Abstract
Background
Increasing long-term evidence supports the safety and effectiveness of minimally invasive sacroiliac joint fusion (SIJF) for sacroiliac joint (SIJ) dysfunction, an important cause of chronic low-back/buttock pain.
Objective
To report 4-year follow-up in patients undergoing SIJF using triangular titanium implants (TTI) as part of two prospective trials.
Methods
We enrolled 103 subjects at 12 centers treated with TTI in two prospective clinical trials (NCT01640353 and NCT01681004) and followed them in the current study (NCT02270203), with clinic visits at 3, 4, and 5 years.
Results
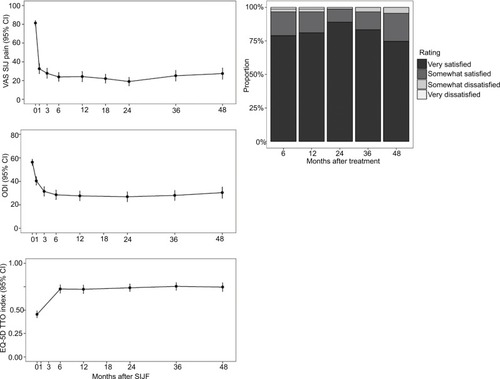
At 4 years, mean SIJ pain scores (available in 91 subjects [88.3%]) had decreased by 54 points from baseline; disability (Oswestry Disability Index) scores decreased by 26 points; and quality of life (EuroQOL-5D) improved by 0.3 points (0–1 scale). Satisfaction rates were high and the proportion of subjects taking opioids decreased from 77% at baseline to 43% at 4-year follow-up.
Conclusion
Four-year follow-up showed continued excellent responses in patients with SIJ pain treated with SIJF using triangular titanium implants.
Introduction
Approximately 15%–30% of all chronic low-back pain involves the sacroiliac joint (SIJ).Citation1–Citation5 Increasing evidence supports the safety and effectiveness of SIJ fusion in patients with chronic SIJ dysfunction, and several device systems are now available. The most commonly studied device – triangular titanium implants (iFuse Implant System, SI-BONE, Santa Clara, CA, USA) – is supported by prospective clinical trialsCitation6–Citation8 as well as a pooled analysis of those trialsCitation9 and numerous case series.Citation10–Citation18 Herein, we report 4-year prospective follow-up, updating a previously published report of the same cohort at 3 years.Citation19
Methods
As previously described, subjects in this study (LOIS, Long Term Outcomes from INSITE and SIFI, NCT02270203) were enrolled at 12 centers that participated in two feeder trials: INSITE (NCT01681004, a prospective, randomized controlled trial of SIJ fusion vs non-surgical management)Citation6 or SIFI (NCT01640353, a prospective multicenter single-arm study).Citation8 In both feeder studies, patients with SIJ pain – diagnosed by history, physical examination, and confirmatory diagnostic SIJ block with local anesthetic – underwent placement of triangular titanium implants in a lateral transiliac fashion during a brief (typically <1 hour) surgery. In the feeder studies, subjects had scheduled follow-up visits up to 2 years. The published 2-year reports showed marked, immediate, and sustained improvements in pain, disability, and quality of life.Citation6,Citation8
Subjects at selected centers enrolled into the current study, which had similar study visits at years 3, 4, and 5 after initial surgery, with telephone visits at 2.5, 3.5, and 4.5 years to maintain contact with participants. At each clinic visit, subjects completed surveys to assess SIJ pain scores using a visual analog (0–100) scale, disability related to back pain as assessed by the Oswestry Disability Index (0 = no disability due to back pain to ≥60 = completely disabled),Citation20 using quality of life ([EuroQOL-5D]; on a 0 [death] to 1 [perfect health] scale),Citation21 overall satisfaction with the procedure, and use of opioid medications for SIJ pain. Questionnaires were identical to those used in the two feeder studies and were administered by trained study research coordinators. Furthermore, study coordinators recorded all negative changes in health as adverse events. The relatedness of the reported event to the index procedure or devices used during the procedure was assessed by the treating physician. All centers obtained institutional review board approval for study conduct.
Results
Of the 103 enrolled subjects, 93 (90.3%) completed 4-year follow-up. Marked improvements in pain (54 points), disability (26 points), and quality of life (0.3 points), previously observed at 3 years, were maintained at 4 years (). Satisfaction rates remained high, except for a slight reduction in the proportion who were very satisfied. The proportion of subjects taking daily opioids decreased from 77% immediately prior to surgery to 43% at the 4-year follow-up.
Figure 1 Left: Improvement in SIJ pain (top), dysfunction due to pain (ODI, middle), and quality of life (EQ5D-TTO, bottom). Right: patient satisfaction levels.
In total, 114 adverse events were reported between years 3 and 4; however, none were rated as probably or definitely related to the study devices or index surgical procedure. Many events indicated underlying degenerative disease associated with age and osteoarthritis (eg, hip, knee, shoulder, neck, and lumbar spine osteoarthritic degeneration). Other than one previously reported subject who underwent surgical revision of the target SIJ at 3.8 years, no other subjects underwent revision procedures between years 3 and 4.
Discussion
In the past, surgeons overlooked the SIJ as a cause of chronic low-back pain, probably because no feasible surgical treatment was available. Our data, reporting the longest prospective follow-up to date, show that SIJ fusion with triangular titanium implants can provide marked and sustained relief of pain, disability, and quality of life in patients for whom no other treatment had provided clinically important relief. Observed improvements were as large as those seen in other commonly conducted spine surgeries. Our data stand in marked contrast to non-surgical treatments, which have shown poor rates of pain relief and increased opioid use.Citation22
Summary
In two prospective clinical trials, 103 subjects with sacroiliac joint dysfunction underwent SIJ fusion with triangular titanium implants. At 4-year follow-up, clinical outcomes were preserved, with no new adverse events related to the index procedure or devices.
Acknowledgments
SI-BONE sponsored this clinical trial.
Disclosure
Emily Darr conducts clinical research as part of prospective trials sponsored by SI-BONE. Daniel Cher is an employee of SI-BONE. The authors report no other conflict of interest in this study.
References
- BernardTNKirkaldy-WillisWHRecognizing specific characteristics of nonspecific low back painClin Orthop Relat Res1987217266280
- SchwarzerACAprillCNBogdukNThe sacroiliac joint in chronic low back painSpine199520131377709277
- MaigneJYAivaliklisAPfeferFResults of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back painSpine19962116188918928875721
- IrwinRWWatsonTMinickRPAmbrosiusWTAgeAWTAge, body mass index, and gender differences in sacroiliac joint pathologyAm J Phys Med Rehabil2007861374417304687
- SembranoJNPollyDWHow often is low back pain not coming from the back?Spine2009341E27E3219127145
- PollyDWSwoffordJWhangPGTwo-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint DysfunctionInt J Spine Surg2016102827652199
- DuhonBSBitanFLockstadtHTriangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: 2-Year Follow-Up from a Prospective Multicenter TrialInt J Spine Surg2016101327162715
- DenglerJDKoolsDPflugmacherR1-Year Results of a Randomized Controlled Trial of Conservative Management vs. Minimally Invasive Surgical Treatment for Sacroiliac Joint PainPain Physician201720653755028934785
- DenglerJDuhonBWhangPPredictors of Outcome in Conservative and Minimally Invasive Surgical Management of Pain Originating From the Sacroiliac Joint: A Pooled AnalysisSpine2017422116641673 Epub March 27, 201728350586
- RudolfLSacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: Report of the First 50 Patients and OutcomesOpen Orthop J20126149550223284593
- RudolfLMIS Fusion of the SI Joint: Does Prior Lumbar Spinal Fusion Affect Patient Outcomes?Open Orthop J2013716316823730380
- SachsDCapobiancoROne year successful outcomes for novel sacroiliac joint arthrodesis systemAnn Surg Innov Res2012611323270468
- SachsDCapobiancoRMinimally invasive sacroiliac joint fusion: one-year outcomes in 40 patientsAdv Orthop2013201353612823997957
- CummingsJCapobiancoRAMinimally invasive sacroiliac joint fusion: one-year outcomes in 18 patientsAnn Surg Innov Res2013711224040944
- SchroederJECunninghamMERossTBoachie-AdjeiOEarly results of sacro-iliac joint fixation following long fusion to the sacrum in adult spine deformityHSS J2014101303524482619
- SmithAGCapobiancoRCherDOpen versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomesAnn Surg Innov Res2013711424172188
- LedonioCGPollyDWSwiontkowskiMFMinimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective?Clin Orthop Relat Res201447261831183824519569
- LedonioCGPollyDWSwiontkowskiMFCummingsJTComparative effectiveness of open versus minimally invasive sacroiliac joint fusionMed Devices201477187193
- DarrEMeyerSCWhangPGLong-term prospective outcomes after minimally invasive trans-iliac sacroiliac joint fusion using triangular titanium implantsMed Devices201811113121
- FairbankJCPynsentPBThe Oswestry Disability IndexSpine2000252229402952 discussion 295211074683
- EuroQol GroupEuroQol-a new facility for the measurement of health-related quality of lifeHealth Policy Amst Neth1990163199208
- VanaclochaVHerreraJMSáiz-SapenaNRivera-PazMVerdú-LópezFMinimally Invasive Sacroiliac Joint Fusion, Radiofrequency Denervation, and Conservative Management for Sacroiliac Joint Pain: 6-Year Comparative Case SeriesNeurosurgery2018821485528431026
