Abstract
Endovascular therapy has evolved as a main treatment option especially in patients with short (<25 cm) femoropopliteal lesion. The latest guideline recommends the use of drug-eluting devices (both drug-coated balloons [DCBs] and drug-eluting stents) in short femoro-popliteal lesions as class IIb recommendation. DCB usage is also recommended for in-stent restenosis lesions (class IIb). DCBs are a more attractive treatment option because the lack of metal prosthesis allows for more flexibility in future treatment options including the option of treating nonstenting zones, previously DCB-treated zones with DCBs again. The IN.PACT™ Admiral™ DCB has shown promising clinical performance in several randomized control trials and global registries, and is currently the market DCB leader for the treatment of femoropopliteal lesions with more than 200,000 patients treated thus far. Currently, more than 10 DCBs have received Conformité Européene mark for the treatment of femoropopliteal atherosclerotic disease. Three of these (including IN.PACT Admiral DCBs) have also received Food and Drug Administration approval in the USA. However, some Conformité Européene-marked DCBs have failed to show consistent results in their clinical studies suggesting all DCBs are not created equal. Each DCB is unique (ie, drug type, drug dose, crystallinity, and excipient) with different clinical outcomes. In the current review, we will focus on the preclinical and clinical results of not only IN.PACT Admiral DCB, but also the other currently available DCBs.
Introduction
Peripheral arterial disease (PAD) contributes to significant morbidity and mortality, affecting approximately 202 million adults worldwide in 2010.Citation1,Citation2 The global prevalence of PAD between 2000 and 2010 has increased by 23.5% in low-income and middle-income countries, and 13.1% in high-income countries.Citation3 The prevalence of asymptomatic PAD is in the range of 3%–10% in individuals 50–69 years increasing to 15%–20% in persons >70 years.Citation4 PAD is primarily caused by atherosclerotic disease, with similar risk factors as coronary artery disease (CAD),Citation5 with diabetes and smoking having the greatest impact.Citation6,Citation7 Diagnosis and management of atherosclerosis are critical in the treatment of PAD.
We have recently evaluated the pathological characteristics of legs in patients with history of abundant coronary risk factors,Citation65 and also in patients with critical limb ischemia (CLI).Citation8 The main findings of these studies were as follows:Citation1 intimal and medial calcification (known as Mönckeberg calcification) more commonly observed in both femoropopliteal and infrapopliteal arteries;Citation2 femoropopliteal arteries demonstrated higher prevalence of fibrocalcific plaque than that reported in coronary arteries; focal bone formation is also more frequently found in 83% of lower extremities of these patients, and is most commonly seen in femoropopliteal arteries;Citation3 plaque rupture and calcified nodule are the major causes of acute thrombotic events in femoropopliteal arteries;Citation4 half of the chronic total occlusion lesions in infra-popliteal arteries occurs secondary to distal emboli from upstream thrombotic lesions.
Given the lower risk of periprocedural complications with shorter hospital stays when compared with surgery, endovascular therapy (EVT) has evolved as a main treatment option especially in patients with short (<25 cm) femoropopliteal lesions.Citation1,Citation2 The latest ESC guideline recommends the use of drug-eluting devices (both drug-coated balloons [DCB] and drug-eluting stents [DES]) in short femoropopliteal lesions as class IIb recommendation. DCB usage is also recommended for in-stent restenosis (ISR) lesions (class IIb).Citation1
However, there is a need for further improvement in the DCB/DES technology for optimal treatment of EVT. Target lesion revascularization (TLR) rate 5 years after DES implantation in femoropopliteal arteries is 17%,Citation9 which is higher than that reported in coronary arteries (~10%).Citation10 In addition to the higher rate of stent fracture due to the changes in bio-mechanical forces after stent implantation,Citation11 decreased wall shear stress along the axis of the stented segmentCitation12 contributes to restenosis. Although the prevalence of stent fracture has been significantly decreased with the latest generation DES (1.9% in the 5 years follow-up),Citation9 DCBs are a more attractive treatment option because the lack of metal prosthesis allows for more flexibility in future treatment options including the option of treating nonstenting zones, previously DCB-treated zones with DCBs again.
The IN.PACT™ Admiral™ DCB (Medtronic Vascular, Santa Clara, CA, USA) has shown promising clinical performance in several randomized control trials (RCTS) and global registries,Citation13–Citation18 and is currently the market DCB leader for the treatment of femoropopliteal lesions with more than 200,000 patients treated thus far.Citation19 Currently, more than 10 DCBs have received Conformité Européene (CE) mark for the treatment of femoropopliteal atherosclerotic disease. Three of these (including IN.PACT Admiral DCB) have also received Food and Drug Administration (FDA) approval in the USA (). However, some CE-marked DCBs have failed to show consistent results in their clinical studies suggesting all DCBs are not created equal. Each DCB is unique (ie, drug type, drug dose, crystallinity, and excipient) with different clinical outcomes. In the current review, we will focus on the preclinical and clinical results of not only IN.PACT Admiral DCB, but also the other currently available DCBs.
Table 1 CE-marked DCBs
Drug effect of DCBs
Uncoated balloon angioplasty (BA) failed to show acceptable clinical outcomes, primarily due to high restenosis rates of 40%–50% at 12 months follow-up and lack of durability of the treatment effect.Citation1,Citation2 Mechanical stress due to BA causes injury to endothelial cells and the medial wall, promotes cracking of the plaque, and is followed by a repair mechanism that involves platelet fibrin deposition, inflammation, release of growth factors, and smooth muscle cell (SMC) proliferation with subsequent deposition of matrix proteins. Stimulation of the cell cycle proteins and mitosis results in the final common pathway that leads to intimal hyperplasia by SMCs.Citation20 Drugs used to coat DCBs inhibit SMC mitosis and thereby prevent restenosis. DCBs are composed of three key ingredients that help deliver the drug to the arterial wall; a standard percutaneous transluminal angioplasty (PTA) balloon catheter, anti-restenotic drug (predominantly paclitaxel), and an excipient for the rapid drug delivery and adherence of the drug to the arterial wall to allow continuous diffusion of the drug. Paclitaxel has the advantage of being highly lipophilic and is insoluble in water, binds to and stabilizes polymerized microtubules, thereby preventing mitotic division, apoptosis, and migration at the nanomolar level, preventing neointimal SMC accumulation. The IN.PACT Admiral is coated with the FreePac® coating solution, which is a proprietary coating with a matrix of paclitaxel on the expanded balloon surface. The FreePac coating contains a hydrophilic excipient (urea) that facilitates the release and transfer of paclitaxel to the target lesion.Citation21 The paclitaxel dose is 3.5 µg/mm2 on the balloon surface. The FreePac coating was developed from the original Paccocath product, which had iopromide as an excipient showing significantly better clinical outcomes compared with PTA alone in the THUNDER randomized trial.Citation22,Citation23 Urea is hydrophilic and facilitates hydration of the coating that promotes release and transfers the paclitaxel from the balloon surface to the arterial wall. In addition, the excipient also promotes sustained solid-phase paclitaxel reservoirs in the tissue.Citation21 The solid-phase paclitaxel remains in the arterial wall for >90 days at therapeutic levels (data on file at Medtronic, manuscript under review), which results in longer-term anti-restenotic effect.Citation69 Similar to the THUNDER trial, Liistro et al demonstrated greater efficacy with IN.PACT Admiral DCB + bare metal stents (BMS) when compared with PTA + BMS at both 6 and 12 months.Citation24
Drugs for lesions with PAD
Although DES with Rapamycin analogs have shown superior clinical outcome in CAD compared with a DES with paclitaxel (TAXUS™; Boston Scientific, Natick, MA, USA),Citation25 for femoropopliteal artery disease, self-expanding DES with Rapamycin analogs (sirolimus and everolimus) failed to show a sustained superior clinical outcomes compared with BMS in several RCTs.Citation26,Citation27 On the other hand, the two CE-marked self-expanding paclitaxel-based DES, Zilver® PTX® (Cook Medical, Bloomington, IN, USA) and Eluvia (Boston Scientific), have shown superior clinical outcomes,Citation28,Citation29 with sustained efficacy at 5 years in the former and 2 years in the latter after stent implantation.Citation9
The main determinant of poor outcome with Rapamycin analogs may have been related to continuous expansion of the nitinol stent. Because of continuous expansion, there is greater injury to the arterial wall over time and greater interstrut distance, resulting in inadequate drug distribution and depletion of the drug availability that results in greater neointimal thickening and lack of efficacy.Citation30,Citation31 Paclitaxel eluting stents and balloons have been efficacious in above the knee PAD which may be due to properties of the drug itself as well as improvement in the nitinol stent platform.
Paclitaxel is primarily used because of its high stability and its lipophilic properties, which allow for passive adsorption through the cell membrane with long-term biologic effect. Paclitaxel binds to beta-tubulin and impairs microtubular disassembly and halts the cell replication. On the other hand, sirolimus inhibits mTOR complex 1 that promotes the translation of cyclin D1 mRNA, one of the cell cycle regulators.Citation32 Several preclinical studies demonstrated neointimal inhibition by Rapamycin analogs-coated balloons,Citation33 and one of them has received CE mark approval (XTREME TOUCH; Concept Medical Inc., Surat, India). The other Rapamycin analogs-coated balloon, SELUTION™ DCB (MedAlliance SA, Irvine, CA, USA), has demonstrated relatively low clinically driven TLR (CD-TLR; 2.2%) at 6 months follow-up in the first in man study (SELUTION trial, ClinicalTrials.gov ID: NCT02941224). However, there are no long-term data of RCTs available for Rapamycin analogs-coated balloons, and further studies are needed.
Drug efficacy of IN.PACT Admiral DCB in preclinical studies
Technical features such as drug dose,Citation34 crystallinity, drug coating integrity, and excipientCitation35 all affect the differences in drug effect across all DCBs (). Several preclinical studies have been performed to compare the paclitaxel tissue levels and drug effect of DCBs. Gongora et al compared paclitaxel tissue levels up to 60 days following treatment with IN.PACT Pacific DCBs, Ranger™ (Boston Scientific), and Lutonix® DCB (BARD, Murray Hill, NJ, USA) in the femoral artery of healthy swine. Although the drug levels were similar at 4 hours, however, higher drug levels were observed thereafter with the IN.PACT Pacific DCB up to 60 days. Neointimal inhibition after DCBs treatment in the ISR model of the familial hypercholesterolemic swine model was also evaluated.Citation36 IN.PACT Pacific DCB demonstrated not only the highest paclitaxel tissue concentration when compared with Ranger and Lutonix DCB especially at 28 days after the treatment, but also the highest neointimal inhibition. As shown in , the drug levels on the balloon are highest for IN.PACT (3.5 µg/mm2) vs all other DCB (Ranger and Lutonix 2.0 µg/mm2). As the “ideal” tissue drug concentration to prevent restenosis in patients still remains unknown, further studies are needed.
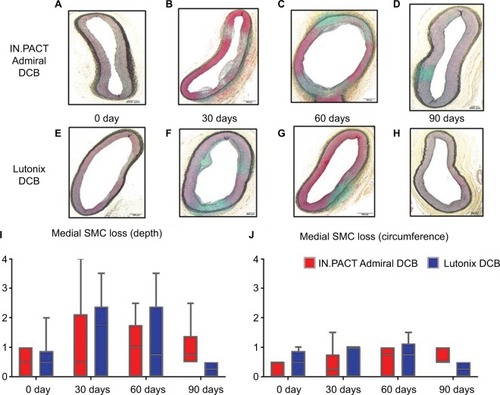
Our preclinical studies with IN.PACT Admiral DCB also demonstrated similar differences in the histological findings after treatment of iliofemoral arteries when compared with Lutonix DCB in healthy swine models. Animals were treated with either IN.PACT Admiral DCB or Lutonix DCB and sacrificed at 0 day (n=6 in IN.PACT Admiral, n=8 in Lutonix DCB), 30 days (n=6 per group), 60 days (n=6 per group), and 90 days (n=6 in IN.PACT Admiral, n=8 in Lutonix DCB) after the treatment. Histologic sections of the treated lesions were examined for SMC cell loss (depth and circumferential) as an indicator of drug effect for both DCBs.
In addition to histological analysis, the mid sections of the treated arterial tissues at 0 and 90 days were also submitted for paclitaxel concentration. Although paclitaxel concentration at 0 day post treatment was similar between IN.PACT Admiral DCB and Lutonix DCB, IN.PACT Admiral DCB demonstrated significantly higher paclitaxel concentrations at 90 days. Histological analysis showed SMC loss peaked at 30–60 days following treatment, although SMC loss progressively decreases for both at 90 days. However the degree of loss remained significantly higher for IN.PACT Admiral DCB compared with Lutonix DCB (; data on file at Medtronic, manuscript under review).Citation69
Figure 1 Representative images of histological changes after IN.PACT™ Admiral™ DCB and Lutonix® DCB treatments, and histological scores of drug biological effects in the swine femoral artery model.
Abbreviations: DCB, drug-coated balloon; SMC, smooth muscle cell.
Long-term clinical outcome of IN.PACT Admiral DCB
Of the available DCBs, IN.PACT Admiral has shown the longest duration of drug release and has demonstrated durable patency of femoropopliteal arteries in clinical trials compared with BA up to 4 years. IN.PACT SFA trial was a multicenter, prospective, single-blind RCT to evaluate the efficacy and safety of IN.PACT Admiral compared with BA treatment in patients with femoropopliteal PAD. Patients were randomly assigned to DCB or BA in a 2:1 ratio (IN.PACT Admiral DCB; 220, BA; 111; ). The primary efficacy endpoint was primary patency, defined as freedom from restenosis or CD-TLR at 12 months. IN.PACT Admiral DCB resulted in a significantly higher primary patency vs BA (IN.PACT Admiral DCB vs BA: 82.2% vs 52.4%, respectively, P<0.001).
Table 2 Result from RCTs of currently available DCBsTable Footnotea
IN.PACT Admiral DCB demonstrated higher freedom from CD-TLR compared with BA (97.5% vs 79.3%, respectively, P<0.0001). The IN.PACT Admiral DCB also achieved the primary safety endpoint, with a composite of freedom from target limb major amputation and freedom from CD-TLR within 12 months.Citation13 Three-year follow-up also demonstrated higher primary patency in patients treated with IN.PACT DCB compared with BA (69.5% vs 45.1%, respectively, P<0.001) with higher freedom from CD-TLR (84.5% vs 70.4%, respectively, P<0.001).Citation37 Schneider et al recently presented 4 years outcomes of IN.PACT SFA trial at VIVA 2017.Citation66 Four years follow-up assessment was performed with adjudicated CD-TLR conducted via telephone interview, which was defined as any reintervention of the target lesion due to symptoms or drop in ankle-brachial index (ABI) of ≥20% or >0.15) when compared with post-procedure baseline ABI. Freedom from CD-TLR at 4 years remained significantly higher in patients treated with IN.PACT Admiral DCB compared with BA (78.8% vs 70.4%, respectively, log-rank P=0.0399). In addition, there were no target limb major amputations in both groups. In summary, IN.PACT Admiral demonstrated a durable drug effect compared with BA even at 4 years.
RCTs of the other CE-marked DCBs and comparison with IN.PACT SFA
RCTs comparing with BA treatment have also been performed for Lutonix DCB, Ranger, Stellarex™ (Spectranetics, Colorado Springs, CO, USA), Passeo-18 Lux (Biotronik, Bülach, Switzerland), and SeQuent® Please (B. Braun, Melsungen, Germany; ). All these DCBs achieved their primary efficacy endpoint, although the definition of primary efficacy was different in many of these studies (). In RCT for IN.PACT SFA,Citation13,Citation15 Stellarex,Citation38,Citation39 and Lutonix DCB,Citation40 the primary efficacy endpoint was primary patency, defined as freedom from restenosis and CD-TLR at 12 months followup. However, each RCT has a different definition for “restenosis”, assessed as duplex ultrasound peak systolic velocity ratio (2.4 for IN.PACT Admiral DCB, 2.5 for Stellarex and Lutonix). On the other hand, the primary efficacy endpoint of Ranger,Citation41 Passeo-18 Lux,Citation42 and SeQuent PleaseCitation43 was late lumen loss (LLL) at 6 months assessed by angiography. Because patient and lesion characteristics were different in each of these RCTs, they cannot be compared directly. In addition, risk of bias, which is due to incomplete description of random sequence generation and assignment concealment, the infeasibility of operator blinding, and possible conflict of interest, is different in each RCT.Citation44 IN.PACT Admiral DCB demonstrated the lowest rate of CD-TLR compared with the other DCBs. Further RCTs that directly compare different DCBs are needed to explore whether differences in clinical outcomes exists between the various CE-marked DCBs.
In addition to the inconsistent primary endpoints of each RCT, long-term follow-up results are available for only a few DCBs. Similar to IN.PACT SFA trial, LEVANT 2 trial was a multicenter, prospective, RCT to evaluate the efficacy and safety of Lutonix DCB compared with BA treatment in patients with femoropopliteal PAD. Patients were randomly assigned to DCB or BA in a 2:1 ratio (Lutonix DCB, 316; BA, 160; ). The primary efficacy endpoint was primary patency, defined as freedom from restenosis or CD-TLR at 12 months. Lutonix DCB showed a significantly higher rate of primary patency vs BA (Lutonix DCB vs BA: 65.2% vs 52.6%, respectively, P=0.02). Although the primary patency was significantly higher at 2 years, as presented by Rosenfield et al at SVS 2015, the statistical difference was of borderline significance (58.6% vs 53.0%, respectively, P=0.05).Citation67
Two-year follow-up data are also available for the other two CE-marked DCBs, Stellarex (presented at LINC 2018) and SeQuent Please.Citation45 In the ILLUMINATE EU RCT study, Stellarex demonstrated significantly greater freedom from CD-TLR compared with BA arm (Stellarex DCB vs BA: 88.9% vs 71.8%, P<0.001). In CONSEQUENT trial, SeQuent Please DCB arm demonstrated significantly lower TLR compared with BA arm (SeQuent Please DCB vs BA: 19.1% vs 40.6%, P=0.007).
Downstream effect after DCB treatment
Recently, three case reports demonstrated patients with painful rashes in lower leg, 1–2 weeks after DCB treatment suggesting downstream particulate emboli may have resulted in vasculitis or panniculitis. The rash disappeared in 3–4 weeks after oral steroid treatment.Citation46–Citation48
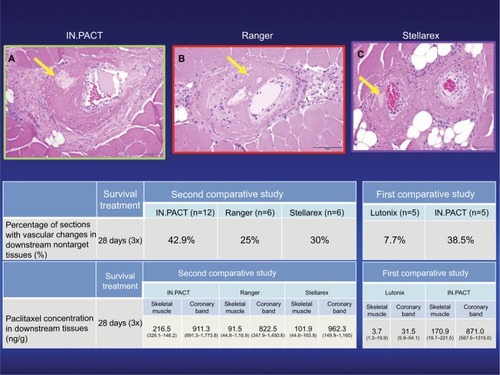
Our published preclinical study evaluated the extent of distal embolization following femoropopliteal DCB use in the porcine animal model.Citation49 In this study, downstream skeletal muscle and coronary band were histologically evaluated at 28 and 90 days after treatment with single or overlapping (3×) IN.PACT Admiral DCB vs Lutonix DCB to femoral arteries of healthy swine. Downstream paclitaxel concentration was also measured. Morphometric analysis of overlapping DCBs demonstrated numerically higher neointimal inhibition in IN.PACT Admiral DCB compared with Lutonix DCB at 28 days after the treatment. In addition, SMC loss score (both depth and circumference) was significantly higher for IN.PACT Admiral than Lutonix DCB. The percentage of sections with vascular changes in the downstream nontarget tissues was significantly higher at 90 days with overlapping (×3) IN.PACT Admiral DCB compared with Lutonix DCB (IN.PACT Admiral DCB vs Lutonix DCB: 46.2% vs 0.0%, P=0.01), with similar trends observed at 28 days following single (15.4% vs 7.7%, respectively, P=0.04) or multiple (×3) DCB usage (38.5% vs 7.7%, respectively, P=0.07). Paclitaxel concentration in nontarget skeletal muscle and coronary band was also significantly higher in IN.PACT Admiral DCB com pared with Lutonix DCB.Citation49 Multiple DCB usage in a single lesion is common in the real-world daily clinical practice; therefore, drug levels achieved at site of treatment are likely different in single vs overlapped DCB.
We have also compared the downstream effect of overlapping IN.PACT Admiral DCB, Ranger, and Stellarex at 28 days utilizing similar methods as described in our previous study in the healthy swine femoral artery model.Citation65
The percentage of sections with vascular changes in downstream nontarget tissues was similar for all three DCBs (IN. PACT vs Ranger vs Stellarex: 42.9% vs 25.0% vs 28.6%, respectively, P=0.2). The downstream level of paclitaxel concentration in skeletal muscle was significantly higher for IN.PACT (P=0.01) compared with Ranger and Stellarex.
These two preclinical studies suggest that IN.PACT Admiral has a high prevalence of distal emboli compared with Lutonix DCB, Ranger, and Stellarex (), although the difference between IN.PACT Admiral, Ranger, and Stel- larex was of borderline significance. One possible reason for the higher prevalence of distal emboli may be the higher drug dose in IN.PACT compared with the other three DCBs (IN.PACT DCB vs the other DCBs, 3.5 µg/mm2 vs 2.0 µg/mm2; ). Also, Katsanos et al have demonstrated previously that higher paclitaxel dose (>3.0 µg/mm2) is the main determinant of significantly improved treatment effect, ie, decreased TLR in meta-analysis of the multiple RCTs and registry studies.Citation34 Therefore, it is likely that a balance view must be adopted from a patient perspective; higher drug dose results in higher efficacy but also at the price of more distal emboli.
Figure 2 Representative images of downstream nontarget skeletal muscle and coronary band tissues from healthy swine after treatment of femoral arteries and downstream incidence of distal embolization after treatment with overlapping DCBs at 28 days follow-up.
Source: Reproduced with permission from Reprinted from Journal of Vascular and Interventional Radiology, 27, Frank D. Kolodgie, Erica Pacheco, Kazuyuki Yahagi, Hiroyoshi Mori, Elena Ladich, Renu Virmani, Comparison of Particulate Embolization after Femoral Artery Treatment with IN.PACT Admiral versus Lutonix 035 Paclitaxel-Coated Balloons in Healthy Swine, 1676-1685.e2., © 2016, with permission from Elsevier. And Reprinted from Journal of Vascular and Interventional Radiology, Sho Torii, Hiroyuki Jinnouchi, Atsushi Sakamoto, Maria E. Romero, Frank D. Kolodgie, Renu Virmani, Aloke V. Finn, Comparison of Biologic Effect and Particulate Embolization after Femoral Artery Treatment with Three Drug-Coated Balloons in Healthy Swine Model, Epub ahead of print., © 2018, with permission from Elsevier.Citation68
Abbreviation: DCBs, drug-coated balloons.
Despite a higher prevalence of distal emboli in the preclinical studies, there is no clear evidence in IN.PACT Admiral DCB in either RCTsCitation13–Citation18 or in real-world registriesCitation37,Citation50 of embolic events. Amputation rates were not significantly different in IN.PACT vs BA. Also, the prevalence of downstream embolic events is difficult to evaluate, especially in the RCTs because the patients are generally healthy and highly selected with simple and short lesions. Therefore, it is likely that the patients enrolled in RCTs are less likely to suffer severe complications from emboli. Further studies utilizing larger number of patients with CLI are needed to clarify the impact of embolization.
DCB is logically the best treatment option for ISR lesions, and it is recommended to be class IIb treatment in the latest guidelines.Citation1 Several studies including prospective single-arm studies,Citation51 RCT,Citation50 and registriesCitation16,Citation17 support the efficacy of IN.PACT Admiral DCB treatment for ISR lesions. The FAIR trial was a prospective, multicenter, RCT that compared safety and efficacy of IN.PACT Admiral DCB (n=62) vs BA (n=57) for the treatment of ISR in the femoropopliteal lesions.Citation50 The primary efficacy endpoint was binary restenosis at 6 months. The IN.PACT Admiral DCB arm demonstrated significantly less prevalence of binary restenosis compared with BA arm (IN.PACT Admiral DCB vs BA: 15.4% vs 44.7%, P=0.002). Also, freedom from TLR at 12 months was significantly higher for IN.PACT Admiral DCB arm compared with BA arm (90.8% vs 52.6%, respectively, P<0.001).
Lutonix DCB also demonstrated acceptable results for ISR lesions. Freedom from TLR after Lutonix DCB treatment at 12 and 24 months was 90.7% and 84.6% in Lutonix Global SFA registry.Citation52 In addition, a prospective multicenter RCT that is comparing safety and efficacy of Lutonix DCB is cur rently ongoing (ClinicalTrials.gov Identifier: NCT02063672). These clinical studies suggest that IN.PACT Admiral or the other DCBs should be the primary treatment option for the treatment of ISR lesions.
DCB in infrapopliteal (CLI) lesions
According to the latest clinical guidelines, DCB usage for infrapopliteal lesions is not recommendedCitation1,Citation2 mainly because of the negative result over BA treatment in the IN.PACT DEEPCitation53 and the BIOLUX P-IICitation54 RCTs. In the IN.PACT DEEP trial, a total of 358 patients mostly with CLI were randomized to IN.PACT Amphirion DCB treatment group or BA treatment group. Coprimary efficacy outcomes were TLR and angiographic LLL at 12 months, and the primary safety endpoint was a 6-month composite of all-cause mortality, TLR, or major amputation. There were no differences in CD-TLR between IN.PACT Admiral DCB group and BA group with more complications in IN.PACT Amphirion DCB group with higher prevalence of major amputations (IN.PACT Amphirion DCB vs BA: 8.8% vs 3.6%, P=0.080) and lower amputation-free survival (81.1% vs 89.2%, respectively, P=0.057). It is conceivable that distal emboli and/or nontarget drug delivery of IN.PACT Amphirion DCB, an older generation of IN.PACT Admiral, might have been one of the reasons for the failure. In IN.PACT Amphirion, used in the IN.PACT DEEP trial,Citation53 urea excipient and paclitaxel were “manually” coated “after” folding of the balloon, perhaps leading to variability in coating/drug load.Citation55 This could have led to the nonuniform paclitaxel distribution on the balloon, resulting in the majority of paclitaxel being peeled away during delivery, resulting in less drug delivery as well as distal emboli. A recent real-world registry demonstrated efficacy and safety of Lutonix DCB in the treatment of infrapopliteal arteries;Citation56 however, prospective RCTs comparing standard BA treatment are not available. There are two ongoing randomized clinical trials comparing EVT and surgical therapyCitation57,Citation58 to confirm efficacy of currently available DCBs in patients with CLI.
DCB in heavily calcified lesions
In 2014, Fanelli et al have demonstrated the effect of calcification on the efficacy of DCB during EVT of femoropopliteal lesions.Citation59 In this study, 60 patients with de novo femoro-popliteal lesions were treated with DCBs. The severity of calcification was evaluated with a combination of CT angiography (CTA), digital subtraction angiography (DSA), and intravascular ultrasound (IVUS). Patients were classified into eight groups according to circumferential and longitudinal distribution of calcification evaluated with CTA and DSA. These findings were further confirmed by IVUS images. Pro gressive worsening of clinical outcomes was observed as the severity of calcification increased (). Further analyses confirmed that circumferential distribution of calcification is the most important determinant of DCB efficacy when compared with longitudinal distribution of calcification.
Figure 3 Primary patency and LLL at 12 months after the treatment in eight groups that were classified according to circumferential and longitudinal distribution of calcification.
Source: Reprinted by permission from Springer Nature Customer Service Centre GmbH: Springer Nature CardioVascular and Interventional Radiology Fanelli F, Cannavale A, Gazzetti M, et al. Calcium burden assessment and impact on drug-eluting balloons in peripheral arterial disease. Cardiovasc Intervent Radiol. 2014;37(4):898–907, © 2014.Citation59
Abbreviation: LLL, late lumen loss.
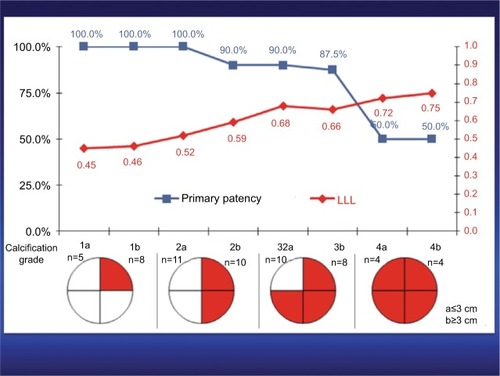
Schmidt et al also demonstrated that heavy calcification is an independent predictor of restenosis following DCB usage with significantly higher risk for the need of provisional stenting.Citation18 Calcification likely acts as a barrier for the transfer and deposition of paclitaxel, leading to greater restenosis. In addition to the “barrier” effects of heavy calcification, a higher risk of recoil and residual stenosis after DCB treatment may also contribute to worse outcome.
We believe DES should be the first line of treatment for severely calcified femoropopliteal lesions since calcification of superficial femoral artery is not itself an independent predictor of restenosis after treatment with DES.Citation60
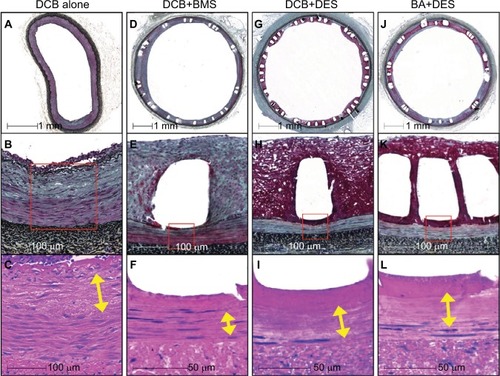
Our preclinical studies in healthy swine iliofemoral artery model support this idea since DES treatment demonstrated significantly higher drug effect (medial SMC loss score) vs DCBCitation61,Citation62 (). Importantly, the median value of circumferential medial SMC loss score was lower (1.2) in DCB than in DES (3.5) treatment groups (scores were dependent on the circumferential distribution of the drug as assessed by loss of SMCs with score of 1= <25%; 2=25 to <50%; 3=50 to <75%, and 4= >75%). The distribution of the treatment effect of DCB (not only circumferential but also transmural in distribution) is not as predictable and reproducible as those observed in DES in animal models. Nevertheless, in severely calcified femoropopliteal lesions, there remains a need for the improvement in DCB technology.
Figure 4 Representative histologic images of the biologic responses to DCB + DES, BA + DES, DCB + BMS, and DCB alone in swine iliofemoral arteries.
Source: Reprinted from Journal of Vascular and Interventional Radiology, 29, Sho Torii,Kazuyuki Yahagi, Hiroyoshi Mori, Emanuel Harari, Maria E. Romero, Frank D. Kolodgie, Brandt Young, Anthony Ragheb, Renu Virmani, Aloke V. Finn, Biologic drug effect and particulate embolization of drug-eluting stents versus drug-coated balloons in healthy swine femoropopliteal arteries, 1041–1049., © 2018, with permission from Elsevier.Citation61
Abbreviations: BA, balloon angioplasty; BMS, bare metal stents; DCB, drug-coated balloon; DES, drug-eluting stents; PTA, percutaneous transluminal angioplasty; SMC, smooth muscle cell.
Conclusion
Three DCBs (IN.PACT Admiral DCB, Lutonix DCB, and Stellarex DCB) have been approved by the FDA following RCTs, and another two DCBs (SurVeil DCB and Ranger DCB) are still to be approved following completion of the trials. However, no trials have been performed to compare the head-to-head efficacy of all the three. All clinical trials have some differences in primary or secondary endpoints, therefore we cannot draw conclusions regarding each one’s efficacy. Although Lutonix DCB was the first to get FDA approval (October 14, 2014) when compared with IN.PACT Admiral DCB (December 30, 2014), long-term results of time to first CD-TLR were significantly different between DCB and PTA at 4 years. Whereas, for Lutonix 035 the primary patency was 58.6% vs 53.0% for PTA. Further work of head-to-head comparison between different DCBs in patients with PAD is needed to examine which DCBs are the most effective.
Disclosure
Sho Torii receives honoraria from Boston Scientific Japan, and Terumo Corporation, and research grants from SUNRISE lab. Renu Virmani and Aloke V Finn have received institutional research support from Abbott Vascular, BioSensors International, Biotronik, Boston Scientific, Cook Medical, Medtronic, and Terumo Corporation. Renu Virmani receives honoraria from Abbott Vascular, Boston Scientific, Cook Medical, Lutonix, Medtronic, and Terumo Corporation, and is a consultant for 480 Biomedical, Abbott Vascular, Medtronic, and W.L. Gore. The authors report no other conflicts of interest in this work.
References
- AboyansVRiccoJBBartelinkMEL2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries endorsed by: the European Stroke Organization (ESO) the task force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS)Eur Heart J201839976381628886620
- Gerhard-HermanMDGornikHLBarrettC2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelinesCirculation201713512e686e72527840332
- FowkesFGRudanDRudanIComparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysisLancet201338299011329134023915883
- NorgrenLHiattWRDormandyJAInter-society consensus for the management of peripheral arterial disease (TASC II)Eur J Vasc Endovasc Surg200733Suppl 1S1S7517140820
- Writing Committee to Develop Clinical Data Standards for Peripheral Atherosclerotic Vascular DiseaseCreagerMABelkinM2012 ACCF/AHA/ACR/SCAI/SIR/STS/SVM/SVN/SVS key data elements and definitions for peripheral atherosclerotic vascular disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Clinical Data Standards for Peripheral Atherosclerotic Vascular Disease)Circulation2012125239546722144570
- DiehmNShangASilvestroAAssociation of cardiovascular risk factors with pattern of lower limb atherosclerosis in 2659 patients undergoing angioplastyEur J Vasc Endovasc Surg2006311596316269257
- LuJTCreagerMAThe relationship of cigarette smoking to peripheral arterial diseaseRev Cardiovasc Med20045418919315580157
- NarulaNDannenbergAJOlinJWPathology of peripheral artery disease in critical limb ischemiaJ Am Coll Cardiol201872182152216330166084
- DakeMDAnselGMJaffMRDurable clinical effectiveness with paclitaxel-eluting stents in the femoropopliteal artery: 5-year results of the zilver PTX randomized trialCirculation2016133151472148326969758
- IqbalJSerruysPWSilberSComparison of zotarolimus- and everolimus-eluting coronary stents: final 5-year report of the RESOLUTE all-comers trialCirc Cardiovasc Interv201586e00223026047993
- IidaONantoSUematsuMEffect of exercise on frequency of stent fracture in the superficial femoral arteryAm J Cardiol200698227227416828607
- SchlagerOZehetmayerSSeidingerDvan der LooBKoppensteinerRWall shear stress in the stented superficial femoral artery in peripheral arterial diseaseAtherosclerosis20142331768224529126
- TepeGLairdJSchneiderPDrug-coated balloon versus standard percutaneous transluminal angioplasty for the treatment of superficial femoral and popliteal peripheral artery disease: 12-month results from the IN.PACT SFA randomized trialCirculation2015131549550225472980
- BrodmannMKeirseKScheinertDDrug-coated balloon treatment for femoropopliteal artery disease: the IN.PACT global study de novo in-stent restenosis imaging cohortJACC Cardiovasc Interv201710202113212329050631
- IidaOSogaYUrasawaKDrug-coated balloon vs standard per-cutaneous transluminal angioplasty for the treatment of atherosclerotic lesions in the superficial femoral and proximal popliteal arteries: one-year results of the MDT-2113 SFA Japan randomized trialJ Endovasc Ther201825110911729264999
- StabileEVirgaVSalemmeLDrug-eluting balloon for treatment of superficial femoral artery in-stent restenosisJ Am Coll Cardiol201260181739174223040582
- VirgaVStabileEBiaminoGDrug-eluting balloons for the treatment of the superficial femoral artery in-stent restenosis: 2-year follow-upJACC Cardiovasc Interv20147441141524630884
- SchmidtAPiorkowskiMGörnerHDrug-coated balloons for complex femoropopliteal lesions: 2-year results of a real-world registryJACC Cardiovasc Interv20169771572427056311
- MedtronicIN.PACT Admiral Drug-Coated Balloon: Overview2018 Available from: https://www.medtronic.com/us-en/healthcare-professionals/products/cardiovascular/drug-coated-balloons/inpact-drug-coated-balloon.htmlAccessed December 16, 2018
- ChaabaneCOtsukaFVirmaniRBochaton-PiallatMLBiological responses in stented arteriesCardiovasc Res201399235336323667187
- PetersonSHasenbankMSilvestroCRainaSIN.PACT™ Admiral™ drug-coated balloon: Durable, consistent and safe treatment for femoropopliteal peripheral artery diseaseAdv Drug Deliv Rev2017112697727771367
- TepeGZellerTAlbrechtTLocal delivery of paclitaxel to inhibit restenosis during angioplasty of the legN Engl J Med2008358768969918272892
- KelschBSchellerBBiedermannMDose response to paclitaxel-coated balloon catheters in the porcine coronary overstretch and stent implantation modelInvest Radiol201146425526321285890
- LiistroFGrottiSPortoIDrug-eluting balloon in peripheral intervention for the superficial femoral artery: the DEBATE-SFA randomized trial (drug eluting balloon in peripheral intervention for the superficial femoral artery)JACC Cardiovasc Interv20136121295130224239203
- PalmeriniTBenedettoUBiondi-ZoccaiGLong-term safety of drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysisJ Am Coll Cardiol201565232496250726065988
- LammerJBosiersMZellerTFirst clinical trial of nitinol self-expanding everolimus-eluting stent implantation for peripheral arterial occlusive diseaseJ Vasc Surg201154239440121658885
- DudaSHBosiersMLammerJDrug-eluting and bare nitinol stents for the treatment of atherosclerotic lesions in the superficial femoral artery: long-term results from the SIROCCO trialJ Endovasc Ther200613670171017154704
- Müller-HülsbeckSKeirseKZellerTSchroëHDiaz-CartelleJTwelve-month results from the majestic trial of the eluvia paclitaxel-eluting stent for treatment of obstructive femoropopliteal diseaseJ Endovasc Ther201623570170727193308
- Müller-HülsbeckSKeirseKZellerTSchroëHDiaz-CartelleJLong-term results from the majestic trial of the eluvia paclitaxel-eluting stent for femoropopliteal treatment: 3-year follow-upCardiovasc Intervent Radiol201740121832183828948322
- ZhaoHQNikanorovAVirmaniRJonesRPachecoESchwartzLBLate stent expansion and neointimal proliferation of oversized Nitinol stents in peripheral arteriesCardiovasc Intervent Radiol200932472072619484292
- ZhaoHQNikanorovAVirmaniRSchwartzLBInhibition of experimental neointimal hyperplasia and neoatherosclerosis by local, stent-mediated delivery of everolimusJ Vasc Surg20125661680168822841285
- HabibAKarmaliVPolavarapuRSirolimus-FKBP12.6 impairs endothelial barrier function through protein kinase C-α activation and disruption of the p120-vascular endothelial cadherin interactionArterioscler Thromb Vasc Biol201333102425243123887639
- CleverYPPetersDCalisseJNovel sirolimus-coated balloon catheter: in vivo evaluation in a porcine coronary modelCirc Cardio-vasc Interv201694e003543
- KatsanosKKitrouPSpiliopoulosSDiamantopoulosAKarnabatidisDComparative effectiveness of plain BA, bare metal stents, drug-coated balloons, and drug-eluting stents for the treatment of infrapopliteal artery disease: systematic review and Bayesian network meta-analysis of randomized controlled trialsJ Endovasc Ther201623685186327708143
- SchellerBSpeckUSchmittABöhmMNickenigGAddition of paclitaxel to contrast media prevents restenosis after coronary stent implantationJ Am Coll Cardiol20034281415142014563585
- GongoraCAShibuyaMWesslerJDImpact of paclitaxel dose on tissue pharmacokinetics and vascular healing: a comparative drug-coated balloon study in the familial hypercholesterolemic swine model of superficial femoral in-stent restenosisJACC Cardiovasc Interv2015881115112326117470
- SchneiderPALairdJRTepeGTreatment effect of drug-coated balloons is durable to 3 years in the femoropopliteal arteries: long-term results of the IN.PACT SFA randomized trialCirc Cardiovasc Interv2018111e00589129326153
- KrishnanPFariesPNiaziKStellarex drug-coated balloon for treatment of femoropopliteal disease: twelve-month outcomes from the randomized ILLUMENATE pivotal and pharmacokinetic studiesCirculation2017136121102111328729250
- SchroederHWernerMMeyerDRLow-dose paclitaxel-coated versus uncoated percutaneous transluminal balloon angioplasty for femoropopliteal peripheral artery disease: one-year results of the ILLU-MENATE European Randomized Clinical Trial (randomized trial of a novel paclitaxel-coated percutaneous angioplasty balloon)Circulation2017135232227223628424223
- RosenfieldKJaffMRWhiteCJTrial of a paclitaxel-coated balloon for femoropopliteal artery diseaseN Engl J Med2015373214515326106946
- BausbackYWillfort-EhringerASievertHSix-month results from the initial randomized study of the ranger paclitaxel-coated balloon in the femoropopliteal segmentJ Endovasc Ther201724445946728558502
- ScheinertDSchulteKLZellerTLammerJTepeGPaclitaxel-releasing balloon in femoropopliteal lesions using a BTHC excipient: twelve-month results from the BIOLUX P-I randomized trialJ Endovasc Ther2015221142125775674
- TepeGGögebakanÖRedlichUAngiographic and clinical outcomes after treatment of femoropopliteal lesions with a novel paclitaxel-matrix-coated balloon catheterCardiovasc Intervent Radiol201740101535154428660441
- GiacoppoDCasseseSHaradaYDrug-coated balloon versus plain balloon angioplasty for the treatment of femoropopliteal artery disease: an updated systematic review and meta-analysis of randomized clinical trialsJACC Cardiovasc Interv20169161731174227539695
- AlbrechtTWaliszewskiMRocaCTwo-year clinical outcomes of the CONSEQUENT trial: can femoropopliteal lesions be treated with sustainable clinical results that are economically sound?Cardiovasc Intervent Radiol20184171008101429589098
- IbrahimTDirschingerRHeinRJaitnerJDownstream panniculitis secondary to drug-eluting balloon angioplastyJACC Cardiovasc Interv2016917e177e17927544006
- ThomasSDMcDonaldRRVarcoeRLVasculitis resulting from a superficial femoral artery angioplasty with a paclitaxel-eluting balloonJ Vasc Surg201459252052323642919
- LakeETwiggMFarquharsonFAcute hypersensitivity reaction to femoral drug-coated balloonsVasa201746322322528045341
- KolodgieFDPachecoEYahagiKMoriHLadichEVirmaniRComparison of particulate embolization after femoral artery treatment with IN.PACT Admiral versus Lutonix 035 paclitaxel-coated balloons in healthy swineJ Vasc Interv Radiol201627111676168527641674
- KrankenbergHTüblerTIngwersenMDrug-coated balloon versus standard balloon for superficial femoral artery in-stent restenosis: the randomized femoral artery in-stent restenosis (fair) trialCirculation2015132232230223626446728
- LiistroFAngioliPPortoIPaclitaxel-eluting balloon vs. standard angioplasty to reduce recurrent restenosis in diabetic patients with in-stent restenosis of the superficial femoral and proximal popliteal arteries: the DEBATE-ISR studyJ Endovasc Ther20142111824502477
- ThiemeMVon BilderlingPPaetzelCThe 24-month results of the Lutonix global SFA Registry: worldwide experience with Lutonix drug-coated balloonJACC Cardiovasc Interv201710161682169028780030
- ZellerTBaumgartnerIScheinertDDrug-eluting balloon versus standard balloon angioplasty for infrapopliteal arterial revascularization in critical limb ischemia: 12-month results from the IN.PACT DEEP randomized trialJ Am Coll Cardiol201464151568157625301459
- ZellerTBeschornerUPilgerEPaclitaxel-coated balloon in infrapopliteal arteries: 12-month results from the BIOLUX P-II randomized trial (BIOTRONIK’S-First in Man Study of the Passeo-18 LUX drug releasing PTA balloon catheter vs. the uncoated Passeo-18 PTA balloon catheter in subjects requiring revascularization of infrapopliteal arteries)JACC Cardiovasc Interv20158121614162226493253
- LairdJRArmstrongEJDrug-coated balloons for infrapopliteal disease: digging deep to understand the impact of a negative trialJ Am Coll Cardiol201464151577157925301460
- ThiemeMLichtenbergMBrodmannMCioppaAScheinertDLutonix® 014 DCB global Below the Knee Registry Study: interim 6-month outcomesJ Cardiovasc Surg201859223223629363894
- PopplewellMADaviesHJarrettHBypass versus angioplasty in severe ischaemia of the leg - 2 (BASIL-2) trial: study protocol for a randomised controlled trialTrials2016171126739146
- MenardMTFarberAAssmannSFDesign and rationale of the best endovascular versus best surgical therapy for patients with critical limb ischemia (BEST-CLI) trialJ Am Heart Assoc201657e00321927402237
- FanelliFCannavaleAGazzettiMCalcium burden assessment and impact on drug-eluting balloons in peripheral arterial diseaseCardiovasc Intervent Radiol201437489890724806955
- IidaOTakaharaMSogaY1-year results of the ZEPHYR Registry (Zilver PTX for the Femoral Artery and Proximal Popliteal Artery): predictors of restenosisJACC Cardiovasc Interv2015881105111226117463
- ToriiSYahagiKMoriHBiologic drug effect and particulate embolization of drug-eluting stents versus drug-coated balloons in healthy swine femoropopliteal arteriesJ Vasc Interv Radiol20182971041104929754850
- ToriiSYahagiKMoriHSafety of Zilver PTX drug-eluting stent implantation following drug-coated balloon dilation in a healthy swine modelJ Endovasc Ther201825111812629161933
- ScheinertDDudaSZellerTThe LEVANT I (Lutonix paclitaxel-coated balloon for the prevention of femoropopliteal restenosis) trial for femoropopliteal revascularization: first-in-human randomized trial of low-dose drug-coated balloon versus uncoated balloon angioplastyJACC Cardiovasc Interv201471101924456716
- SteinerSWillfort-EhringerASievertH12-month results from the first-in-human randomized study of the ranger paclitaxel-coated balloon for femoropopliteal treatmentJACC Cardiovasc Interv2018111093494129730375
- ToriiSMustaphaJANarulaJHistopathologic Characterization of Peripheral Arteries in Subjects With Abundant Risk FactorsJACC Cardiovasc Imaging Epub2018126
- Data Presented for Medtronic’s In.Pact Admiral DCB [webpage on the Internet]WayneEndovascular Today2017 Available from https://evtoday.com/2017/09/12/data-presented-for-medtronics-inpact-admiral-dcbAccessed December 21, 2018
- Bard’s LEVANT 21-Year Data Published in NEJM2-Year Data Presented at SVS [webpage on the Internet]WayneEndovascular Today2015 Available from https://evtoday.com/2015/06/bards-levant-2-1-year-data-published-in-nejm-2-year-data-presented-at-SVSAccessed December 21, 2018
- ToriiSJinnouchiHSakamotoAComparison of Biologic Effect and Particulate Embolization after Femoral Artery Treatment with Three Drug-Coated Balloons in Healthy Swine ModelJ Vasc Interv Radiol201930110310930527654
- GranadaJFVirmaniRSchulz-JanderDTunevSMelderRJRate of drug coating dissolution determines in-tissue drug retention and durability of biological efficacyJ Drug Deliv2018
