remaining 42 patients who underwent placement of an indwelling tunneled hemodialysis catheter in the right internal jugular vein as the first option (22 patients) and right femoral vein as the second option (20 patients) were analyzed (). Among these 42 patients, 23 patients were followed up for 12 months, 8 patients were followed up for 6 months, 10 patients were followed up for 3 months, and 1 patient was followed up for 1 month ().
Parameters of hemodialysis
Single pooled KT/V (spKT/V) values were calculated each month by previously reported formulae.Citation12 The median spKT/V was calculated for each patient after placement of the indwelling tunneled hemodialysis catheter.
Statistical analysis
Data are expressed as median and range. Statistical analysis was performed using the Mann–Whitney U test; a p value of <0.05 was considered statistically significant. Logistic regression analysis was used to detect independent predictors of catheter survival.
Results
The 42 analyzed patients underwent placement of indwelling tunneled hemodialysis catheters because of problems associated with their existing arteriovenous fistula or arteriovenous graft, including occlusion (18 patients), steal syndrome (3 patients), rupture or varicose of the arteriovenous fistula (4 patients), severe puncture pain (2 patients), and difficult general conditions for creation of the arteriovenous fistula or arteriovenous graft such as a bed-bound status (6 patients), marked edema (5 patients), and mental disorders (4 patients). Among the 42 patients, 22 underwent placement of the indwelling tunneled hemodialysis catheter in the right internal jugular vein as the first option. Among these 22 patients, 18 (81.8%) could ambulate and 4 (18.2%) were bedridden or had very low activity. The remaining 20 patients underwent placement in the right femoral vein as the second option because of occlusion of the right internal jugular vein (5 patients), presence of a pacemaker (1 patient) or central vein port (1 patient) in the right chest, or difficulty maintaining the required surgical position for the following reasons: bedridden status (6 patients), mental disorders (4 patients), and neck diseases such as cervical vertebral syndrome (3 patients). Among these 20 patients, 12 (60.0%) could ambulate and 8 (40.0%) were bedridden or had very low activity. The details of the patients and their hemodialysis conditions are summarized in . The patients’ mean body mass index was 20.3 ± 6.2 kg/m2. No major complications occurred during catheter insertion, including hematoma, air embolism, or pneumothorax formation, in all patients in both the right internal jugular vein and right femoral vein groups.
Table 1 Patients’ characteristics
Hemodialysis conditions
The blood flow rate from the tunneled hemodialysis catheter was set at 150 ml/min in all patients to prevent interruption of the hemodialysis session due to catheter dysfunction. The KT/V of patients who underwent placement of indwelling tunneled hemodialysis catheters in the right internal jugular vein was 1.40 (1.2–1.62). The KT/V of patients who underwent placement of indwelling tunneled hemodialysis catheters in the right femoral vein was 1.19 (0.91–1.47).
Primary patency rate of tunneled hemodialysis catheter
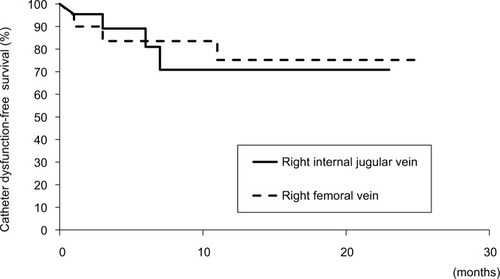
The primary patency rate of the catheters in the right internal jugular vein was 95.5% (21/22) at 1 month, 95.5% (21/22) at 3 months, 81.3% (13/16) at 6 months, and 58.3% (7/11) at 12 months. The primary patency rate of the catheters in the right femoral vein was 95.0% (19/20) at 1 month, 89.5% (17/19) at 3 months, 86.7% (13/15) at 6 months, and 66.7% (8/12) at 12 months. There was no statistically significant difference in the patency of the tunneled hemodialysis catheters in the right internal jugular vein versus right femoral vein at 1, 3, 6, and 12 months (). No factors, including age, sex, body mass index, dialysis condition, spKT/V, coexisting diseases, and medications, were significantly associated with catheter survival in patients with an indwelling tunneled hemodialysis catheter in either the right internal jugular vein or right femoral vein.
Table 2 Primary patency rate of tunneled hemodialysis catheter
Catheter-related problems
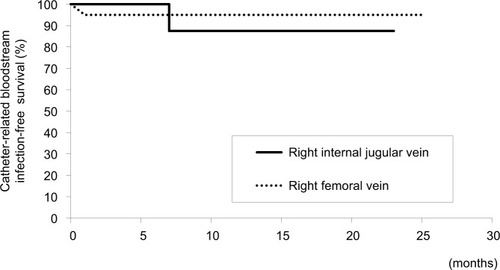
Dysfunction of the tunneled hemodialysis catheter was observed in 3 patients with an indwelling tunneled hemodialysis catheter in the right internal jugular vein and 3 patients with a catheter in the right femoral jugular vein (). The catheters were removed from these 6 patients. Two patients with an indwelling tunneled catheter in the right internal jugular vein (1 patient) and right femoral vein (1 patient) underwent catheter removal due to catheter-related bloodstream infection (). No exit site infections were observed in patients with an indwelling tunneled hemodialysis catheter in either the right internal jugular vein or right femoral vein. There was no significant difference in catheter-related problems such as catheter-dysfunction and catheter-related infection between the right internal jugular vein and right femoral vein groups ().
Table 3 Catheter-related problems
Discussion
In this study, there was no significant difference in the primary patency rate at 1, 3, 6, and 12 months or in catheter-related problems such as catheter dysfunction and infection between the tunneled hemodialysis catheters in the right internal jugular vein versus right femoral vein among patients undergoing maintenance hemodialysis. These results suggest that the right femoral vein might be a useful option for placement of indwelling tunneled hemodialysis catheters in patients undergoing maintenance hemodialysis.
The right internal jugular vein is reportedly the most effective first option for indwelling tunneled hemodialysis catheters because of its higher rate of primary patency.Citation8,Citation9 A previous study showed that the catheter patency rate at 180 days after indwelling catheter placement was 67.0% in the right internal jugular vein and 14.0% to 27.1% in the femoral vein.Citation8 In contrast, the catheter-related infection rate was not significantly different between the right internal jugular vein and right femoral vein.Citation8–Citation11 In the present study, the 6-month and 12-month primary patency rates of tunneled hemodialysis catheters in the femoral vein were high at 86.7% and 66.7%, respectively, compared with those of previous study.Citation8 The primary patency rate and catheter-related infection rate were not different between the right internal jugular vein and right femoral vein. One study revealed that the hemodialysis catheter-related infection rate was higher in the femoral vein than right internal jugular vein in patients with obesity (body mass index of >28 kg/m2).Citation11 In the present study, the low to moderate body mass index of the studied patients may have contributed to the improved primary patency rate and catheter-related problems, including catheter dysfunction and infection, in the right femoral vein. In addition, we employed a 19-cm-long tunneled hemodialysis catheter for both the right femoral vein and right internal jugular vein because it was long enough for placement in the right femoral vein of all studied patients without obesity. A longer tunneled hemodialysis catheter (35 cm) reportedly causes more catheter-related problems than does a shorter catheter.Citation13 The short length of the tunneled hemodialysis catheter in this study may have also contributed to the improved primary patency rate and catheter-related problems in the right femoral vein. Another possibility is that the advice regarding catheter care provided by the medical staff and the performance of catheter care by the patients in this study might have also contributed to the improved catheter condition. One study revealed that catheter care and antimicrobial treatment performed by the dialysis center staff and patients may contribute to an improved catheter prognosis.Citation9 In the present study, no major complications occurred including hematoma, air embolism, or pneumothorax formation in all patients regardless of catheter location during either the catheter insertion or removal process, and bleeding around catheters during the observation period. These results suggest that the right femoral vein might be a feasible route for placement of an indwelling tunneled hemodialysis catheter and may not have a higher rate of catheter-related problems. The spKT/V was low in patients who underwent placement of indwelling tunneled hemodialysis catheters in the right internal jugular vein (1.40 [1.20–1.62]) and in the right femoral vein (1.19 [0.91–1.47]). An increased blood flow rate or prolonged dialysis time may be necessary for adequate long-term dialysis.
Limitations
This study had some limitations. First, it was a single-center retrospective study, and the number of patients was small. Second, the rate of blood flow from the tunneled hemodialysis catheter was set at 150 ml/min in all patients to prevent interruption of the hemodialysis session due to catheter dysfunction, which may have resulted in low dialysis efficiency. Large-scale, multicenter trials are required to investigate the availability and safety of the right femoral vein for placement of an indwelling tunneled hemodialysis catheter with an increased blood flow rate.
Conclusion
The primary patency rate and catheter-related problems of tunneled hemodialysis catheters in the right femoral vein were not different from those in the right internal jugular vein as a first option in patients undergoing maintenance hemodialysis. These results suggest that the right femoral vein might be a useful option for indwelling tunneled hemodialysis catheters in patients undergoing maintenance hemodialysis.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors thank the members of the Division of Nephrology, First Department of Integrated Medicine, Saitama Medical Center, Jichi Medical University, and Department of Dialysis and Transplant Surgery, Hidaka Hospital, Gunma, Japan. The authors also thank Angela Morben, DVM, ELS, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
This study was supported by the Division of Nephrology, First Department of Integrated Medicine, Saitama Medical Center, Jichi Medical University, Saitama, Japan.
Disclosure
The authors report no conflicts of interest in this work.
References
- LiyanageTNinomiyaTJhaVWorldwide access to treatment for end-stage kidney disease: a systematic reviewLancet201538599811975198225777665
- US Renal Data SystemUSRDS 2009Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States2 Chapter 2Incidence & prevalence of ESRD Bethesda, MDNational Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases2009
- CoryellLLottJPStavropoulosSWThe case for primary placement of tunneled hemodialysis catheters in acute kidney injuryJ Vasc Interv Radiol200920121578158119944983
- WeijmerMCVervloetMGter WeePMCompared to tunnelled cuffed haemodialysis catheters, temporary untunnelled catheters are associated with more complications already within 2 weeks of useNephrol Dial Transplant200419367067714767025
- KukitaKOhiraSAmanoI2011 update Japanese Society for Dialysis Therapy guidelines of vascular access construction and repair for chronic hemodialysisTher Apher Dial201519Suppl 1139
- KhwajaAKDIGO clinical practice guidelines for acute kidney injuryNephron Clin Pract20121204c179c18422890468
- EngstromBIHorvathJJStewartJKTunneled internal jugular hemodialysis catheters: impact of laterality and tip position on catheter dysfunction and infection ratesJ Vasc Interv Radiol20132491295130223891045
- MayaIDAllonMOutcomes of tunneled femoral hemodialysis catheters: comparison with internal jugular vein cathetersKidney Int20056862886288916316366
- BurtonKRGuoLLTanKTPatency of femoral tunneled hemodialysis catheters and factors predictive of patency failureCardiovasc Intervent Radiol20123561396140222139368
- DuguéAELevesqueSPFischerMOVascular access sites for acute renal replacement in intensive care unitsClin J Am Soc Nephrol201271707722076877
- ParientiJJThirionMMégarbaneBFemoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trialJAMA2008299202413242218505951
- ShinzatoTNakaiSFujitaYDetermination of Kt/V and protein catabolic rate using pre- and postdialysis blood urea nitrogen concentrationsNephron19946732802907936017
- ClarkEKappelJMacRaeJPractical aspects of nontunneled and tunneled hemodialysis cathetersCan J Kidney Health Dis20163205435811666912828270920