Abstract
Background
The mainstay of sacroiliac joint disruption/degenerative sacroiliitis therapy has been nonoperative management. This nonoperative management often includes a regimen of physical therapy, chiropractic treatment, therapeutic injections, and possibly radiofrequency ablation at the discretion of the treating physician. When these clinical treatments fail, sacroiliac joint fusion has been recommended as the standard treatment. Open and minimally invasive (MIS) surgical techniques are typical procedures. This study aims to compare the perioperative measures and Oswestry Disability Index (ODI) outcomes associated with each of these techniques.
Methods
A comparative retrospective chart review of patients with sacroiliac joint fusion and a minimum of 1 year of follow-up was performed. Perioperative measures and ODI scores were compared using the Fisher’s exact test and two nonparametric tests, ie, the Mann–Whitney U test and the Wilcoxon signed-rank test. The results are presented as percent or median with range, as appropriate.
Results
Forty-nine patients from two institutions underwent sacroiliac joint fusion between 2006 and 2012. Ten patients were excluded because of incomplete data, leaving 39 evaluable patients, of whom 22 underwent open and 17 underwent MIS sacroiliac joint fusion. The MIS group was significantly older (median age 66 [39–82] years) than the open group (median age 51 [34–74] years). Surgical time and hospital stay were significantly shorter in the MIS group than in the open group. Preoperative ODI was significantly greater in the open group (median 64 [44–78]) than in the MIS group (median 53 [14–84]). Postoperative improvement in ODI was statistically significant within and between groups, with MIS resulting in greater improvement.
Conclusion
The open and MIS sacroiliac joint fusion techniques resulted in statistically and clinically significant improvement for patients with degenerative sacroiliitis refractory to nonoperative management. However, the number of patients reaching the minimal clinically important difference and those showing overall improvement were greater in the MIS group.
Introduction
The sacroiliac joint is a frequent source of pain in patients presenting with low back or buttock pain.Citation1–Citation13 In a recent study by Sembrano and Polly, 200 consecutive new patients were examined in a spine clinic with a chief complaint of low back pain and no prior history of spine, sacroiliac joint, or hip surgery.Citation12 Sixty-five percent of these patients were found to have pain attributed to the spine only, while 5% had pain attributed to the sacroiliac joint only, and 14.5% had pain attributed to both.Citation12
The mainstay of therapy for disorders of the sacroiliac joint has been nonoperative treatment, including modification of activity, nonsteroidal anti-inflammatory drugs, physical therapy, sacroiliac joint injections, and radiofrequency ablation.Citation6,Citation13,Citation14 The durability of these interventions is not well established. When nonoperative treatment fails, surgical arthrodesis has been the standard treatment. Many different techniques have been described for fusion of the sacroiliac joint.Citation15
To date, the clinical studies have primarily consisted of small case series using a variety of assessments of success.Citation16 More recently, the Oswestry Disability Index (ODI) has been used to evaluate outcomes in patients with sacroiliac joint pain.Citation17 This tool is well validated for patients with low back pain.Citation18 Because of the overlap between low back pain and sacroiliac joint pain, it makes intuitive sense to use it.
With the use of a common outcome tool, it is then possible to compare treatment efficacy between the different fusion techniques. While this does not provide the same level of evidence as a randomized controlled trial, it does provide some potential insight into the effect of different treatments.
The aim of this research was to compare the perioperative measures and patient-reported outcomes of two different surgical techniques for sacroiliac joint fusion. The first group was a cohort of patients who underwent arthrodesis using an open anterior ilioinguinal approach, local bone grafting, and anterior plating (open group). The second group underwent minimally invasive surgery (MIS), comprising transgluteal, iliosacral fixation with triangular, porous coated titanium implants (MIS group).
Materials and methods
This retrospective comparative study was exempted by our institutional review board. The patients underwent either open or MIS sacroiliac joint fusion by one of two spine surgeons. One orthopedic surgeon performed exclusively open operations while the neurosurgeon performed exclusively MIS procedures. All patients had sacroiliac joint disruption/degenerative sacroiliitis confirmed by specific provocative physical examination tests, diagnostic/therapeutic fluoroscopic image-guided sacroiliac joint injections using a local anesthetic and steroid, and had failed nonoperative treatment.Citation19 Deidentified medical records for patients with a minimum of 1-year follow-up were reviewed and analyzed. A minimal clinically important difference (MCID) for the ODICitation12 of 12.8 was applied to the differences between the preoperative and postoperative ODI scores for both groups. The MCID is defined as the smallest change in a treatment outcome that a patient would identify as important and has been used previously in the treatment of lumbar spine disorders.Citation20
The Fisher’s exact test was used to compare categorical measures, such as sex of patient and history of prior lumbar surgery. The Shapiro–Wilk test was applied to check for normal or skewed distributions. The Mann–Whitney U test was used to compare measures such as patient age, surgical time, and ODI scores between groups, and the Wilcoxon signed-rank test was used to compare preoperative and postoperative ODI scores within groups. The level of significance of all tests was set at 0.05. All tests were performed using Vassar Stats.Citation21 A Hochberg correction for multiple comparisons was performed.Citation22 The results are presented as percent for categorical variables, such as male and female, or median with range for continuous variables, such as age and ODI scores.
Open anterior sacroiliac joint fusion technique
The sacroiliac joint was approached anteriorly through an ilioinguinal incision of approximately 20 cm in length. The skin and subcutaneous tissue were incised. With sharp dissection, the external oblique and gluteal fascia were exposed and an interval developed. The iliacus was elevated from the iliac fossa with a subperiosteal dissection and a retractor placed inside the iliopectineal line of the pelvis. With retraction, electrocautery was used to expose the superior capsule of the sacroiliac joint. Under headlamp illumination, the capsule was removed off the iliac and sacral portion of the sacroiliac joint with a 15 blade. A pointed Hohmann retractor was inserted on the sacral ala after careful exposure. The sacroiliac joint cartilage was resected using a series of curettes and rongeurs, removing all cartilage back to the posterior ligament and structures. A bone graft was harvested from the inner table of the ilium then morselized. All the bone graft was packed into the sacroiliac joint after predrilling both the sacral and the iliac side with multiple 2.5 mm drill holes. A three-hole 4.5 mm reconstruction plate was contoured and fixed with a fully threaded 6.5 mm cancellous screw on the sacral side and with two cortical screws on the iliac side (). The plate was inspected to make sure there was no soft tissue under it or stretched over it. The soft tissues were allowed to fall back in place and a 1/8 inch Hemovac drain was placed into the iliac fossa. Gelfoam (Pfizer, Inc, New York, New York, USA) was placed into the bone graft harvest site. The external oblique and transversalis fascia were repaired to the gluteal fascia with multiple figure-of-eight sutures and the wound closed in layers.
Figure 1 Postoperative radiograph of a pelvis with a three-hole reconstruction plate spanning the sacroiliac joint.

Postoperatively, a program of gradual return to weight-bearing and exercise was employed. This protocol consisted of toe-touch weight-bearing for 6 weeks, 4 weeks of pool therapy with progressive weight-bearing, and finally 8 weeks of land-based therapy focusing on core body strengthening.
Minimally invasive sacroiliac joint fusion
MIS sacroiliac joint fusion using a series of triangular fusion implants (iFuse implant system; SI-BONE Inc., San Jose, CA, USA) was performed in all cases by a single neurosurgeon in private practice. The patient was placed in the prone position on a radiolucent table to facilitate the use of intraoperative fluoroscopy. After general endotracheal anesthesia was administered, the patient was prepped in the normal sterile fashion. A 3 cm lateral incision was made into the buttock region and the gluteal fascia was bluntly dissected to reach the outer table of the ilium. A Steinmann pin was passed through the ilium across the sacroiliac joint lateral to the neural foramen within the sacrum. After a soft tissue protector was passed over the pin, a hand drill was used to create a pathway and decorticate the bone. Finally, a triangular broach was used to further decorticate the bone and prepare the pathway to receive the first implant. Using a pin guidance system, a total of three implants were placed. The most cephalad implant was seated within the sacral ala. The second implant was generally located above or immediately lateral to the S1 foramen, and the third between the S1 and S2 foramina (). The incision was then irrigated and the tissue layers were closed with Vicryl and Monocryl sutures (Ethicon, Inc, Somerville, NJ, USA).
Figure 2 Postoperative radiograph demonstrating placement of three fusion implants across the sacroiliac joint.

Patients were instructed to ambulate with the assistance of a walker for the first 4 weeks, after which time toe-touch ambulation was recommended for a further 4 weeks. After 8 weeks of gradual return to full weight-bearing, the patients began 4 weeks of physical therapy.
Results
From 2006 to 2012, 49 consecutive patients from two institutions underwent either open or MIS sacroiliac joint fusion. Of these patients, ten were excluded due to incomplete records, resulting in 39 patients included in the analysis, ie, 22 in the open group and 17 in the MIS group. There was a total of 12 statistical comparisons, and a HochbergCitation22 correction for multiple comparisons was performed. This correction resulted in P-values ≤0.01 being significant. In the open group, there were 13 females and nine males with a median age of 51 (range 3 4–74) years, while the MIS group had eleven females and six males with a median age of 66 (range 39–82) years; the MIS patients were significantly older than the open group patients (). Of the 22 patients in the open group, eleven (50%) had a history of spine surgery, while 14 of 17 (82%) patients in the MIS group had a history of spine surgery (). The surgical time for the open group (median 128 [range 73–180] minutes) was significantly longer than that for the MIS group (median 27 [range 18–72] minutes), and the length of hospital stay for the open group (median 3 [range 2–6] days) was significantly longer than that for the MIS group (median 1 [range 1–2] days, ).
Table 1 Comparative analysis of demographics and perioperative measures between groups
ODI scores
ODI scores were collected preoperatively and at a median of 15 (range 11–18) months postoperatively in the MIS group and at a median of 13 (range 11–33) months postoperatively in the open group. The postoperative ODI scores improved significantly compared with baseline scores in both groups, from a median of 64 (range 44–78) to a median of 46 (range 10–80) in the open group ( and ) and from a median of 53 (range 14–84) to a median of 13 (range 0–30) in the MIS group ( and ). In addition, the ODI change in the MIS group (median 4 2 [range 0 –80]) was significantly greater than that in the open group (median 9 [range –8 to 56], ). Finally, the percent change was significantly greater in the MIS group (median 78% [range 0%–100%]) compared with the open group (median 6% [range –13% to 85%], ).
Figure 3 Plot of ODI scores per patient in open sacroiliac joint fusion group.
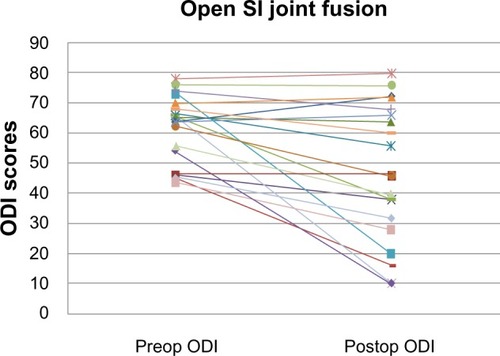
Figure 4 Plot of ODI scores per patient in the MIS SI joint fusion group.
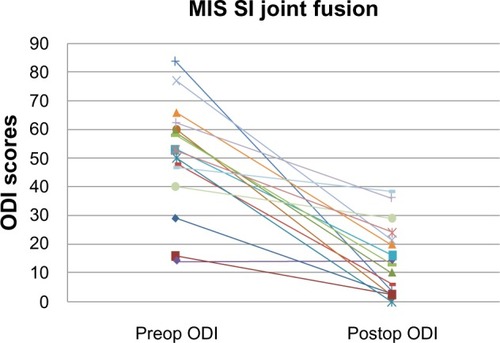
Table 2 Comparing ODI scores between groups and within groups
ODI scores did not improve in all patients. In the open group, the scores were worse in four patients (18%), unchanged in three patients (14%), and improved in 15 patients (68%). In the MIS group, ODI scores were unchanged in one patient (6%) and improved in 16 patients (94%). Ten patients in the open group (45%) reached the threshold of MCID and 14 patients (82%) reached the threshold of MCID in the MIS group ().
Table 3 Comparing patients reaching MCID between groups
There was no significant difference in preoperative ODI scores between open group patients with prior lumbar surgery (median 68 [range, 44–78]) and those without prior lumbar surgery (median 64 [range 44–73], P>0.114). Similarly, there was no significant difference in postoperative ODI scores between open group patients with prior lumbar surgery (median 60 [range 10–80]) and those without prior lumbar surgery (median 44 [range 10–72], P>0.167). The sample size of the MIS patients without prior lumbar surgery (n=3) was too small for analysis with the nonparametric Mann–Whitney U test, so this test was not performed.
Complications
There were no intraoperative complications in the MIS group. Postoperatively, three patients in the MIS group experienced transient trochanteric bursitis and were treated with medical management, one patient developed a hematoma at the operative site, one patient had transient toe numbness of unclear relationship to sacroiliac joint fusion surgery, and one patient had a malpositioned implant that was subsequently removed. There were three complications in the open group, with one patient developing pulmonary embolism that resolved with treatment and two requiring revision due to a failed implant and nerve root irritation.
Discussion
In this study, both techniques resulted in significant clinical improvement for patients, consistent with several previously reported case series demonstrating improvement using various assessment tools.Citation17,Citation23–Citation27 The percentage of patients who reached the threshold for an MCID of 12.8 pointsCitation28–Citation31 indicates that the change was not only statistically significant but also clinically significant. However, the MIS group experienced over four times greater improvement in ODI score (median 42 versus 9, respectively) and 82% of patients exceeded MCID values (versus 45% in the open group). In addition, the median percent difference in ODI was significantly greater in the MIS group than in the open group (median 78% versus 16%, respectively). Finally, the surgical times and length of hospital stay were significantly reduced in the MIS group.
Although the MIS group demonstrated several advantages compared with the open group, this information is a little harder to interpret because there is heterogeneity between the two cohorts. For example, although not statistically significant, the open group was more disabled than the MIS group at baseline, as indicated by the mean preoperative ODI scores. It is possible that the MIS technique gives slightly greater percentage improvement or it could be that patients who have greater initial disability have less improvement with surgical intervention. Propensity-matched cohorts or a randomized controlled trial (RCT) would be required to investigate this question further.
There are significant limitations to this study. The criteria for selection of these two cohorts are that there were preoperative and postoperative ODI scores available for patients initially diagnosed with a sacroiliac joint disorder. The selection process for offering surgery to the patients was based upon the individual surgeon’s experience. The patients had undergone a trial of nonoperative management and failed. Image-guided diagnostic/therapeutic sacroiliac blocks were used to confirm the sacroiliac joint as the generator of their pain. There was no prespecified threshold of relief that was used as a cutoff, although most agree that a minimum patient self-report of at least 50% pain relief for the duration of the local anesthetic is a minimum criterion. In addition, the patients were treated at two medical centers by two different surgeons, which may have contributed to the different effects of the treatments.
There are many potential confounding variables in the treatment of patients with sacroiliac joint pain. Frequently they have spine pathology that may have been treated surgically and the ODI as used does not discriminate between sacroiliac joint-based low back/buttock pain and spine-based low back/buttock pain. While there is compelling evidence that there are radiographic changes within the sacroiliac joint after lumbosacral fusion, it is not well established that these radiographic findings have a high correlation with symptoms.Citation32,Citation33 Similarly, it is not clear if patients with previous spine fusions respond to all sacroiliac joint fusion techniques in a manner similar to that of patients who have isolated sacroiliac joint pain. Poorer outcomes were reported by Slinkard et alCitation20 who used an open anterior approach and Mason et alCitation34 using a hollow modular anchorage screw MIS technique, while Rudolf,Citation26 Cummings and Capobianco,Citation35 and Sachs and CapobiancoCitation36 reported similar outcomes for both patient groups after using the same triangular implant as that used in the present study.
Another limitation is that the ODI is a patient self-report of pain and limitation.Citation37 Other studies in spine pathology suggest that a patient’s psychological status affects their interpretation of pain.Citation38 Similarly, workers’ compensation is a well-recognized negative prognostic factor for patients with low back pain.Citation39 Presumably, this will be similar for patients with sacroiliac joint pain. Emerging data and thought also suggest that socioeconomic status affects outcomes as well.Citation40,Citation41 These were not controlled for or compared in this cohort.
Further, the postoperative treatment protocol was not prespecified and varied between the two cohorts. Even when the postoperative protocol is well specified, the authors’ experience is that patient compliance is variable. Patients’ willingness to comply with toe-touch weight-bearing starts to decrease when they start to feel better. The optimal postoperative regimen merits further study.
On the other hand, this study also has several strengths. For example, preoperative and postoperative ODI outcomes were available for two distinct surgical treatments used in sacroiliac joint disorders. The comparative nature of this study with its patient-reported outcomes reflects actual clinical practice at two different centers but with similar patient populations. Lastly, this study provides some evidence that sacroiliac joint fusion can result in functional improvement, regardless of technique.
Of note, cases for the open SI joint fusion group in this study is the same cohort from a recently published propensity matched study by Ledonio et al but the cases for the MIS group in this study are not.Citation42
In the future, development of standard reporting of the nonoperative treatment strategy, diagnostic strategy, and standardized reporting of patient characteristics will improve the comparability of surgical cohorts. This will allow propensity-matching and provide better insight as to whether or not a particular surgical technique is better than another.
Conclusion
In conclusion, both the open and MIS sacroiliac joint fusion techniques resulted in statistically and clinically significant improvement for patients with sacroiliac joint pain refractory to nonoperative management who had a temporary response to image-guided diagnostic/therapeutic block. However, MIS sacroiliac joint fusion resulted in at least four-fold improvement in ODI scores over the open technique (median 44 versus 9, respectively). Additionally, nearly 40% more patients in the MIS group reached MCID, and the surgical times and hospital stays were significantly reduced. Surgeons who treat sacroiliac disorders via their surgical technique of choice are encouraged to report their case series using the ODI and attempt to characterize their patient cohorts as much as possible. This will allow the different techniques to be compared in the future.
Author contributions
CGTL, DWP, MFS, and JTC Subtantially contributed to the study design. CGTL and DWP collected and analyzed the outcomes, and drafted the manuscript. All authors provided critical revisions to the manuscript, and provided final approval to the published version. All authors are accountable for all aspects of the article including the accuracy and integrity.
Disclosure
JTC is a paid consultant of SI-BONE Inc. CGTL, DWP, and MFS report no conflicts of interest in this work.
References
- SlipmanCWLipetzJSPlastarasCTFluoroscopically guided therapeutic sacroiliac joint injections for sacroiliac joint syndromeAm J Phys Med Rehabil20018042543211399003
- SlipmanCWSterenfeldEBChouLHThe value of radionuclide imaging in the diagnosis of sacroiliac joint syndromeSpine199621225122548902970
- SlipmanCWSterenfeldEBChouLHThe predictive value of provocative sacroiliac joint stress maneuvers in the diagnosis of sacroiliac joint syndromeArch Phys Med Rehabil1998792882929523780
- GemmellHAJacobsonBHIncidence of sacroiliac joint dysfunction and low back pain in fit college studentsJ Manipulative Physiol Ther19901363672137851
- ChanKFMusculoskeletal pain clinic in Singapore – sacroiliac joint somatic dysfunction as cause of buttock painAnn Acad Med Singapore1998271121159588285
- BernardTNJrKirkaldy-WillisWHRecognizing specific characteristics of nonspecific low back painClin Orthop Relat Res19872172662802951048
- KatzVSchoffermanJReynoldsJThe sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrumJ Spinal Disord Tech200316969912571491
- Kirkaldy-WillisWHFive common back disorders: how to diagnose and treat themGeriatrics1978333233152221
- Kirkaldy-WillisWHHillRJA more precise diagnosis for low-back painSpine19794102109162546
- MaigneJYAivaliklisAPfeferFResults of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back painSpine199621188918928875721
- SchwarzerACAprillCNBogdukNThe sacroiliac joint in chronic low back painSpine19952031377709277
- SembranoJNPollyDWJrHow often is low back pain not coming from the back?Spine200934E27E3219127145
- BernardTNJrCassidyJDThe Sacroiliac Joint Syndrome: Pathophysiology, Diagnosis and ManagementNew York, NY, USARaven Press1991
- SpikerWRLawrenceBDRaichALSurgical versus injection treatment for injection-confirmed chronic sacroiliac joint painEvid Based Spine Care J20123415323526911
- StarkJGFuentesJAFuentesTIThe history of sacroiliac joint arthrodesis: a critical review and introduction of a new techniqueCurr Orthop Pract201122545557
- AckermanSPDKimEKnightTYerbySWhat is the frequency of minimally invasive sacroiliac joint fusion annually in the United States?Paper presented at the 8th Interdisciplinary World Congress on Low Back and Pelvic PainOctober 27–31, 2013Dubai
- Al-KhayerAHegartyJHahnDPercutaneous sacroiliac joint arthrodesis: a novel techniqueJ Spinal Disord Tech20082135936318600147
- DjurasovicMGlassmanSDDimarJR2ndDoes fusion status correlate with patient outcomes in lumbar spinal fusion?Spine20113640440921325934
- LaslettMAprillCNMcDonaldBProvocation sacroiliac joint tests have validity in the diagnosis of sacroiliac joint painArch Phys Med Rehabil20068787416731225
- SlinkardNAgelJSwiontkowskiMFDocumentation of outcomes for sacroiliac joint fusion: does prior spinal fusion influence the outcome?Eur Spine J2013222318232423975440
- Vassarstats.net [homepage on the Internet]Richard Lowry, Vassar CollegePoughkeepsie, NY1998–2014 Available from www.vassarstats.netLast accessed January 31, 2014
- HochbergYA sharper Bonferroni procedure for multiple tests of significanceBiometrika198875800802
- BuchowskiJMKebaishKMSinkovVFunctional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac jointSpine J2005552052816153580
- KhuranaAGuhaARMohantyKPercutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcomeJ Bone Joint Surg Br20099162763119407297
- RudolfLSacroiliac joint arthrodesis – MIS technique with titanium implants: report of the first 50 patients and outcomesOpen Orthop J2012649550223284593
- RudolfLMIS fusion of the SI joint: Does prior lumbar spinal fusion affect patient outcomes?Open Orthop J2013716316823730380
- WiseCLDallBEMinimally invasive sacroiliac arthrodesis: outcomes of a new techniqueJ Spinal Disord Tech20082157958419057252
- CopayAGGlassmanSDSubachBRMinimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scalesSpine J2008896897418201937
- GatchelRJMayerTGChouRWhat does/should the minimum clinically important difference measure? A reconsideration of its clinical value in evaluating efficacy of lumbar fusion surgeryClin J Pain20122838739722395333
- LauridsenHHHartvigsenJMannicheCResponsiveness and minimal clinically important difference for pain and disability instruments in low back pain patientsBMC Musculoskelet Disord200678217064410
- CarreonLYBratcherKRCananCEDifferentiating minimum clinically important difference for primary and revision lumbar fusion surgeriesJ Neurosurg Spine20121810210623157276
- ElgafyHSemaanHBEbraheimNAComputed tomography findings in patients with sacroiliac painClin Orthop200138211211811153977
- HaKYLeeJSKimKWDegeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-upSpine2008331192119818469692
- MasonLWChopraIMohantyKThe percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: a prospective outcome studyEur Spine J201322102325233123686478
- CummingsJJrCapobiancoRAMinimally invasive sacroiliac joint fusion: one-year outcomes in 18 patientsAnn Surg Innov Res201371224040944
- SachsDCapobiancoRMinimally invasive sacroiliac joint fusion: one-year outcomes in 40 patientsAdv Orthop2013201353612823997957
- CarreonLYGlassmanSDHowardJFusion and nonsurgical treatment for symptomatic lumbar degenerative disease: a systematic review of Oswestry Disability Index and MOS Short Form-36 outcomesSpine J2008874775518037354
- PollockRLakkolSBudithiCEffect of psychological status on outcome of posterior lumbar interbody fusion surgeryAsian Spine J2012617818222977697
- WebsterBSVermaSPranskyGSOutcomes of workers’ compensation claimants with low back pain undergoing intradiscal electrothermal therapySpine20042943544115094540
- CampbellPWynne-JonesGMullerSThe influence of employment social support for risk and prognosis in nonspecific back pain: a systematic review and critical synthesisInt Arch Occup Environ Health20128611913722875173
- MrozTENorvellDCEckerEFusion versus nonoperative management for chronic low back pain: do sociodemographic factors affect outcome?Spine201136S75S8621952191
- LedonioCGPollyDWJrSwiontkowskiMFMinimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective? Clin Orthop Relat ResJune2014472618311838
