Abstract
Transmyocardial laser revascularization (TMR) emerged as treatment modality for patients with diffuse coronary artery disease not amendable to percutaneous or surgical revascularization. The procedure entails the creation of laser channels within ischemic myocardium in an effort to better perfuse these areas. Currently, two laser devices are approved by the US Food and Drug Administration for TMR – holmium:yttrium–aluminum–garnet and CO2. The two devices differ in regard to energy outputs, wavelengths, ability to synchronize with the heart cycle, and laser–tissue interactions. These differences have led to studies showing different efficacies between the two laser devices. Over 50,000 procedures have been performed worldwide using TMR. Improvements in angina stages, quality of life, and perfusion of the myocardium have been demonstrated with TMR. Although several mechanisms for these improvements have been suggested, evidence points to new blood vessel formation, or angiogenesis, within the treated myocardium, as the major contributory factor. TMR has been used as sole therapy and in combination with coronary artery bypass grafting. Clinical studies have demonstrated that TMR is both safe and effective in angina relief long term. The objective of this review is to present the two approved laser devices and evidence for the safety and efficacy of TMR, along with future directions with this technology.
Introduction
As life expectancy and coronary-event survival rates rise, an increasing number of patients with severe coronary artery disease experience angina that is not amenable to percutaneous coronary intervention or surgical revascularization.Citation1–Citation3 Moreover, up to 25% of coronary artery bypass grafting (CABG) patients have incomplete revascularization, a strong independent predictor of operative mortality and morbidity.Citation4,Citation5 Therefore, a great deal of interest in alternative strategies to traditional revascularization has been pursued. These experimental approaches include pharmacologic interventions,Citation6 enhanced external counterpulsation,Citation7,Citation8 spinal cord stimulation,Citation9 protein,Citation10 gene,Citation11 or stem cell therapyCitation12,Citation13 to promote angiogenesis (the formation of new blood vessels), and the topic of this discussion – transmyocardial laser revascularization (TMR).
TMR is a US Food and Drug Administration (FDA)-approved intervention utilizing a laser device intended to treat ischemic myocardium. This procedure was approved by the FDA in 1998 to treat moderate to severe angina (class 3–4 based on the Canadian Cardiovascular Society Classification SystemCitation14 – ) as a result of diffuse coronary artery disease not amendable to conventional medical therapy, percutaneous coronary intervention, or surgical revascularization via CABG. Over 50,000 TMR procedures have been performed worldwide in more than 38 countries, with over 20,000 performed in the United States to date. Over the past two decades, results from prospective and retrospective studies on TMR have been reported.Citation15–Citation31 A few meta-analyses have also been reported, along with an FDA review on short-term and long-term outcomes with the use of TMR.Citation29,Citation31–Citation33 This review covers two different FDA-approved devices for TMR, evidence-based practice, and future directions aimed at utilizing a combined TMR and stem cell therapy approach.
Table 1 Canadian Cardiovascular Society Angina Classification System
Proposed mechanism
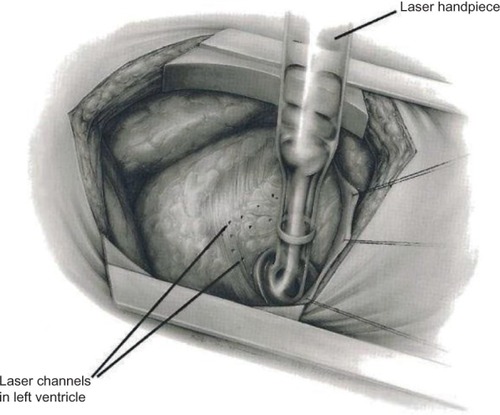
TMR is an approved surgical procedure that induces transmural laser channels within ischemic myocardium. The thought behind direct perfusion to the myocardium was based on descriptions of reptilian heart sinusoids that allowed blood to flow directly from the ventricles into the myocardium, perfusing the heart muscle. TMR creates channels that are 1 mm in diameter, with the number of channels depending on heart size and ischemic territory (). The exact mechanism of angina relief is debated.
Figure 1 Illustration showing left thoracotomy and exposure of the heart for TMR.
Abbreviation: TMR, transmyocardial revascularization.
Patent channels that allow perfusion from the ventricle to the myocardium may provide a potential mechanism for TMR and angina relief. Clinical and experimental work have shown evidence of long-term patency.Citation34,Citation35 However, several autopsy case reports and reviews have demonstrated that channels created by TMR in humans do not remain patent.Citation35–Citation39 Therefore, it is believed that patency of channels providing perfusion to the ischemic myocardium is not the mechanism of action for TMR.
Denervation of the sympathetic nerve fibers innervating the heart is another proposed mechanism of angina relief following TMR. Afferent, sympathetic efferent postganglionic, and parasympathetic efferent postganglionic neurons all innervate the heart. Conflicting experimental evidence has been reported regarding denervation playing a role in angina relief.Citation40–Citation42 These experiments only focused on short-term results. Furthermore, it is difficult to assess and isolate the afferent nerves involved in pain signaling. A study by Al-Sheikh et alCitation43 utilizing positron emission tomography scanning demonstrated that sympathetic denervation occurs following TMR. Nevertheless, evidence indicating that denervation is the primary cause of angina relief is lacking.
Angiogenesis has shown the strongest experimental and clinical evidence for being the primary basis of angina relief after TMR. Several independent groups have provided concrete histological evidence of increased angiogenesis and neovascularization as a direct result of TMR channel creation.Citation44–Citation48 Additionally, upregulation of proangiogenic factors, such as vascular endothelial growth factor, fibroblast growth factor 2, and platelet-derived endothelial cell growth factor, was demonstrated in myocardial tissue following TMR.Citation49–Citation51 This neovascularization process is not specific to laser only, but can also be seen with other means of myocardial channel formation, such as hot and cold needles and radiofrequency ablation. However, TMR minimizes scar formation, which allows optimal functional contribution of the new blood vessels. Therefore, the evidence from a histological and molecular standpoint supports the notion of angiogenesis promotion in the ischemic heart following TMR, with the minimization of scar tissue following channel creation.
Another critical issue explored by several studies is the notion that angiogenesis following TMR may lead to improvement in heart function. Improvement in subjective quality of life was shown following TMR.Citation25 Moreover, objective improvements were demonstrated based on dobutamine stress echocardiography, positron emission tomography scanning, and cardiac magnetic resonance imaging (MRI).Citation52–Citation55 Improvements in perfusion and myocardial function were noted in animal models of chronic myocardial ischemia as well, supporting the proangiogenic basis of improvement.Citation56–Citation59 The role of angiogenesis was further supported by a study that showed emergence of small vessels perfusing the heart on follow-up angiography 10 years after TMR.Citation60 These secondary blood vessels were not present prior to TMR. Thus, neovascularization and angiogenesis seem to be the predominant driving force for angina improvement and increased myocardial perfusion.
Devices
Many different wavelengths of laser light have been studied experimentally, including xenon–chloride,Citation61 neodymium:yttrium–aluminum–garnet (YAG),Citation62 erbium:YAG,Citation63 thulium–holmium–chromium:YAG,Citation64 holmium:YAG (Ho:YAG),Citation61 and CO2.Citation65 Two different laser devices are currently FDA-approved and utilized for TMR () – the Heart Laser CO2 Transmyocardial Revascularization System (Novadaq Technologies Inc., BC, Canada) and the SolarGen TMR Ho:YAG Laser System (CardioGenesis Corporation, Foothill Ranch, CA, USA). In addition to different wavelengths, these lasers employ different energy outputs and require slightly different surgical approaches.
Figure 2 Transmyocardial revascularization lasers.
Abbreviations: Ho:YAG, holmium:yttrium–aluminum–garnet; TMR, transmyocardial revascularization.

The CO2 laser has a wavelength of 10,600 nm and uses an energy level of 15–20 J per pulse with a pulse duration of 25–40 ms. A single pulse is used, and the pulse beam is directed within the device to the myocardium using a system of mirrors (). Using this level of energy and single pulses, the laser photons do not create tissue explosions, limiting the total structural damage (). The CO2 laser is also synchronized with the R-wave (maximal ventricular filling) of the electrocardiogram cycle. Transesophageal echocardiography can be used to confirm accurate transmural channel formation, as a result of vaporization of blood within the ventricle. This characteristic acoustic response is helpful in assessing whether proper laser pulse delivery was achieved.
Figure 3 Illustration of CO2 laser.
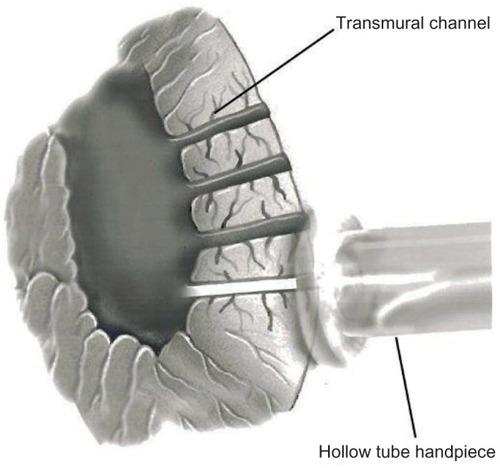
Figure 4 Stop-action photography of laser pulses.
Abbreviation: Ho:YAG, holmium:yttrium–aluminum–garnet.
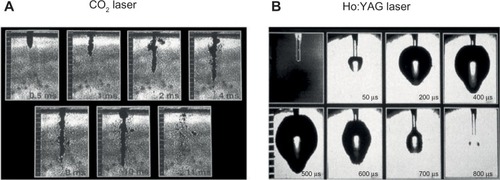
In contrast to the CO2 laser, the Ho:YAG laser system has a wavelength of 2,120 nm and uses pulsed laser beam sequences of 1–2 J and 6–8 W per pulse. This laser beam is projected through a 1 mm fiberoptic bundle at a rate of five pulses per second. The arrival of the sequential pulses must be separated by time in order to allow for proper thermal dissipation to avoid excess heat accumulation. If the pulses are incorrectly timed, this can lead to tissue explosions and subsequent structural trauma, along with thermocoagulation.Citation66 Even with the pulsed low sequences, high levels of peak power are delivered to the tissue, causing small explosions (). During the procedure using the Ho:YAG laser, the laser fiber is advanced manually through the myocardium. Due to this physical manipulation, it is not possible to decipher whether the channel in the myocardium is being created as a result of the mechanical effects of the fiber or whether there has been enough time for thermal dissipation to occur prior to the next initiated pulse. Furthermore, the Ho:YAG laser is unsynchronized to the cardiac cycle and is prone to producing ventricular arrhythmias.
TMR sole therapy
TMR has been performed solely or in combination with other procedures, such as CABG. Sole TMR may be done without the use of cardiopulmonary bypass or anticoagulation. The procedure requires general anesthesia, generally done via a double-lumen endotracheal tube or bronchial blocker to isolate the left lung. Exposure to the left ventricle is obtained via a left anterolateral thoracotomy performed on the fifth intercostal space. Upon laser activation, transesophageal echocardiography is used to monitor whether a successful channel was created with the CO2 laser. Channel formation using the Ho:YAG laser is monitored by tactile and auditory feedback. Upon completion, a chest tube is placed and the thoracotomy is closed. In most cases, the patient is extubated in the operating room.
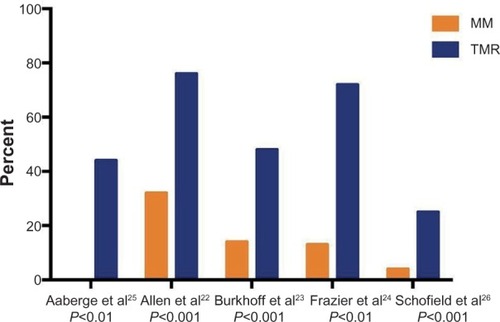
Preliminary nonrandomized trials showed benefit for sole TMR in patients with diffuse coronary artery disease and no other options to alleviate severe angina.Citation15–Citation17 This symptomatic improvement led to prospective randomized control trials, which were designed to test TMR plus optimal medical management versus optimal medical management alone.Citation22–Citation26 Over 1,200 patients were enrolled in these trials. In order to fit inclusion and exclusion criteria, all patients had refractory angina that was not amenable to percutaneous coronary intervention or CABG (confirmed on recent angiogram), evidence of reversible ischemia upon myocardial perfusion scanning, and a left ventricular ejection fraction greater than 25%. Three of the five trials used the CO2 laser,Citation24–Citation26 and two trials used the Ho:YAG laser.Citation22,Citation23 The major subjective endpoint investigated entailed a change in angina symptoms. Other study endpoints included: operative mortality, 1-year survival, myocardial perfusion, exercise tolerance, quality of life, cardiac-related hospitalizations, and major adverse events. Patients were evaluated and assessed at 3 months, 6 months, and 12 months following randomization.
Significant angina improvement was seen in all studies (). Based on all five clinical trials, a summary odds ratio of 9.3 (95% confidence interval =4.6–18.5; P<0.001) for angina reduction was calculated. Moreover, quality of life, freedom from rehospitalization at 1 year, exercise tolerance, and decreased need for nitrates were significantly improved in patients who received laser treatment. A meta-analysis looking at 1-year survival in randomized patients showed similar survival between patients treated with laser and those managed with medical therapy alone.Citation32 Functional analysis looking at myocardial perfusion showed some evidence of improvement in reversible ischemic defects and perfusion of ischemic territories with the CO2 laser.Citation24,Citation26
Figure 5 Angina relief at 12 months.
Abbreviations: MM, medical management; TMR, transmyocardial revascularization.
Long-term follow-up of the prospective randomized controlled trials showed continued angina relief in the TMR group. Specifically, intention-to-treat analyses showed that at a mean of 5 years, 88% of patients who received TMR experienced at least a 2-level reduction in angina class, compared with 44% of patients managed medically (P<0.001).Citation67 Furthermore, long-term analysis of a trial that did not allow crossover between groups showed an improvement in angina symptoms (P<0.001) and reduction in unstable angina hospitalizations in the TMR group (P<0.05) at 43 months of follow-up.Citation25 A long-term outcome analysis conducted by the FDA, Society of Thoracic Surgeons, and Duke Clinical Research Institute showed that there were no differences in long-term morbidity or mortality between CO2 and Ho:YAG lasers used for sole TMR.Citation29 On the basis of the evidence demonstrated by the randomized clinical trials, both the American College of Cardiology/American Heart Association and the Society of Thoracic Surgeons have provided practice guidelines favoring the use of TMR in patients with medically refractive angina not amenable to revascularization procedures.Citation68,Citation69
CABG plus adjuvant TMR
TMR plus CABG is reserved for patients who have ischemia that is able to be bypassed coupled with ischemic zones not amenable to bypass grafting. This combined procedure may be performed with or without the use of cardiopulmonary bypass. Both CO2 and Ho:YAG lasers have been used with this hybrid approach. The efficacy of CABG plus TMR has been challenging to assess, due to the inability to delineate the influence of coronary bypass grafts and also the lack of randomized controlled arms in several studies.Citation70–Citation72
Only two randomized controlled trials assessing CABG plus adjuvant TMR versus CABG alone have been reported.Citation73,Citation74 In these trials, patients were blinded to treatment assignment through 1 year of follow-up. Patient characteristics and number of bypass grafts were similar between groups. Outcomes from one of the trials showed reduced postoperative mortality (1.5% versus 7.6%, P=0.02), increased 30-day freedom from major adverse cardiac events (97% versus 91%, P=0.04), and improved 1-year Kaplan–Meier survival (95% versus 89%, P=0.05).Citation73 The other trial showed a similar trend in postoperative mortality within high-risk patients (9% versus 33%, P=0.09).Citation74 On subsequent 4-year follow-up of these patients, survival was similar between groups; however, there was an increase in the need for revascularization in the CABG-alone group (24% versus 0%, P<0.05).Citation75 Furthermore, a retrospective study showed no difference in survival between TMR plus CABG and CABG-alone groups, although with 4-year follow-up in the TMR plus CABG group there was a sustained improvement in New York Heart Association Classification (P<0.001).Citation76 No differences in long-term outcomes for morbidity and mortality were noted between CO2 and Ho:YAG lasers used in combination with CABG.Citation29
Percutaneous TMR
In an attempt to reduce perioperative morbidity, a minimally invasive percutaneous approach to myocardial revascularization has been previously pursed.Citation77,Citation78 This approach is carried out using a laser fiber inserted into a peripheral artery and guided into the left ventricle. Electromechanical mapping is used to verify the fiber position within the heart. The fiber utilized Ho:YAG laser to create 2–3-mm-deep divots in the subendocardial tissue.
Results with percutaneous myocardial revascularization (PMR) have been less favorable than those observed with TMR.Citation79–Citation81 Furthermore, a pilot study evaluating the efficacy of PMR in combination with percutaneous coronary intervention showed a high rate of periprocedural adverse events (11.5%).Citation82 Given these results, the FDA has rendered PMR unapprovable. The failure associated with PMR may result from several factors. The maximal depth of channel formation is only 6 mm with PMR. This is significantly less than the full-thickness channel formation found with TMR. Additionally, fewer channels are created with PMR. The exact location of channel formation is also a critical issue within the beating ventricle. Lastly, there are inherent limitations with using the Ho:YAG laser in PMR.
TMR plus adjuvant cell therapy
A plethora of research has centered on cell therapy in an effort to stimulate angiogenesis and myogenesis for heart disease. Stem cells, including hematopoietic stem cells, endothelial progenitor cells, mesenchymal stem cells, myoblasts, and undifferentiated side-population cells, have been used clinically with various routes of administration for ischemic heart disease.Citation83–Citation90 Of the different cells studied, bone marrow stem cells have shown promise. It is believed that bone marrow stem cells promote the paracrine secretion of growth factors and cytokines, which stimulate angiogenesis and aid in the survival of cardiomyocytes through the mobilization of progenitor cells.
The combination of cell therapy and TMR has been studied in both animal modelsCitation91 and in several clinical studies.Citation92–Citation97 One group showed that TMR assisted in mesenchymal stem cell engraftment in rat hearts, with corresponding increases in expression of stem cell factor, stromal derived factor-1, c-kit, and chemokine receptor type 4, as compared to control rats who received only stem cells.Citation98 Clinical studies of mesenchymal stem cells plus TMR include individual case reports or series of patients with angina refractory to CABG or percutaneous coronary intervention. The bone marrow stem cells that were transplanted were autologous and harvested on the same day of surgery. All of these studies demonstrated that injection of stem cells in addition to TMR was safe and showed an improvement in angina class. Several studies showed some evidence of improvement in perfusion and left ventricular contractility.Citation94–Citation96 One of the major limitations of these studies is lack of differentiation between the effects of injected autologous stem cells versus laser revascularization. Furthermore, these studies may have been limited as a result of the small number of cells being injected due to no ex vivo expansion of these stem cells prior to injection. Future investigation into the concomitant use of cell therapy and TMR is warranted.
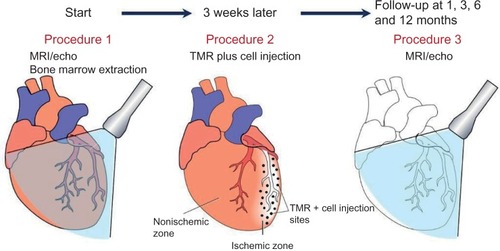
Our group is currently working on an NIH-sponsored clinical trial (NCT01557543) to study the effects of direct injection of ex-vivo-expanded autologous mesenchymal stem cells in patients undergoing CABG or TMR using the CO2 laser (). The outcomes of interest include cardiac function, quality of life, and reduction of cardiac events in patients versus historical controls at 3 months and 6 months after intervention. With expansion of the autologous mesenchymal stem cells ex vivo coupled with direct injection into the myocardium, we believe this technique should provide further clinical benefit in addition to the CABG or TMR procedure.
Figure 6 Procedural timeline for NIH Clinical Trial (NCT01557543) in patients undergoing TMR plus direct mesenchymal stem cell injections.
Abbreviations: MRI, magnetic resonance imaging; NIH, National Institutes of Health; TMR, transmyocardial revascularization.
Conclusion
TMR is a surgical procedure pioneered in the 1990s that provides angina relief to patients with diffuse coronary disease. The predominant theory behind improvement involves myocardial angiogenesis leading to increased perfusion. Both Ho:YAG and CO2 laser devices have been approved by the FDA. TMR can be combined with CABG to target ischemic areas that cannot be readily bypassed. Safety of the procedure and long-term angina relief has been shown both with sole TMR and with CABG plus adjuvant TMR. PMR with the use of Ho:YAG has been attempted as a minimally invasive option of TMR, yet it has demonstrated less-favorable results than TMR. Finally, current efforts have been aimed at combining TMR with adjuvant stem cell therapy to better improve functional outcomes in patients.
Disclosure
The authors have no commercial associations or financial disclosures that might pose or create a conflict of interest with information presented in this manuscript (such associations include consultancies, stock ownership, or other equity interests, patent licensing arrangements, and payments for conducting or publicizing a study described in the manuscript). The authors report no other conflicts of interest in this work.
References
- MannheimerCCamiciPChesterMRThe problem of chronic refractory angina; report from the ESC Joint Study Group on the Treatment of Refractory AnginaEur Heart J200223535537011846493
- JolicoeurEMGrangerCBHenryTDWorking Group MembersClinical and research issues regarding chronic advanced coronary artery disease: part I: Contemporary and emerging therapiesAm Heart J2008155341843418294474
- JolicoeurEMOhmanEMTempleRWorking Group MembersClinical and research issues regarding chronic advanced coronary artery disease part II: Trial design, outcomes, and regulatory issuesAm Heart J2008155343544418294475
- WeintraubWSJonesELCraverJMGuytonRAFrequency of repeat coronary bypass or coronary angioplasty after coronary artery bypass surgery using saphenous venous graftsAm J Cardiol19947321031128296729
- OsswaldBRBlackstoneEHTochtermannUDoes the completeness of revascularization affect early survival after coronary artery bypass grafting in elderly patients?Eur J Cardiothorac Surg200120112012511423284
- PatelPDAroraRRUtility of ranolazine in chronic stable angina patientsVasc Health Risk Manag20084481982419065998
- AroraRRChouTMJainDThe multicenter study of enhanced external counterpulsation (MUST-EECP): effect of EECP on exercise-induced myocardial ischemia and anginal episodesJ Am Coll Cardiol19993371833184010362181
- ManchandaASoranOEnhanced external counterpulsation and future directions: step beyond medical management for patients with angina and heart failureJ Am Coll Cardiol200750161523153117936150
- EckertSHorstkotteDManagement of angina pectoris: the role of spinal cord stimulationAm J Cardiovasc Drugs200991172819178129
- SimonsMAnnexBHLahamRJPharmacological treatment of coronary artery disease with recombinant fibroblast growth factor-2: double-blind, randomized, controlled clinical trialCirculation2002105778879311854116
- KastrupJJørgensenERückAEuroinject One GroupDirect intramyocardial plasmid vascular endothelial growth factor-A165 gene therapy in patients with stable severe angina pectoris A randomized double-blind placebo-controlled study: the Euroinject One trialJ Am Coll Cardiol200545798298815808751
- ZhouYWangSYuZHoytRFJrQuXHorvathKAMarrow stromal cells differentiate into vasculature after allogeneic transplantation into ischemic myocardiumAnn Thorac Surg20119141206121221353199
- BoomsmaRAGeenenDLMesenchymal stem cells secrete multiple cytokines that promote angiogenesis and have contrasting effects on chemotaxis and apoptosisPLoS One201274e3568522558198
- CampeauLLetter: Grading of angina pectorisCirculation1976543522523947585
- HorvathKAManntingFCummingsNShernanSKCohnLHTransmyocardial laser revascularization: operative techniques and clinical results at two yearsJ Thorac Cardiovasc Surg19961115104710538622302
- CooleyDAFrazierOHKadipasaogluKATransmyocardial laser revascularization: clinical experience with twelve-month follow-upJ Thorac Cardiovasc Surg19961114791797 discussion 797–7998614139
- HorvathKACohnLHCooleyDATransmyocardial laser revascularization: results of a multicenter trial with transmyocardial laser revascularization used as sole therapy for end-stage coronary artery diseaseJ Thorac Cardiovasc Surg19971134645653 discussion 653–6549104973
- KrabatschTTambeurLLiebackEShaperFHetzerRTransmyocardial laser revascularization in the treatment of end-stage coronary artery diseaseAnn Thorac Cardiovasc Surg19984264719577000
- HattlerBGGriffithBPZenatiMATransmyocardial laser revascularization in the patient with unmanageable unstable anginaAnn Thorac Surg19996841203120910543480
- MilanoAPrataliSTartariniGEarly results of transmyocardial revascularization with a holmium laserAnn Thorac Surg19986537007049527198
- DowlingRDPetracekMRSelingerSLAllenKBTransmyocardial revascularization in patients with refractory, unstable anginaCirculation199898Suppl 19II73II75 discussion II75–II769852884
- AllenKBDowlingRDFudgeTLComparison of transmyocardial revascularization with medical therapy in patients with refractory anginaN Engl J Med1999341141029103610502592
- BurkhoffDSchmidtSSchulmanSPTransmyocardial laser revascularisation compared with continued medical therapy for treatment of refractory angina pectoris: a prospective randomised trial. ATLANTIC Investigators. Angina Treatments-Lasers and Normal Therapies in ComparisonLancet1999354918288589010489946
- FrazierOHMarchRJHorvathKATransmyocardial revascularization with a carbon dioxide laser in patients with end-stage coronary artery diseaseN Engl J Med1999341141021102810502591
- AabergeLRootweltKBlomhoffSSaatvedtKAbdelnoorMForfangKContinued symptomatic improvement three to five years after transmyocardial revascularization with CO(2) laser: a late clinical follow-up of the Norwegian Randomized trial with transmyocardial revascularizationJ Am Coll Cardiol200239101588159312020484
- SchofieldPMSharplesLDCaineNTransmyocardial laser revascularisation in patients with refractory angina: a randomised controlled trialLancet1999353915251952410028979
- JonesJWSchmidtSERichmanBWHolmium:YAG laser transmyocardial revascularization relieves angina and improves functional statusAnn Thorac Surg199967615961601 discussion 1601–160210391261
- HorvathKAResults of prospective randomized controlled trials of transmyocardial laser revascularizationHeart Surg Forum200251333911937460
- TavrisDRBrennanJMSedrakyanALong-term outcomes after transmyocardial revascularizationAnn Thorac Surg20129451500150822835557
- HorvathKAArankiSFCohnLHSustained angina relief 5 years after transmyocardial laser revascularization with a CO(2) laserCirculation200110412 Suppl 1I81I8411568035
- BrionesELacalleJRMarinITransmyocardial laser revascularization versus medical therapy for refractory anginaCochrane Database Syst Rev20091CD00371219160223
- ChengDDiegelerAAllenKTransmyocardial laser revascularization: a meta-analysis and systematic review of controlled trialsInnovations (Phila)20061629531322436830
- LiaoLSarria-SantameraAMatcharDBMeta-analysis of survival and relief of angina pectoris after transmyocardial revascularizationAm J Cardiol200595101243124515878002
- CooleyDAFrazierOHKadipasaogluKAPehlivanogluSShannonRLAngeliniPTransmyocardial laser revascularization. Anatomic evidence of long-term channel patencyTex Heart Inst J19942132202248000270
- HorvathKASmithWJLaurenceRGSchoenFJAppleyardRFCohnLHRecovery and viability of an acute myocardial infarct after transmyocardial laser revascularizationJ Am Coll Cardiol19952512582637798512
- KrabatschTSchäperFLederCTülsnerJThalmannUHetzerRHistological findings after transmyocardial laser revascularizationJ Card Surg19961153263318969377
- GasslerNWintzerHOStubbeHMWullbrandAHelmchenUTransmyocardial laser revascularization. Histological features in human nonresponder myocardiumCirculation19979523713759008451
- BurkhoffDFisherPEApfelbaumMKohmotoTDeRosaCMSmithCRHistologic appearance of transmyocardial laser channels after 4 1/2 weeksAnn Thorac Surg199661515321534 discussion 1534–15358633979
- SigelJEAbramovitchCMLytleBWRatliffNBTransmyocardial laser revascularization: three sequential autopsy casesJ Thorac Cardiovasc Surg19981156138113859628684
- KwongKFKanellopoulosGKNikolsJCTransmyocardial laser treatment denervates canine myocardiumJ Thorac Cardiovasc Surg19971146883889 discussion 889–8909434682
- HirschGMThompsonGWAroraRCHirschKJSullivanJAArmourJATransmyocardial laser revascularization does not denervate the canine heartAnn Thorac Surg1999682460468 discussion 468–46910475413
- MinisiAJTopazOQuinnMSMohantyLBCardiac nociceptive reflexes after transmyocardial laser revascularization: implications for the neural hypothesis of angina reliefJ Thorac Cardiovasc Surg2001122471271911581603
- Al-SheikhTAllenKBStrakaSPCardiac sympathetic denervation after transmyocardial laser revascularizationCirculation1999100213514010402442
- FisherPEKhomotoTDeRosaCMSpotnitzHMSmithCRBurkhoffDHistologic analysis of transmyocardial channels: comparison of CO2 and holmium:YAG lasersAnn Thorac Surg19976424664729262595
- ZlotnickAYAhmadRMReulRMLaurenceRGAretzHTCohnLHNeovascularization occurs at the site of closed laser channels after transmyocardial laser revascularizationSurg Forum199648286287
- KohmotoTFisherPEDeRosaCSmithCRBurkhoffDEvidence of angiogenesis in regions treated with transmyocardial laser revascularizationCirculation19969481714
- SpanierTSmithCRBurkhoffDAngiogenesis: a possible mechanism underlying the clinical benefits of transmyocardial laser revascularizationJ Clin Laser Med Surg19971562692739641082
- HughesGCLoweJEKypsonAPNeovascularization after transmyocardial laser revascularization in a model of chronic ischemiaAnn Thorac Surg1998666202920369930489
- HorvathKAChiuEMaunDCUp-regulation of vascular endothelial growth factor mRNA and angiogenesis after transmyocardial laser revascularizationAnn Thorac Surg199968382582910509969
- LiWChibaYKimuraTTransmyocardial laser revascularization induced angiogenesis correlated with the expression of matrix metalloproteinases and platelet-derived endothelial cell growth factorEur J Cardiothorac Surg200119215616311167105
- PelletierMPGiaidASivaramanSAngiogenesis and growth factor expression in a model of transmyocardial revascularizationAnn Thorac Surg199866112189692432
- DonovanCLLandolfoKPLoweJEClementsFColemanRBRyanTImprovement in inducible ischemia during dobutamine stress echocardiography after transmyocardial laser revascularization in patients with refractory angina pectorisJ Am Coll Cardiol19973036076129283515
- FrazierOHCooleyDAKadipasaogluKAMyocardial revascularization with laser. Preliminary findingsCirculation199592Suppl 9II58II657586462
- LahamRJSimonsMPearlmanJDHoKKBaimDSMagnetic resonance imaging demonstrates improved regional systolic wall motion and thickening and myocardial perfusion of myocardial territories treated by laser myocardial revascularizationJ Am Coll Cardiol20023911811755279
- HorvathKAKimRJJuddRMParkerMAFullertonDAContrast enhanced MRI assessment of microinfarction after transmyocardial laser revascularizationCirculation200010218II-765
- HorvathKAGreeneRBelkindNKaneBMcPhersonDDFullertonDALeft ventricular functional improvement after transmyocardial laser revascularizationAnn Thorac Surg19986637217259768921
- HughesGCKypsonAPSt LouisJDImproved perfusion and contractile reserve after transmyocardial laser revascularization in a model of hibernating myocardiumAnn Thorac Surg19996761714172010391280
- KrabatschTModersohnDKonertzWHetzerRAcute changes in functional and metabolic parameters following transmyocardial laser revascularization: an experimental studyAnn Thorac Cardiovasc Surg20006638338811173353
- LutterGMartinJvon SamsonPHeilmannCSaraiKBeyersdorfFMicroperfusion enhancement after TMLR in chronically ischemic porcine heartsCardiovasc Surg20019328129111336852
- SansoneFDatoGMZingarelliELate angiograms ten years after transmyocardial laser revascularizationCoron Artery Dis201122858358421959715
- HughesGCKypsonAPAnnexBHInduction of angiogenesis after TMR: a comparison of holmium: YAG, CO2, and excimer lasersAnn Thorac Surg200070250450910969671
- WhittakerPSpariosuKHoZZSuccess of transmyocardial laser revascularization is determined by the amount and organization of scar tissue produced in response to initial injury: results of ultraviolet laser treatmentLasers Surg Med199924425326010327042
- GenykIAFrenzMOttBWalpothBHSchaffnerTCarrelTPAcute and chronic effects of transmyocardial laser revascularization in the nonischemic pig myocardium by using three laser systemsLasers Surg Med200027543845011126438
- YanoOJBielefeldMRJeevanandamVPrevention of acute regional ischemia with endocardial laser channelsAnn Thorac Surg199356146538328875
- HorvathKAClinical studies of TMR with the CO2 laserJ Clin Laser Med Surg19971562812859641084
- KadipaşaogluKASartoriMMasaiTIntraoperative arrhythmias and tissue damage during transmyocardial laser revascularizationAnn Thorac Surg199967242343110197664
- AllenKBDowlingRDAngellWWTransmyocardial revascularization: 5-year follow-up of a prospective, randomized multicenter trialAnn Thorac Surg20047741228123415063241
- GibbonsRJAbramsJChatterjeeKAmerican College of CardiologyAmerican Heart Association Task Force on Practice GuidelinesCommittee on the Management of Patients With Chronic Stable Angina. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina – summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina)Circulation2003107114915812515758
- BridgesCRHorvathKANugentWCSociety of Thoracic SurgeonsThe Society of Thoracic Surgeons practice guideline series: transmyocardial laser revascularizationAnn Thorac Surg20047741484150215063303
- TrehanNMishraMBapnaRMishraAMaheshwariPKarlekarATransmyocardial laser revascularisation combined with coronary artery bypass grafting without cardiopulmonary bypassEur J Cardiothorac Surg19971222762849288519
- StamouSCBoyceSWCookeRHCarlosBDSweetLCCorsoPJOne-year outcome after combined coronary artery bypass grafting and transmyocardial laser revascularization for refractory angina pectorisAm J Cardiol200289121365136812062729
- WehbergKEJulianJSToddJCOgburnNKloppEBuchnessMImproved patient outcomes when transmyocardial revascularization is used as adjunctive revascularizationHeart Surg Forum20036532833014721803
- AllenKBDowlingRDDelRossiAJTransmyocardial laser revascularization combined with coronary artery bypass grafting: a multicenter, blinded, prospective, randomized, controlled trialJ Thorac Cardiovasc Surg2000119354054910694615
- FrazierOHBoyceSWGriffithBPTransmyocardial revascularization using a synchronized CO2 laser as adjunct to coronary artery bypass grafting: results of a prospective, randomized multi-center trial with 12-month follow-upCirculation1999100I-1248
- FrazierOHTuzunEEichstadtHTransmyocardial laser revascularization as an adjunct to coronary artery bypass grafting: a randomized, multicenter study with 4-year follow-upTex Heart Inst J200431323123915562842
- EldaifSMLattoufOMKilgoPGuytonRAPuskasJDThouraniVHLong-term outcomes after CABG with concomitant CO2 transmyocardial revascularization in comparison with CABG aloneInnovations (Phila)20105210310822437356
- KimCBOesterleSNPercutaneous transmyocardial revascularizationJ Clin Laser Med Surg19971562932989641086
- LauerBJunghansUStahlFKlugeROesterleSNSchulerGCatheter-based percutaneous myocardial laser revascularization in patients with end-stage coronary artery diseaseJ Am Coll Cardiol19993461663167010577553
- OesterleSNSanbornTAAliNPercutaneous transmyocardial laser revascularisation for severe angina: the PACIFIC randomised trial. Potential Class Improvement From Intramyocardial ChannelsLancet200035692431705171011095257
- StoneGWTeirsteinPSRubensteinRA prospective, multicenter, randomized trial of percutaneous transmyocardial laser revascularization in patients with nonrecanalizable chronic total occlusionsJ Am Coll Cardiol200239101581158712020483
- LeonMBKornowskiRDowneyWEA blinded, randomized, placebo-controlled trial of percutaneous laser myocardial revascularization to improve angina symptoms in patients with severe coronary diseaseJ Am Coll Cardiol200546101812181916286164
- StoneGWSt GoarFGTaussigAPowerJAKosinskiEShawlFFirst experience with hybrid percutaneous transmyocardial laser revascularization and angioplasty in patients with lesions at high risk for restenosis: Results of a phase I feasibility studyAm Heart J2001142467968311579359
- AssmusBSchächingerVTeupeCTransplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI)Circulation2002106243009301712473544
- AssmusBFischer-RasokatUHonoldJOPCARE-CHD RegistryTranscoronary transplantation of functionally competent BMCs is associated with a decrease in natriuretic peptide serum levels and improved survival of patients with chronic postinfarction heart failure-results of the TOPCARE-CHD registryCirc Res200710081234124117379833
- StrauerBEBrehmMZeusTRegeneration of human infarcted heart muscle by intracoronary autologous bone marrow cell transplantation in chronic coronary artery disease: the IACT StudyJ Am Coll Cardiol20054691651165816256864
- MeyerGPWollertKCLotzJIntracoronary bone marrow cell transfer after myocardial infarction: 5-year follow-up from the randomized-controlled BOOST trialEur Heart J200930242978298419773226
- PerinECDohmannHFBorojevicRTransendocardial, autologous bone marrow cell transplantation for severe, chronic ischemic heart failureCirculation2003107182294230212707230
- ZohlnhöferDOttIMehilliJREVIVAL-2 InvestigatorsStem cell mobilization by granulocyte colony-stimulating factor in patients with acute myocardial infarction: a randomized controlled trialJAMA200629591003101016507801
- PatelANGeffnerLVinaRFSurgical treatment for congestive heart failure with autologous adult stem cell transplantation: a prospective randomized studyJ Thorac Cardiovasc Surg200513061631163816308009
- HeldmanAWDiFedeDLFishmanJETransendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC-HFT randomized trialJAMA20143111627324247587
- PatelANSpadaccioCKuzmanMImproved cell survival in infarcted myocardium using a novel combination transmyocardial laser and cell delivery systemCell Transplant200716989990518293888
- Babin-EbellJSieversHHCharitosEITransmyocardial laser revascularization combined with intramyocardial endothelial progenitor cell transplantation in patients with intractable ischemic heart disease ineligible for conventional revascularization: preliminary results in a highly selected small patient cohortThorac Cardiovasc Surg2010581111620072970
- Konstanty-KalandykJPiątekJMiszalski-JamkaTThe combined use of transmyocardial laser revascularisation and intramyocardial injection of bone-marrow derived stem cells in patients with end-stage coronary artery disease: one year follow-upKardiol Pol201371548549223788089
- ReyesGAllenKBAlvarezPMid term results after bone marrow laser revascularization for treating refractory anginaBMC Cardiovasc Disord2010104220849586
- GowdakLHSchettertITRochitteCETransmyocardial laser revascularization plus cell therapy for refractory anginaInt J Cardiol2008127229529717669519
- GowdakLHSchettertITRochitteCECell therapy plus transmyocardial laser revascularization for refractory anginaAnn Thorac Surg200580271271416039237
- KleinHMGhodsizadABorowskiAAutologous bone marrow-derived stem cell therapy in combination with TMLR. A novel therapeutic option for endstage coronary heart disease: report on 2 casesHeart Surg Forum200475E416E41915799915
- ShahzadULiGZhangYYauTMTransmyocardial revascularization induces mesenchymal stem cell engraftment in infarcted heartsAnn Thorac Surg201294255656222542071
